Abstract
Background
Frailty becomes more pronounced with advancing age, tightly intertwined with adverse clinical outcomes. Across diverse medical disciplines, frailty is now universally recognized as not only a risk factor but also a predictive indicator for unfavorable clinical prognosis.
Methods
This study was a retrospective cohort study that included clinical data from patients (aged ≥ 65 years) with esophageal cancer treated surgically at the First Affiliated Hospital of Anhui Medical University in 2021. For each patient, we calculated their 11-index modified frailty index(mFI-11) scores and categorized the patients into a frailty group (mFI-11hign) and a non-frailty group (mFI-11low) based on the optimal grouping cutoff value of 0.27 from a previous study. The primary study index was the incidence of postoperative pulmonary infection, arrhythmia, anastomotic fistula, chylothorax, and electrolyte disturbance complications. Secondary study indicators included postoperative ICU stay, total hospitalization time, readmission rate within 30 days of discharge, and mortality within 30 days after surgery. We performed univariate and multivariate analyses to assess the association between mFI-11 and adverse outcomes as well as postoperative complications.
Results
Five hundred and fifteen patients were included, including 64.9% (334/515) in the non-frailty group and 35.1% (181/515) in the frailty group. Comparing postoperative complication rates between the two groups revealed lower incidences of postoperative anastomotic fistula (21.5% vs. 4.5%), chylothorax (16.0% vs. 2.1%), cardiac arrhythmia (61.9% vs. 9.9%), pulmonary infections (85.1% vs. 26.6%), and electrolyte disturbance (84.5% vs. 15.0%) in patients of the non-frailty group was lower than that in the frailty group (p < 0.05). mFI-11 showed better prognostic results in predicting postoperative complications. anastomotic fistula (area under the ROC curve AUROC = 0.707), chylothorax (area under the ROC curve AUROC = 0.744), pulmonary infection (area under the ROC curve AUROC = 0.767), arrhythmia (area under the ROC curve AUROC = 0.793), electrolyte disturbance (area under the ROC curve AUROC = 0.832), and admission to ICU (area under the ROC curve AUROC = 0.700).
Conclusion
Preoperative frail elderly patients with esophageal cancer have a high rate of postoperative complications. mFI-11 can be used as an objective indicator for identifying elderly patients at risk for esophageal cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Esophageal cancer has been one of the common malignant tumors worldwide, with 604,000 new cases and 544,000 deaths according to the global cancer statistics in 2020 [1]. China is a region with high incidence of esophageal cancer, and although the incidence and mortality rates of esophageal cancer in China are on a decreasing trend, it is still one of the major malignant tumors threatening the health of Chinese residents. Nowadays, with the accelerated aging of the population, the number of elderly patients with esophageal cancer has increased, and esophageal cancer surgery itself is characterized by complex surgery, high incidence of postoperative complications, and long hospital stay, and elderly and frailty patients are a challenge for thoracic surgeons [2]. Elderly patients tend to have varying degrees of organ degeneration, mostly associated with chronic diseases and a higher risk of cardiovascular complications. For the same surgical procedure, the elderly are more susceptible to poor prognosis [3, 4]. These factors can adversely affect prognosis and recovery.
In order to decide whether to recommend surgery, clinicians attempt to predict the risk of adverse postoperative outcomes before surgery. Numerous studies have shown that some metrics are predictive of postoperative complications, such as tumor lymph node metastasis (TNM) pathologic stage and prognostic nutritional index (PNI) [5], whereas current preoperative risk stratification strategies do not take into account physiological impairments specific to elderly adults and typically assess physiological impairments specific to a single end organ rather than more comprehensive physiological impairments related to the entire patient [6]. These metrics lack the ability to measure a patient’s physiologic reserve, which is why this paper introduces the concept of frailty. Frailty is a term used for elderly adults, and this increased vulnerability due to physical causes is defined as frailty, which reflects the loss of physiological reserve due to stressors, and elderly patients who are particularly subject to oncological treatments and surgical procedures are at higher risk [7].Velanovich and colleagues summarized the frailty index into 11 variables called the Modified Frailty Index-11 (mFI-11) [8], and previous studies have confirmed that frailty is one of the independent risk factors for perioperative complications in elderly patients. The more frail the patient, the higher the incidence of adverse outcomes after surgery [9].
At this stage, there are still fewer assessments studying the correlation between preoperative frailty index and postoperative complications in elderly patients with esophageal cancer. In this paper, we retrospectively summarized the clinical data of patients with esophageal cancer who were surgically treated in the Department of Thoracic Surgery of the First Affiliated Hospital of Anhui Medical University in the year of 2021 with the aim of exploring the relationship between mFI-11 and the perioperative clinical characteristics and clinical prognosis of elderly patients with esophageal cancer, and to compare the effects of mFI-11, TNM, and PNI in predicting the postoperative adverse outcomes.
Materials and methods
Patient screening and grouping
Clinical data of elderly patients with esophageal cancer treated by surgery in the First Affiliated Hospital of Anhui Medical University in 2021 were retrospectively analyzed. Inclusion criteria: Inclusion criteria: (1) diagnosis of esophageal cancer, (2) patients who underwent radical surgery for esophageal cancer, (3) aged ≥ 65 years. Exclusion criteria: (1) personal oncological history, (2) patients with preoperative neoadjuvant radiotherapy, (3) patients treated with blood transfusion for reoperation or intraoperative bleeding within 24 h after surgery due to surgical factors, (4) patients with missing covariate data.
Date collection
The data were collected through the following data in the Tung Wah Digital Hospital Information Management System (HIS) of Tung Wah Medical Technology Co: Baseline data, including age, gender, body mass index (BMI), diabetes mellitus, hypertension, history of cardiovascular disease, delirium, independent functional status, and preoperative American Society of Anesthesiologists (ASA) classification; laboratory indicators, including serum albumin and lymphocytes; perioperative clinical data, including surgical approach, duration of surgery, bleeding, urine output, fluid infusion, preoperative and postoperative oxygenation index, ICU stay, total hospitalization time, the presence of complications (pulmonary infection, cardiac arrhythmia, anastomotic fistula, chylothorax, and electrolyte disturbance, etc.); and the rate of readmission within 30 days of discharge and the rate of mortality in the first 30 days of postoperative period;
Measurements
We chose mFI-11, TNM staging and PNI to predict poor prognosis after radical esophageal cancer surgery in elderly patients and to compare the prognostic value of all three. mFI-11 was calculated using 11 variables (10 comorbidities and 1 functional status measure) from the Canadian Study of Health and Aging (CSHA) center. Including functional status, history of diabetes, respiratory problems, congestive heart failure, myocardial infarction, cardiac problems, arterial hypertension, delirium, history related to cognitive impairment or loss, cerebrovascular problems, and history of stroke/decreased peripheral pulses [10, 11]. For frailty, the number of positive variables was calculated by dividing the patient’s number of positive variables by the total number of variables [11]. Scores ranged from 0 to 1. High risk of frailty (mFI-11 High) was defined when the mFI-11 score was ≥ 0.27, and low risk of frailty (mFI-11 Low) when the mFI-11 score was less than 0.27. The PNI was calculated as 10 × peripheral serum protein (g/L) + 0.005 × peripheral blood lymphocyte count (mm3) [12].
Statistical analysis
Measures that followed a normal distribution were presented as mean ± standard deviation (x ± s), and comparisons between groups were made using the independent sample t-test. Categorical variables were described using frequencies and percentages and were compared using the χ2 test or Fisher’s exact test, as appropriate. Univariate and multivariate logistic regression were conducted to identify independent risk factors for postoperative complications, mortality, and ICU admission. A significance level of P ≤ 0.05 was used to determine statistical significance. Receiver operating characteristic (ROC) curve analysis was utilized to evaluate the impact of various factors on the prediction of postoperative complications, mortality, and ICU admission. SPSS 26.0 software was utilized for all statistical analyses.
Result
515 patients were part of the study, with 64.85% classified as having low mFI-11 and 35.15% classified as having high mFI-11. The flow chart of the study is depicted in Fig. 1.The frailty group was older than the non-frailty group (73.86 ± 0.19 vs. 70.94 ± 0.22), with a lower percentage of ASA classification I-II (26.4% vs. 73.6%) and a higher percentage of classification III ~ IV (38.4% vs. 61.6%).Hospitalization duration was significantly longer in the frailty group compared to the non-frailty group (16.93 ± 0.71 vs. 14.84 ± 0.36), and surgery duration was longer in the frailty group compared to the non-frailty group(266.35 ± 6.70 vs. 257.12 ± 3.66), with a p-value of less than 0.05.There was no significant difference in the remaining baseline and surgical data (p > 0.05); refer to Table 1.
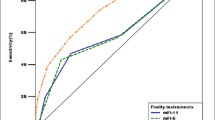
Prognostic value of 11-index modified frailty index, tumor-node-metastasis stage, and prognostic nutritional index for postoperative adverse outcomes. In comparison to the other two measures, the 11-index modified frailty index scale showed the best predictive value in terms of the area under the curve. A-F: The receiver operating characteristic (ROC) curves of 11-index modified frailty index (mFI-11), tumor-node-metastasis (TNM) stage, and prognostic nutritional index (PNI) in predicting anastomotic fistula (A), chylothorax (B), pulmonary infection (C), arrhythmia (D), electrolyte disturbance (E), admission to ICU (F)
The adverse outcomes following radical treatment in elderly patients with esophageal cancer are analyzed using multivariate logistic regression in Table 2. Analysis of multiple variables indicated that mFI-11 was a significant predictor of postoperative results (Anastomotic fistula: aOR = 6.550, P < 0.001; chylothorax: aOR = 9.125, P < 0.001; Arrhythmia: aOR = 19.911, P < 0.001; Pulmonary infection: aOR = 15.582, P < 0.001; Electrolyte disturbance: aOR = 35.330, P < 0.001; Admission to ICU: aOR = 6.487 P = 0.021; Readmission 30 days after discharge: aOR = 2.046, P = 0.044, a statistically significant difference. 1-mouth mortality: aOR = 3.187, P = 0.353, difference not statistically significant).
Figure 2 shows the prognostic value of the mFI-11, TNM staging, and PNI for adverse postoperative outcomes. The mFI-11 scale showed the best predictive value for area under the curve compared to the other two measures. The mFI-11 had the greatest predictive value for postoperative anastomotic fistula, with an area under the curve of (0.707), while TNM staging had a value of (0.606) and PNI had the lowest at (0.500).mFI-11 was the most accurate in predicting postoperative chylothorax with an area under the curve of (0.744), PNI followed closely behind with (0.693), and TNM staging had the lowest accuracy at (0.563).When it comes to forecasting postoperative pulmonary infection, mFI-11 showed the greatest area under the curve at (0.767), with PNI following at (0.571), and TNM staging coming in last at (0.536).mFI-11 was the most accurate in predicting postoperative arrhythmia with an area under the curve of (0.793), while TNM staging had a lower accuracy at (0.608), and PNI had the lowest accuracy at (0.598).In predicting postoperative electrolyte disturbance, mFI-11 had the highest area under the curve at (0.832), with PNI following at (0.555), and TNM staging having the lowest at (0.441).The mFI-11 demonstrated the greatest area under the curve for ICU admission (0.700), with TNM staging following closely behind (0.634), while PNI had the lowest value (0.580).
Discussion
With the progression of the aging population and the consequent corresponding increase in the number of elderly patients of all types, frailty is becoming an increasingly established risk factor for poor postoperative prognosis [13]. mFI-11 is considered to be a reliable tool for predicting adverse clinical outcomes and providing risk stratification in healthcare. Radical esophageal cancer surgery is considered one of the best treatments for patients [14]. However, radical surgery, as a more traumatic surgery, which is more complicated, prolonged, and traumatizing, and can result in complications related to pulmonary infection, chylothorax, and anastomotic fistula [15, 16]. Therefore, preoperative risk assessment is particularly important. In response to the interest in accurate risk stratification, the surgical community has largely moved away from assessments based on subjective clinical judgment (e.g., ASA classification) to more objective analytical methods such as the mFI-11 [17]. In addition, elderly patients with esophageal cancer in the frailty group had a higher readmission rate within 30 days of discharge and a higher mortality rate within 30 days after surgery. For the first time, we compared the prognostic value of mFI-11, TNM staging (TNM early stages (I + II) vs. advanced stages (III + IV)), and PNI on postoperative outcomes in elderly esophageal cancer patients. After comparing the prognostic value of mFI-11, TNM staging, and PNI for the three postoperative adverse outcomes, we found that mFI-11 had the best prognostic value. It also proves that frailty condition is an independent risk factor for poor postoperative outcome, which provides some reference for clinicians to intervene in Perioperative frailty status, and this study helps to fill the gap in our understanding of how frailty affects the postoperative prognosis of elderly esophageal cancer patients.
In this study, TNM stage was an independent risk factor for postoperative complications in esophageal cancer. However, cancer is a systemic disease and its prognosis depends not only on the tumor itself, but also on the underlying physical condition and functional reserve [18]. PNI was used as a representative parameter of the patients’ nutritional status in this study and has been used as a surrogate for the nutritional status of various oncologic diseases [19]. Unlike other tumor patients undergoing surgery, patients with esophageal cancer often experience choking on food and reduced oral food intake, and some even require parenteral nutritional support preoperatively, and the cancer disease is considered to be consumptive [20]. Due to the lack of screening programs, many patients are diagnosed at an advanced stage. Many patients seek medical advice only after unexpected and significant weight loss, which may have resulted in severely compromised nutritional supply, vitamins and micronutrients [21]. In this study, PNI was an independent risk factor for postoperative complications in patients with esophageal cancer. Deteriorating nutritional status may lead to a poor prognosis, and improving the nutritional status of patients with low preoperative PNI may improve the outcome of perioperative treatment in patients with esophageal cancer; however, the use of nutritional status indicators alone did not incorporate functional reserve.
Frailty is more common in the elderly group, especially in the higher age group, because of the weakening of the body and the decline in functional reserve with age, and because most of them are associated with chronic diseases and the risk of cardiovascular complications increases with age [22]. In our study, the median age was 70 years in the non-frailty group and 72 years in the frailty group, which is significantly elderly and also suggests that frailty is more common in elderly patients. However, it is worth noting that not all elderly patients are frailty, a study has shown that patients over 90 years old can safely undergo curative esophagectomy for esophageal cancer, and elderly patients with good preoperative performance continue to achieve favorable short-term and long-term outcomes postoperatively [23]. mFI-11 provides rapid identification in clinical practice, allowing for early recognition and improvement of a patient’s physiologic reserve. This approach can lead to the best outcomes for patients with underlying disease or low functional reserve.
The results of the data were analyzed to show an increased incidence of postoperative complications in frail elderly esophageal cancer patients, the highest incidence of complications is pulmonary infection, followed by electrolyte disturbance, cardiovascular disease, and anastomotic fistula. This study showed that the total incidence of postoperative pulmonary infection in elderly esophageal cancer patients was 46.9%, with 29.7% in the frailty group, which was significantly higher than that in the non-frailty group. Esophageal cancer surgery requires cervical, thoracic, and abdominal incisions, which is more complicated to operate, with a long operating time, high surgical trauma, and the open thoracic cavity will increase the pulmonary circulation resistance and aggravate the cardiac load, and prolonged surgery is prone to postoperative cardiovascular and cerebrovascular complications [24]. In our study, we also found that the incidence of postoperative cardiac arrhythmia was higher in frailty patients, so we should do a good preoperative cardiopulmonary function examination, active preoperative intervention and strengthen postoperative monitoring for elderly frailty patients, so that the patients can successfully pass through the perioperative period.
The mFI-11 score has been applied to the National Surgical Quality Improvement (NSQIP data) repository, which provides a more comprehensive and systematic preoperative risk assessment. However, it lacks indicators of physical function such as nutrition and metabolism [2], and may be considered for joint assessment with the PNI.
The mFI-11 score was calculated using 11 variables assessed by CSHA and has been shown to be helpful in predicting the prognosis of elderly patients. Optimization and intervention of preoperative status benefits both the patient and the physician while reducing the burden on the healthcare system. It has been found that anastomotic leakage after gastroesophageal anastomosis leads to a longer postoperative hospital stay of 22–28 days on average compared to cases without anastomotic leakage [25], which is a significant burden for patients and their families. Therefore, incorporating the mFI-11 into clinical decision-making can help to identify and stratify elderly patients undergoing radical esophagectomy for cancer, enhance understanding of the additional risks associated with increased frailty, raise expectations for the recovery process, and optimize patient prognosis.
Our study has several limitations. First, this study was a single-center retrospective study, and the results may not be fully representative of the overall situation of Chinese patients due to the lack of large-scale epidemiological surveys and studies in China for elderly patients undergoing radical esophageal cancer treatment. Therefore, future studies with larger samples are necessary to further validate these findings. Second, this study only analyzed the data of esophageal cancer patients in our hospital in 2021, focusing on the data within 1 month after surgery, which may have underestimated the complication rate. Therefore, our next step should be to track the follow-up data of esophageal cancer patients for 2 and 5 years or even longer after surgery. Nonetheless, this study used the mFI-11 > 0.27 score as a threshold for radical esophageal cancer surgery in the elderly, demonstrating that the mFI-11 can be used as an objective indicator for identifying high-risk patients and can be used to predict adverse outcomes in elderly patients with esophageal cancer, which suggests that the mFI-11 is promising for use in rapid preoperative clinical risk stratification, thereby better guiding the allocation of healthcare resources.
Conclusion
In summary, the mFI-11 index based on case data studies proved to be a reliable predictor of complications within 30 days after radical esophageal cancer surgery. Preoperative frailty assessment may more accurately identify high-risk patients and provide useful prognostic information for elderly patients undergoing radical esophageal cancer surgery.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- mFI-11:
-
11-Factor Modified Frailty Index
- BMI:
-
Body mass index
- CSHA:
-
Canadian Study of Health and Aging
- ASA:
-
American Society of Anesthesiologists
- TNM:
-
Tumor-node-metastases
- PNI:
-
Prognostic nutritional index
- ICU:
-
Intensive care unit
- ROC:
-
Receiver operating characteristic
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Zheng C, Luo C, Xie K, Li JS, Zhou H, Hu LW et al. Surgical Apgar score could predict complications after esophagectomy: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2022;35(1).
Huang L, Li Z, Jian M, Wu X, Chen H, Qin H, et al. Application of MFI-5 in severe complications and unfavorable outcomes after radical resection of colorectal cancer. World J Surg Oncol. 2023;21(1):307.
Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–8.
Zhang Q, Qian L, Liu T, Ding JS, Zhang X, Song MM, et al. Prevalence and Prognostic Value of Malnutrition among Elderly Cancer patients using three Scoring systems. Front Nutr. 2021;8:738550.
Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American: Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):1971-96.
Xu SJ, Lin LQ, Chen C, Chen TY, You CX, Chen RQ, et al. Textbook outcome after minimally invasive esophagectomy is an important prognostic indicator for predicting long-term oncological outcomes with locally advanced esophageal squamous cell carcinoma. Ann Transl Med. 2022;10(4):161.
Araújo-Andrade L, Rocha-Neves JP, Duarte-Gamas L, Pereira-Neves A, Ribeiro H, Pereira-Macedo J, et al. Prognostic effect of the new 5-factor modified frailty index in patients undergoing carotid endarterectomy with regional anesthesia - A prospective cohort study. Int J Surg. 2020;80:27–34.
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394(10206):1376–86.
Mathur S, Prince L, Bucher O, Xue L, Banerji S, Dawe DE. The impact of the modified frailty index on clinical outcomes for patients with stage IV non-small cell lung cancer receiving chemotherapy. J Geriatr Oncol. 2022;13(5):654–61.
Rath D, Chatterjee M, Müller I, Müller K, Böckmann C, Droppa M, et al. Platelet expression of transforming growth factor beta 1 is enhanced and associated with cardiovascular prognosis in patients with acute coronary syndrome. Atherosclerosis. 2014;237(2):754–9.
Okadome K, Baba Y, Yagi T, Kiyozumi Y, Ishimoto T, Iwatsuki M, et al. Prognostic Nutritional Index, Tumor-infiltrating lymphocytes, and prognosis in patients with esophageal Cancer. Ann Surg. 2020;271(4):693–700.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–75.
Francischetto T, Pinheiro V, Viana EF, Moraes ED, Protásio BM, Lessa MAO, et al. EARLY POSTOPERATIVE OUTCOMES OF THE ESOPHAGECTOMY MINIMALLY INVASIVE IN ESOPHAGEAL CANCER. Arq Bras Cir Dig. 2023;36:e1743.
Schuring N, Jezerskyte E, van Berge Henegouwen MI, Sprangers MAG, Lagergren P, Johar A, et al. Influence of postoperative complications following esophagectomy for cancer on quality of life: a European multicenter study. Eur J Surg Oncol. 2023;49(1):97–105.
Lee DU, Hastie DJ, Fan GH, Addonizio EA, Han J, Karagozian R. Clinical frailty is a risk factor of adverse outcomes in patients with esophageal cancer undergoing esophagectomy: analysis of 2011–2017 US hospitals. Dis Esophagus. 2022;35(8).
Palliyaguru DL, Moats JM, Di Germanio C, Bernier M, de Cabo R. Frailty index as a biomarker of lifespan and healthspan: focus on pharmacological interventions. Mech Ageing Dev. 2019;180:42–8.
Xu ZY, Hao XY, Wu D, Song QY, Wang XX. Prognostic value of 11-factor modified frailty index in postoperative adverse outcomes of elderly gastric cancer patients in China. World J Gastrointest Surg. 2023;15(6):1093–103.
Jiang P, Li X, Wang S, Liu Y. Prognostic significance of PNI in patients with pancreatic Head Cancer undergoing laparoscopic pancreaticoduodenectomy. Front Surg. 2022;9:897033.
Reim D, Friess H. Feeding challenges in patients with esophageal and gastroesophageal cancers. Gastrointest Tumors. 2016;2(4):166–77.
Vandebroek AJ, Schrijvers D. Nutritional issues in anti-cancer treatment. Ann Oncol. 2008;19(Suppl 5):v52–5.
Uchikado Y, Ikeda Y, Ohishi M. Current understanding of the role of Frailty in Cardiovascular Disease. Circ J. 2020;84(11):1903–8.
Pultrum BB, Bosch DJ, Nijsten MW, Rodgers MG, Groen H, Slaets JP, et al. Extended esophagectomy in elderly patients with esophageal cancer: minor effect of age alone in determining the postoperative course and survival. Ann Surg Oncol. 2010;17(6):1572–80.
Soh CH, Guan L, Reijnierse EM, Lim WK, Maier AB. Comparison of the modified Frailty-Index based on laboratory tests and the clinical Frailty Scale in predicting mortality among geriatric rehabilitation inpatients: RESORT. Arch Gerontol Geriatr. 2022;100:104667.
Fabbi M, Hagens ERC, van Berge Henegouwen MI, Gisbertz SS. Anastomotic leakage after esophagectomy for esophageal cancer: definitions, diagnostics, and treatment. Dis Esophagus. 2021;34(1).
Acknowledgements
Not applicable.
Funding
This study was supported by grants from Natural Science Foundation of Anhui Medical Universities (KJ2019ZD22); Natural Science Foundation of Anhui Province (1808085QH271).
Author information
Authors and Affiliations
Contributions
X.C. and Y.D.: wrote the main manuscript text. Q.Z. and M.Y.H.: Conducted the study and managed the database. H.L.W. and J.R.X.: Designed and drafted the manuscript. Y.F.X. and L.Y.: collected the data, edited and reviewed the manuscript. R.Q.Z: writing-review and editing, investigation, validation, supervision, and conceptualization. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the ethics committee of the First Affiliated Hospital of Anhui Medical University, Hefei, China (Approval number: Quick -PJ 2023-14-80). All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, X., Dang, Y., Zhang, Q. et al. MFI-11 in Chinese elderly esophageal cancer patients with postoperative adverse outcomes. BMC Geriatr 24, 677 (2024). https://doi.org/10.1186/s12877-024-05281-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05281-x