Abstract
Introduction
Anaemia is a disease of public health importance with multi-causal pathways. Previous literature suggests the role of indoor air pollution (IAP) on haemoglobin levels, but this has been studied less due to logistic constraints. A high proportion of the population in developing countries, including India, still depends on unclean fuel, which exacerbates IAP. The objective was to study the association between anaemia and IAP among the older Indian adult population (≥ 45 years) as per gender.
Methods
Our study analysed the nationally representative dataset of the Longitudinal Ageing Study in India (LASI 2017–18, Wave-1). We have documented the association of anaemia (outcome variable) with IAP (explanatory variable). To reduce the confounding effects of demographic and socioeconomic; health related and behavioural covariates; propensity score matching (PSM) was conducted. Nested multilevel regression modelling was conducted. States and union territories were categorised cross tabulated as low, middle and high as per anaemia and IAP exposure. P value < 0.05 was considered statistically significant. SATA version 17 was used for analysis.
Results
More than half (52.52%) of the participants were exposed to IAP (male (53.55%) > female (51.63%)). The odds of having anaemia was significantly 1.19 times higher (AOR 1.19 (1.09–1.31)) among participants using unclean/ solid fuel. The adjusted odds were significantly higher among participants exposed to pollution-generating sources (AOR 1.30; 1.18–1.43), and household indoor smoking (AOR 1.17 (1.07–1.29). The odds of having anaemia were significantly higher (AOR 1.26; 1.15–1.38) among participants exposed to IAP, which was higher in males (AOR 1.36; 1.15–1.61) than females (AOR 1.21; 1.08–1.35). Empowered Action Group (EAG) states like Uttar Pradesh, Chhattisgarh, Madhya Pradesh, Bihar had both high anaemia and IAP exposure.
Conclusion
This study established the positive association of anaemia with indoor air pollution among older Indian adults through a nationally representative large dataset. The association was higher among men. Further research is recommended to understand detailed causation and to establish temporality. It is a high time to implement positive intervention nationally to decrease solid/ unclean fuel usage, vulnerable ventilation, indoor smoking, IAP and health hazards associated with these with more focused actions towards EAG states.
Similar content being viewed by others
Introduction
Anaemia is essentially a homeostatic imbalance in the hemoglobin concentration (< 12 g/dL in women and 13 g/dL in men) whereby the production of erythrocytes is outpaced by destruction or loss of erythrocytes. It leads to poor health, economic loss and social burden [1]. It is the result of a wide variety of causes that can be isolated, but often they coexist. Globally, the most common cause of nutrient deficiency anaemia is due to iron deficiency, although other conditions, such as folate, vitamin B12 and vitamin A deficiencies, chronic inflammation, parasitic infections, and inherited disorders can cause anaemia [2].
Prevalence of anaemia is higher in developing countries, south Asian countries contributing 37.5% of global anaemia [3]. Poverty, inadequate diet, diseases, pregnancy/lactation and poor access to health services are some of the key factors contributing to the high burden [4]. Globally prevalence of anaemia was 12–17% among older adults (≥ 65 years); 40% hospitalised and 47% patients in nursing home had anaemia [5]. Given that the world's population is getting older due to demographic shifts, the overall burden of disease related to anaemia among the elderly is probably only going to increase [6].
The emergence and advancement of anaemia may be influenced by common environmental exposures, such as air pollution. Numerous extremely common chronic diseases, such as respiratory, mental, and cardiovascular conditions, are recognised to be at risk due to ambient air pollution [7]. In developing nations, ambient air pollution has had a severe negative influence on public health [8]. Industrialisation in these areas, propelled by economic expansion, has resulted in significant rises in air pollution levels, frequently an order of magnitude more than those found in industrialised nations. The latter has exacerbated bad health outcomes and increased the risk to human life [9]. There are few studies on the relationship between air pollution and anaemia, and the majority of the earlier studies concentrated on the population of children or short-term exposures [10,11,12]. There were very few study showing among older adults (≥ 45 years) [13, 14]. Hence, we have conducted this study to show the association of anaemia with indoor air pollution among older Indian adults (≥ 45 years).
Objective
To determine the association with anaemia with Indoor air pollution
-
among older Indian population (≥ 45 years).
-
among male and female older Indian population (≥ 45 years).
Methodology
Data source: LASI-1st wave is a longitudinal survey with a national representation that intends to collect detailed information on the psychological, social, economic, and health aspects of ageing in India from all the states and union territories. It was developed to fill the information vacuum regarding thorough and internationally comparable survey data on India's ageing population. The study, which is the biggest of its kind in the world and the first of its kind in India, evaluates the scientific evidence in the context of variables like demographics, household economic status, chronic health conditions, symptom-based health conditions, functional health, mental health (cognition and depression), biomarkers, healthcare utilisation, family and social networks, social welfare programmes, employment, retirement, satisfaction, and life expectations. The survey intends to follow a representative sample of the older adult population every two years for the following 25 years, with a revised sample size to account for attrition due to death, migration, non-reachable, and non-response [15]. The funding agencies were National Institute on Ageing, the Government of India's Ministry of Health and Family Welfare, and the United Nations Population Fund. The University of Southern California, the International Institute for Population Sciences, and the Harvard T.H. Chan School of Public Health were the contributors.
Study population
A total of 73,396 adult Indians were surveyed from during April 2017-December 2018 (Sikkim: 2020–2021). Out of them, 65,295 participants were included for the present study. Details of study flow and sample selection with missing data handling (row wise complete deletion/ complete case analysis) were documented in Fig. 1.
Study variables
Outcome variable
The outcome variable of choice was anaemia. Self-reported anaemia prevalence was obtained by questioning ‘In the past 2 years, have you had anaemia?’ Answering ‘yes’ was considered as anaemia present.
Explanatory variables
Participants exposed to indoor air pollution (IAP) was the explanatory variable of choice. IAP includes contamination of the air from physical, chemical, and biological sources. A distinct component on IAP was surveyed as part of the LASI study. Six questions from the LASI survey were used to calculate IAP. There were two questions concerning the fuel utilised for cooking and other purposes:
(i)” What is your main source of cooking fuel?” and.
(ii) “What are those other sources of fuel used for other purposes (such as boiling water for bathing, lighting, etc.)?” (Responses: Liquefied Petroleum Gas (LPG), Biogas, Kerosene, Electric, Charcoal/Lignite/Coal, Crop residue, Wood/Shrub, Dung cake, do not cook at home, Other, please specify). ‘Fuel type’ was generated considering LPG, Biogas, and Electric methods as clean fuels and the rest as unclean or solid fuels. ‘Pollution generating source’ was generated from type of oven used: (iii) “In this household, is food mostly cooked on a mechanical stove, on a traditional chullah or over an open fire?” (Responses: Mechanical Stove/Improved cook stove, Traditional chullah, Open fire, Other, please specify). Traditional chullah and opened fire was taken as the higher pollution generating source. Next two questions were about place of cooking and ventilation: (iv) “Is the cooking usually done in the house, in a separate building, or outdoors?” (Responses: In the house, In a separate building, Outdoors, Other, please specify); (v) “Is the cooking mainly done under a traditional chimney, exhaust fan, electric chimney or near window/door?” (Responses: Traditional chimney, Electric chimney, Exhaust fan, Near window/door, None). No ventilation with in-house cooking was considered as vulnerable ventilation. Next question was on ‘Household Indoor Smoking’: (vi) “Does any usual member of your household smoke inside the home?”(Responses: Yes, No). Thus, all six factors were used to generate ‘Indoor Air Pollution’: exposed (Participants using unclean/ solid fuel for cooking and others by utilising traditional chullah or open fire and inhouse cooking without any ventilation system along with presence of indoor smoking.) and non-exposed participants. Thus ‘fuel type’, ‘pollution generating source’, ‘vulnerable ventilation’, ‘household indoor smoking’ and’indoor air pollution’ were considered as explanatory variables.
Covariates
These variables were categorised into demographic and socioeconomic, health related and behavioural factors. Under demographic and socioeconomic factors, we have included- age group (45–64, ≥ 65 years), gender (male, female), education (illiterate, less than primary. primary completed, middle completed, secondary school, higher secondary, and Diploma/ graduate), residence (rural, urban), marital status (unmarried, married/ in live-in, Widow/ separated/ divorced), MPCE (monthly per capita expenditure- poorest, poorer, middle, richer, richest) quintile, health insurance (no, yes), occupation (unemployed, professional and semi-professional- ‘legislators and senior officials, professionals, technicians and associate professionals’, clerical and skilled- ‘clerks, service workers and shopkeepers, skilled agriculture and fishery workers, craft and related trade worker, plant and machine operator’, unskilled). Under health-related factors, we have included- physical activity (everyday, once per week, 1–3 times per week, once per month, never), self-rated health (excellent, very good, good, fair, poor) and multimorbidity. Following chronic morbidities were included- hypertension, diabetes, cancer, chronic lung diseases (e.g.- chronic obstructive pulmonary disease, asthma, chronic bronchitis, other chronic lung problems), chronic heart disease (e.g.- congestive heart failure, myocardial infarction, heart attack, other chronic heart diseases), stroke, musculoskeletal disorder (MSD e.g.- rheumatism, arthritis, osteoporosis, other chronic joint or bone disorders), dyslipidaemia (high cholesterol), thyroid disorders, Chronic renal failure, visual impairment and hearing impairment. Interviewer asked related question about chronic health conditions/ morbidities with dichotomous answers (no/ yes)- “Has any health professional ever diagnosed you with the following chronic conditions or diseases?” Participants having at least two chronic health conditions were described as multimorbidity. Under behavioural factors, we have included- tobacco abuse (no, yes) and alcohol abuse (no, yes).
Statistical analysis
Data was analysed in Stata version 17 (StataCorp. 2017. Stata Statistical Software: Release 17. College Station, TX: StataCorp LP.). The characteristics of the participants were described as mean (standard deviation) for continuous variable frequencies and percentages for categorical variables. Individual sample weights were considered during the analysis. Chi-square p-value was estimated. Indian states and union territories were categorised into low (0 to 33rd percentile), middle (34 to 66th percentile) and high (67 to 100th percentile) as per anaemia and indoor air pollution each. We have produced Indian map to document these categories with Microsoft excel. We have further cross tabulated them to obtain common categories.
To reduce the confounding effects of covariates, we have used propensity score matching (PSM). We have used nested multilevel modelling to show the association between anaemia and IAP. We have used total 4 models. In the Model-1, we have included IAP. In the Model-2, Model-3 and Model-4; we have subsequently added demographic and socioeconomic, health related and behavioural factors, respectively after assessing the multicollinearity among explanatory variables using the VIF (Variance inflation factor), and variables > 5 indicate a high correlation and were omitted. (Self-related health and marital status had VIF > 5. (Supplementary Table S1)) Hence, all the covariates except these two were included in the final association. We have also documented pseudo R2, log-likelihood, likelihood ratio, AIC (Akaike Information Criterion) and BIC (Bayesian Information Criterion) to evaluate the best model. We have then documented the association as per gender. We reported state wise variations of this association. P-value < 0.05 were considered as statistically significant.
Ethical statement
Dataset is freely available in the public domain, ethical approval for the present study was not deemed necessary. However, the ethical approval to conduct LASI was given by the Indian Council of Medical Research's (ICMR) Central Ethics Committee on Human Research (CECHR) [15].
Results
The mean (SD) age of the participants were 60.27 (10.77) years. Around 50.82% of participants were illiterate, which was higher in females (65.32%). Around 69.75% of participants resided in the rural area. Almost three-fourth of the participants were married. Only 2.31% of participants had health insurance. Almost half of the participants (49.90%) were unemployed, which was higher among females (67.11%). Almost one-fourth (25.07%) of the participants exercised every day, which was higher among males (32.92%). Multimorbidity was 36.55% overall, higher among females (38.42%). Around 37.26% and 15.00% of participants had a history of tobacco abuse and alcohol abuse, respectively, which was more in men in both cases. (Table 1).
Unclean/ solid fuel usage was 38.35% overall. Higher vulnerable ventilation was seen among 18.09% participants. Around 48.90% and 25.00% participants were exposed to pollution generating source and household indoor smoking, respectively. More than half (52.52%) of the participants were exposed to the indoor air pollution (IAP). All the above were higher among males except in using unclean/ solid fuel and higher vulnerable ventilation. (Table 2).
IAP was highest in Meghalaya (79.43%) and lowest in Goa (16.46%). Self-reported anaemia was present among 2962 (4.54%) participants. Anaemia was more prevalent among female (5.75%) than male (3.12%) participants. The anaemia prevalence was highest in Punjab (8.98%) and lowest in Puducherry (0.12%) (Supplementary Table S2). Figure 2 represents the categorisation of Indian states and union territories as per anaemia and IAP. Central states like Uttar Pradesh, Chhattisgarh, Madhya Pradesh, Bihar had both high anaemia and IAP. In the contrary both low anaemia and IAP was documented in Puducherry, Sikkim, Telangana, Daman and Diu, Tamil Nadu. Though the IAP was high in Nagaland, Meghalaya, Tripura, West Bengal; still the anaemia prevalence was low. Though the LAP was low in Goa, Delhi, Karnataka; anaemia was high. (Table 3).
The coefficient for the estimated treatment effect of IAP over anaemia across population (ATE) is 0.0083. After adjusting for covariates, individuals exposed to indoor air pollution (IAP) have significantly increased risk of anaemia compared to non-exposed individuals. The estimated effect size is approximately 0.83% higher odds of having anaemia in the participants exposed to IAP. (Table 4).
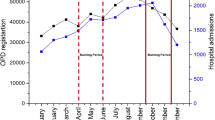
We have reported the association of anaemia and IAP using nested multilevel modelling using 4 models. Out of all, Model-4 was the best with highest pseudo R2 and log-likelihood; and lowest AIC (Akaike Information Criterion) and BIC (Bayesian Information Criterion) values with statistically significant p-value. The odds of having anaemia was significantly 1.19 times higher (AOR 1.19 (1.09–1.31)) among participants using unclean/ solid fuel than clean fuel; which was higher among male (AOR 1.42 (1.20–1.67)). The odds of having anaemia was significantly higher (AOR 1.30 (1.18–1.43)) among participants exposed to pollution generating source, which was higher in male (1.58 (1.33–1.88)). The odds was significantly higher (AOR 1.17 (1.07–1.29)) among participants exposed to household indoor smoking, which was higher in female (1.21 (1.08–1.35)). The odds of having anaemia was significantly 1.26 times higher (AOR 1.26 (1.15–1.38)) among participants exposed to indoor air pollution, which was higher in male (1.36 (1.15–1.61)) than female (1.21 (1.08–1.35)). (Fig. 3, Tables 5 and 6).
Females had 1.86 times (AOR 1.86 (1.67–2.08)) higher adjusted odds of having anaemia. With increase in the educational status, the odds of having anaemia decreased. Participants residing in rural area had 1.47 times (AOR 1.47 (1.33–1.62)) higher odds of having anaemia. The odds of having anaemia was highest (AOR 1.37 (1.19–1.57)) among poorest participants. Participants having multimorbidity (AOR 1.86 (1.71–2.03)) and history of tobacco abuse (AOR 1.23 (1.12–1.35)) had significantly higher odds of having anaemia as per Model-4. (Fig. 3) Chhattisgarh (AOR 3.30 (1.59–6.84)), Maharashtra (AOR 1.93 (1.29–2.90)) and Odisha (AOR 1.88 (1.13–3.11)) had significantly higher odds of anaemia associated with IAP exposure. (Fig. 4).
Discussion
This study is one of the very few studies to show the association of anaemia with indoor air pollution among older Indian adult population with a significantly large nationally representative dataset. There are several key findings of the study.
The odds of having anaemia was significantly higher among participants exposed to pollution generating source (AOR 1.30 (1.18–1.43)), household indoor smoking (AOR 1.17 (1.07–1.29. The odds was significantly 1.26 times higher (AOR 1.26 (1.15–1.38)) among participants exposed to indoor air pollution, which was higher in male (1.36 (1.15–1.61)) than female (1.21 (1.08–1.35)). Similar results were describes by studies conducted by Kelly et al. and Elbarbary et al. [13, 14]. The potential cause might be due to prolonged exposure to indoor pollution which might cause oxidative stress, inflammation, decrease absorption of iron and changes in blood parameters, such as haemoglobin levels. Pollutants present in indoor air pollution might cause haemolysis. Breathing in tiny particles (PM2.5) and gaseous pollutants can make your body more inflamed and affect how your bone marrow works [16, 17], especially if you already have conditions like diabetes or obesity. Our study documented that, the participants having multimorbidity (AOR 1.86 (1.71–2.03)) had significantly higher odds of having anaemia. Most studies have looked at how these pollutants affect inflammation in the short term [18,19,20], but recent research suggests they could keep causing inflammation over a long time [21,22,23]. This could lead to a chain reaction in your body: it might make human body to produce less of a hormone called erythropoietin, make blood cells less responsive to this hormone, and increase the levels of a protein that controls iron in the body [24, 25]. All of these things combined could mean that body makes fewer red blood cells, leading to anaemia, especially in older people.
Study by Mehta et al. revealed that increase in each 10 μg/m3 PM 2.5 exposure, the average prevalence of anaemia increased by 1.90% (1.43- 2.36) and the average haemoglobin concentration decreased by 0.07 gm/dL (0.05–0.09) in ecological analysis at district level. Individual level analysis produced that the odds of having anaemia was 1.09 (95% CI 1.06, 1.11) time higher with increase in each 10 μg/m3 PM 2.5 exposure in ambient air [26].
We found that, the central states like Uttar Pradesh, Chhattisgarh, Madhya Pradesh, Bihar had both high anaemia and IAP. The high anaemia prevalence might be due to nutritional factors, like- lack of dietary diversity, less iron rich diet and excessive milk consumption; limited health care awareness and infrastructure leading to delayed screening and diagnosis; parasitic infestation; lack of literacy and local cultural belief [27,28,29]. The high burden of IAP might be due to higher usage of solid/ unclean fuels (timber, straw, dung, crop residues). When these fuels are burned indoors, dangerous pollutants are released, such as fine particulate matter (PM2.5), which can worsen anaemia and cause respiratory problems [30]. Most of these states have rural participants contributing to higher traditional cooking practices with lack of proper ventilation system leading to higher IAP. Beside these, being Empowered Action Group (EAG) states having increase poverty, lack of literacy, health education, poor health indicators, lack of accessibility and affordability of improved healthcare infrastructures; participants from these states had higher anaemia and IAP exposure [31].
With increase in the educational status, the odds of having anaemia decreased. This might be due to with increase in the education status, the participants became more aware about their health status, which leads to early detection, prevention and treatment of anaemia. Participants residing in rural area had 1.47 times higher odds of having anaemia. Factors which might contribute to this were higher education, awareness, improved nutrition, better maternal education and early access to healthcare infrastructure. The odds of having anaemia was highest (AOR 1.37 (1.19–1.57)) among poorest participants. This might be due to lesser awareness, education, prevention, access to healthcare inability to pay the out-of-pocket expenditure due to treatment. Participants having multimorbidity (AOR 1.86 (1.71–2.03)) and history of tobacco abuse (AOR 1.23 (1.12–1.35)) had higher odds. This might be due to shared risk factors (inflammation, poor nutrition), interaction with iron metabolism, challenging and stigma is accessing healthcare services. Similar results were documented by various studies [32, 33].
There are certain strengths and limitations of the study
The biggest strength lies in the large nationally representative dataset which increased its generalisability. We have established the positive association between anaemia and indoor air pollution among older adults which was noble of its kind. This study not only showed the prevalence of exposure of indoor air pollution throughout the lifetime with stratified details but also unveil the curtain from the association between anaemia and indoor air pollution which was further stratified into detailed classification as per gender. Despite these there were some limitations. Due to its cross-sectional nature temporality could not be established. We were not able to calculate the degree of exposure to pollutants. We were not able to eliminate the effect of external air pollution. Due to self-reporting type of documentation of data, the actual prevalence of anaemia might be higher. Due to the self-reporting style, there were higher probability of recall bias and social desirability bias, which could not be eliminated.
There are key policy implications and recommendations emerging from the study. Owing to the limited access to clean fuel and compulsion to use biomass owing to financial hardship in the rural areas, IAP is becoming a serious public health hazard in the nation. Nonetheless, the Indian government has made a number of efforts to improve it, including 'Pradhan Mantri Ujjwala Yojana' (PMUY) [34] and the National Programme on Improved Chula (NPIC) [35]. Due to the pandemic's devastating effects and decimation of rural people's income and way of life, studies must be done in order to adequately examine and reconsider the price of liquified petroleum gas (LPG) and subsidies for the poor. More attention should be paid to educating the public about the negative impacts of using unclean biomass energy sources, indoor air pollution, and the necessity of a functional kitchen ventilation system, among other things. In unavoidable circumstances, substitutes such enhanced chullha powered by biomass with chimneys and cookstoves can be recommended, as indicated by a previous study, which may result in reduced indoor air pollution [36]. We recommend proper clinical or community-based trial to establish the temporality, causation and natural history of association of anaemia with indoor air pollution among older adults.
Conclusion
This study establishes convincing statistical evidence regarding positive association of anaemia with indoor air pollution among older Indian adults through a nationally representative large dataset. Interestingly, the association appears to be more pronounced among men. These findings might raise awareness and assist individuals in avoiding the negative effects of using solid/unclean fuels, inadequate ventilation, and indoor smoking. Implementing measures such as upgrading residential stoves with chimneys, providing access to clean cooking fuel, and enhancing home ventilation systems can significantly reduce exposure to indoor air pollution. The study highlights the urgency of initiating programs aimed at improving the accessibility and availability of clean fuel and technologies. By doing so, the nation can make strides toward achieving Sustainable Development Goal 7: Ensuring universal access to affordable, reliable, and modern energy services. More focused policies should be implemented towards the Empowered Action Group (EAG) states. Further evidence-based research is recommended to understand detailed causation and to establish temporality.
Availability of data and materials
The study utilizes nationally representative LASI survey data, which is publicly accessible and can be obtained by registering at https://iipsindia.ac.in/sites/default/files/LASI_DataRequestForm_0.pdf The processed data can be provided by the authors upon request by Dr. Pritam Halder (corresponding author).
Abbreviations
- LASI:
-
Longitudinal Aging Study in India
- PM 2.5:
-
Particulate matter 2.5
- LPG:
-
Liquefied Petroleum Gas
- MPCE:
-
Monthly per capita expenditure
- IAP:
-
Indoor air pollution
- PSM:
-
Propensity Score Matching
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence Interval
- LL:
-
Log-likelihood
- LR:
-
Likelihood Ratio
- AIC:
-
Akaike Information Criterion
- BIC:
-
Bayesian Information Criterion
- μg:
-
Microgram
- EAG:
-
Empowered Action Group
References
Government of India. Anemia Mukt Bharat training tool kit. New Delhi; 2018. Available from: https://anemiamuktbharat.info/wp-content/uploads/2019/11/English Anemia-MuktBharat-Training-Modules FolderLowress.pdf. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6697587/. Cited 2024 Feb 10.
Bagla P. Bagla P. World Health Organization. Anaemia policy brief. 2014 Available from: http://thousanddays.org/tdayscontent/uploads/Anameia-Policy-Brief.pdf.
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1(1):e16-25.
World Health Organization. The global prevalence of anaemia. Geneva: World Health Organization; 2011. Available from: https://apps.who.int/iris/bitstream/handle/10665/177094/9789241564960_eng.pdf?sequence=1. Cited 2024 June 18.
Gaskell H, Derry S, Andrew Moore R, McQuay HJ. Prevalence of anaemia in older persons: systematic review. BMC Geriatr. 2008;8(1):1.
Vanasse GJ, Berliner N. Anemia in elderly patients: an emerging problem for the 21st century. Hematology/the Education Program of the American Society of Hematology American Society of Hematology Education Program. Hematology. 2010;2010:271–5.
Cohen AJ, Ross Anderson H, Ostro B, Pandey KD, Krzyzanowski M, Künzli N, et al. The global burden of disease due to outdoor air pollution. J Toxicol Environ Health A. 2005;68(13–14):1301–7.
Mannucci PM, Franchini M. Health effects of ambient air pollution in developing countries. Int J Environ Res Public Health. 2017;14(9):1048.
Huang YCT. Outdoor air pollution: a global perspective. J Occup Environ Med. 2014;56:S3–7. Available from: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. Cited 2024 Feb 10.
Mittal H, Roberts L, Fuller GW, O’Driscoll S, Dick MC, Height SE, et al. The effects of air quality on haematological and clinical parameters in children with sickle cell anaemia. Ann Hematol. 2009;88(6):529–33.
Hong CH, Falvey C, Harris TB, Simonsick EM, Satterfield S, Ferrucci L, et al. Anemia and risk of dementia in older adults: findings from the Health ABC study. Neurology. 2013;81(6):528–33.
Honda T, Pun VC, Manjourides J, Suh H. Anemia prevalence and hemoglobin levels are associated with long-term exposure to air pollution in an older population. Environ Int. 2017;101:125–32. Available from: https://pubmed.ncbi.nlm.nih.gov/28153527/. Cited 2024 Feb 10.
Kelly FJ, Fussell JC. Air pollution and public health: emerging hazards and improved understanding of risk. Environ Geochem Health. 2015;37(4):631–49.
Elbarbary M, Honda T, Morgan G, Guo Y, Guo Y, Kowal P, et al. Ambient air pollution exposure association with anaemia prevalence and haemoglobin levels in Chinese older adults. IJERPH. 2020;17(9):3209.
International Institute for Population Sciences (IIPS) NP for, Health Care of Elderly (NPHCE), MoHFW HTHCS of, (USC) PH (HSPH) and the U of SC. Longitudinal Ageing Study in India (LASI) wave 1, 2017–18, India report. 2020. https://www.iipsindia.ac.in/sites/default/files/LASI_India_Report_2020_compressed.pdf. Cited 2023 Oct 4.
Dubowsky SD, Suh H, Schwartz J, Coull BA, Gold DR. Diabetes, obesity, and hypertension may enhance associations between air pollution and markers of systemic inflammation. Environ Health Perspect. 2006;114(7):992–8. Available from: https://pubmed.ncbi.nlm.nih.gov/16835049/. Cited 2024 Mar 26.
Marchini T, Zirlik A, Wolf D. Pathogenic role of air pollution particulate matter in cardiometabolic disease: evidence from mice and humans. Antioxid Redox Signal. 2020;33(4):263–79.
Gao N, Xu W, Ji J, Yang Y, Wang ST, Wang J, et al. Lung function and systemic inflammation associated with short-term air pollution exposure in chronic obstructive pulmonary disease patients in Beijing, China. Environ Health. 2020;19(1):12.
Dauchet L, Hulo S, Cherot-Kornobis N, Matran R, Amouyel P, Edmé JL, Giovannelli J. Short-term exposure to air pollution: associations with lung function and inflammatory markers in non-smoking, healthy adults. Environ Int. 2018;121:610–9. Available from: https://pubmed.ncbi.nlm.nih.gov/30312964/. Cited 2024 Mar 26.
Watanabe M, Noma H, Kurai J, Sano H, Hantan D, Ueki M, et al. Effects of short-term exposure to particulate air pollutants on the inflammatory response and respiratory symptoms: a panel study in schoolchildren from rural areas of Japan. Int J Environ Res Public Health. 2016;13(10):983.
Adami G, Pontalti M, Cattani G, Rossini M, Viapiana O, Orsolini G, et al. Association between long-term exposure to air pollution and immune-mediated diseases: a population-based cohort study. RMD Open. 2022;8(1):e002055. Available from: https://pubmed.ncbi.nlm.nih.gov/35292563/. Cited 2024 Mar 26.
Viehmann A, Hertel S, Fuks K, Eisele L, Moebus S, Möhlenkamp S, et al. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup Environ Med. 2015;72(9):656–63.
Xu Z, Wang W, Liu Q, Li Z, Lei L, Ren L, et al. Association between gaseous air pollutants and biomarkers of systemic inflammation: a systematic review and meta-analysis. Environ Pollut. 2022;292:118336. Available from: https://pubmed.ncbi.nlm.nih.gov/34634403/. Cited 2024 Mar 26.
Marques O, Weiss G, Muckenthaler MU. The role of iron in chronic inflammatory diseases: from mechanisms to treatment options in anemia of inflammation. Blood. 2022;140(19):2011–23. Available from: https://pubmed.ncbi.nlm.nih.gov/35994752/. Cited 2024 Mar 26.
Abiri B, Vafa M. Iron deficiency and anemia in cancer patients: the role of iron treatment in anemic cancer patients. Nutr Cancer. 2020;72(5):864–72. Available from: https://pubmed.ncbi.nlm.nih.gov/31474155/. Cited 2024 Mar 26
Mehta U, Dey S, Chowdhury S, Ghosh S, Hart JE, Kurpad A. The association between ambient PM2.5 exposure and anemia outcomes among children under five years of age in India. Environ Epidemiol. 2021;5(1):e125.
Let S. Prevalence and determinants of anaemia among women of reproductive age in Aspirational Districts of India: an analysis of NFHS 4 and NFHS 5 data | BMC Public Health | Full Text. 2024. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-17789-3. Cited 2024 Jun 1.
Roy TB, Das P, Das T. Unique contribution of maternal factors and its association with anemia among under 5 children in Indian context. Glob Soc Welf. 2024;11(1):45–60.
Singh RK, Patra S. Extent of anaemia among preschool children in EAG States, India: a challenge to policy makers. Anemia. 2014;2014:868752.
Cropper M, Park Y. The health benefits of air pollution control in India. Indian Econ Rev. 2022;57(2):245–63.
National Rural Health Mission, Health and Population Policies, Empowered Action Group States. Available from: https://main.mohfw.gov.in/sites/default/files/CHAPTER%202.pdf. Cited 2024 Jun 1.
Al-kassab-Córdova A, Mendez-Guerra C, Quevedo-Ramirez A, Espinoza R, Enriquez-Vera D, Robles-Valcarcel P. Rural and urban disparities in anemia among Peruvian children aged 6–59 months: a multivariate decomposition and spatial analysis. Rural Remote Health. 2022;22:6936. https://doi.org/10.22605/RRH6936. Available from: https://www.rrh.org.au/journal/article/6936. Cited 2024 Feb 10.
Abate TW, Getahun B, Birhan MM, Aknaw GM, Belay SA, Demeke D, et al. The urban–rural differential in the association between household wealth index and anemia among women in reproductive age in Ethiopia, 2016. BMC Womens Health. 2021;21(1):311.
Ranjan R, Singh S. Household cooking fuel patterns in rural India: pre- and post-Pradhan Mantri Ujjwala Yojana. Indian J Hum Dev. 2020;14(3):518–26.
Hanbar RD, Karve P. National Programme on Improved Chulha (NPIC) of the Government of India: an overview. Energy Sustain Dev. 2002;6(2):49–55.
Adane MM, Alene GD, Mereta ST. Biomass-fuelled improved cookstove intervention to prevent household air pollution in Northwest Ethiopia: a cluster randomized controlled trial. Environ Health Prev Med. 2021;26(1):1.
Acknowledgements
We want to convey our sincere gratitude towards the participants and Indian Council of Medical Research
Clinical trial number
Not applicable (this is a cross-sectional study.)
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Dr. Pritam Halder- Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing, Visualization, Supervision., Dr. Madhur Verma- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, Dr. Saumyarup Pal- Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing, Dr. Amit Kumar Mishra- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, Dr. Trideep Jyoti Deori- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, Dr. Riya Biswas- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, Dr. Jaya Tiwari- Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing, Dr. Anshul Mamgai- Resources, Data Curation, Writing- Review and editing, Visualization, Supervision, Shivani Rathor- Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing, Dr. Manish Chandra Prabhakar- Conceptualization, Methodology, Resources, Data Curation, Writing- Review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Being a secondary analysis of a dataset freely available in the public domain, ethical approval for the present study was not deemed necessary. However, the ethical approval to conduct LASI was given by the Indian Council of Medical Research's (ICMR) Central Ethics Committee on Human Research (CECHR) [15].
Consent for publication
Not applicable.
Competing interests
Authors have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Halder, P., Verma, M., Pal, S. et al. Association of anaemia with indoor air pollution among older Indian adult population: multilevel modelling analysis of nationally representative cross-sectional study. BMC Geriatr 24, 567 (2024). https://doi.org/10.1186/s12877-024-05171-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05171-2