Abstract
Background
Our aim was to compare the 12-month incidence and clearance of oral high-risk HPV infection between HIV-infected men who have sex with men (MSM) and HIV-negative MSM.
Methods
MSM aged 18 years or older were recruited in Amsterdam, the Netherlands. Questionnaire data and oral-rinse and gargle samples were collected at baseline, and after 6 and 12 months. HPV DNA was genotyped using the SPF10-PCR & DEIA-LiPA25 system (version 1). Determinants of oral HPV incidence and clearance were explored using Cox and logistic regression analyses respectively.
Results
433 HIV-negative and 290 HIV-infected MSM were included in these analyses. The median follow-up time per participant was 12 months (range 3–15). During follow-up, 114 incident oral high-risk HPV infections were observed. The incidence rate of HPV-16 was 3.5/1000 person-months (PM) in HIV-infected and 0.9/1000 PM in HIV-negative MSM (IRR 4.1; 95% CI 1.3-13.2). The incidence rates of other high-risk HPV types ranged between 1.3-3.5/1000 PM in HIV-infected and 0.0-1.1/1000 PM in HIV-negative MSM. In multivariable analyses, HIV infection (adjusted hazard ratio [aHR] 3.8; 95% CI 2.3-6.2) and a higher number of recent oral sex partners (aHR 2.4 for ≥8 partners compared to ≤2; 95% CI 1.4-4.2) were associated with HPV incidence. Of the 111 baseline oral high-risk infections, 59 (53.2%) were cleared. In multivariable analyses, only a higher number of recent oral sex partners was associated with HPV clearance (adjusted odds ratio 3.4 for ≥8 compared to ≤2 partners; 95% CI 1.3-9.0).
Conclusions
The incidence rate of oral high-risk HPV infection was higher in HIV-infected MSM and in those with a higher number of recent oral sex partners. Just over half of the oral high-risk HPV infections at baseline were cleared after 12 months, with a higher likelihood of clearance among MSM reporting higher numbers of recent oral sex partners, but no difference by HIV status.
Similar content being viewed by others
Background
Human Papillomavirus (HPV), in particular oral infection with high-risk HPV type 16, has recently been recognized as a main etiologic agent for a subset of head and neck cancers [1]. Although the prevalence of oral high-risk HPV infection is relatively low among the general population, with estimates around 3.5% [2], a much higher prevalence of up to 25% has been reported among HIV-infected men who have sex with men (MSM) [3],[4].
The natural history of oral HPV infection is not yet well understood. Previous studies suggest that the incidence rate of oral HPV infection is lower than that of anal and genital HPV infections [5]-[7], whereas the clearance rate seems similar or higher compared to genital and anal HPV infection [5],[6],[8]. Oral sex is thought to be the most important risk factor of prevalent oral HPV infection, but also male gender, increasing age, a higher number of recent or lifetime partners, current smoking and HIV-infection have often been associated with oral HPV infection [3],[4],[9],[10]. Factors that have been associated with incident and persistent infections differ across studies. Recent data suggest that older age and current smoking could be stronger risk factors for oral HPV persistence than the acquisition [5],[8].
Data reported on the incidence and clearance rates of oral high-risk HPV among (HIV-infected) MSM are scarce, especially those describing the effect of HIV-infection [7],[11],[12]. As HIV-infected MSM are at increased risk of HPV infection and HPV-related head and neck cancer [13],[14], our aim was to compare the 12-month incidence and clearance of oral high-risk HPV infection between HIV-infected and HIV-negative MSM participating in the HIV & HPV in MSM (H2M) cohort in Amsterdam, the Netherlands. In addition, we aimed to assess determinants for oral high-risk HPV incidence and clearance.
In an earlier paper regarding the H2M cohort, we reported 6-month incidence and clearance data of oral HPV infections [15], but we were not able to estimate incidence rates because of limited follow-up time. In the current report covering a longer follow-up period with three measurements per participant, we were able to estimate incidence rates of individual high-risk HPV types, and to assess the effect of HIV infection on time to infection. We also studied clearance using a more rigorous definition (requiring two negative sample results after a positive baseline result rather than just one) than was possible in our earlier paper.
Methods
Ethics statement
The Medical Ethics Committee of the Academic Medical Center (AMC) Amsterdam approved this study, and all participants provided written informed consent prior to participation.
Study participants and sample collection
The H2M study design and sample collection methods have been described previously [4],[15]. In brief, HIV-negative and HIV-infected MSM aged 18 years or older were recruited for a prospective cohort study in 2010–2011 in Amsterdam. Data were collected at baseline, and after 6 and 12 months follow-up. At each visit, participants provided oral samples by rinsing and gargling for 30 seconds using 10–15 ml Scope mouthwash (Procter & Gamble, Toronto, Ontario), and completed detailed risk-factor questionnaires. HIV-related data at baseline were obtained from the Dutch HIV Monitoring Foundation’s national HIV patient database.
HPV DNA genotyping and classification
Processing of the oral samples and HPV DNA genotyping methods have been described before [4]. DNA extraction was performed using the MagNA Pure LC Total Nucleic Acid Isolation Kit (Roche, Mannheim, Germany), and subsequently HPV DNA amplification was performed using the highly sensitive SPF10-PCR DEIA/LiPA25 system (version 1) [16]. LiPA25 allows simultaneous identification of 25 specific mucosal HPV genotypes, of which the following were classified as high-risk types: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59 [1].
Statistical analyses
Since participants could have been infected with or be at risk for more than one high-risk HPV type, the main outcomes of interest were time to incidence of oral type-specific high-risk HPV infections, and clearance of type-specific HPV infections. An incident HPV infection was defined as a type-specific positive test result at 6 or 12 months follow-up in a participant who was free of that specific HPV type at baseline. For incidence analyses, we assumed that a new infection occurred at the midpoint between the date of the first detection and the date of the prior negative test result. Incidence rate ratios (IRR) were calculated using Poisson regression. Kaplan-Meier curves were constructed to explore the cumulative probability of type-specific HPV incidence; log-rank tests were used to compare HIV-infected and HIV-negative MSM. We assessed the independent effect of HIV infection on time to incident oral high-risk HPV infection using the Wei-Lin-Weissfeld method, which is basically a Cox model stratified by HPV type, to account for multiple HPV infections per person, while adjusting for within-subject correlations [17]. We also explored determinants associated with incident oral high-risk HPV infection stratified by HIV-status using the Wei-Lin-Weissfeld method. Multivariable analyses could not be performed for HIV-negative MSM due to low numbers of incident infections.
Among participants who tested positive at baseline, type-specific clearance of oral high-risk HPV infections was explored. Clearance was defined as a participant testing negative at two consecutive visits after a prevalent infection at baseline. Persistence was defined as a participant testing positive at two consecutive visits after a prevalent infection at baseline. Participants with a missing visit were excluded from these analyses. To assess the independent effect of HIV infection on clearance, logistic regression analyses were performed, with generalized estimating equations (GEEs) to account for multiple HPV infections per person, assuming an exchangeable correlation structure [9]. Because of low numbers of oral HPV infections at baseline, determinants associated with clearance could not be examined stratified by HIV status.
For both incidence and clearance analyses, variables that were biologically plausible as well as known determinants from the literature were included a priori in the multivariable models. P-values were considered statistically significant at P < 0.05. All analyses were performed using Stata (version 13.0; Stata Corp, College Station, Texas, USA).
Results
Study participants
Of the 795 participants that were enrolled in the H2M study (previously described [18]), 723 were included in the current analyses. Participants for whom data collection was incomplete (i.e., no HPV test results and/or no questionnaire data, n = 72) were excluded. The 72 excluded participants were younger than the 723 included participants (rank-sum P = 0.046), but comparable with respect to HIV status. At baseline, the median age was 38 (IQR 34–42) years among 433 HIV-negative MSM and 47 (IQR 40–53) years among 290 HIV-infected MSM (P < 0.001). HIV-infected MSM generally showed higher sexual risk behavior, e.g., the median number of lifetime male sex partners was 300 (IQR 100–1000) for HIV-infected MSM versus 100 (IQR 50–400) for HIV-negative MSM (P < 0.001). The median follow-up time was 370 days for HIV-negative MSM (IQR 356–384) and 350 days for HIV-infected MSM (IQR 314–373; P < 0.001). Among HIV-infected MSM, the median CD4+ cell count was 530 cells/mm3 (IQR 410–694), the median nadir CD4+ cell count was 220 cells/mm3 (IQR 170–320), and 79% (192/243) had an undetectable HIV viral load at baseline.
Oral high-risk HPV incidence
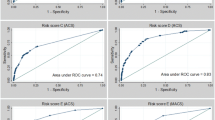
In total, 114 incident oral high-risk HPV infections were detected. For each HPV type, the incidence rate was higher in HIV-infected than in HIV-negative MSM (Table 1). For HPV-16, the incidence rate was 3.5/1000 person months (PM) in HIV-infected MSM versus 0.9/1000 PM in HIV-negative MSM, with an IRR of 4.1 (95% confidence interval (CI) 1.3-13.2). The incidence rate of HPV-18 was 2.8/1000 PM and 0.4/1000 PM in HIV-infected and HIV-negative MSM respectively (IRR 6.6; 95% CI 1.4-30.8). The 12-month cumulative incidence of HPV-16 was 4.0% in HIV-infected MSM and 1.0% in HIV-negative MSM; for HPV-18 this was 3.0% in HIV-infected MSM and 0.5% in HIV-negative MSM (Figure 1).
In multivariable analyses, incident oral high-risk HPV infection was significantly associated with HIV infection (adjusted hazard ratio (aHR) 3.8, 95% CI 2.3-6.2) and with a higher number of recent oral sex partners among MSM overall (aHR 2.4; 95% CI 1.4-4.2 for ≥8 compared to ≤2 partners). Among HIV-infected MSM only, a higher number of recent oral sex partners and both recent tobacco smoking and cannabis use were associated with incident oral high-risk HPV infection in multivariable analyses (Table 2). Oral-anal contact in the previous six months was significantly associated with incident oral high-risk HPV infection in univariable analysis, but was not associated in multivariable analyses. We did not find an association of incident oral high-risk HPV infection with age nor with nadir CD4+ cell count (Table 2).
Oral high-risk HPV clearance
At baseline, 111 oral high-risk HPV infections were observed, of which 59 (53.2%) were cleared, 25 (22.5%) persisted, and 27 (24.3%) showed other patterns (Table 3). After 12 months, 38.5% (n = 5/13) and 55.6% (n = 5/9) of the oral HPV-16 infections were cleared in HIV-infected MSM and HIV-negative MSM respectively.
HIV status was borderline significantly associated with clearance of HPV infection in univariable analysis, but was not associated in multivariable analyses (aOR 0.5; 95% CI 0.2-1.3; Table 4). In multivariable analyses, a higher number of recent oral sex partners was significantly and positively associated with clearance of high-risk HPV infection (adjusted odds ratio (aOR) 3.4; 95% CI 1.3-9.0 for ≥8 compared to ≤2 partners). Neither age nor tobacco smoking were associated with oral high-risk HPV clearance in uni- and multivariable analyses.
Discussion
In our cohort of HIV-negative and HIV-infected MSM, we found that HIV infection was an independent determinant for oral high-risk HPV incidence, and that around half of the oral HPV infections were cleared within 12 months.
The type-specific incidence rates among HIV-negative MSM (e.g. HPV-16: 0.9/1000 PM) were generally comparable to or somewhat higher than incidence rates reported in a large multinational study among HIV-negative, mainly heterosexual men (HPV-16: 0.8/1000 PM) [5], but the incidence rates among HIV-infected MSM in our study were substantially higher (HPV-16: 3.5/1000 PM). This indicates that HIV infection may be an important determinant for oral HPV incidence. This was even the case after adjustment for age, smoking, oral-anal contact and the number of recent oral sex partners. A higher number of recent oral sex partners was also significantly associated with oral HPV incidence, which is in line with previous reports suggesting that oral sexual behavior may be a risk factor for both oral HPV prevalence [3],[9] and HPV-related head and neck cancer [19].
Although oral high-risk HPV clearance was generally lower among HIV-infected MSM, HIV infection was not a significant determinant for clearance in multivariable analyses. Strikingly, a higher number of recent oral sex partners was significantly associated with increased oral HPV clearance. We hypothesize that newly acquired HPV infections (which may be more common among participants with more recent oral sex partners) are more likely to clear within one year, as compared to long-standing persistent infections [6]. This finding could also be explained by the fact that our method of HPV detection was based on the detection of HPV DNA which is not necessarily indicative of an active infection. Therefore, the higher clearance rate in those with a higher number of recent oral sex partners might be because part of the oral HPV in this group could be detections rather than actual active infections.
The current study builds on data previously published, in which the 6-month oral high-risk HPV incidence and persistence were analyzed within the same cohort [15]. Most determinants identified in this report were comparable to those in our earlier report, notably the association between HIV infection and oral HPV incidence. However, in the earlier report an increasing number of recent oral sex partners was borderline significantly associated with oral high-risk HPV incidence in multivariable analyses, while in this report it was a strong and independent determinant. Moreover, while in our previous report no determinants for clearance were identified, we now observed an independent association with the number of recent oral sex partners. Although the study population, sampling and laboratory methods, and research questions were largely the same, the current study adds important information: 1) the follow-up time was doubled, which increased the power of the study and enabled us to assess incidence rates, which facilitates comparisons across studies, and 2) we used a stricter definition of clearance (requiring two negative samples after a positive sample).
This study has some limitations. First, despite the increased follow-up time, the current study still had limited power, especially in the analyses of HPV clearance in HIV-negative MSM. Second, it has been reported that oral HPV genotypes might be missed with a single oral rinse sample and, that this sampling technique could be improved by prior epithelial abrasion or by using multiple sampling methods [20],[21]. Although this potential error could have impact on the accuracy of the incidence and clearance rates, it would not have affected the difference in the incidence or clearance rates between risk groups because the error would be similar for each group. Finally, our analysis of clearance was based on prevalent oral infections: the duration of the infection before enrollment was unknown. Long-term follow-up studies are needed to further assess the natural history or oral HPV infection. Future research could also investigate the role of oral health in acquisition and persistence of oral high-risk HPV infections as recent studies indicated that poor oral health is an independent risk factor for oral HPV infection [22],[23].
Conclusions
In conclusion, oral high-risk HPV incidence was independently associated with HIV infection and a higher number of recent oral sex partners, while just over half of the prevalent infections were cleared within 12 months. As the incidence of HPV-related head and neck cancer is increasing in many parts of the world [24]-[26], better understanding of the natural history of oral HPV infection is essential for prevention of these HPV-related cancers, especially among high-risk groups such as HIV-infected MSM.
Abbreviations
- HPV:
-
Human Papillomavirus
- MSM:
-
Men who have sex with men
- H2M:
-
HIV & HPV in MSM
- IRR:
-
Incidence rate ratio
- GEEs:
-
Generalized estimating equations
- IQR:
-
Interquartile range
- PM:
-
Person months
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- aHR:
-
Adjusted hazard ratio
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
References
Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V: A review of human carcinogens–Part B: biological agents. Lancet Oncol. 2009, 10 (4): 321-322. 10.1016/S1470-2045(09)70096-8.
Kreimer AR, Bhatia RK, Messeguer AL, Gonzalez P, Herrero R, Giuliano AR: Oral human papillomavirus in healthy individuals: a systematic review of the literature. Sex Transm Dis. 2010, 37 (6): 386-391.
Beachler DC, Weber KM, Margolick JB, Strickler HD, Cranston RD, Burk RD, Wiley DJ, Minkoff H, Reddy S, Stammer EE, Gillison ML, D’Souza G: Risk factors for oral HPV infection among a high prevalence population of HIV-positive and at-risk HIV-negative adults. Cancer Epidemiol Biomarkers Prev. 2012, 21 (1): 122-133. 10.1158/1055-9965.EPI-11-0734.
Mooij SH, Boot HJ, Speksnijder AG, Stolte IG, Meijer CJ, Snijders PJ, Verhagen DW, King AJ, de Vries HJ, Quint WG, van der Sande MA, Schim van der Loeff MF: Oral human papillomavirus infection in HIV-negative and HIV-infected MSM. Aids. 2013, 27 (13): 2117-2128. 10.1097/QAD.0b013e328362395c.
Kreimer AR, Pierce Campbell CM, Lin HY, Fulp W, Papenfuss MR, Abrahamsen M, Hildesheim A, Villa LL, Salmeron JJ, Lazcano-Ponce E, Giuliano AR: Incidence and clearance of oral human papillomavirus infection in men: the HIM cohort study. Lancet. 2013, 382 (9895): 877-887. 10.1016/S0140-6736(13)60809-0.
Beachler DC, D’Souza G, Sugar EA, Xiao W, Gillison ML: Natural history of anal vs oral HPV infection in HIV-infected men and women. J Infect Dis. 2013, 208 (2): 330-339. 10.1093/infdis/jit170.
Videla S, Darwich L, Canadas MP, Coll J, Pinol M, Garcia-Cuyas F, Molina-Lopez RA, Cobarsi P, Clotet B, Sirera G: Natural history of human papillomavirus infections involving anal, penile, and oral sites among HIV-positive men. Sex Transm Dis. 2013, 40 (1): 3-10. 10.1097/OLQ.0b013e31827e87bd.
Edelstein ZR, Schwartz SM, Hawes S, Hughes JP, Feng Q, Stern ME, O’Reilly S, Lee SK, Fu Xi L, Koutsky LA: Rates and determinants of oral human papillomavirus infection in young men. Sex Transm Dis. 2012, 39 (11): 860-867. 10.1097/OLQ.0b013e318269d098.
D’Souza G, Agrawal Y, Halpern J, Bodison S, Gillison ML: Oral sexual behaviors associated with prevalent oral human papillomavirus infection. J Infect Dis. 2009, 199 (9): 1263-1269. 10.1086/597755.
Gillison ML, Broutian T, Pickard RK, Tong ZY, Xiao W, Kahle L, Graubard BI, Chaturvedi AK: Prevalence of oral HPV infection in the United States, 2009–2010. Jama. 2012, 307 (7): 693-703. 10.1001/jama.2012.101.
Ong JJ, Read TR, Vodstrcil LA, Walker S, Chen M, Bradshaw CS, Garland SM, Tabrizi SN, Cornall A, Grulich A, Hocking J, Fairley CK: Detection of oral human papillomavirus in HIV-positive men who have sex with men 3 years after baseline: a follow up cross-sectional study. PLoS One. 2014, 9 (7): e102138-10.1371/journal.pone.0102138.
Darwich L, Canadas MP, Videla S, Coll J, Molina-Lopez RA, Cobarsi P, Sirera G, Clotet B: Oral human papillomavirus type-specific infection in HIV-infected men: a prospective cohort study among men who have sex with men and heterosexual men. Clin Microbiol Infect. 2014, 20 (9): O585-O589. 10.1111/1469-0691.12523.
Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM: Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet. 2007, 370 (9581): 59-67. 10.1016/S0140-6736(07)61050-2.
Silverberg MJ, Chao C, Leyden WA, Xu L, Tang B, Horberg MA, Klein D, Quesenberry CP, Towner WJ, Abrams DI: HIV infection and the risk of cancers with and without a known infectious cause. Aids. 2009, 23 (17): 2337-2345. 10.1097/QAD.0b013e3283319184.
Mooij SH, Boot HJ, Speksnijder AG, Meijer CJ, King AJ, Verhagen DW, de Vries HJ, Quint WG, Molijn A, de Koning MN, van der Sande MA, van der Loeff MF: Six-month incidence and persistence of oral HPV infection in HIV-negative and HIV-infected men who have sex with men. PLoS One. 2014, 9 (6): e98955-10.1371/journal.pone.0098955.
Molijn A, Kleter B, Quint W, van Doorn LJ: Molecular diagnosis of human papillomavirus (HPV) infections. J Clin Virol. 2005, 32 (Suppl 1): S43-S51. 10.1016/j.jcv.2004.12.004.
Xue X, Gange SJ, Zhong Y, Burk RD, Minkoff H, Massad LS, Watts DH, Kuniholm MH, Anastos K, Levine AM, Fazzari M, D’Souza G, Plankey M, Palefsky JM, Strickler HD: Marginal and mixed-effects models in the analysis of human papillomavirus natural history data. Cancer Epidemiol Biomarkers Prev. 2010, 19 (1): 159-169. 10.1158/1055-9965.EPI-09-0546.
van Aar F, Mooij SH, van der Sande MA, Speksnijder AG, Stolte IG, Meijer CJ, Verhagen DW, King AJ, de Vries HJ, van der Loeff MF S: Anal and penile high-risk human papillomavirus prevalence in HIV-negative and HIV-infected MSM. Aids. 2013, 27 (18): 2921-2931. 10.1097/01.aids.0000432541.67409.3c.
Gillison ML, D’Souza G, Westra W, Sugar E, Xiao W, Begum S, Viscidi R: Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst. 2008, 100 (6): 407-420. 10.1093/jnci/djn025.
Read TR, Hocking JS, Vodstrcil LA, Tabrizi SN, McCullough MJ, Grulich AE, Garland SM, Bradshaw CS, Chen MY, Fairley CK: Oral human papillomavirus in men having sex with men: risk-factors and sampling. PLoS One. 2012, 7 (11): e49324-10.1371/journal.pone.0049324.
Ong JJ, Read T, Chen M, Walker S, Law M, Bradshaw C, Garland SM, Tabrizi SN, Cornall A, Grulich A, Hocking J, Fairley CK: Improving oral human papillomavirus detection using toothbrush sampling in HIV-positive men who have sex with men. J Clin Microbiol. 2014, 52 (6): 2206-2209. 10.1128/JCM.00286-14.
Bui TC, Markham CM, Ross MW, Mullen PD: Examining the association between oral health and oral HPV infection. Cancer Prev Res (Phila). 2013, 6 (9): 917-924. 10.1158/1940-6207.CAPR-13-0081.
Hang D, Liu F, Liu M, He Z, Sun M, Liu Y, Li J, Pan Y, Ning T, Guo C, Liang Y, Xu R, Zhang L, Cai H, Ke Y: Oral human papillomavirus infection and its risk factors among 5,410 healthy adults in china, 2009–2011. Cancer Epidemiol Biomarkers Prev. 2014, 23 (10): 2101-2110. 10.1158/1055-9965.EPI-14-0084.
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, Liu L, Lynch CF, Wentzensen N, Jordan RC, Altekruse S, Anderson WF, Rosenberg PS, Gillison ML: Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011, 29 (32): 4294-4301. 10.1200/JCO.2011.36.4596.
Hocking JS, Stein A, Conway EL, Regan D, Grulich A, Law M, Brotherton JM: Head and neck cancer in Australia between 1982 and 2005 show increasing incidence of potentially HPV-associated oropharyngeal cancers. Br J Cancer. 2011, 104 (5): 886-891. 10.1038/sj.bjc.6606091.
Rietbergen MM, Leemans CR, Bloemena E, Heideman DA, Braakhuis BJ, Hesselink AT, Witte BI, de Jong RJ B, Meijer CJ, Snijders PJ, Brakenhoff RH: Increasing prevalence rates of HPV attributable oropharyngeal squamous cell carcinomas in the Netherlands as assessed by a validated test algorithm. Int J Cancer. 2013, 132 (7): 1565-1571. 10.1002/ijc.27821.
Acknowledgements
The authors would like to thank Stichting HIV Monitoring (SHM), in particular Frank de Wolf and Colette Smit, for their contributions in data collection; the members of the H2M steering committee for their advice; the personnel of the ACS, MC Jan van Goyen, and the Amsterdam STI clinic for their contributions to the implementation of the study and data collection; Martijn van Rooijen and Linda May for assisting in data management; Wilma Vermeulen (Public Health Service of Amsterdam) for HPV genotyping; Jan Sonsma and Marina Burger (RIVM) for DNA isolation; Anna Giuliano for practical help and advice; and Claire Buswell for editorial review. Above all, we gratefully acknowledge all study participants for their co-operation.
Funding
This work was supported by Aids Fonds [grant number 2009029], and additional funding was provided by the Public Health Service of Amsterdam and RIVM. Sanofi Pasteur MSD funded laboratory analysis of the 6-month oral samples through an unrestricted grant. The Amsterdam Cohort Studies on HIV infection and AIDS, a collaboration between the Public Health Service of Amsterdam, the Academic Medical Center of the University of Amsterdam, Sanquin Blood Supply Foundation, and the University Medical Center Utrecht, are part of the Netherlands HIV Monitoring Foundation and financially supported by the Netherlands National Institute for Public Health and the Environment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
M. Schim van der Loeff participated in a Merck-funded investigator-initiated study on Gardasil®. M. Schim van der Loeff, C.J.L.M. Meijer, and T. Heijman are co-investigators on an HPV vaccine trial of Sanofi-Pasteur MSD. All other authors declare that they have no competing interests.
Authors’ contributions
MSvdL, MvdS, CM, SM and RC conceived and designed the study. SM, DV, and TH included participants and collected data. SM and AK analyzed and interpreted laboratory results. FvA analyzed the data. SM, CM, RC and MSvdL contributed to the data analysis and interpretation of the data. FvA and SM drafted the manuscript. All authors contributed to critical revision of the article, and read and approved the final version.
Fleur van Aar, Sofie H Mooij contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
van Aar, F., Mooij, S.H., van der Sande, M.A. et al. Twelve-month incidence and clearance of oral HPV infection in HIV-negative and HIV-infected men who have sex with men: the H2M cohort study. BMC Infect Dis 14, 668 (2014). https://doi.org/10.1186/s12879-014-0668-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-014-0668-z