Abstract
Introduction
Frailty is an age-related condition with increased risk for adverse health outcomes. Assessing frailty according to the Clinical Frailty Scale (CFS) based on data from medical records is useful for previously unassessed patients, but the validity of such scores in exclusively geriatric populations and in patients with dementia is relatively unknown.
Methods
Patients admitted for the first time to one of two geriatric wards at Örebro University hospital between January 1st – December 31st, 2021, were included in this study if they had been appointed a CFS-score by anamnestic interview (CFSI) at admission. CFS scores based on medical records (CFSR) were appointed by a single medical student, who was blinded to the CFSI score. Score-agreement was evaluated with quadratic weighted Cohen’s kappa (κ).
Results
In total, 145 patients between the age of 55–101 were included in the study. The CFSR and CFSI scores agreed perfectly in 102 cases (0.7, 95% CI 0.65–0.77). There was no significant difference regarding age, sex, comorbidity, or number of patients diagnosed with dementia between the patients with complete agreement and the patients whose scores did not agree. Agreement between the scores was substantial, κ = 0.66, 95% CI 0.53–0.80.
Conclusions
CFS scores based on information from medical records can be generated with substantial agreement to CFS scores based on in-person anamnestic interviews. A dementia diagnosis does not influence the agreement between the scores. Therefore, these scores are a useful tool for assessing frailty in geriatric patients who previously lack a frailty assessment, both in clinical practice and future research. The results support previous findings, but larger studies are warranted.
Similar content being viewed by others
Introduction
Old age poses an increased risk for frailty, thereby, as the general population of the world is getting older, the prevalence of frailty increases [1,2,3]. Frailty poses an increased risk to adverse health outcomes such as falls, hospitalization, admission to nursing homes and mortality [1]. It may also affect the response to treatments and recovery of mobility in older patients [4].
There is currently no consensus definition for frailty. The condition is commonly described as a multifactorial state or syndrome of higher risk for health issues due to a reduction in biological reserves and the ability of the body to adapt and resist external stressors. As the ability to adapt is compromised, this creates vulnerability [1, 2, 5]. Frailty and the lack of adaptive capacity is closely related to ageing [1, 3], but may arise from other conditions such as systemic illnesses or severe injuries [2].
Since there is no general definition for frailty, there also is no standard tool for measuring or grading frailty [6]. Grading frailty is important for risk stratification as well as for diagnosing and health care planning, such as to identify patients who would benefit from a comprehensive geriatric assessment (CGA) [7, 8]. The Clinical Frailty Scale (CFS) is a widely used, easily applicable tool for measuring frailty and has shown good predictive ability and high inter-rater reliability [9,10,11]. The CFS, developed in 2005 by Rockwood et al., considers matters of both physical and mental frailty [5]. It was later expanded to include guidelines on how to score patients with dementia [10]. Dementia significantly influences several aspects evaluated by the CFS, which complicates its use as a frailty assessment tool.
The CFS can be a component of a comprehensive geriatric assessment and is commonly used during consultations with patients or their caregivers. To achieve individualized care, the department of Geriatrics at Örebro University Hospital decided in the year of 2021 to assess frailty by means of the CFS on all patients on admittance to the clinic. Because of several reasons, staff shortage among others, these assessments could not be carried out as planned in clinical everyday practice. To produce data on possible frailty for patients who were not assessed on admittance, frailty assessments according to the CFS needed to be conducted in retrospect based on information from medical records. Several studies have previously demonstrated the validity of CFS scores based on data from medical records [11,12,13,14]. However, there is still insufficient data to confirm the validity of these CFS scores, especially in geriatric populations and in patients with dementia.
The aim of this study is to examine agreement between CFS scores acquired from studying medical records (CFSR) and CFS scores determined by hospital staff through anamnestic interviews at admission (CFSI), along with the possible impact on this agreement by a dementia diagnosis.
Methods
Study design and population
This is a cross sectional study evaluating patients admitted to two separate wards at the department of Geriatrics at Örebro University Hospital. Patients were included in the study if they were admitted for the first time between January 1st – December 31st, 2021, and had been appointed a CFSI score.
Collection of data
Frailty was assessed according to a verified Swedish translation of the CFS version 2.0 [15]. The CFS 2.0 is an ordinal scale ranging from 1 (very fit) to 9 (terminally ill). Scoring is based on the patient’s baseline state, which is usually defined as their state two weeks prior to assessment [10]. Patients with a score of CFS > 5 were considered frail. The CFSI score for each patient had been appointed at admission to the Geriatric wards according to a routine frailty assessment. This assessment consists of an interview with the patient and, sometimes, their close relatives, friends, or caregivers, and is conducted by a nurse, occupational therapist, or physiotherapist. The CFSR scores were generated through a systematic review of each patient’s medical records. This was conducted by a single medical student, who was blinded to the CFSI scores. Record entries from nurses, occupational therapists, physiotherapists, and physicians, dating at least 14 days prior admission, were reviewed. The CFSR scores were then based on information about the patient’s activities of daily life (ADL), cognition, living situation, medical history, and physical abilities. In cases of uncertainty about a score, the higher score was appointed. At two occasions, the medical student accidentally saw the CFSI score in the records. The patients in question were therefore not included from the study. The CFSR score was subsequently compared to the CFSI score.
Measurement
A customized standardized form designed for the purpose of this study was used to obtain relevant patient characteristics. The form included the patients’ gender, birthyear, and primary and secondary diagnoses based on the ICD-10. The latter were required to calculate the Charlson Comorbidity Index (CCI), which was used to weigh the patients’ comorbidities. The CCI was developed by Charlson et al. in 1987 and later adapted for register-based research in Sweden by Ludvigsson et al. The index is used to weigh comorbidities to estimate one-year mortality and consists of a numeric scale based on the presence of specific diagnoses as well as the patient’s age [16]. A higher score on the CCI indicates a higher one-year mortality [17]. A patient’s primary diagnosis was defined as the diagnosis set as main diagnosis on admission to the geriatric ward. Any other diagnoses were defined as secondary diagnoses. To portrait patient characteristics in Table 1, the primary diagnoses were sorted into six categories according to prevalence: orthopaedic, dementia, respiratory, cardio-vascular, surgical, and other. Any diagnosis not among the first five most prevalent categories was included in “others”.
Statistical analysis
To analyze differences in age and comorbidities by means of the CCI, the Unpaired t-test and Mann-Whitney U-test were utilized respectively. The Chi-squared test was used to analyze differences in gender and dementia diagnoses. Agreement between the CFSI and CFSR scores was measured with paired-sample sign test and quadratic weighted Cohen’s kappa (κ). The κ-value was interpreted according to Viera et al. [18]. The level of statistical significance was set to p < 0.05. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 29.0, Armonk, Ny: IBM Corp.
The method described by Newcombe & Altman [19] was used to calculate the 95% confidence interval (CI) for the proportion of CFS scores with perfect agreement. Results were deemed significant if the 95% CI did not include zero. The analysis was conducted using the software Confidence Interval Analysis version 2.2.0, University of Southampton.
Ethical considerations
All collected personal data was encoded and stored in a locked file cabinet at the department of Geriatrics. The study is approved by the Swedish Ethical Review Authority (Dnr 2022-01360-01 and dnr 2023-00994-02) and no written consent was required from the patients.
Results
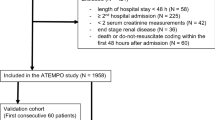
In the year of 2021, 415 patients were admitted to the department of Geriatrics at Örebro University Hospital. Of these, 269 patients were not included because they either had not been appointed a CFSI score on admission, because of restricted access to their medical records, or due to accidental discovery of the CFSI score while reading their medical records (Fig. 1). There was no significant difference in gender, age or comorbidity between the patients included and the patients not included in the study (p = 0.23, p = 0.21 and p = 0.14 respectively). Patient characteristics are presented in Table 1. Apart from the patients having a dementia diagnosis as their main diagnosis, as seen in Table 1, several other patients were diagnosed with dementia as a secondary diagnosis. In total there were 30 patients (21%) with a dementia diagnosis enrolled in this study.
Primary outcome- agreement between the CFSI- and CFSR-scores
All generated CFSI and CFSR scores are presented in Table 2. The two scores agreed perfectly in 102 of 145 cases (0.7, 95% CI 0.65–0.77). In 12 cases, the CFSR score was higher than the CFSI score, and in 31 cases it was lower than the CFSI score. CFS 7 was the most appointed score. No patient was appointed a score of 1 (very fit) or 2 (fit). CFS 3 and 9 were only appointed to one patient respectively. A comparatively low prevalence was also seen for CFS 4 and 8. The median CFSR score was 6 (IQR 5–7) and the median CFSI was 7 (IQR 6–7), p < 0.005. Agreement between the CFSR and CFSI scores was substantial (κ = 0.66, 95% CI 0.53–0.80).
Secondary outcome- impact of dementia on agreement
There was no significant difference in age, comorbidity, gender or the prevalence of dementia between the patients for whom the CFSI and CFSR scores agreed and the patients for whom the scores did not agree (Table 3).
Discussion
This study examined 145 patients who were admitted to the department of Geriatrics at Örebro University hospital during 2021. The aim was to examine agreement between CFS scores acquired from studying medical records (CFSR) and CFS scores determined by hospital staff through anamnestic interviews at admission (CFSI), along with the possible impact on this agreement by a dementia diagnosis. Perfect agreement between the scores was seen in 102 of 145 cases (70%). There was no significant difference regarding age, sex, comorbidity, or number of patients diagnosed with dementia between the 102 patients with complete agreement and the 43 patients whose scores did not agree.
This study shows a substantial agreement between CFSI and CFSR scores, which is in accordance with previous studies [11,12,13,14]. For two of these studies, a direct comparison cannot be made due to differences in the methods used for presenting agreement between the scores [11, 14]. Two other studies presented their results by means of Cohen’s kappa, as was done in this study [12, 13]. As one of these studies did not specifically use weighted Cohen’s kappa, a direct comparison may again not be possible [12]. The second study, a German study from 2020 including 110 patients, presented a weighted Cohen’s kappa value of 0.89, which represents an excellent agreement [13]. Compared to the value presented in this study, which was 0.66 and represents substantial agreement, the German study showed a higher rate of agreement. It is possible that this difference can be attributed to the different strategies used for appointing raters. Compared to this study, the German study had three staff members in total rating all scores, albeit being blinded to the individual patient’s other CFS score [13]. It is possible that fewer raters lead to higher agreement since it minimizes the variabilities in experience and methods applied by different people.
The score with best agreement between the CFSI and CFSR scores was CFS 7. This may be attributed to the distinct criteria set for CFS 7 by Rockwood et al. [10], which may have been easier to recognize in a patient. Determining agreement for the lowest and highest scores of the CFS was difficult as the prevalence of these scores was low, as seen in Table 2. Only a few patients were appointed a score of CFS 3, 8 or 9, and no patient was appointed a score of CFS 1 or 2. The distribution of scores shown in Table 2 is a credible reflection of the generally frail, but not terminally ill, population which is at higher risk to be admitted to a geriatric ward in the next 14 days. Since the agreement for the lowest and highest scores could not be correctly determined, it is possible that it may be either lower or higher compared to the agreement for the scores closer to the middle of the scale. A lower agreement would be a disadvantage for affected patients, as treatment based on their CFSR score would likely be insufficient or inappropriate. Comparing agreement for these scores specifically would be relevant to study in the future, particularly as they have had a low prevalence in previous studies as well [11, 12].
This study showed a statistically significant tendency to produce lower CFS scores when using information from medical records compared to when using information from anamnestic interviews, and therefore deeming patients as being less frail when using medical records (p < 0.005). The same tendency was observed in a German study from 2020, however, it was deemed clinically insignificant [13]. Perhaps a reason for this tendency may be that a person appointing a CFS score by means of studying medical records is less likely to be biased by the patient’s current condition as the patient is not present at the time of assessment. This would suggest that, in those cases where the CFSR and the the CFSI scores differ, the CFSR score may more accurately represent the patient’s frailty status, as the patient’s condition at the time of assessment for the CFSI is likely worse than their habitual condition due to the current hospitalization. Another reason for appointing lower CFSR scores may have been outdated information in medical records, which would instead result in a probable underestimation of frailty by CFSR scoring. In contrast, a study from 2022 showed a tendency for CFSR scores to be higher than CFSI scores, but the difference was not statistically significant [14]. Until sufficient research can rule out a possible tendency to over- or underestimate frailty through CFSR scores, they should only be utilized if the patient was for some reason not assigned a CFSI score but a score is needed for research or as guide to deciding further treatment. This minimizes the risk of excluding a potential patient from treatment that is reserved for patients with a certain CFS score, such as CGA.
Applying the CFS on patients with a dementia diagnosis may prove to be especially difficult as information on the patient’s physical and mental health state may be more difficult to obtain. This study found no significant difference in prevalence of a dementia diagnosis between the patients for whom the CFSI and CFSR scores agreed and the patients for whom the scores did not agree. This suggests that a dementia diagnosis does not influence the accuracy of CFSR scores, indicating that they may be used for patients with dementia as well.
Generating CFS scores solely based on information in medical records is dependent on the quality of the records. In those cases where patients have not been recently hospitalized, information is scarce and appointing an appropriate score is difficult. However, if a patient has been treated recently, the information provided is detailed and well suited for CFS-scoring. As the quality of medical records may vary throughout medical institutions, this may limit the generalisability of this study. This limitation does not apply when generating CFS scores based on in-person interviews as information about the patient’s health status 14 days prior to admission is obtained first hand, with the possibility to complete any missing information by further asking the patient’s close family, friends, or caregivers. The quality of information with this approach is instead dependent on the person conducting the interview, wherefore adequate training in CFS-scoring is essential. As in-person interviews pose more advantages, CFSR scores should not replace CFSI scores, only complement them.
A limitation of this study is its small patient sample. This was mainly due to it being a single centre study and due to the major drop out resulting predominantly from the lack of CFSI scores. The drop out itself may have been a weakness, although drop out analysis did not show any significant differences in age, gender or CCI between the inclusion group and the patients not included. Additionally, as CFSI scores were appointed by different hospital staff, equal assessment of all patients cannot be guaranteed. Based on recent studies, which showed high inter-rater agreement between CFS scores [11, 13, 14], this was deemed to not significantly have affected the study outcome. Another possible limitation regarding the CFSI scores is recall bias and not taking in count that the scores reflect the patients state of health 14 days prior to the assessment day. A possible bias for this study design would be basing the CFSR-scores on record entries containing information from the anamnestic interview conducted on admission for assessing the CFSI-scores. This bias was avoided by basing the CFSR-scores solely on information from record entries dated earlier than the patients’ admission to the department of Geriatrics.
A strength seen in this study was that all CFSR scores were appointed by the same person. Together with the use of the standardized forms employed for each patient, this ensured equal assessment of all patients in regard to CFSR scoring. In addition, the medical student appointing these CFS scores had no contact with the hospital staff appointing the CFSI scores or the patients involved. This ensured that the student was completely blinded to the CFSI score and to information about the patients outside of the medical records. However, the fact that only one person appointed all CFSR scores may also be a weakness.
The drop out seen in this study due to missing CFSI scores illustrates the need for CFSR scoring in clinical settings. As frailty is related to adverse health outcomes and may affect treatment response or recovery of mobility in elderly patients [1, 4], evaluating the possibility of frailty in geriatric patients is of great importance. Implicating CFSR scores for patients who, for several reasons, were not appointed a CFSI score on admission is therefore an important measure.
Conclusions
CFS scores based on information from medical records can be generated with substantial agreement to CFS scores based on in-person anamnestic interviews. A dementia diagnosis does not influence the agreement between the scores. Therefore, these scores are a useful tool for assessing frailty in geriatric patients who previously lack a frailty assessment, both in clinical practice and future research. The results support previous findings, but larger studies are warranted.
Data Availability
The datasets generated and analysed in this study are not publicly available due to ethical restrictions and laws (GDPR) of disclosing personal data. Inquiries for data access should be sent to the corresponding author, asa.andersson@oru.se, who will then contact the ethics board at Örebro University for permission to openly share the data.
Abbreviations
- ADL:
-
Activities of daily life
- CCI:
-
Charlson Comorbidity Index
- CFS:
-
Clinical Frailty Scale
- CFSR :
-
Clinical Frailty Scale score based on medical records
- CFSI :
-
Clinical Frailty Scale score based on anamnestic interviews
- CGA:
-
Comprehensive Geriatric Assessment
- CI:
-
Confidence interval
- FI:
-
Frailty Index
- ICUs:
-
Intensive Care Units
References
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A. 2001;56:M146–57.
Song X, Mitnitski A, Rockwood K. Prevalence and 10-Year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010;58:681–7.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–36.
Hatheway OL, Mitnitski A, Rockwood K. Frailty affects the initial treatment response and time to recovery of mobility in acutely ill older adults admitted to hospital. Age Ageing. 2017;46:920–5.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005;173:489–95.
Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med Elsevier. 2016;31:3–10.
Rockwood K, Theou O, Mitnitski A. What are frailty instruments for? Age Ageing. 2015;44:545–7.
Turner G, Clegg A. Best practice guidelines for the management of frailty: a British geriatrics society, age UK and royal college of general practitioners report. Age Ageing. 2014;43:744–7.
Church S, Rogers E, Rockwood K, Theou O. A scoping review of the clinical frailty scale. BMC Geriatr. 2020;20:393.
Rockwood K, Theou O. Using the clinical frailty scale in allocating scarce health care resources. Can Geriatr J. 2020;23:210–5.
Shears M, Takaoka A, Rochwerg B, Bagshaw SM, Johnstone J, Holding A, et al. Assessing frailty in the intensive care unit: a reliability and validity study. J Crit Care. 2018;45:197–203.
Davies J, Whitlock J, Gutmanis I, Kane S-L. Inter-rater reliability of the retrospectively assigned clinical frailty scale score in a geriatric outreach population. Can Geriatr J. 2018;21:1–5.
Stille K, Temmel N, Hepp J, Herget-Rosenthal S. Validation of the clinical frailty scale for retrospective use in acute care. Eur Geriatr Med. 2020;11:1009–15.
Kay RS, Hughes M, Williamson TR, Hall AJ, Duckworth AD, Clement ND. The clinical frailty scale can be used retrospectively to assess the frailty of patients with hip fracture: a validation study. Eur Geriatr Med. 2022;13:1101–7.
Ekerstad N, Swahn E, Janzon M, Alfredsson J, Löfmark R, Lindenberger M, et al. Frailty is independently associated with short-term outcomes for elderly patients with non–ST-segment elevation myocardial infarction. Circulation Am Heart Association. 2011;124:2397–404.
Ludvigsson JF, Appelros P, Askling J, Byberg L, Carrero J-J, Ekström AM, et al. Adaptation of the charlson comorbidity index for register-based research in Sweden. Clin Epidemiol. 2021;13:21–41.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Viera AJ, Garrett JM. Understanding interobserver agreement: the Kappa statistic. Fam Med. 2005;37(5):360–3.
Newcombe RG, Altman DG. Statistics with confidence. Proportions their Differ. London: BMJ Books; 2000. pp. 45–56.
Acknowledgements
Appreciation is expressed to all personnel at the department of Geriatrics who assisted with the collection of data and to Anders Magnuson, Clinical Epidemiology and Biostatistics, Örebro University, for advice on statistics.
Funding
Open access funding provided by Örebro University. The study was partly founded by Region Örebro County, Sweden. Grant number OLL 961450.
Open access funding provided by Örebro University.
Author information
Authors and Affiliations
Contributions
KJ, MiH, MaH, TA and ÅA contributed to this study as authors. ÅA is the corresponding author and managed the project administration. PW revised the manuscript and approved the final version. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Swedish Ethical Review Authority (Dnr 2022-01360-01 and 2023-00994-02), which also approved that no informed consent from the patients was needed.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jackwert, K., Holmér, M., Hallongren, M. et al. Agreement between Clinical Frailty Scale-scores based on information from patient interviews and Clinical Frailty Scale-scores based on information from medical records - a cross sectional study. BMC Geriatr 24, 570 (2024). https://doi.org/10.1186/s12877-024-05160-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05160-5