Abstract
Background
“Multidisciplinary fast-track” (MFT) care can accelerate recovery and improve prognosis after surgery, but whether it is effective in older people after hip fracture surgery is unclear.
Methods
We retrospectively compared one-year all-cause mortality between hip fracture patients at least 80 years old at our institution who underwent hip fracture surgery between January 2014 and December 2018 and who then received MFT or conventional care. Multivariable regression was used to assess the association between MFT care and mortality after adjustment for confounders.
Results
The final analysis included 247 patients who received MFT care and 438 who received conventional orthopedic care. The MFT group showed significantly lower one-year mortality (8.9% vs. 14.4%, P = 0.037). Log-rank testing of Kaplan-Meier survival curves confirmed the survival advantage. However, the two groups did not differ significantly in rates of mortality during hospitalization or at 30 or 90 days after surgery. Regression analysis confirmed that MFT care was associated with lower risk of one-year mortality (hazard ratio [HR] 0.47, 95% confidence interval [CI] 0.281–0.788, P = 0.04), and the survival benefit was confirmed in subgroups of patients with anemia (HR 0.453, 95% CI 0.268–0.767, P = 0.003) and patients with American Society of Anesthesiologists grade III (HR 0.202, 95% CI 0.08–0.51, P = 0.001).
Conclusions
MFT care can reduce one-year mortality among hip fracture patients at least 80 years old. This finding should be verified and extended in multi-center randomized controlled trials.
Similar content being viewed by others
Introduction
By 2050, the global incidence of hip fractures is expected to exceed 6 million per year [1], and such fractures are associated with high mortality and morbidity, especially among the older people [1,2,3,4,5,6,7]. Older people are at far greater risk than young people of suffering hip fractures after falls, slips or minor trauma, which reflects loss of bone mass and muscle strength around hip joints during aging [8, 9]. Numerous studies point to the importance of surgical intervention as early as possible after hip fracture in order to optimize prognosis, particularly for patients at least 80 years old [6,7,8,9].
Consensus guidelines [7, 10] have begun recommending multidisciplinary collaborative diagnosis and perioperative management of hip fracture patients in order to accelerate surgical intervention and improve prognosis [11,12,13,14,15,16,17,18]. The term “multidisciplinary fast-track” (MFT) is often used to refer to the close cooperation of various clinical departments to diagnose, treat and rehabilitate patients after medical interventions [7, 10, 19]. While MFT care has proven effective at improving prognosis for patients undergoing various types of surgery [12, 13, 15], studies have reported mixed results for its effects on mortality among older people after hip fracture surgery [13, 17, 20, 21]. One reason for the mixed results may be that those studies examined a wide age range of patients, from 60 years and older.
We examined here whether MFT care can improve mortality specifically among patients 80 years and older after hip fracture surgery. We also wished to identify risk factors for worse survival among such patients, regardless of whether they received MFT or conventional orthopedic care.
Materials and methods
This single-center retrospective cohort study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (approval I2019001002), which waived the requirement for informed consent.
Patients
We retrospective analyzed medical records for patients who underwent hip fracture surgery at our medical center between January 1, 2014 and December 31, 2018 and who were at least 80 years old at the time of surgery. We excluded patients who had pathological or repeat fractures, multiple injuries or fractures, or high-energy trauma such as from an automobile accident.
Perioperative management
Patients who were enrolled before May 2017 received conventional orthopedic care, i.e. the procedures for diagnosis, treatment and rehabilitation routinely applied to older people with hip fracture at our institution. Patients were examined and admitted to the orthopedic ward after diagnosis of hip fracture, where they underwent additional preoperative testing. If their condition was complex, specialists were consulted. This preoperative examination and assessment might take several days, reflecting the large patient volume at our medical center. As a result, patients typically underwent surgery more than 5 days after admission.
Patients enrolled from May 2017 onwards received MFT care. After admission to the emergency room, patients were examined within 24 h by a multidisciplinary team drawn from at least three departments, which always included the Departments of Emergency Medicine, Orthopedic Trauma, and Anesthesiology. The team focused on stabilizing and optimizing the patient’s preoperative condition and, if appropriate, scheduling surgery within 72 h of admission. Surgeries were conducted in the first available operating room, after which patients received early nutritional support and rehabilitation.
Data collection and outcomes
Clinical data were extracted from the Electronic Medical Record System and “Do care” Anesthesia Information System at our hospital. Preoperative data included demographics, laboratory tests, American Society of Anesthesiologists (ASA) grade, fracture type, comorbidities, and Charlson comorbidity index [22]. Intra-operative data included the type and duration of surgery, type of anesthesia and volume of blood loss. Postoperative data included survival up to 12 months, postoperative complications (new-onset pneumonia, heart failure, deep vein thrombosis, pulmonary embolism), admission to the intensive care unit, length of hospital stay and total treatment costs. Patients were followed up by telephone for at least one year after surgery, and they were considered lost to follow-up if they or their family members could not be reached by telephone.
The primary outcome in this study was all-cause mortality within one year of surgery. Secondary outcomes included all-cause mortality during hospitalization as well as at 30 and 90 days after surgery, postoperative complications, postoperative admission to the intensive care unit, length of hospital stay, and total treatment costs.
Statistical analysis
We estimated the minimal size of the MFT and conventional groups to be 215 in order to detect a difference of 12% in one-year postoperative mortality with statistical power of 90% at an alpha level of 5%. The difference of 12% was based on a previous study of older hip fracture people who received MFT or usual care [23].
Continuous data in this study showed a skewed distribution, so they were reported as median (interquartile range), and differences between the two groups were assessed for significance using non-parametric testing. Categorical data were reported as n (%), and intergroup differences were assessed using the chi-squared or Fisher’s exact test.
One-year survival curves were generated using the Kaplan-Meier method and compared using the log-rank test. Regression analysis was performed to identify variables associated with one-year mortality: variables that were associated with P < 0.1 in univariate regression were then included in multivariate Cox regression to control confounding. Results were reported, where appropriate, as hazard ratios (HRs) or odds ratios (ORs) and associated 95% confidence intervals (CIs). Regression was repeated for subgroups of patients stratified by sex, anemia, and ASA grade.
All statistical analyses were performed using SPSS 25.0 (IBM, Chicago, IL, USA) or R 4.1.0 (https://www.r-project.org). Results associated with P < 0.05 were considered significant.
Results
Of the 891 patients who underwent hip fracture surgery at our medical center during the enrollment period, we included 685, comprising 247 in the MFT group and 438 in the conventional group (Fig. 1). The two groups did not differ significantly in age or sex, with women accounting for more than 74% of patients in each group (Table 1). The two groups did not differ significantly in most other clinicodemographic variables examined, except that the MFT group showed significantly higher prevalence of pneumonia (39.3% vs. 26.7%, P = 0.001) and chronic obstructive pulmonary disease (9.3% vs. 3.9%, P = 0.004). A significantly larger proportion of the MFT group received regional anesthesia.
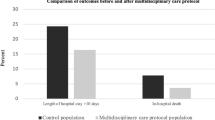
The MFT group showed significantly lower all-cause mortality at one year (8.9% vs. 14.4%, P = 0.037; Table 2), which was confirmed by Kaplan-Meier analysis (chi-squared = 4.12, P = 0.042; Fig. 2). However, the two groups did not differ significantly in rates of mortality during hospitalization or at 30 or 90 days after surgery.
The MFT group showed a significantly lower rate of admission to the intensive care unit after surgery (4.9% vs. 10.7%, P = 0.009) and shorter intervals until surgery and discharge, leading to lower total treatment costs (Table 2). The two groups did not differ significantly in incidence of new-onset pneumonia, heart failure, deep vein thrombosis or pulmonary embolism.
Univariate regression identified 17 clinicodemographic variables that showed a P < 0.1 association with one-year all-cause mortality, of which 15 also emerged as significant in bivariate analysis (Table 3): age, sex, body mass index, ASA grade, hemoglobin level, albumin level, creatinine level, preoperative comorbidities, Charlson comorbidity index, fracture type, type and duration of surgery, type of anesthesia, intraoperative blood loss and MFT care. Based on the literature [7, 16, 22], we included the following 10 variables in multivariate logistic regression (Table 4): age, sex, pneumonia, hemoglobin level, albumin level, ASA grade, type of anesthesia, duration of surgery, Charlson comorbidity index and MFT care. Regression analysis linked MFT to significantly lower risk of one-year all-cause death after controlling for the other variables in the model (HR 0.47, 95% CI 0.281–0.788, P = 0.004). Across all patients in the study, risk of one-year all-cause mortality was significantly lower among women than men (HR 0.623, 95% CI 0.393–0.987, P = 0.044), higher among those with ASA grades III-IV than those with grades I-II (HR 6.238, 95% CI 3.649–10.664, P < 0.001), and lower among those with normal hemoglobin levels than among those with anemia (HR 0.985, 95% CI 0.973–0.997, P = 0.014), after controlling for the other variables in the model (Table 5).
After adjusting for other factors, MFT care was associated with significantly lower risk of one-year all-cause mortality in subgroups of patients with anemia (HR 0.453, 95% CI 0.268–0.767, P = 0.003) or ASA grade III (HR 0.202, 95% CI 0.08–0.51, P = 0.001).
Discussion
Our single-center study suggests that MFT perioperative management of hip fracture patients at least 80 years old can significantly reduce risk of postoperative admission to the intensive care unit, shorten hospital stay, reduce medical costs and reduce risk of one-year all-cause mortality. We observed trends toward lower rates of mortality during hospitalization as well as at 30 and 90 days after surgery with MFT care, but these trends did not achieve statistical significance.
Our results support previous studies that found MFT care to shorten hospitalization and accelerate recovery among geriatric patients covering a wide age range from 60 years and older who underwent.hip fracture surgery [11,12,13,14,15,16,17,18]. At least in the present study, the advantages of MFT care are likely due in part to clinicians’ efforts to perform surgery within 72 h after admission. Delaying hip fracture surgery, especially among older people, may increase risk of postoperative mortality [24].
Previous work concurs with our finding of no clear benefit of MFT care on short-term survival [11, 14, 15, 25]. This may reflect that the primary risk factors for mortality soon after hip fracture surgery are age, sex, and preoperative complications [9, 26]. A meta-analysis concluded that treatment pathway was not significantly associated with short-term mortality of older people with hip fracture [27].
We found that our male older people, regardless of whether they received MFT or conventional care, were at higher risk of one-year mortality than female patients, which is consistent with previous studies [28,29,30]. This may reflect the greater prevalence of pneumonia, chronic obstructive pulmonary disease, smoking, and drinking among men [30].
We found that patients with anemia were at greater risk of one-year mortality than those with normal hemoglobin levels, regardless of whether they received MFT or conventional care. Consistently, previous work showed that normalizing low hemoglobin levels preoperatively can reduce the risk of one-year all-cause mortality in younger and older hip fracture patients [25, 26]. The present study and previous work highlight the need to optimize perioperative management of hemoglobin and nutrition for older people, especially those with known risk factors of anemia, such as metabolic disorders, blood loss, and chronic comorbidities [27].
We found that patients with ASA grades III-IV were at greater risk of one-year mortality than those with milder ASA grades, regardless of whether they received MFT or conventional care. This finding concurs with previous work identifying ASA grade as a predictor of postoperative mortality in older people with hip fractures [23, 31,32,33]. Our observation of ASA grade III as a “threshold” in risk of one-year mortality should be interpreted with caution, given that 70% of our study participants belonged to that grade. If this threshold can be verified in further studies, it may mean that patients with severe systemic comorbidities (ASA > III) are less likely than other patients to benefit from MFT care. This possibility should be explored in future work.
The present study focused on patients at least 80 years old, and its findings echo previous work on the benefits of MFT care for hip fracture patients at least 65 years old. In contrast to younger patients, our patients at least 80 years old were more likely to have life-threatening comorbidities or to suffer postoperative complications. One study has suggested that the risk of postoperative death among older people with hip fracture increases by 6% with every year of aging [23]. The similarities between patients below and above 80 years is interesting given that susceptibility to traumatic stress, time needed to recover from surgery, and overall risk of mortality increase strongly with age [34], while organ function and resilience decline [18, 35,36,37].
Our findings should be interpreted with caution given several limitations. First, the retrospective nature of the study prevented us from assessing the potential influence of events before admission or after discharge on postoperative mortality. In addition, nearly 90% of study participants had a Charlson cormobidity index of 0 or 1, so our results may not be generalizable to frailer patient populations. These low indices may underestimate actual comorbidity in our sample because certain conditions may not have been recorded appropriately. Third, we considered MFT care as a “whole” in our study without attempting to identify the influence of specific measures or practices on mortality. Given the lack of standardization about MFT care around the world, future work should examine particular MFT components that may be more effective at improving prognosis. Our results should be verified in larger, multi-center studies.
Conclusions
MFT perioperative care can improve survival among hip fracture patients at least 80 years old. If these findings can be verified in larger studies, they argue for continuing research into MFT protocols for older people undergoing hip fracture surgery and for expanding such research to other types of orthopedic surgery.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- CCI:
-
Charlson comorbidity index
- CI:
-
Confidence interval
- COC:
-
Conventional orthopedic care
- HR:
-
Hazard ratio
- MFT:
-
Multidisciplinary fast-track
References
Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49(8):1458–60.
Jürisson M, Pisarev H, Kanis J, Borgström F, Svedbom A, Kallikorm R, et al. Quality of life, resource use, and costs related to hip fracture in Estonia. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2016;27(8):2555–66.
Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A, et al. Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2017;28(10):2791–800.
Ryan DJ, Yoshihara H, Yoneoka D, Egol KA, Zuckerman JD. Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma. 2015;29(8):343–8.
Lieten S, Herrtwich A, Bravenboer B, Scheerlinck T, Van Laere S, Vanlauwe J. Analysis of the effects of a delay of surgery in patients with hip fractures: outcome and causes. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2021;32(11):2235–45.
Association of Anaesthetists of Great Britain and Ireland, Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, et al. Management of proximal femoral fractures 2011: Association of anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67(1):85–98.
Bhandari M, Swiontkowski M. Management of Acute Hip fracture. N Engl J Med. 2017;377(21):2053–62.
Zebaze RMD, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M, Price RI, et al. Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet Lond Engl. 2010;375(9727):1729–36.
Zhang YW, Lu PP, Li YJ, Dai GC, Chen MH, Zhao YK, et al. Prevalence, characteristics, and Associated Risk factors of the Elderly with hip fractures: a cross-sectional analysis of NHANES 2005–2010. Clin Interv Aging. 2021;16:177–85.
Griffiths R, Babu S, Dixon P, Freeman N, Hurford D, Kelleher E, et al. Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia. 2021;76(2):225–37.
Fan J, Lv Y, Xu X, Zhou F, Zhang Z, Tian Y, et al. The Efficacy of Multidisciplinary Team Co-management Program for Elderly patients with intertrochanteric fractures: a retrospective study. Front Surg. 2022;8:816763.
Jiang M, Liu S, Deng H, Liang X, Bo Z. The efficacy and safety of fast track surgery (FTS) in patients after hip fracture surgery: a meta-analysis. J Orthop Surg. 2021;16(1):162.
Sura-amonrattana U, Tharmviboonsri T, Unnanuntana A, Tantigate D, Srinonprasert V. Evaluation of the implementation of multidisciplinary fast-track program for acute geriatric hip fractures at a University Hospital in resource-limited settings. BMC Geriatr. 2021;21(1):548.
Liu G, Yang M, Zhu S, Zhang P, Wang G, Wang M, et al. Effect of Orthogeriatric Co-management on geriatric hip fractures in China. Orthop Surg. 2022;14(4):671–7.
Reguant F, Arnau A, Lorente JV, Maestro L, Bosch J. Efficacy of a multidisciplinary approach on postoperative morbidity and mortality of elderly patients with hip fracture. J Clin Anesth. 2019;53:11–9.
Kulshrestha V, Sood M, Kumar S, Sharma P, Yadav YK. Outcomes of fast-track Multidisciplinary Care of Hip fractures in veterans: a geriatric hip fracture program report. Clin Orthop Surg. 2019;11(4):388.
Shigemoto K, Sawaguchi T, Horii T, Goshima K, Iwai S, Higashikawa T, et al. Multidisciplinary care model for geriatric patients with hip fracture in Japan: 5-year experience. Arch Orthop Trauma Surg. 2022;142(9):2205–14.
Boddaert J, Raux M, Khiami F, Riou B. Perioperative management of elderly patients with hip fracture. Anesthesiology. 2014;121(6):1336–41.
Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–7.
Fu M, Guo J, Zhang Y, Zhao Y, Zhang Y, Hou Z, et al. Effect of integrated management bundle on 1-year overall survival outcomes and perioperative outcomes in super elderly patients aged 90 and over with hip fracture: non-concurrent cohort study. BMC Musculoskelet Disord. 2022;23(1):778.
Maher S, Moore Z, Avsar P, Patton D. What is the impact of a fast-track pathway on length of stay for adult patients with a hip fracture? A systematic review. Arch Orthop Trauma Surg. 2022;142(12):3803–16.
Charlson ME, Carrozzino D, Guidi J, Patierno C. Charlson Comorbidity Index: a critical review of Clinimetric Properties. Psychother Psychosom. 2022;91(1):8–35.
Folbert EC, Hegeman JH, Vermeer M, Regtuijt EM, van der Velde D, Ten Duis HJ, et al. Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2017;28(1):269–77.
Maheshwari K, Planchard J, You J, Sakr WA, George J, Higuera-Rueda CA, et al. Early surgery confers 1-Year Mortality Benefit in hip-fracture patients. J Orthop Trauma. 2018;32(3):105–10.
Manosroi W, Atthakomol P, Isaradech N, Phinyo P, Vaseenon T. Preoperative correction of low hemoglobin levels can reduce 1-Year all-cause mortality in osteoporotic hip fracture patients: a retrospective observational study. Clin Interv Aging. 2022;17:165–73.
Atthakomol P, Manosroi W, Phinyo P, Pipanmekaporn T, Vaseenon T, Rojanasthien S. Prognostic factors for all-cause Mortality in Thai patients with fragility fracture of hip: comorbidities and laboratory evaluations. Med Kaunas Lith. 2020;56(6):E311.
Stauder R, Valent P, Theurl I. Anemia at older age: etiologies, clinical implications, and management. Blood. 2018;131(5):505–14.
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2009;20(10):1633–50.
Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, Quirós Donate FJ, Peña M, Alonso-Blas C, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg. 2019;14(1):203.
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing. 2010;39(2):203–9.
Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17(1):53–6.
Chiang MH, Huang YY, Kuo YJ, Huang SW, Jang YC, Chu FL, et al. Prognostic factors for mortality, activity of Daily Living, and quality of life in Taiwanese older patients within 1 year following hip fracture surgery. J Pers Med. 2022;12(1):102.
Araiza-Nava B, Méndez-Sánchez L, Clark P, Peralta-Pedrero ML, Javaid MK, Calo M, et al. Short- and long-term prognostic factors associated with functional recovery in elderly patients with hip fracture: a systematic review. Osteoporos Int. 2022;33(7):1429–44.
Lewis MC, Abouelenin K, Paniagua M. Geriatric trauma: special considerations in the Anesthetic Management of the Injured Elderly Patient. Anesthesiol Clin. 2007;25(1):75–90.
Lewis SK, Nachun D, Martin MG, Horvath S, Coppola G, Jones DL. DNA methylation analysis validates Organoids as a viable model for studying human intestinal aging. Cell Mol Gastroenterol Hepatol. 2020;9(3):527–41.
Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–17.
Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5(7):374–81.
Acknowledgements
The authors acknowledge the staff in this study for their collaboration involved in this work.
Funding
This trial is supported in part by grants from the National Clinical Key Specialty Construction Project of China 2021(2021-LCZDZK-01), National Natural Science Foundation of China (NSFC)“The Mechanism of ZNF382 Regulation in Neuropathic Pain in the Dorsal Root Ganglion” (number: 82071227). The funding agency has no infuence on study design, data collection, data analysis, data interpretation, manuscript writing, or publication decisions.
Author information
Authors and Affiliations
Contributions
Y. Z. and M. L. wrote the manuscript. M.Y. and B. Z. revised the manuscript. Y. Y and G. L. contributed to the methodology. Z. C. and Y. Y. collected data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All analyses of human data conducted in this study were approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. We use the medical record data of our medical unit to conduct retrospective research that does not involve personal privacy and commercial interests.The basic information and data used in the study come from previous hospitalized patients in our hospital, and the informed consent of the subjects could not be obtained objectively. The Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine agreed to exempt informed consent (Approval number: I2019001002).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhong, Y., Liu, M., Cheng, Z. et al. “Multidisciplinary fast-track” care can significantly reduce risk of mortality among hip fracture patients at least 80 years old: a single-center retrospective study. BMC Geriatr 24, 592 (2024). https://doi.org/10.1186/s12877-024-05183-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05183-y