Abstract
Background
The occurrence of nasopharyngeal tuberculosis is rare even in areas where tuberculosis is endemic. Here, we report a case of rare primary nasopharyngeal tuberculosis, promptly evaluated by nasolaryngoscopy.
Case presentation
A 78-year-old woman presented with postnasal drip and a cough of 1-month duration. Endoscopic examination of the nasopharynx revealed irregular mucosal thickening of the right lateral and posterior wall of the naso (epi)-pharynx, which was covered with yellow discharge presenting as postnasal drip. Computed tomography (CT) demonstrated enhanced soft tissue area in the right lateral and posterior wall of the nasopharynx. Bacteriological examination from a nasopharyngeal swab revealed that staining for acid-fast bacilli was positive and the quenching probe PCR test was positive for Mycobacterium tuberculosis. Histopathological examination from the thickening nasopharyngeal mucosa revealed granulomatous formation with caseous necrosis. Ziehl-Nielsen staining directly could detect acid-fast bacilli. Chest X-ray and CT scan ruled out the pulmonary tuberculosis. Base on these findings, we diagnosed it as primary nasopharyngeal tuberculosis. After six months anti-tuberculous therapy, the patient’s symptoms had completely disappeared. Nasolaryngoscopic examination and CT image after 6 months post therapy revealed a normal nasopharynx with complete resolution of the lesion.
Conclusion
We recommend endoscopic examination for patients suffering from chronic postnasal drips to avoid inappropriate diagnosis.
Similar content being viewed by others
Background
Mild symptoms related to the nasopharynx can be easily overlooked, and may present themselves as serious medical conditions at a later stage. When symptoms become chronic, nasolaryngoscopy is used to rule out serious medical conditions such as malignancies. Nasolaryngoscopy is easy to learn, safe, painless, convenient to perform, and readily accepted by patients. Furthermore, it also allows direct visualization and evaluation of both the lesion and the nasopharynx and larynx anatomy, under local anesthesia. It thus allows for early diagnosis and treatment in a primary care center by reducing unnecessary referral [1, 2].
The occurrence of nasopharyngeal tuberculosis is rare even in areas where tuberculosis is endemic. Our literature search for primary nasopharyngeal tuberculosis revealed that very few cases have been published thus far [3–5]. Here, we report a case of rare primary nasopharyngeal tuberculosis, promptly evaluated by nasolaryngoscopy.
Case presentation
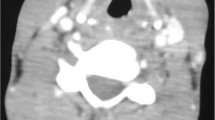
A 78-year-old woman presented with postnasal drip and a cough of one month duration. There were no cervical lymph nodes palpable. General symptoms of tuberculosis (evening rise fever and weight loss) were not observed. Endoscopic examination of the nasopharynx revealed irregular mucosal thickening of the right lateral and posterior wall of the naso (epi)-pharynx, which was covered with yellow discharge presenting as postnasal drip (Fig. 1a). Computed tomography (CT) demonstrated enhanced soft tissue area in the right lateral and posterior wall of the nasopharynx (Fig. 1b). Bacteriological examination from a nasopharyngeal swab revealed that staining for acid-fast bacilli was positive (Gaffky-1) and the quenching probe PCR test was positive for Mycobacterium tuberculosis. Moreover, QuantiFERON-TB Gold was positive. Histopathological examination from the thickening nasopharyngeal mucosa revealed granulomatous formation with caseous necrosis (Fig. 1c). Ziehl-Nielsen staining directly could detect acid-fast bacilli (Fig. 1d). Indigenous bacterial flora was only detected in sputum culture. Chest X-ray and CT scan ruled out the pulmonary tuberculosis (Fig. 1e and f). Base on these findings, we diagnosed it as primary nasopharyngeal tuberculosis. After six months anti-tuberculous therapy, the patient’s symptoms (sore throat and postnasal drip) had completely disappeared. Repeat bacteriological examination of the nasopharyngeal swab at the same time was negative for acid-fast bacilli. The quenching probe PCR test was also negative for Mycobacterium tuberculosis. Nasolaryngoscopic examination and CT image after 6 months post therapy revealed a normal nasopharynx with complete resolution of the lesion (Fig. 1g and h).
Nasopharyngeal tuberculosis. a Nasolaryngoscopic examination showing irregular mucosal thickening of the right lateral and posterior wall of naso (epi)-pharynx, which was covered with yellow discharge presenting as postnasal drip (arrow). b Computed tomography (CT) of the nasopharynx. CT images showing the enhanced soft tissue area in the right lateral and posterior wall of the nasopharynx (arrow). c Histopathological examination of the thickened nasopharyngeal mucosa showing granuloma formation with caseous necrosis. d Ziehl-Nielsen staining from biopsy specimens with acid-fast bacilli (arrow). Chest X-ray e and CT scan f ruled out the pulmonary tuberculosis. g and h Nasolaryngoscopic examination and CT image after 6 months anti-tuberculous therapy showing a normal nasopharynx with complete resolution of the lesion
Conclusions
Nasopharyngeal tuberculosis is commonly associated with cervical lymphadenopathy [3, 4]. In the present case, we did not find any palpable or enlarged lymph nodes on clinical and CT scan examination, respectively. Although nasopharyngeal tuberculosis may present itself in many ways, signs and symptoms can be missed easily if they are less obvious [5]. Such symptoms in the form of chronic cough and postnasal drip were found in the present case, which is rather unusual. We wish to highlight the fact that considering the age of the patient and chronicity of symptoms, this case could have been diagnosed much earlier if a nasolaryngoscopy had been performed. As early as 1988, a study of nasolaryngoscopy has shown that family physicians can perform the procedure with a mean examination time of 4.6 min with good patient tolerability [6]. Although, primary nasopharyngeal tuberculosis is extremely rare [4], we recommend endoscopic examination by family physicians at primary care centers for patients with chronic nasopharyngeal complaints.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Abbreviations
- CT:
-
computed tomography
- PCR:
-
polymerase chain reaction
References
Hayes JT, Houston R. Flexible nasolaryngoscopy. A low-risk, high-yield procedure. Postgrad Med. 1999;106(3):107–10. 114.
Hocutt Jr JE, Corey GA, Rodney WM. Nasolaryngoscopy for family physicians. Am Fam Physician. 1990;42(5):1257–68.
Srirompotong S, Yimtae K, Jintakanon D. Nasopharyngeal tuberculosis: manifestations between 1991 and 2000. Otolaryngol Head Neck Surg. 2004;131(5):762–4.
Tse GM, Ma TK, Chan AB, Ho FN, King AD, Fung KS, Ahuja AT. Tuberculosis of the nasopharynx: a rare entity revisited. Laryngoscope. 2003;113(4):737–40.
Patil C, Kharat Patil R, Deshmukh P, Biswas J, John B. Primary tuberculosis of nasopharynx (adenoid)- a rare presentation. Asian Pac J Trop Med. 2013;6(3):246–8.
Corey GA, Hocutt Jr JE, Rodney WM. Preliminary study of rhinolaryngoscopy by family physicians. Fam Med. 1988;20(4):262–5.
Acknowledgement
Medical writing services were provided by Cactus Communications. The authors retained full control of the manuscript content.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interest
The authors declare that they have no competing interests.
Authors’ contributors
YN were involved in the patient diagnosis and management. YN, RS, TM and TT drafted and revised the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nakao, Y., Shibata, R., Murohara, T. et al. Primary nasopharyngeal tuberculosis: a case report. BMC Infect Dis 16, 121 (2016). https://doi.org/10.1186/s12879-016-1449-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-1449-7