Abstract
Background
Although neonatal infections cause a significant proportion of deaths in the first week of life, little is known about the burden of neonatal disease originating from maternal infection or colonization globally. This paper describes the prevalence of vertical transmission – the percentage of newborns with neonatal infection among newborns exposed to maternal infection.
Methods
We searched Pubmed, Embase, Scopus, Web of Science, Cochrane Library, and WHO Regional Databases for studies of maternal infection, vertical transmission, and neonatal infection. Studies that measured prevalence of bacterial vertical transmission were included. Random effects meta-analyses were used to pool data to calculate prevalence estimates of vertical transmission.
Results
122 studies met the inclusion criteria. Only seven studies (5.7%) were from very high neonatal mortality settings. Considerable heterogeneity existed between studies given the various definitions of infection (lab-confirmed, clinical signs), colonization, and risk factors of infection. The prevalence of early onset neonatal lab-confirmed infection among newborns of mothers with lab-confirmed infection was 17.2% (95%CI 6.5-27.9). The prevalence of neonatal lab-confirmed infection among newborns of colonized mothers was 0% (95% CI 0.0-0.0). The prevalence of neonatal surface colonization among newborns of colonized mothers ranged from 30.9-45.5% depending on the organism. The prevalence of neonatal lab-confirmed infection among newborns of mothers with risk factors (premature rupture of membranes, preterm premature rupture of membranes, prolonged rupture of membranes) ranged from 2.9-19.2% depending on the risk factor.
Conclusions
The prevalence of early-onset neonatal infection is high among newborns of mothers with infection or risk factors for infection. More high quality studies are needed particularly in high neonatal mortality settings to accurately estimate the prevalence of early-onset infection among newborns at risk.
Similar content being viewed by others
Background
Neonatal infections account for a significant proportion of neonatal deaths in the first week of life [1]. In sub-Saharan Africa, south Asia, and Latin America where neonatal infections are most prevalent, the case fatality risk associated with possible severe bacterial infections in the first month of life is 9.8% [2]. Infections are one of the three major causes of neonatal mortality and account for approximately a quarter of newborn deaths in the first month of life [3]. Neonatal infections are acquired horizontally (from the environment) or vertically (from mother). Not much is known about the routes of transmission globally where different environments and risk factors may affect paths of transmission. In resource-rich settings, interventions such as intrapartum antibiotic prophylaxis for high risk women has been effective in reducing the incidence of early-onset neonatal sepsis. In contrast, these interventions are rare or absent in resource-poor settings, which have the highest rates of neonatal mortality. To develop research priorities and strategies for prevention, we need to better understand the prevalence of neonatal infections that are maternally acquired. In this systematic review and meta-analysis, we estimate the prevalence of early-onset neonatal infection in cases where the pregnant woman was infected or colonized with bacterial pathogens (hereafter referred to “vertical transmission”) to better understand the global rates of vertical transmission. We used a relaxed inclusion criteria to include studies that at minimum measured maternal infections and neonatal infections without necessarily having the comparison group of women without maternal infections.
Methods
Definitions and classification
Although laboratory confirmed infections are considered the gold standard measure of infection, the limited number of studies in African, eastern Mediterranean, and southeast Asian regions with laboratory capabilities would underestimate the prevalence of neonatal sepsis among pregnant women who were infected or colonized. Rather than restricting to only lab-confirmed definitions, we also included clinical signs, colonization, and risk factors for infection (maternal only) to best estimate the prevalence of vertical transmission. We specified these definitions, our methods of analysis, and our inclusion criteria in a protocol a priori.
We defined our exposure, maternal infection or colonization during labor, in three categories:
-
(i)
Maternal Infection
-
Laboratory confirmed bacterial infection (hereafter referred to as “lab”): culture or PCR confirmed bacteremia, amnionitis, urinary tract infections, chorioamnionitis;
-
Clinical signs of infection (hereafter referred to as “signs”): intrapartum maternal fever, uterine tenderness, maternal tachycardia, malodorous vaginal discharge, elevated white cell count, elevated c-reactive protein, physician diagnosis of clinical chorioamnionitis using a combination of the above signs, or clinical infection undefined.
-
-
(ii)
Maternal Colonization: positive reproductive tract/genital bacterial cultures without signs or symptoms of infection.
-
(iii)
Risk factors for infection: premature rupture of membranes (PROM - rupture of membranes prior to onset of labor ≥ 37 weeks gestation), preterm premature rupture of membranes (PPROM - rupture of membranes prior to onset of labor < 37 weeks gestation), and prolonged rupture of membranes (duration of rupture of membranes [ROM] ≥ 18-24 hours or undefined).
The outcome, early-onset neonatal infection or colonization during the first seven days of life, was defined in two categories:
-
(i)
Neonatal Infection
-
Laboratory confirmed bacterial infection (“lab”): bacteremia, meningitis, urinary tract infection (positive culture of blood, cerebral spinal fluid, or urine);
-
Clinical signs of infection (“signs”): pneumonia, fever, hypothermia, respiratory distress, bradycardia, tachycardia, irritability, lethargy, hypotonia, seizures, poor feeding, oxygen requirement, increased frequency of apnea, poor capillary refill, metabolic acidosis, elevated white cell count, high immature to total neutrophil ratio, elevated c-reactive protein, or physician diagnosis of clinical sepsis using a combination of the above signs;
-
Laboratory or clinical infection (hereafter referred to as “lab/lab&signs”): a combination of either laboratory confirmed infection or clinical signs of infection, or undefined.
-
-
(ii)
Newborn Colonization: positive ear canal, umbilical, axilla, or anal cultures without signs or symptoms of infection.
We use the term “maternal exposure” as an overarching description of exposures and “neonatal outcome” to describe the outcomes.
Search strategy and section criteria
We searched Pubmed (Medline), Embase, Scopus, Web of Science, the Cochrane Library, and the World Health Organization (WHO) Regional Databases. A comprehensive search strategy was developed with three concepts: maternal infection, vertical transmission, and neonatal infection (Additional file 1: Table S1). We performed final searches of databases on February 20, 2012 with no date restrictions. We downloaded and reviewed articles using EndNote (version X4). Hand-searches through the reference lists of screened articles and published systematic reviews did not produce any additional articles. Source articles included publications, abstracts, and conference proceedings available in the public domain.
We included studies of any design that measured the prevalence or incidence (assumed to be period prevalence) of bacterial vertical transmission, or contained raw data to calculate these measures, even if vertical transmission was not the main aim of the study. To be included, studies needed to be original full-text articles, provide a measure of maternal exposures and a measure of neonatal outcomes, and be written in English. We excluded studies if: the sample size was less than ten; all subjects (pregnant women) received antibiotics or steroids; or data related to nonbacterial infections, tetanus infections, or sexually transmitted infections such as chlamydia and syphilis, which have different mechanisms of transmission.
Screening and data abstraction
Two reviewers independently screened titles, abstracts, and articles using predetermined selection criteria and standardized data abstraction forms. Two data abstractors independently gathered data from included studies to assess risk of bias, classify exposures and outcomes, determine the number of newborns in each exposure-outcome category, and calculate a prevalence measure. One reviewer abstracted study characteristics data. To improve data quality, a second reviewer abstracted study characteristics for a random 10% of the studies. At each stage, the reviewers compared their results and resolved disagreements by reaching a consensus. For articles missing information critical to our analysis, we contacted the authors to request the missing data.
We obtained basic data on author, country, study design, sample size, and study setting: (1) health facility, multi-center, or community-based, and (2) urban versus rural. The studies provided limited data on intrapartum antibiotic use; we categorized studies based on whether they had no intrapartum antibiotic use, some antibiotic use, or unknown if the study did not report antibiotic use. We defined our outcome, early-onset neonatal infection, to the first seven days of life. Studies that used the term “early-onset neonatal sepsis” but did not specify timing (i.e. seven days or three days) were also included. We also included studies that examined only high risk populations such as preterm labor, PROM, PPROM, and prolonged rupture of membranes. To assess for variations by region, we grouped studies by World Health Organization region, 2010 World Bank gross national income per capita in US dollars (low $1005 or less, lower-middle $1006-3975, upper-middle $3976-12 275, high income $12 276 or more), and 2009 UNICEF neonatal mortality rates (very low <5 deaths per 1000 live births, low 5-14 deaths/1000, high 15-27 deaths/1000, and very high more than 27 deaths/1000) [4-6].
Two independent reviewers assessed the methodological quality of included studies, examining selection methods, missing data, loss-to-follow-up, misclassification or measurement errors of exposures or outcomes, and confounding bias. Biases in selection and misclassification would have the largest effect on prevalence results. Studies were given an overall rating of low risk of bias if both selection and misclassification biases were at low risk. Studies that were high risk for either selection or misclassification bias or both were rated as high risk of bias. Studies that did not meet the low or high risk criteria were rated as having unclear risk of bias.
Statistical analysis
We used random-effects meta-analyses to calculate weighted mean estimates across studies and the 95% CI for the point prevalence of vertical transmission (Stata v12). If raw data were not available, we used the reported vertical transmission prevalence and calculated the standard error SE = √ [p(1 - p)/n]. If there were two or more studies included in the meta-analysis, we assessed measures of heterogeneity with I2 statistics. For each combination of maternal exposure and neonatal outcome, we calculated a pooled estimate of the prevalences. Because of the substantial heterogeneity across all combinations of maternal exposures and neonatal outcomes, we did not calculate an overall pooled estimate of the prevalences.
The studies we examined used numerous combinations of maternal exposure and neonatal outcome. This paper presents the following combinations:
-
i)
maternal lab confirmed infection and neonatal lab confirmed infection (lab/lab);
-
ii)
maternal lab confirmed infection and neonatal clinical signs of infection (lab/signs);
-
iii)
maternal lab confirmed infection and neonatal lab or clinical infection (lab/lab&signs);
-
iv)
maternal clinical signs of infection and neonatal lab confirmed infection (signs/lab);
-
v)
maternal clinical signs of infection and neonatal clinical signs of infection (signs/signs);
-
vi)
maternal clinical signs of infection and neonatal lab or clinical infection (signs/lab&signs);
-
vii)
maternal colonization and neonatal lab confirmed infection (colonization/lab);
-
viii)
maternal colonization and neonatal clinical signs of infection (colonization/signs);
-
ix)
maternal colonization and neonatal lab or clinical infection (colonization/lab&signs);
-
x)
maternal colonization and neonatal colonization (colonization/colonization);
-
xi)
maternal risk factor and neonatal lab confirmed infection (risk/lab);
-
xii)
maternal risk factor and neonatal clinical signs of infection (risk/signs).
The four forest plots presented in this paper estimate the vertical transmission point prevalence, 95% CI, and relative weights for four different groupings of these combinations: (i-vi) maternal infection and neonatal infection; (vii-ix) maternal colonization and neonatal infection; (x) maternal colonization and neonatal colonization; and (xi-xii) maternal risk factors and neonatal infections.
We originally planned for subgroup analyses by region, gross national income per capita in US dollars stratum, intrapartum antibiotic use, and neonatal mortality rate stratum. However, given the scarcity of data in the lower income and higher mortality rates countries, we were only able to describe the distribution of studies by region, income, and neonatal mortality rate. For the maternal colonization and neonatal colonization analysis, we examined pathogen-specific subgroups with Staphylococcus aureus, non-group B Streptococcus species, Group B streptococcus, Klebsiella pneumoniae, Escherichia coli, Ureaplasma species, Mycoplasma hominis, and multiple organisms. In our sensitivity analyses, we repeated meta-analyses excluding studies with (i) some or unknown intrapartum antibiotics use to understand the natural history of vertical transmission in settings of most LIC where intrapartum antibiotics are not available and (ii) high risk of bias. We planned these subgroup and sensitivity analyses a priori.
Role of the funding source
The funding source had no role in the study design, data collection, analysis, interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit the publication.
Results
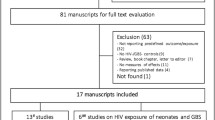
Our search identified 4436 articles of which 3486 were unique records. We reviewed 331 full-text articles. Eighteen authors were contacted regarding missing data and provided with a sample 2×2 table to complete. One [7] out of the four authors who responded provided usable data. Data from 122 studies met the inclusion criteria. Our qualitative analysis included all 122 studies; our quantitative meta-analysis included 107 of them (Figure 1, Additional file 2: Table S2). The majority of studies used cohort designs (n = 117, 95.9%) set in single health facilities (n = 94, 77.0%). In 75 studies (61.5%), researchers measured early-onset neonatal infection during the first seven days of life. Twenty-eight studies (23.0%) had data on women who did not use intrapartum antibiotics (either the study cohort did not use antibiotics, the study excluded women who received antibiotics, or data were abstracted from the placebo arm of an intervention trial); 51 studies (41.8%) reported some antibiotic use in a subset of women for prophylaxis or treatment; and 43 studies (35.2%) did not specify whether antibiotics were used. A sensitivity analysis around studies without or unknown use of antibiotics was limited by the data available and only possible in the subgroup maternal colonization and neonatal infection.
Thirty eight of the studies (31.1%) restricted their enrolment to a specific subset of women (preterm labor, PROM, PPROM, prolonged rupture), while a majority of studies (n = 80, 65.6%) examined all pregnant women. Four studies (3.3%) did not report the inclusion or exclusion criteria. Most studies (n = 101, 82.8%) occurred in the Americas or Europe, ten studies (8.2%) were in the western Pacific, five studies (4.1%) were in southeast Asia, three studies (2.5%) were in the eastern Mediterranean region, and three studies (2.5%) were in Africa. Most studies (n = 104, 85.2%) were in high income and low mortality settings (Table 1). Table 1 describes the number of studies and study characteristics in each meta-analysis. A study could report more than one maternal condition but was used only once in each meta-analysis (Additional file 3: Table S3, Additional file 4: Table S4).
Using available data from this pool of studies, we calculated the following median prevalence of exposures and outcomes: maternal lab-confirmed infection (17 studies, median prevalence 24.0%, interquartile range [IQR] 10.0-28.3), maternal clinical signs of infection (8 studies, median prevalence 11.6%, IQR 2.7-15.6), maternal colonization (60 studies, median prevalence 16.3%, IQR 7.9-23.5), neonatal lab-confirmed infection (37 studies, median prevalence 1.5%, IQR 0.1-7.1), neonatal clinical signs of infection (8 studies, median prevalence 11.3%, IQR 4.5-24.9), neonatal lab-confirmed or clinical signs of infection (8 studies, median prevalence 9.3%, IQR 6.0-16.8), and neonatal colonization (31 studies, median prevalence 7.3%, IQR 3.8-17.3). Ten studies defined maternal exposures or neonatal outcomes in categories that were too heterogeneous to place in a meta-analysis [8-17].
Regional
Available data on laboratory cultures, clinical signs, colonization status, and risk factors varied by region. The Americas, Europe and western Pacific regions had studies that examined maternal lab-confirmed, clinical signs, colonization, and risk factors. None of the studies in Africa, the eastern Mediterranean, and southeast Asia provided lab-confirmed maternal infection data, and no studies in Africa, the eastern Mediterranean, and the western Pacific provided clinical signs data. We were able to find studies in every region with maternal colonization data and with neonatal lab confirmed infection and colonization data, with the majority in the Americas and Europe. There were no studies of neonatal clinical infection from Africa or the eastern Mediterranean.
Risk of bias
Among the 122 included studies, 10 (8.2%) studies were rated overall as low risk; 57 (46.7%) were rated as unclear risk; and 55 (45.1%) were rated as high risk after considering selection and misclassification biases (Additional file 5: Figure S1). Eighteen (14.8%) studies had different eligibility criteria or baseline characteristics between the exposed and comparison groups. These studies were at high risk of selection bias. In assessing for misclassification bias, the majority of studies measured exposures or outcomes using reliable laboratory based culture methods. However, 24 (19.6%) studies determined the exposure from risk factors or clinical signs and 18 (14.7%) studies determined the outcome from clinical signs of sepsis.
Meta-analyses
The meta-analysis results are presented by exposure outcome combination: (i) maternal infection and neonatal infection; (ii) maternal colonization and neonatal infection; (iii) maternal colonization and neonatal colonization; and (iv) maternal risk factors and neonatal clinical infection. The study characteristics and exposure/outcome definitions for individual study data are shown in the Additional file 2: Table S2 and Additional file 3: Table S3.
Maternal infection and neonatal infection
Thirty-eight studies reported data on maternal infections and neonatal infections. We excluded five studies from the meta-analysis: three studies that measured maternal urinary tract infection exposure, which reported zero to two percent vertical transmission rates, and two population surveillance studies that looked at only at rare infections such as Listeria species and Bacteriodes species infections [11,18-21].
In studies where mothers had lab-confirmed infection, 17.2% (95% CI 6.5-27.9) of their newborns were infected (“lab/lab”) (Figure 2). Of the 11 studies reporting lab-confirmed maternal infection in the “lab/lab” meta-analysis, four (36.4%) examined amniotic fluid cultures, two (18.2%) used blood cultures, two studied blood and/or amniotic fluid cultures, two tested placental swab cultures, and one (9.1%) detected funisitis by histologic examination of the umbilical cord. A sensitivity analysis excluding high risk for bias studies produced a slightly increased prevalence of 19.5% (95% CI 2.3-36.8).
Similarly, in studies where mothers were diagnosed with clinical signs of infection, 20.1% (95% CI 8.1-32.1) of their newborns had lab confirmed infection (“signs/lab”). Of the ten studies reporting maternal clinical signs of infection in the “signs/lab” analysis, four (40.0%) examined intrapartum fever, two (20.0%) clinical chorioamnionitis, two (20.0%) intra-amnionitic infection, one (10.0%) intrapartum risk factors, and one (10.0%) nonspecific clinical infection.
In studies where mothers had lab-confirmed infection, 37.6% (95% CI 27.2-48.0) of their newborns had clinical signs of infection (“lab/signs”). In studies where mothers had lab-confirmed infection, 40.0% (95% CI 15.4-64.7) of their newborns had lab or clinical signs of infection (“lab/lab&signs”). Sufficient data were not available for the sensitivity analysis separating studies by antibiotic use.
Maternal colonization and neonatal infection
Thirty-seven studies reported data on maternal colonization and neonatal infections. One study, Craig et al, was excluded from the meta-analysis as an outlier, as it reported that 80% of newborns of colonized mothers were infected [30]. In studies that measured neonatal infection with lab tests (“colonization/lab”), the prevalence of neonatal infection among newborns of colonized mothers was 0% (95% CI 0.0-0.0) (24 studies, median 2.0%, IQR 0.3-4.6) and 0% (95% CI -0.1-0.1) (10 studies, median 9.6%, IQR 1.8-9.4) in studies that measured neonatal infection with clinical signs (“colonization/signs”). In studies that used lab tests and collected clinical signs of neonatal infection (“colonization/lab&signs”), 5.0% (95% CI 1.9-8.2) (7 studies, median 5.6%, IQR 1.8-9.4) of colonized mothers had newborns with infection (Figure 3). A sensitivity analysis excluding studies with known or possible antibiotic use showed a slight increase in prevalence of neonatal infections in studies that tested lab outcomes (1.1%, 95% CI 0.2-2.0), studies that diagnosed clinical signs of neonatal infection (6.5%, 95% CI -6.5-19.5), and studies that collected clinical signs of infection and conducted labs tests (7.6%, 95% CI 1.4-13.8).
Most studies focused on maternal Group B Streptococcus (GBS) colonization. We conducted meta-analyses by region of studies that tested maternal GBS colonization and that measured neonatal infection with lab tests (“colonization/lab”). In the Americas, 3.2% (95% CI 1.8-4.7) (10 studies, median 3.0%, IQR 1.6-4.5) of GBS colonized mothers had newborns with infection. In Europe, 0.2% (95% CI -0.1-0.4) (4 studies, median 0.4%, IQR 0.2-0.7) of GBS colonized mothers had newborns with infection. In western Pacific region, 0.0% (95% CI 0.0-0.0) (2 studies, median 0.0%, IQR 0.0-0.0) of GBS colonized mothers had newborns with infection. We did not have sufficient data to conduct a sensitivity analysis excluding studies with some or unknown antibiotic use.
Maternal colonization and neonatal colonization
Thirty-nine studies reported data on maternal colonization and neonatal colonization (“colonization/colonization”). We present these results by pathogen-specific subgroups. In thirty-one studies where mothers were colonized with GBS, 38.9% (95% CI 29.6-48.2) of the newborns had surface GBS colonization. In seven studies where mothers were colonized with Staphylococcus aureus, 39.5% (95% CI 16.1-63.0) of the newborns had surface S. aureus colonization. In three studies where mothers were colonized with Escherichia coli, 34.3% (95% CI 4.2-64.5) of the newborns had E. coli colonization. In three studies where mothers were colonized with Ureaplasma species, 45.5% (95% CI 26.4-64.5) of the newborns were colonized with Ureaplasma species. Two studies did not differentiate clearly between organisms. In these studies, 30.9% (95% CI 25.6-87.4) of the newborns were colonized (Figure 4).
Maternal risk factors and neonatal infection
Twenty-seven studies presented data on maternal risk factors and neonatal infections. All were included in the meta-analysis. In studies where mothers had prolonged rupture of membranes, 19.2% (95% CI 7.0-31.3) of the newborns had positive lab cultures for infection. In studies where mothers had PPROM, 8.5% (95% CI 2.9-14.1) of the newborns had positive lab cultures for infection. In studies where mothers had PROM or PPROM, 3.5% (95% CI -3.0-9.9) of newborns had positive lab cultures for infection. In studies where mothers had PROM, 3.1% (95% CI -2.2-8.4) of the newborns had positive lab cultures. In studies where mothers experienced preterm labor, 2.9% (95% CI 1.7-4.2) of the newborns had positive lab cultures (Figure 5).
The prevalence of neonatal infection was higher in studies that measured neonatal clinical signs of infection (“risk/signs”). In studies where mothers had preterm labor, 7.0% (95% CI 1.4-12.6) of the newborns had clinical signs of infection. In studies where mothers had PROM, 14.1% (95% CI 10.6-17.6) of the newborns had clinical signs of infection. In studies where mothers had PPROM, 32.1% (95% CI 3.7-60.6) of the newborns had clinical signs of infection. In studies where mothers had prolonged rupture of membranes, 18.6% (95% CI 0.4-36.7) of the newborns had clinical signs of infection (Figure 5). In studies that measured neonatal clinical signs or lab tests (“risk/lab&signs”), the prevalence of neonatal infection was even higher among newborns born to women with preterm labor (37.5%, 95% CI -3.1-78.2) or PROM (16.1%, 95% CI 1.3-31.0) although the 95% CIs overlapped with the studies that measured neonatal clinical signs only.
Discussion
We estimate a high prevalence of neonatal infection in the first seven days of life where mothers had genital tract infection or risk factors for infection. In studies of pregnant mothers with laboratory confirmed infection, 17% of their newborns had positive laboratory cultures for infection. Similarly, in studies of pregnant mothers with clinical signs of infection, 20% of newborns had positive lab cultures for infection.
We included studies that measured maternal colonization or risk factors for infection. After excluding studies with known or possible antibiotic use, 1-7% (depending on definition of infection) of newborns exposed to maternal colonization developed neonatal infections. Most studies in our review that assessed maternal colonization examined GBS. Our findings are consistent with a US based review showing 2.0% of newborns exposed to maternal GBS developed early-onset GBS neonatal sepsis [128,129]. The lower prevalence of GBS colonization among newborns exposed to maternal GBS colonization in Europe compared to the US may be related to regional differences in GBS strains or a sampling bias in the studies meeting our inclusion criteria. Approximately 30-45% of newborns were surface colonized if they were born to a colonized mother, suggesting a high rate of surface bacterial transmission via direct contact through the birth canal between the mother and newborn. Pregnant women with risk factors, particularly PPROM, preterm labor, and prolonged rupture of membranes, had a high prevalence of neonatal infection. These risk factors may lead to bacterial infections, and may be indications for women to present to a health facility. In settings where laboratory or clinical measures are not available, the presence of risk factors may be a useful target for interventions to prevent early-onset neonatal sepsis.
Studies with lab tests for neonatal infection provided a more conservative measure of prevalence than studies with clinical signs of neonatal infection. The true prevalence of neonatal infection is likely to be between the specific lab-confirmed measures and sensitive clinical signs measures. Studies with colonization measures were also dependent on laboratory facilities and these findings may not be generalizable to populations without such facilities. Not many studies utilized molecular diagnostic methods in our review. As PCR-based diagnoses of maternal and neonatal infections are becoming more widely used, our ability to detect true neonatal infections will improve.
More studies are needed to accurately estimate the prevalence of early-onset neonatal infection in cases where mothers are infected or colonized, especially in low-income countries. Among our included studies, there was no maternal infection data (lab confirmed or clinical signs) from Africa and the eastern Mediterranean. In southeast Asia, no studies looked at lab-confirmed maternal infection and only two studies reported clinical signs of infection.
Our review has several limitations. Most studies were assessed to be at high risk or unclear risk of bias, which introduced systematic differences in baseline characteristics, outcome measurements, and estimates of point prevalence. We conducted a sensitivity analysis to exclude high risk studies in order to provide less biased estimates.
Since all studies were facilities-based, mostly concentrated in urban settings in the Americas and Europe, we could not capture the prevalence of early-onset neonatal sepsis among home births, rural births, or births at community facilities in lower-income countries, thereby limiting the generalizability of these findings. Included studies tended to have high prevalence of maternal infections, suggesting that these studies may be more biased towards pregnant women with more severe disease or risk factors. Authors are more likely to report positive findings in international English journals, whereas negative findings are published in non-English journals. We excluded non-English articles due to our limited resources. To assess for publication bias, we used funnel plots of standard error and prevalence to graph the correlation between the variance and distribution of effect sizes. Results were not statistically significant (p = 0.10).
There were limited data available on intrapartum antibiotic use in these studies. The majority of studies had either some or unknown antibiotic use. The inclusion of pregnant mothers who had received antibiotics would lead a study to underestimate the vertical transmission rates that would occur without antibiotic intervention.
There was significant heterogeneity of the prevalence results included in the meta-analysis because of the different measures of exposures and outcomes (lab-confirmed, clinical signs, colonization, and risk factors). To minimize heterogeneity, we grouped studies by exposure and outcome definitions and conducted separate meta-analyses for each group, although this reduced the number of studies in each meta-analysis. To account for additional differences, we used a random-effects model. We did not provide an overall estimate of vertical transmission across all studies because we assessed the studies to be too heterogeneous.
A strength of our study was our comprehensive search strategy; we included all articles with a measure or raw data on maternal and neonatal infections or colonization. Our study is the first to synthesize different measures of infection and provide prevalence estimates of neonatal early-onset infection among newborns of women with infections, colonization, or risk factors. Our findings highlight the need for better screening and diagnostics to identify pregnant women with infections and/or colonization to better understand the population based prevalence of maternal infections and/or colonization with common EOS pathogens in LMIC, which if treated would have the potential to reduce the burden of early-onset neonatal infections. Additional studies, such as a randomized controlled trial on the effect of intrapartum antibiotic prophylaxis on early-onset neonatal sepsis in low resource settings, are also needed.
Conclusion
This study reinforces the importance of ongoing efforts in research and policy development to prevent early-onset neonatal sepsis by targeting pregnant women with infections (laboratory-confirmed, clinical signs), bacterial colonization, and risk factors. Standardizing definitions for maternal infections and newborns would be helpful to compare studies. High quality studies, with laboratory-confirmed, clinical signs, colonization, and risk factors are needed in low-resource areas, especially southeast Asia and Africa.
Abbreviations
- CI:
-
Confidence interval
- GBS:
-
Group B Streptococcus
- IQR:
-
Interquartile range
- PROM:
-
Premature rupture of membranes
- PPROM:
-
Preterm premature rupture of membranes
- ROM:
-
Rupture of membranes
- WHO:
-
World Health Organization
References
Baqui AH, Darmstadt GL, Williams EK, Kumar V, Kiran TU, Panwar D, et al. Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programmes. Bull World Health Organ. 2006;84(9):706–13.
Seale AC, Blencowe H, Manu AA, Nair H, Bahl R, Qazi SA, et al. Estimates of possible severe bacterial infection in neonates in sub-Saharan Africa, south Asia, and Latin America for 2012: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(8):731–41.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61.
GNI per capita, Atlas method. [http://data.worldbank.org/indicator/NY.GNP.PCAP.CD]
Global Burden of Disease Regions used for WHO-CHOICE Analyses. [http://www.who.int/choice/demography/regions/en/]
The State of the World's children 2005: Table 7. Economic Indicators.
Pylipow M, Gaddis M, Kinney JS. Selective intrapartum prophylaxis for group B streptococcus colonization: management and outcome of newborns. Pediatrics. 1994;93(4):631–5.
Frederiksen B, Samuelsson S. Feto-maternal listeriosis in Denmark 1981–1988. J Infect. 1992;24(3):277–87.
Kunze M, Zubler B, Muller C, Flecken U, Clad A. Evaluation of placental membrane swabs in the diagnosis of intrauterine infections. Geburtsh Frauenheilk. 2006;66(6):575–8.
McLauchlin J. Human listeriosis in Britain, 1967–85, a summary of 722 cases. 1. Listeriosis during pregnancy and in the newborn. Epidemiol Infect. 1990;104(2):181–9.
Persson K, Bjerre B, Elfstrom L, Polberger S, Forsgren A. Group B streptococci at delivery: high count in urine increases risk for neonatal colonization. Scand J Infect Dis. 1986;18(6):525–31.
Smith B, Kemp M, Ethelberg S, Schiellerup P, Bruun BG, Gerner-Smidt P, et al. Listeria monocytogenes: maternal-foetal infections in Denmark 1994–2005. Scand J Infect Dis. 2009;41(1):21–5.
Morales WJ, Angel JL, O'Brien WF, Knuppel RA. Use of ampicillin and corticosteroids in premature rupture of membranes: a randomized study. Obstet Gynecol. 1989;73(5 Pt 1):721–6.
Tuppurainen N, Hallman M. Prevention of neonatal group B streptococcal disease: intrapartum detection and chemoprophylaxis of heavily colonized parturients. Obstet Gynecol. 1989;73(4):583–7.
Carlan SJ, Richmond LB, O'Brien WF. Randomized trial of endovaginal ultrasound in preterm premature rupture of membranes. Obstet Gynecol. 1997;89(3):458–61.
Vergani P, Patane L, Colombo C, Borroni C, Giltri G, Ghidini A. Impact of different prevention strategies on neonatal group B streptococcal disease. Am J Perinatol. 2002;19(6):341–8.
Quentin R, Musser JM, Mellouet M, Sizaret PY, Selander RK, Goudeau A. Typing of urogenital, maternal, and neonatal isolates of Haemophilus influenzae and Haemophilus parainfluenzae in correlation with clinical source of isolation and evidence for a genital specificity of H. influenzae biotype IV. J Clin Microbiol. 1989;27(10):2286–94.
Elder HA, Santamarina BA, Smith S, Kass EH. The natural history of asymptomatic bacteriuria during pregnancy: the effect of tetracycline on the clinical course and the outcome of pregnancy. Am J Obstet Gynecol. 1971;111(3):441–62.
McGrady GA, Daling JR, Peterson DR. Maternal urinary tract infection and adverse fetal outcomes. Am J Epidemiol. 1985;121(3):377–81.
Nolla-Salas J, Bosch J, Gasser I, Vinas L, de Simon M, Almela M, et al. Perinatal listeriosis: a population-based multicenter study in Barcelona, Spain (1990–1996). Am J Perinatol. 1998;15(8):461–7.
Wood EG, Dillon Jr HC. A prospective study of group B streptococcal bacteriuria in pregnancy. Am J Obstet Gynecol. 1981;140(5):515–20.
Bobitt JR, Ledger WJ. Unrecognized amnionitis and prematurity: a preliminary report. J Reprod Med. 1977;19(1):8–12.
Pass MA, Gray BM, Dillon Jr HC. Puerperal and perinatal infections with group B streptococci. Am J Obstet Gynecol. 1982;143(2):147–52.
Wallace Jr RJ, Baker CJ, Quinones FJ, Hollis DG, Weaver RE, Wiss K. Nontypable Haemophilus influenzae (biotype 4) as a neonatal, maternal, and genital pathogen. Rev Infect Dis. 1983;5(1):123–36.
Feinstein SJ, Vintzileos AM, Lodeiro JG, Campbell WA, Weinbaum PJ, Nochimson DJ. Amniocentesis with premature rupture of membranes. Obstet Gynecol. 1986;68(2):147–52.
Gibbs RS, Dinsmoor MJ, Newton ER, Ramamurthy RS. A randomized trial of intrapartum versus immediate postpartum treatment of women with intra-amniotic infection. Obstet Gynecol. 1988;72(6):823–8.
Gauthier DW, Meyer WJ, Bieniarz A. Expectant management of premature rupture of membranes with amniotic fluid cultures positive for Ureaplasma urealyticum alone. Am J Obstet Gynecol. 1994;170(2):587–90.
Matsuda Y, Maruyama H, Kuraya K. Relationship between granulocyte elastase levels and perinatal infections. Gynecol Obstet Invest. 1995;39(3):162–6.
Averbuch B, Mazor M, Shoham-Vardi I, Chaim W, Vardi H, Horowitz S, et al. Intra-uterine infection in women with preterm premature rupture of membranes: maternal and neonatal characteristics. Eur J Obstet Gynecol Reprod Biol. 1995;62(1):25–9.
Craig S, Permezel M, Doyle L, Mildenhall L, Garland S. Perinatal infection with Listeria monocytogenes. Aust N Z J Obstet Gynaecol. 1996;36(3):286–90.
Yoon BH, Romero R, Park JS, Kim M, Oh SY, Kim CJ, et al. The relationship among inflammatory lesions of the umbilical cord (funisitis), umbilical cord plasma interleukin 6 concentration, amniotic fluid infection, and neonatal sepsis. Am J Obstet Gynecol. 2000;183(5):1124–9.
Goldenberg RLA WW, Goepfert AR, Faye-Petersen O, Cliver SP, Carlo WA, Hauth JC. The Alabama Preterm Birth Study: Umbilical cord blood Ureaplasma urealyticum and Mycoplasma hominis cultures in very preterm newborn infants. Am J Obstet Gynecol. 2008;198(1):43. e41-43.e45.
Coultrip LL, Lien JM, Gomez R, Kapernick P, Khoury A, Grossman JH. The value of amniotic fluid interleukin-6 determination in patients with preterm labor and intact membranes in the detection of microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 1994;171(4):901–11.
Kasper DC, Mechtler TP, Reischer GH, Witt A, Langgartner M, Pollak A, et al. The bacterial load of Ureaplasma parvum in amniotic fluid is correlated with an increased intrauterine inflammatory response. Diagn Microbiol Infect Dis. 2010;67(2):117–21.
Gibbs RS, Blanco JD. Streptococcal infections in pregnancy. A study of 48 bacteremias. Am J Obstet Gynecol. 1981;140(4):405–11.
Broekhuizen FF, Gilman M, Hamilton PR. Amniocentesis for gram stain and culture in preterm premature rupture of the membranes. Obstet Gynecol. 1985;66(3):316–21.
Dudley J, Malcolm G, Ellwood D. Amniocentesis in the management of preterm premature rupture of the membranes. Aust N Z J Obstet Gynaecol. 1991;31(4):331–6.
Puchner T, Egarter C, Wimmer C, Lederhilger F, Weichselbraun I. Amniotic-Fluid Interleukin-8 as a Marker for Intraamniotic Infection. Arch Gynecol Obstet. 1993;253(1):9–14.
de Araujo MC, Schultz R, Vaz FA, Massad E, Feferbaum R, Ramos JL. A case–control study of histological chorioamnionitis and neonatal infection. Early Hum Dev. 1994;40(1):51–8.
Papantoniou NE, Antsaklis AJ, Protopapas AG, Vogiatzi AI, Aravantinos DI. Predictive value of amniotic fluid and fetal blood cultures in pregnancy outcome in preterm prelabour rupture of membranes. J Obstet Gynaecol. 1997;17(1):18–22.
Wilson JC, Levy DL, Wilds PL. Premature rupture of membranes prior to term: consequences of nonintervention. Obstet Gynecol. 1982;60(5):601–6.
Philip AG. Neonatal sepsis resulting from possible amniotic fluid infection: risk and detection. Clin Pediatr (Phila). 1982;21(4):210–4.
Sperling RS, Ramamurthy RS, Gibbs RS. A comparison of intrapartum versus immediate postpartum treatment of intra-amniotic infection. Obstet Gynecol. 1987;70(6):861–5.
Newton ER, Prihoda TJ, Gibbs RS. Logistic regression analysis of risk factors for intra-amniotic infection. Obstet Gynecol. 1989;73(4):571–5.
Rosemond RL, Glass CA, Wingo CE. Daily Fetal Movement and Breathing Assessments in the Management of Preterm Membrane Rupture. J Matern-Fetal Inves. 1995;5(4):236–9.
Mitra S, Panigrahi D, Narang A. Anaerobes in neonatal septicaemia: a cause for concern. J Trop Pediatr. 1997;43(3):153–5.
Mercer BM, Carr TL, Beazley DD, Crouse DT, Sibai BM. Antibiotic use in pregnancy and drug-resistant infant sepsis. Am J Obstet Gynecol. 1999;181(4):816–21.
Dutta S, Reddy R, Sheikh S, Kalra J, Ray P, Narang A. Intrapartum antibiotics and risk factors for early onset sepsis. Arch Dis Child Fetal Neonatal Ed. 2010;95(2):F99–103.
Puopolo KM, Draper D, Wi S, Newman TB, Zupancic J, Lieberman E, et al. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics. 2011;128(5):e1155–1163.
Koh KS, Chan FH, Monfared AH, Ledger WJ, Paul RH. The changing perinatal and maternal outcome in chorioamnionitis. Obstet Gynecol. 1979;53(6):730–4.
Dollner H, Vatten L, Halgunset J, Rahimipoor S, Austgulen R. Histologic chorioamnionitis and umbilical serum levels of pro-inflammatory cytokines and cytokine inhibitors. BJOG. 2002;109(5):534–9.
Kordek A, Torbe A, Czajka R. Maternal venous procalcitonin levels do not correlate with umbilical cord blood and venous blood concentrations in the neonate. J Perinat Med. 2006;34(6):462–5.
Kordek A, Torbe A, Podraza W, Loniewska B, Jursa-Kulesza J, Rudnicki J. Does prenatal antibiotic therapy compromise the diagnosis of early-onset infection and management of the neonate? J Perinat Med. 2011;39(3):337–42.
Boyer KM, Gadzala CA, Kelly PC. Rapid identification of maternal colonization with group B streptococci by use of fluorescent antibody. J Clin Microbiol. 1981;14(5):550–6.
Christensen KK, Svenningsen N, Dahlander K, Ingemarsson E, Linden V, Christensen P. Relation between neonatal pneumonia and maternal carriage of group B streptococci. Scand J Infect Dis. 1982;14(4):261–6.
Morales WJ, Lim DV, Walsh AF. Prevention of neonatal group B streptococcal sepsis by the use of a rapid screening test and selective intrapartum chemoprophylaxis. Am J Obstet Gynecol. 1986;155(5):979–83.
Liang ST, Lau SP, Chan SH, Fok TF, Murai T, Kaneko Y. Perinatal colonization of group B streptococcus–an epidemiological study in a Chinese population. Aust N Z J Obstet Gynaecol. 1986;26(2):138–41.
Kishore K, Deorari AK, Singh M, Bhujwala RA. Early onset neonatal sepsis--vertical transmission from maternal genital tract. Indian Pediatr. 1987;24(1):45–8.
Simor AE, Ferro S. Campylobacter jejuni infection occurring during pregnancy. Eur J Clin Microbiol Infect Dis. 1990;9(2):142–4.
Towers CV, Garite TJ, Friedman WW, Pircon RA, Nageotte MP. Comparison of a rapid enzyme-linked immunosorbent assay test and the Gram stain for detection of group B streptococcus in high-risk antepartum patients. Am J Obstet Gynecol. 1990;163(3):965–7.
Matorras R, García-Perea A, Omeñaca F, Diez-Enciso M, Madero R, Usandizaga JA. Intrapartum chemoprophylaxis of early-onset group B streptococcal disease. Eur J Obstet Gynecol Reprod Biol. 1991;40(1):57–62.
Burman LG, Christensen P, Christensen K, Fryklund B, Helgesson AM, Svenningsen NW, et al. Prevention of excess neonatal morbidity associated with group B streptococci by vaginal chlorhexidine disinfection during labour. The Swedish Chlorhexidine Study Group. Lancet. 1992;40(8811):65–9.
Regan JA, Klebanoff MA, Nugent RP, Eschenbach DA, Blackwelder WC, Lou Y, et al. Colonization with group B streptococci in pregnancy and adverse outcome. VIP Study Group. Am J Obstet Gynecol. 1996;174(4):1354–60.
Sensini A, Tissi L, Verducci N, Orofino M, Von Hunolstein C, Brunelli B, et al. Carriage of group B streptococcus in pregnant women and newborns: A 2-year study at Perugia General Hospital. Clin Microbiol Infect. 1997;3(3):324–8.
Piper JM, Georgiou S, Xenakis EM, Langer O. Group B streptococcus infection rate unchanged by gestational diabetes. Obstet Gynecol. 1999;93(2):292–6.
Matsubara K, Katayama K, Baba K, Nigami H, Harigaya H, Sugiyama M. Seroepidemiologic studies of serotype VIII group B Streptococcus in Japan. J Infect Dis. 2002;186(6):855–8.
Orrett FA. Colonization with Group B streptococci in pregnancy and outcome of infected neonates in Trinidad. Pediatr Int. 2003;45(3):319–23.
Niduvaje K, Amutha C, Roy J. Early neonatal streptococcal infection. Indian J Pediatr. 2006;73(7):573–6.
Kalinka J, Krajewski P, Sobala W, Wasiela M, Brzezinska-Blaszczyk E. The association between maternal cervicovaginal proinflammatory cytokines concentrations during pregnancy and subsequent early-onset neonatal infection. J Perinat Med. 2006;34(5):371–7.
Namavar Jahromi B, Poorarian S, Poorbarfehee S. The prevalence and adverse effects of group B streptococcal colonization during pregnancy. Arch Iran Med. 2008;11(6):654–7.
Andrews WW, Schelonka R, Waites K, Stamm A, Cliver SP, Moser S. Genital tract methicillin-resistant Staphylococcus aureus: risk of vertical transmission in pregnant women. Obstet Gynecol. 2008;111(1):113–8.
Buckler B, Bell J, Sams R, Cagle W, Bell SA, Allen C, et al. Unnecessary workup of asymptomatic neonates in the era of group B streptococcus prophylaxis. Infect Dis Obstet Gynecol. 2010;2010:3.
Faro S, Brehm B, Smith F, Mouzoon M, Greisinger A, Wehmanen O, et al. Screening for group B streptococcus: a private hospital's experience. Infect Dis Obstet Gynecol. 2010;2010:4.
Ghanim N, Alchyib O, Morrish D, Tompkins D, Julliard K, Visconti E, et al. Maternal-neonatal outcome with Staphylococcus aureus rectovaginal colonization. J Reprod Med. 2011;56(9–10):421–4.
Hashavya S, Benenson S, Ergaz-Shaltiel Z, Bar-Oz B, Averbuch D, Eventov-Friedman S. The use of blood counts and blood cultures to screen neonates born to partially treated group B Streptococcus-carrier mothers for early-onset sepsis: is it justified? Pediatr Infect Dis J. 2011;30(10):840–3.
Reid TM. Emergence of group B streptococci in obstetric and perinatal infections. Br Med J. 1975;2(5970):533–5.
Bobitt JR, Damato JD, Sakakini Jr J. Perinatal complications in group B streptococcal carriers: a longitudinal study of prenatal patients. Am J Obstet Gynecol. 1985;151(6):711–7.
Morales WJ, Lim D. Reduction of group B streptococcal maternal and neonatal infections in preterm pregnancies with premature rupture of membranes through a rapid identification test. Am J Obstet Gynecol. 1987;157(1):13–6.
Syrogiannopoulos GA, Kapatais-Zoumbos K, Decavalas GO, Markantes CG, Katsarou VA, Beratis NG. Ureoplasma urealyticum colonization of full term infants: Perinatal acquisition and persistence during early infancy. Pediatr Infect Dis J. 1990;9(4):236–40.
Natale N, Bertuletti PA, Goglio A, Pasinetti G, Della Fiorentina F, Parea M, et al. Group B Streptococcus prevalence in pregnancy and maternal-fetal transmission: A multicenter study. Italian J Gynaecol Obstetr. 1995;7(3):124–30.
Itakura A, Kurauchi O, Morikawa S, Matsuzawa K, Mizutani S, Tomoda Y. A prospective study on the relationship between intrapartum maternal group-B streptococcal concentration and signs of infection in neonates. J Obstet Gynaecol Res. 1996;22(2):101–5.
Lim CT, Thong MK, Parasakthi N, Ngeow YF. Group B streptococcus: maternal carriage rate and early neonatal septicaemia. Ann Acad Med Singapore. 1997;26(4):421–5.
Muthusami A, Devi CS, Kanungo R, Shashikala, Srinivasan, Murmu UC, et al. Vaginal colonization as a risk factor for the development of neonatal sepsis. Biomedicine. 2007;27(4):186–8.
Mercer BM, Miodovnik M, Thurnau GR, Goldenberg RL, Das AF, Ramsey RD, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. JAMA. 1997;278(12):989–95.
AbeleHorn M, Peters J, GenzelBoroviczeny O, Wolff C, Zimmermann A, Gottschling M. Vaginal Ureaplasma urealyticum colonization: Influence on pregnancy outcome and neonatal morbidity. Infection. 1997;25(5):286–91.
Volumenie JL, Fernandez H, Vial M, Lebrun L, Frydman R. Neonatal group B streptococcal infection. Results of 33 months of universal maternal screening and antibioprophylaxis. Eur J Obstet Gynecol Reprod Biol. 2001;94(1):79–85.
Franciosi RA, Knostman JD, Zimmerman RA. Group B streptococcal neonatal and infant infections. J Pediatr. 1973;82(4):707–18.
Gerard P, Verghote-D'Hulst M, Bachy A, Duhaut G. Group B streptococcal colonization of pregnant women and their neonates. Epidemiological study and controlled trial of prophylactic treatment of the newborn. Acta Paediatr Scand. 1979;68(6):819–23.
Merenstein GB, Todd WA, Brown G, Yost CC, Luzier T. Group B beta-hemolytic streptococcus: randomized controlled treatment study at term. Obstet Gynecol. 1980;55:315–8.
Weintraub Z, Regev R, Iancu TC, Ferne M, Rabinowitz BS. Perinatal group B streptococcal infections in Israel. Isr J Med Sci. 1983;19(10):900–2.
Visconti A, Orefici G, Notarnicola AM. Colonization and infection of mothers and neonates with group B streptococci in three Italian hospitals. J Hosp Infect. 1985;6(3):265–76.
Easmon CS, Hastings MJ, Neill J, Bloxham B, Rivers RP. Is group B streptococcal screening during pregnancy justified? Br J Obstet Gynaecol. 1985;92(3):197–201.
Kollee LA, Speyer I, van Kuijck MA, Koopman R, Dony JM, Bakker JH, et al. Prevention of group B streptococci transmission during delivery by vaginal application of chlorhexidine gel. Eur J Obstet Gynecol Reprod Biol. 1989;31(1):47–51.
Hervas JA, Gonzalez L, Gil J, Paoletti LC, Madoff LC, Benedi VJ. Neonatal group B streptococcal infection in Mallorca, Spain. Clin Infect Dis. 1993;16(5):714–8.
Ayata A, Guvenc H, Felek S, Aygun AD, Kocabay K, Bektas S. Maternal Carriage and Neonatal Colonization of Group-B Streptococci in Labor Are Uncommon in Turkey. Paediatr Perinat Ep. 1994;8(2):188–92.
Suara RO, Adegbola RA, Baker CJ, Secka O, Mulholland EK, Greenwood BM. Carriage of Group-B Streptococci in Pregnant Gambian Mothers and Their Infants. J Infect Dis. 1994;170(5):1316–9.
Saez-Llorens X, Ah-Chu MS, Castano E, Cortes L, Torres A, Suarez M, et al. Intrapartum prophylaxis with ceftriaxone decreases rates of bacterial colonization and early-onset infection in newborns. Clin Infect Dis. 1995;21(4):876–80.
Adriaanse AH, Kollee LA, Muytjens HL, Nijhuis JG, de Haan AF, Eskes TK. Randomized study of vaginal chlorhexidine disinfection during labor to prevent vertical transmission of group B streptococci. Eur J Obstet Gynecol Reprod Biol. 1995;61(2):135–41.
Hickman ME, Rench MA, Ferrieri P, Baker CJ. Changing epidemiology of group B streptococcal colonization. Pediatrics. 1999;104(2 Pt 1):203–9.
El-Kersh TA, Al-Nuaim LA, Kharfy TA, Al-Shammary FJ, Al-Saleh SS, Al-Zamel FA. Detection of genital colonization of group B streptococci during late pregnancy. Saudi Med J. 2002;23(1):56–61.
Tsolia M, Psoma M, Gavrili S, Petrochilou V, Michalas S, Legakis N, et al. Group B streptococcus colonization of Greek pregnant women and neonates: prevalence, risk factors and serotypes. Clin Microbiol Infect. 2003;9(8):832–8.
Eren A, Kucukercan M, Oguzoglu N, Unal N, Karateke A. The carriage of group B streptococci in Turkish pregnant women and its transmission rate in newborns and serotype distribution. Turk J Pediatr. 2005;47(1):28–33.
Kadanali A, Altoparlak U, Kadanali S. Maternal carriage and neonatal colonisation of group B streptococcus in eastern Turkey: Prevalence, risk factors and antimicrobial resistance. Int J Clin Pract. 2005;59(4):437–40.
Lijoi D, Di Capua E, Ferrero S, Mistrangelo E, Giannattasio A, Morano S, et al. The efficacy of 2002 CDC guidelines in preventing perinatal group B Streptococcal vertical transmission: a prospective study. Arch Gynecol Obstet. 2007;275(5):373–9.
Elzbieta K, Joanna SM, Janusz W, Edyta B, Tomasz K, Anna K, et al. The incidence of Streptococcus Group B in 100 parturient women and the transmission of pathogens to the newborn. Ginekol Pol. 2009;80(4):285–9.
Cutland CL, Madhi SA, Zell ER, Kuwanda L, Laque M, Groome M, et al. Chlorhexidine maternal-vaginal and neonate body wipes in sepsis and vertical transmission of pathogenic bacteria in South Africa: a randomised, controlled trial. Lancet. 2009;374(9705):1909–16.
Seoud M, Nassar AH, Zalloua P, Boghossian N, Ezeddine J, Fakhoury H, et al. Prenatal and neonatal Group B Streptococcus screening and serotyping in Lebanon: incidence and implications. Acta Obstet Gynecol Scand. 2010;89(3):399–403.
Kunze M, Ziegler A, Fluegge K, Hentschel R, Proempeler H, Berner R. Colonization, serotypes and transmission rates of group B streptococci in pregnant women and their infants born at a single University Center in Germany. J Perinat Med. 2011;39(4):417–22.
Berardi A, Rossi C, Biasini A, Minniti S, Venturelli C, Ferrari F, et al. Efficacy of intrapartum chemoprophylaxis less than 4 hours duration. J Matern Fetal Neonatal Med. 2011;24(4):619–25.
Ayengar V, Madhulika, Vani SN. Neonatal sepsis due to vertical transmission from maternal genital tract. Indian J Pediatr. 1991;58(5):661–4.
Mitsuda T, Arai K, Fujita S, Yokota S. Demonstration of mother-to-infant transmission of Staphylococcus aureus by pulsed-field gel electrophoresis. Eur J Pediatr. 1996;155(3):194–9.
Pinter DM, Mandel J, Hulten KG, Minkoff H, Tosi MF. Maternal-infant perinatal transmission of methicillin-resistant and methicillin-sensitive Staphylococcus aureus. Am J Perinatol. 2009;26(2):145–51.
Bourgeois-Nicolaos N, Lucet JC, Daubie C, Benchaba F, Rajguru M, Ruimy R, et al. Maternal vaginal colonisation by Staphylococcus aureus and newborn acquisition at delivery. Paediatr Perinat Epidemiol. 2010;24(5):488–91.
Kafetzis DA, Skevaki CL, Skouteri V, Gavrili S, Peppa K, Kostalos C, et al. Maternal genital colonization with Ureaplasma urealyticum promotes preterm delivery: association of the respiratory colonization of premature infants with chronic lung disease and increased mortality. Clin Infect Dis. 2004;39(8):1113–22.
Gilbert RE, Pike K, Kenyon SL, Tarnow-Mordi W, Taylor DJ. The effect of prepartum antibiotics on the type of neonatal bacteraemia: insights from the MRC ORACLE trials. BJOG. 2005;112(6):830–2.
Kappy KA, Cetrulo CL, Knuppel RA, Ingardia CJ, Sbarra AJ, Scerbo JC, et al. Premature rupture of the membranes: a conservative approach. Am J Obstet Gynecol. 1979;134(6):655–61.
Varner MW, Galask RP. Conservative management of premature rupture of the membrane. Am J Obstet Gynecol. 1981;140(1):39–45.
Spinnato JA, Shaver DC, Bray EM, Lipshitz J. Preterm premature rupture of the membranes with fetal pulmonary maturity present: a prospective study. Obstet Gynecol. 1987;69(2):196–201.
Christmas JT, Cox SM, Andrews W, Dax J, Leveno KJ, Gilstrap LC. Expectant management of preterm ruptured membranes: effects of antimicrobial therapy. Obstet Gynecol. 1992;80(5):759–62.
Höckel M, Queisser-Luft A, Beck T, Zielberg R, Stopfkuchen H, Lissner R. The effect of antenatal intravenous immunoglobulin on ascending intrauterine infection after preterm premature rupture of the membranes: a pilot study. J Perinat Med. 1992;20:101–10.
Canpolat FE, Yigit S, Korkmaz A, Yurdakok M, Tekinalp G. Procalcitonin versus CRP as an early indicator of fetal infection in preterm premature rupture of membranes. Turkish J Pediatr. 2011;53(2):180–6.
Tafari N, Ljungh-Wadstrom A. Consequences of amniotic fluid infections: early neonatal septicaemia. Ciba Found Symp. 1979;77:55–67.
McCaul JF, Perry Jr KG, Moore Jr JL, Martin RW, Bucovaz ET, Morrison JC. Adjunctive antibiotic treatment of women with preterm rupture of membranes or preterm labor. Int J Gynaecol Obstet. 1992;38(1):19–24.
Nadisauskiene R, Bergstrom S. Impact of intrapartum intravenous ampicillin on pregnancy outcome in women with preterm labor: a randomised, placebo-controlled study. Gynecol Obstet Invest. 1996;41(2):85–8.
Blott M, Greenough A. Neonatal outcome after prolonged rupture of the membranes starting in the second trimester. Arch Dis Child. 1988;63(10 Spec No):1146–50.
Cararach V, Botet F, Sentis J, Almirall R, Perez-Picanol E. Administration of antibiotics to patients with rupture of membranes at term: a prospective, randomized, multicentric study. Collaborative Group on PROM. Acta Obstet Gynecol Scand. 1998;77(3):298–302.
Graham RL, Gilstrap 3rd LC, Hauth JC, Kodack-Garza S, Conaster DG. Conservative management of patients with premature rupture of fetal membranes. Obstet Gynecol. 1982;59(5):607–10.
Benitz WE, Gould JB, Druzin ML. Risk factors for early-onset group B streptococcal sepsis: estimation of odds ratios by critical literature review. Pediatrics. 1999;103(6):e77.
Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, et al. Group B streptococcal disease in the era of intrapartum antibiotic prophylaxis. N Engl J Med. 2000;342(1):15–20.
Acknowledgements
We thank Swaroop Vedula, Kristina Lindsley, and Kay Dickersin at the Center for Clinical Trials at Johns Hopkins University for their systematic reviews and meta-analysis expertise. Jennifer Robinson, Vivek Charu, and Ann Tukpah devoted much time and effort in reviewing and abstracting data. We thank Kate Lobner for her support in developing and running the search strategy. We appreciate the mothers and newborns who participated in these studies to better understand the causes and modes of transmission of early-onset neonatal sepsis. This work was carried out when Grace Chan was at Johns Hopkins Bloomberg School of Public Health.
Funding
This work was supported by Grant Number 5KL2RR025006 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declared that they have no competing interests.
Authors’ contributions
GC conceptualized the study, abstracted and analyzed the data, and wrote the first draft of the manuscript. AL critically reviewed the study design, search strategy, analysis, and edited the manuscript. JT abstracted data, analyzed the risk of bias, and created the tables and figures. AB and RB provided technical support and edited the paper. All authors reviewed and approved the final manuscript as submitted.
Additional files
Additional file 1: Table S1.
Search terms by database.
Additional file 2: Table S2.
Studies included in systematic review and meta-analysis.
Additional file 3: Table S3.
Studies included in systematic review and meta-analysis: Maternal exposure and neonatal outcome combinations.
Additional file 4: Table S4.
Maternal exposure and neonatal outcome definitions and prevalences.
Additional file 5: Figure S1.
Risk of bias summary.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chan, G.J., Lee, A.C., Baqui, A.H. et al. Prevalence of early-onset neonatal infection among newborns of mothers with bacterial infection or colonization: a systematic review and meta-analysis. BMC Infect Dis 15, 118 (2015). https://doi.org/10.1186/s12879-015-0813-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-015-0813-3