Abstract
Background
Due to the high prevalence of multimorbidity and realistic health service demands for fall prevention, there is growing interest in the association between multimorbidity and falls. Our study aimed to identify multimorbidity patterns among Chinese older adults and explore the association between multimorbidity patterns and falls.
Methods
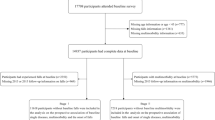
Data from 4,579 Chinese community-dwelling older adults was included in this analysis. Information regarding falls and 10 chronic conditions was collected. An exploratory factor analysis was performed to determine multimorbidity patterns. Regression models were fitted to explore the associations of individual chronic disease or multimorbidity patterns with falls.
Results
Among 4,579 participants, 368 (8.0%) were defined as fallers, including 92 (2.0%) frequent fallers, and multimorbidity affected 2,503 (54.7%) participants. Older adults with multimorbidity were more likely to be fallers [odds ratio (OR) = 1.3, P = 0.02] and frequent fallers (OR = 1.7, P = 0.04). Three multimorbidity patterns were identified (i.e., cardiovascular-metabolic diseases, psycho-cognitive diseases and organic diseases), and the associations between psycho-cognitive diseases/organic diseases and prevalent falls or frequent falls were found to be significant.
Conclusions
The psycho-cognitive disease pattern and organic disease pattern are significantly associated with falls. Therefore, more attention should be paid to patients with psycho-cognitive diseases and timely, targeted diagnostic and treatment services should be provided in fall prevention.
Similar content being viewed by others
Introduction
Falls, defined as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level” [1], have become the second leading cause of death in older adults [2]. Approximately 30% older adults aged 65 years and above experience falls annually [3]. Even without injury-related death [4], falls can lead to a series of adverse health outcomes, such as activity restriction [5], mental health disorders [6] and reduced quality of life [7], which may result in a heavy health care burden. Meanwhile, the substantial costs related directly or indirectly to fall management should also be recognized [8]. Thus, it is imperative to investigate the risk factors associated with falls, which may offer invaluable insights for formulating effective prevention strategies tailored to older adults.
To date, numerous studies have investigated the association between falls and chronic conditions and confirmed the adverse effect of a single chronic condition, such as stroke, cataracts and depression [9,10,11]. Considering that 65–85% of older adults suffer from multimorbidity [12], which is defined as the co-occurrence of two or more chronic conditions in the same person [13], focusing only on single-disease models may fail to meet the realistic health service demands of fall prevention [14]. Several studies have assessed the potential relationship between multimorbidity and falls among older adults. For example, a community-based study including 12,669 older adults in America found that an increasing number of chronic conditions was associated with the frequency of falls in the previous year [15]. Moreover, a longitudinal study in Ireland determined that multimorbidity increased the risk for incident falls in older adults. However, the majority of relevant studies have been conducted in developed countries [16,17,18], and there is a lack of research in developing countries such as China, which is facing the conflict between the rapid population aging problem and a shortage of healthcare resources for older adults [19]. Additionally, most studies focused on the number of chronic diseases [17], and few of them identified the patterns of multimorbidity and further investigated the influence of particular combinations of chronic diseases on fall experience or frequency.
Therefore, in this community-based study among older Chinese adults, we aimed to identify patterns of multimorbidity and investigate the relationship between patterns of multimorbidity and falls.
Methods
Study population
This study was a community-based study among adults aged 60 years or older residing in Weitang town in Suzhou, China. Details of the baseline study have been described elsewhere [20,21,22]. Based on the official records, there are 6,030 individuals aged 60 years or older in the town. At the recruitment stage, an invitation letter with the study objectives explained was sent to each family, inviting all the adults aged 60 years or older to participate in the study. The exclusion criteria were: (1) under 60 years old; (2) migration from the residing address; (3) living period less than 6 months in the Weitang town; and (4) death. From August 2014 to February 2015, a total of 4,611 subjects (82.1%) attended the clinic. Then, 32 subjects were excluded for incomplete data. Finally, 4,579 older adults were included for the analysis.
This study followed the tenets of the Helsinki Declaration and was approved by the Institutional Review Board of Soochow University. Written informed consent was obtained from all the participants.
Falls
Detailed information on falls of the eligible participants was collected through interviews by a trained research assistant. Participants responded to the question “How many times have you fallen down during the past twelve months?” Those who responded “at least once” were identified as “fallers”, while other participants were defined as “non-fallers”. If participants had fallen over once, he or she was regarded as a “frequent faller”.
Chronic conditions and multimorbidity
A total of ten chronic conditions were identified, including hypertension, diabetes, hyperlipidemia, obesity, stroke, heart disease, headache, cognitive dysfunction, depression and visual impairment. Given their considerable prevalence among Chinese older adults, as well as the potential associations with falls, they were taken into consideration [4, 16, 17, 23,24,25,26]. Participants were defined as having hypertension if their systolic/diastolic blood pressure was > 140/90 mmHg, respectively, or if they were taking anti-hypertension medications. Diabetes mellitus was defined as a fasting serum glucose level > 7.0 mmol/L or use of antidiabetic medication. We defined hyperlipidemia as the serum total cholesterol > 6.22 mmol/L, low density lipoprotein cholesterol > 4.14 mmol/L, triglycerides > 2.26 mmol/L or use of lipid-lowering medication. Participants with a body mass index equal to or greater than 28 kg/m2 were considered obese [27]. The presence of headache was self-reported by the participants. The presence of stroke and heart disease was determined through questions such as “Have you ever been told by a doctor that you had.?” The Abbreviated Mental Test (AMT) was used to assess cognitive status, with an AMT score of 6 or less suggestive of significant cognitive dysfunction [28]. The Patient Health Questionnaire-9 (PHQ-9) was applied to evaluate the psychological status of the participants. A total PHQ-9 score of 5 or above indicates clear depression [29]. The Chinese version of the AMT and PHQ-9 have been validated to have good reliability and validity in Chinese older adults [30,31,32,33]. Visual impairment was determined if the participant’s visual acuity, as measured by the Snellen Eye Chart, was worse than 20/40 in the better-seeing eye [34].
Assessment of covariates
Social-demographic characteristics (i.e., age, sex, education level, marital status) were collected using a predesigned questionnaire, in which marital status was divided into living “with” and “without partner”, education level was classified into “primary education or below” and “secondary education or above” and monthly income was categorized into three groups: “no more than 1000 Chinese Yuan (CNY)”, “1001 to 3000 CNY” and “more than 3000 CNY”. Moreover, information regarding lifestyle-related variables, including smoking status (smokers/non-smokers), alcohol status (drinkers/non-drinkers), tea consumption (drinkers/non-drinkers) and physical activity (with/without), was collected.
Statistical analysis
Means and standard deviations were used to describe continuous variables with percentages for categorical variables in descriptive studies. To compare the differences in characteristics of participants in demographic and behavioral aspects, Student’s t test and chi-square test were used for continuous and categorical variables, respectively. We performed an exploratory factor analysis of the 10 morbidities to determine multimorbidity patterns based on a tetrachoric correlation matrix. Eigenvalues greater than 1.0 combined with a scree plot were used to determine the number of domains [35]. A chronic condition with a factor loading of lower than 0.40 was excluded in a given pattern of multimorbidity. Multiple logistic regression models were used to examine the associations of chronic conditions and multimorbidity with fall experience and frequencies. Logistic models were controlled for social-demographic characteristics (i.e., age and gender) and lifestyle habits (i.e., education level, marriage status, monthly income, smoking status, alcohol consumption, tea consumption and physical activity).
All analyses were performed using SPSS version 21.0 (SPSS Inc., Chicago, IL, USA). A two-sided P value of less than 0.05 was considered statistically significant.
Results
Table 1 summarizes the sociodemographic characteristics of the study participants. Among 4,579 participants, 368 (8.0%) were defined as fallers in the current study, including 92 (2.0%) frequent fallers, and multimorbidity affected 2,503 (54.7%) participants. Compared to the non-fallers, the proportion of women among the fallers was higher than that of men (66.8% vs. 50.7%, P < 0.001). Participants who lived with a partner were less likely to be fallers (P = 0.036). Smokers and alcohol drinkers had a significantly lower risk of falls than non-smokers (P = 0.001) and non-alcoholic drinkers (P = 0.018), respectively. Fallers tended to have a significantly higher prevalence of stroke (3.3%, P = 0.011), heart disease (10.6%, P = 0.048), headache (28.0.6%, P < 0.001), depression (14.4%, P = 0.029), and visual impairment (21.2%, P = 0.029). The number of chronic diseases was significantly higher in the fallers (2.1 ± 1.4) than in the non-fallers (1.8 ± 1.2) (P < 0.001). The prevalence of multimorbidity was higher in the fallers (64.1%) than in the non-fallers (53.8%) (P < 0.001).
Table 2 demonstrates the association between different chronic conditions and falls, adjusting for different confounders. Participants with stroke [odds ratio (OR) = 2,144, 95% confidence interval (CI): 1.130–4.067, P = 0.020], headache (OR = 1.604, 95% CI: 1.253–2.053, P < 0.001), and depression (OR = 1.844, 95% CI: 1.331–2.556, P < 0.001) had a higher risk for falls. Participants with stroke (OR = 3.189, 95% CI: 1.223–8.316, P = 0.018), heart disease (OR = 2.288, 95% CI: 1.295–4.044, P = 0.004), and depression (OR = 2.379, 95% CI: 1.364–4.150, P = 0.002) were more likely to be frequent fallers.
Figure 1 suggests 3 patterns of multimorbidity, which could explain 36.83% of the total variance. Multimorbidity pattern 1 was cardiovascular-metabolic diseases, including hypertension, diabetes, hyperlipidemia and obesity. Multimorbidity pattern 2 contained cognitive dysfunction and depression, which was summarized as psycho-cognitive diseases. Multimorbidity pattern 3 referred to organic diseases consisting of stroke, heart disease, headache and visual impairment. The cumulative percentages of multimorbidity patterns 1, 2 and 3 were 12.38%, 24.68% and 36.83%, respectively.
The prevalence of falls and frequent falls based on different patterns of multimorbidity are shown in Figs. 2 and 3, respectively. The psycho-cognitive disease pattern of multimorbidity suggested the highest prevalence of falls (18.9%) and frequent falls (7.5%). In each of these patterns, the prevalence of falls and frequent falls was generally higher in participants with multimorbidity than in those without disease or with a single disease.
The associations between multimorbidity and falls are presented in Table 3. The higher the number of chronic conditions among participants, the more likely they were to be fallers (OR = 1.152, 95% CI: 1.049–1.265, P = 0.003) or frequent fallers (OR = 1.384, 95% CI: 1.180–1.623, P < 0.001). Additionally, participants with multimorbidity were also more likely to be fallers (OR = 1.308, 95% CI: 1.037–1.649, P = 0.024) or frequent fallers (OR = 1.668, 95% CI: 1.033–2.692, P = 0.036). The cardiovascular-metabolic disease pattern was not related to falls or frequent falls (all P > 0.05). The psycho-cognitive disease pattern with two or more diseases was positively associated with both falls (OR = 2.273, 95% CI: 1.445–3.575, P < 0.001) and frequent falls (OR = 3.150, 95% CI: 1.525–6.507, P = 0.002). The organic disease pattern with two or more diseases was also positively associated with both falls (OR = 1.814, 95% CI: 1.278–2.576, P = 0.001) and frequent falls (OR = 2.442, 95% CI: 1.308–4.557, P = 0.005).
Discussion
Within a sample of community-dwelling older adults in eastern China, our study results revealed that multiple chronic conditions were significantly related to falls among Chinese older adults, and two multimorbidity patterns (psycho-cognitive diseases and organic diseases) were found to be positively associated with prevalent falls or frequent falls.
In our study, 368 participants were defined as fallers, and 92 fallers were classified as frequent fallers. Surprisingly, our findings suggest that smokers and alcohol drinkers are associated with a lower risk of falls. This contradicts previous studies [34, 36, 37], which indicated that smokers and drinkers face a heightened risk of falls. The inconsistency observed may stem from the cross-sectional nature of our study, which limits our ability to establish the temporal sequence of events and control for all potential confounding factors associated with falls.
Our results suggested that the number of chronic conditions among older adults were positively associated with prevalent falls and frequent falls. Such results were consistent with previous studies [2, 16, 17], which is not surprising. Notably, we found three main patterns of multimorbidity in participants. Due to the remarkable heterogeneity in the methodological criteria among studies addressing patterns of multimorbidity, especially the difference in the number and types of chronic conditions under consideration, patterns from different studies appear to be diverse [38]. According to a systematic review of 14 original studies, older adults living in Western countries have 3 major patterns of multimorbidity, including cardiovascular and metabolic diseases, mental health problems and musculoskeletal disorders [38]. This result was similar to our findings. In terms of cardiovascular-metabolic diseases, the impact of certain diseases on falls has been widely reported [39,40,41,42]. For example, older adults suffering from hypertension are more likely to experience transient cerebral ischemia because of acute orthostatic drops in blood pressure, which may exacerbate a chronic decrease in cerebral blood flow and finally lead to falls [39, 40]. However, a significant association between cardiovascular-metabolic diseases and falls was not observed in the current study. The following 2 reasons may have contributed to this inconsistency. On the one hand, the community-based participants in our study reported a low prevalence of prevalent falls and frequent falls (8.0% and 2.0%, respectively), which may lead to the failure to detect a statistically significant association. On the other hand, specific drug therapy and lifestyle modifications after developing certain cardiovascular-metabolic diseases tend to attenuate the effect of the disease itself on falls. For instance, as antilipidemic drugs, statins might beneficially increase bone health and subsequently reduce the risk of falls [43]. Additionally, studies have indicated that obese older adults prefer to reduce their daily activities to rest at rest because of fear of falling, thus decreasing the chances of falling [44]. Further studies are needed to determine the association and underlying mechanisms between cardiovascular-metabolic diseases and falls.
According to our study results, older adults suffering from organic diseases were at greater risk of being fallers. In contrast to primary cardiovascular-metabolic diseases, the role of secondary organic diseases that contributed to falls appeared to be more evident. A cross-sectional study in Singapore analyzed data from 10,033 participants and suggested that diabetes per se was not linked to a higher risk of falls, but diabetes patients with diabetic retinopathy were more likely to have fallen (OR = 1.31, 95% CI: 1.07–1.60, P = 0.008) than participants without diabetes, which revealed that secondary visual impairment actually increased the risk of falls [45]. In addition, the results of our study showed that stroke was significantly associated with both falls and frequent falls in the regression models of individual diseases. Falls are common accidents at all stages after stroke, including the acute, rehabilitative, and chronic phases [9]. A series of impairments from stroke substantially increases the probability of falls, such as decreased strength and balance, perceptual or visual problems and hemineglect [9].
It is worth noting that the pattern of psycho-cognitive diseases was found to exhibit the largest OR value in predicting fallers and frequent fallers (2.3 and 3.2, respectively), suggesting a great risk of falls when cognitive dysfunction and depression co-occurred. Previous studies have reported that impaired orientation, confusion and misperception of functional ability in patients suffering from cognitive dysfunction could significantly increase the risk of falls [43]. Meanwhile, the adverse effect of depression on falls has been widely confirmed [11, 46, 47]. The psychological and behavioral changes due to depression could contribute to accidental falls, including reduced motivation/apathy, social isolation and physical inactivity [48]. The side effects of antidepressants are also noteworthy, which have been classified as risk-increasing drugs [49]. Moreover, the co-occurrence of cognitive dysfunction and depression seems to lead to a larger risk of falls than having a single disease. A systematic review focused on older adults with cognitive dysfunction suggested that patients simultaneously suffering from depression symptoms were more likely to be fallers than patients without depression [50]. The structures in the brain that regulate cognitive functions and process emotional information (i.e., the hippocampal formation and prefrontal cortex) have strong neural synchrony and interact in a bidirectional manner, leading to a firm link between cognitive and mental disorders [51]. Thus, the co-occurrence of cognitive dysfunction and depression might contribute to further deterioration of each. Such results may remind policy makers to pay more attention to older adults with the multimorbidity of psycho-cognitive diseases when developing fall prevention programs.
To the best of our knowledge, this was the first study exploring the relationship between multimorbidity and falls in China, including identifying the patterns of multimorbidity. In addition, the large sample size of our research enhances the trustworthiness of the results. Our findings are expected to provide useful information for the development of fall prevention programs for older adults in the community. However, our study still has several limitations. First, considering our cross-sectional study design, the causal direction of the relationship could not be inferred. Second, due to study design we have only included a limited number of chronic conditions and failed to incorporate several diseases that have a high prevalence among older adults, such as cancer [52], arthritis [52], seizure disorder [53] and overactive bladder [54]. Third, the information on falls and partial data on chronic disease used in our study were self-reported; therefore, recall and reporting bias cannot be excluded.
Conclusions
In summary, our study revealed that multimorbidity patterns were significantly associated with prevalent falls and frequent falls among Chinese older adults. Moreover, the psycho-cognitive disease pattern and organic disease pattern were positively related to falls. Therefore, more attention should be paid to the combination of specific diseases in the heath management among older adults, especially the psycho-cognitive diseases.
Data availability
The datasets analyzed in this study are available from the corresponding author (Chen-Wei Pan, pcwonly@gmail.com) upon reasonable request.
References
Kruschke C, Butcher HK. Evidence-based Practice Guideline: fall Prevention for older adults. J Gerontol Nurs. 2017;43:15–21.
Barik M, Panda SN, Tripathy SS, Sinha A, Ghosal S, Acharya AS, et al. Is multimorbidity associated with higher risk of falls among older adults in India? BMC Geriatr. 2022;22:486.
Ganz DA, Latham NK. Prevention of Falls in Community-Dwelling older adults. N Engl J Med. 2020;382:734–43.
Colón-Emeric CS, McDermott CL, Lee DS, Berry SD. Risk Assessment and Prevention of Falls in Older Community-Dwelling adults: a review. JAMA. 2024. https://doi.org/10.1001/jama.2024.1416.
Ang G, Low S, How C. Approach to falls among the elderly in the community. Smedj. 2020;61:116–21.
Iaboni A, Flint AJ. The Complex interplay of Depression and Falls in older adults: a clinical review. Am J Geriatric Psychiatry. 2013;21:484–92.
Hartholt KA, Van Beeck EF, Polinder S, Van Der Velde N, Van Lieshout EMM, Panneman MJM, et al. Societal Consequences of Falls in the older Population: injuries, Healthcare costs, and long-term reduced quality of life. J Trauma: Injury Infect Crit Care. 2011;71:748–53.
Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21:1295–306.
Batchelor FA, Mackintosh SF, Said CM, Hill KD. Falls after Stroke. Int J Stroke. 2012;7:482–90.
Karlsson MK, Vonschewelov T, Karlsson C, Cöster M, Rosengen BE. Prevention of falls in the elderly: a review. Scand J Public Health. 2013;41:442–54.
Stubbs B, Stubbs J, Gnanaraj SD, Soundy A. Falls in older adults with major depressive disorder (MDD): a systematic review and exploratory meta-analysis of prospective studies. Int Psychogeriatr. 2016;28:23–9.
Hung WW, Ross JS, Boockvar KS, Siu AL. Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC Geriatr. 2011;11:47.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–9.
Boyd CM, Ritchie CS, Tipton EF, Studenski SA, Wieland D. From Bedside to Bench: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Comorbidity and multiple morbidity in older adults. Aging Clin Exp Res. 2008;20:181–8.
Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare Population: incidence, Associated factors, and impact on Health Care. Phys Ther. 2009;89:324–32.
Jacob L, Shin JI, Kostev K, Haro JM, López-Sánchez GF, Smith L, et al. Prospective Association between Multimorbidity and Falls and its mediators: findings from the Irish longitudinal study on Ageing. J Clin Med. 2022;11:4470.
Sibley KM, Voth J, Munce SE, Straus SE, Jaglal SB. Chronic disease and falls in community-dwelling canadians over 65 years old: a population-based study exploring associations with number and pattern of chronic conditions. BMC Geriatr. 2014;14:22.
Vu T, Finch CF, Day L. Patterns of comorbidity in community-dwelling older people hospitalised for fall-related injury: a cluster analysis. BMC Geriatr. 2011;11:45.
Feng Z, Glinskaya E, Chen H, Gong S, Qiu Y, Xu J, et al. Long-term care system for older adults in China: policy landscape, challenges, and future prospects. Lancet. 2020;396:1362–72.
Liu J-H, Qian Y-X, Ma Q-H, Sun H-P, Xu Y, Pan C-W. Depressive symptoms and metabolic syndrome components among older Chinese adults. Diabetol Metab Syndr. 2020;12:18.
Liu J-H, Zhang Y-J, Ma Q-H, Sun H-P, Xu Y, Pan C-W. Elevated blood neutrophil to lymphocyte ratio in older adults with cognitive impairment. Arch Gerontol Geriatr. 2020;88:104041.
Yang X-J, Tian S, Ma Q-H, Sun H-P, Xu Y, Pan C-W. Leukocyte-related parameters in older adults with metabolic syndrome. Endocrine. 2020;68:312–9.
Tiseo C, Vacca A, Felbush A, Filimonova T, Gai A, Glazyrina T, et al. Migraine and sleep disorders: a systematic review. J Headache Pain. 2020;21:126.
Carvalho GF, Luedtke K, Bevilaqua-Grossi D. Balance disorders and migraine. Musculoskelet Sci Pract. 2023;66:102783.
Hermenegildo-Lopez Y, Sandoval-Insausti H, Donat-Vargas C, Ramon Banegas J, Rodriguez-Artalejo F, Guallar-Castillon P. General and central obesity operate differently as predictors of falls requiring medical care in older women: a population-based cohort study in Spain. Age Ageing. 2021;50:213–9.
Montero-Odasso M, Speechley M. Falls in cognitively impaired older adults: implications for Risk Assessment and Prevention. J Am Geriatr Soc. 2018;66:367–75.
Pan X-F, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9:373–92.
Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing. 1972;1:233–8.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Chu L, Pei C, Ho M, Chan P. Validation of the abbreviated Mental Test (Hong Kong version) in the elderly medical patient. Hong Kong Med J. 1995;1:207–11.
Sahadevan S, Lim PPJ, Tan NJL, Chan SP. Diagnostic performance of two mental status tests in the older Chinese: influence of education and age on cut-off values. Int J Geriat Psychiatry. 2000;15:234–41.
Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36:539–44.
Zhai Y, Yi H, Shen W, Xiao Y, Fan H, He F, et al. Association of empty nest with depressive symptom in a Chinese elderly population: a cross-sectional study. J Affect Disord. 2015;187:218–23.
Yang W-Y, Li J, Zhao C-H, Qian D-J, Niu Z, Shen W, et al. Population-based assessment of visual impairment among ethnic Dai adults in a rural community in China. Sci Rep. 2016;6:22590.
Prados-Torres A, Poblador-Plou B, Calderón-Larrañaga A, Gimeno-Feliu LA, González-Rubio F, Poncel-Falcó A, et al. Multimorbidity Patterns in Primary Care: Interactions among Chronic Diseases Using Factor Analysis. PLoS ONE. 2012;7:e32190.
Guo X, Tang P, Zhang L, Li R. Tobacco and alcohol consumption and the risk of frailty and falling: a mendelian randomisation study. J Epidemiol Community Health. 2023;77:349–54.
Sun Y, Zhang B, Yao Q, Ma Y, Lin Y, Xu M, et al. Association between usual alcohol consumption and risk of falls in middle-aged and older Chinese adults. BMC Geriatr. 2022;22:750.
Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, Van Den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67:254–66.
Lipsitz LA. Abnormalities in blood pressure homeostasis that contribute to falls in the elderly. Clin Geriatr Med. 1985;1:637–48.
Gangavati A, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P, et al. Hypertension, Orthostatic Hypotension, and the risk of Falls in a Community-Dwelling Elderly Population: the maintenance of Balance, Independent Living, Intellect, and Zest in the Elderly of Boston Study: Hypertension, Orthostatic Hypotension, and Falls. J Am Geriatr Soc. 2011;59:383–9.
Yau RK, Strotmeyer ES, Resnick HE, Sellmeyer DE, Feingold KR, Cauley JA, et al. Diabetes and risk of hospitalized fall Injury among older adults. Diabetes Care. 2013;36:3985–91.
Hewston P, Deshpande N. Falls and Balance impairments in older adults with type 2 diabetes: thinking Beyond Diabetic Peripheral Neuropathy. Can J Diabetes. 2016;40:6–9.
Yano AG, Sheik S, Yu AM, Okuyama A, Takeda K. Effect of Multimorbidity on Fragility fractures in Community-Dwelling older adults: Shimane CoHRE Study. JCM. 2021;10:3225.
Yang F, Kim J, Yang F. Effects of obesity on dynamic stability control during recovery from a treadmill-induced slip among young adults. J Biomech. 2017;53:148–53.
Gupta P, Aravindhan A, Gan ATL, Man REK, Fenwick EK, Mitchell P, et al. Association Between the Severity of Diabetic Retinopathy and Falls in an Asian Population With Diabetes: The Singapore Epidemiology of Eye Diseases Study. JAMA Ophthalmol. 2017;135:1410.
Van Poelgeest EP, Pronk AC, Van Der Rhebergen D. Depression, antidepressants and fall risk: therapeutic dilemmas—a clinical review. Eur Geriatr Med. 2021;12:585–96.
Gambaro E, Gramaglia C, Azzolina D, Campani D, Molin AD, Zeppegno P. The complex associations between late life depression, fear of falling and risk of falls. A systematic review and meta-analysis. Ageing Res Rev. 2022;73:101532.
Schuch F, Vancampfort D, Firth J, Rosenbaum S, Ward P, Reichert T, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord. 2017;210:139–50.
Zia A, Kamaruzzaman SB, Tan MP. Polypharmacy and falls in older people: balancing evidence-based medicine against falls risk. Postgrad Med. 2015;127:330–7.
Chantanachai T, Sturnieks DL, Lord SR, Payne N, Webster L, Taylor ME. Risk factors for falls in older people with cognitive impairment living in the community: systematic review and meta-analysis. Ageing Res Rev. 2021;71:101452.
Sampath D, Sathyanesan M, Newton S. Cognitive dysfunction in major depression and Alzheimer’s disease is associated with hippocampal-prefrontal cortex dysconnectivity. NDT. 2017;Volume 13:1509–19.
Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic Diseases–A systematic review on existing Multimorbidity indices. Journals Gerontol Ser A: Biol Sci Med Sci. 2011;66A:301–11.
Sapkota S, Kobau R, Pastula DM, Zack MM. Close to 1 million US adults aged 55 years or older have active epilepsy—National Health interview Survey, 2010, 2013, and 2015. Epilepsy Behav. 2018;87:233–4.
Przydacz M, Gasowski J, Grodzicki T, Chlosta P. Lower urinary tract symptoms and overactive bladder in a large cohort of older Poles-A Representative Tele-Survey. J Clin Med. 2023;12:2859.
Acknowledgements
We frankly thank all participants and the schools involved in the survey, as well as other staff members on the scene.
Funding
This work was supported by Key medical discipline of Jiangsu Province (No. ZDXK202252).
Author information
Authors and Affiliations
Contributions
Xin-Yi Nie: Visualization, Validation, Writing - Review & Editing. Xing-Xuan Dong: Visualization, Formal analysis, Writing - original draft, Writing - review & editing. Heng Lu: Visualization, Formal analysis, Writing - original draft, Writing - review & editing. Dan-Lin Li: Writing - review & editing. Chun-Hua Zhao: Writing - Review & Editing. Yueqing Huang: Writing - review & editing, Funding. Chen-Wei Pan: Conceptualization, Visualization, Formal analysis, Writing - original draft, Writing - review & editing, Validation.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study followed the tenets of the Helsinki Declaration and ethics approval was obtained from the Institutional Review Board of the Soochow University. Written informed consent was obtained from each participant at the recruitment stage of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest in relation to the subject of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nie, XY., Dong, XX., Lu, H. et al. Multimorbidity patterns and the risk of falls among older adults: a community-based study in China. BMC Geriatr 24, 660 (2024). https://doi.org/10.1186/s12877-024-05245-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05245-1