Abstract
Background
The impact of social frailty on older adults is profound including mortality risk, functional decline, falls, and disability. However, effective strategies that respond to the needs of socially frail older adults are lacking and few studies have unpacked how social determinants operate or how interventions can be adapted during periods requiring social distancing and isolation such as the COVID-19 pandemic. To address these gaps, we conducted a scoping review using JBI methodology to identify interventions that have the best potential to help socially frail older adults (age ≥65 years).
Methods
We searched MEDLINE, CINAHL (EPSCO), EMBASE and COVID-19 databases and the grey literature. Eligibility criteria were developed using the PICOS framework. Our results were summarized descriptively according to study, patient, intervention and outcome characteristics. Data synthesis involved charting and categorizing identified interventions using a social frailty framework.
Results
Of 263 included studies, we identified 495 interventions involving ~124,498 older adults who were mostly female. The largest proportion of older adults (40.5%) had a mean age range of 70-79 years. The 495 interventions were spread across four social frailty domains: social resource (40%), self-management (32%), social behavioural activity (28%), and general resource (0.4%). Of these, 189 interventions were effective for improving loneliness, social and health and wellbeing outcomes across psychological self-management, self-management education, leisure activity, physical activity, Information Communication Technology and socially assistive robot interventions. Sixty-three interventions were identified as feasible to be adapted during infectious disease outbreaks (e.g., COVID-19, flu) to help socially frail older adults.
Conclusions
Our scoping review identified promising interventions with the best potential to help older adults living with social frailty.
Similar content being viewed by others
Background
By the year 2050, two billion people worldwide will be 60 years of age and older [1, 2]. In Canada, the prevalence of frailty in those age 65+ years is almost twice that of those age 50-64 years [3]. The association of older age with increased prevalence of frailty may be due to the accumulation of multiple risk factors over time [3] and includes physical, psychological and social dimensions [4,5,6]. As such, frailty is considered “a syndrome that affects biological, psychological, and social processes of a person’s life and leads to increased vulnerability and adverse outcomes in old age” [7, 8]. Frailty has traditionally been conceptualized as a physiological phenomenon, and related assessment tools often emphasize physical qualities such as multimorbidity, nutrition, and functional independence [9]. In social frailty, it is a person’s social activities, social supports, social networks, loneliness and whether they are living alone that are involved [10]. Social frailty has been identified as a risk to healthy aging and defined as: “a continuum of being at risk of losing, or having lost, social and general resources, activities or abilities that are important for fulfilling one or more basic social needs during the life span” [11]. Social frailty is associated with other related and overlapping concepts [12,13,14,15] such as loneliness, social isolation, social vulnerability and resilience, which highlights that we cannot investigate social frailty in isolation. We need to understand not only how these social frailty concepts operate within a person’s physical and psychological health state, but what strategies are the most helpful during stressful periods when this population becomes more vulnerable (e.g., COVID-19 or other infectious disease outbreaks such as the flu).
As adults get older, their physical and cognitive capacity can decrease [16], which can progressively decrease their social activities, social circles, and increase the likelihood of living alone [17] – all these factors can lead to social isolation and social frailty [17]. The prevalence of social frailty varies widely and estimated to be between 7.7% to 47% (socially frail), and between 25% to 32.1% (pre-socially frail) [18,19,20]. During the first three years of the COVID-19 pandemic (2020-2022), social frailty prevalence rose to 18-25% among community-dwelling older adults [20, 21] and 47.3% in hospital [20], which was largely attributed to lockdown measures and quarantine leading to increased social isolation and loneliness among older adults. The impact of social frailty on older adults is profound. It is associated with the risk of all-cause mortality [22], physical and cognitive decline [18] including the onset of Alzheimer’s disease [23], reduced social and psychological well-being [17], depression and anxiety [24], moderate hearing loss [25], and decreased quality of life [26]. As such, social frailty represents one of the greatest challenges to the care for older adults and the health care system today. However, very little is known about effective strategies that can address social frailty.
Many existing knowledge syntheses focus on the clinical aspects of frailty (i.e., physical and psychological) or only on social isolation, vulnerability or loneliness [27,28,29,30]. Very few studies consider how social factors intersect with physical or psychological frailty [31, 32] (Fig. 1). Increasingly, the physical, social and cognitive problems experienced by older adults are being considered as part of psychological frailty, but their differences and associations are not well understood in the context of overall frailty [31].
Existing reviews also have not identified how interventions can address social frailty or related concepts (e.g., social isolation, loneliness, resilience; poverty risk; housing; physical safety; and social roles, networks, and relationships). Furthermore, little is known about which social frailty interventions have potential to be adapted for use during social distancing and isolation measures due to infectious disease outbreaks such as the COVID-19 pandemic. The pandemic response had indirect consequences on older adults as these measures led to an even greater risk of morbidity and mortality and reduced physical, mental and social wellbeing [33,34,35]. To address these gaps, our objectives were to:
-
1)
generate knowledge about which interventions have the best potential to help older adults (age ≥65 years) living with or at risk for social frailty or related concepts (e.g., social isolation, loneliness); and
-
2)
to identify interventions that may be the most helpful (and can be adapted) during infectious disease outbreaks requiring isolation (e.g., the COVID-19 pandemic, flu) when older adults are at even greater risk to become social frail.
Methods
Study design
We conducted a scoping review using the JBI methodology [36]. Our protocol was registered with the Open Science Framework (OSF) (registration: https://doi.org/10.17605/OSF.IO/2MDQF). We used the PRISMA extension for scoping reviews (PRISMA-ScR) [37] to prepare this manuscript. Our integrated knowledge translation (IKT) team contributed to the design and conduct of our scoping review. Our IKT team included knowledge users with expertise in social frailty (clinicians), scoping review methods (clinicians, researchers), patient partners with lived experience of social frailty and their caregivers. Our patient partners contributed to refining our research objectives, provided feedback on our data gathering tools, screened articles and helped to interpret findings.
Search strategy
An experienced information specialist (librarian) developed the search strategy, and a second information specialist appraised this strategy using the Peer Review of Electronic Search Strategies (PRESS) checklist [38]. We searched MEDLINE, CINAHL (EPSCO), EMBASE and COVID-19 databases (medRxiv and LitCovid) in English from 2000 to October 29, 2023, using a validated, age-specific search filter [39] to focus our search on studies on the older adult population (Supplement file 1). The search strategy utilized a combination of controlled vocabulary (e.g., “Social Isolation”, “Loneliness”, “Social Alienation”) and keywords (e.g., “connectedness”, “social vulnerability”, “aloneness”). We also searched the grey literature using the Canadian Agency for Drugs and Technologies in Health (CADTH) Grey Matter approach [40], including the sources of the Centre for Evidence-Based Medicine, Oxford COVID-19 Evidence Service.
Eligibility criteria
Our draft eligibility criteria were defined by our IKT team (including our patient partners) and developed using the PICOS framework [41]: Population: Community-dwelling older adults (age ≥ 65 years) at risk for or living with social frailty with or without concurrent disease(s) (e.g., diabetes). We excluded interventions targeting older adults living in long-term care homes (i.e., nursing home) or admitted to the hospital. Intervention: Any intervention addressing social frailty or related concepts (loneliness, social isolation, social vulnerability). Interventions that focused only on physical or psychological frailty were excluded. Outcomes: Social frailty or related concepts as reported by included studies (e.g., social support, social participation, social networks, social frailty index, loneliness score). We also considered quality of life (QOL), functional status (social), and general well-being (overall, social) outcomes. Study design: Any qualitative, quantitative, mixed-methods, multi-methods studies and systematic knowledge syntheses and excluded opinion driven reports (e.g., commentaries, editorials).
Article selection and extraction
Experienced reviewer pairs (IH, JH, JM, JS, KA, LH, LP, MM, MK) screened all potentially eligible records in duplicate for title and abstract screening and a verification process for full-text screening (one reviewer screened articles, and another verified 10% of these records). Reviewer pairs were calibrated at each screening level to ensure screening reliability (i.e., screening the same 10% set of articles by all reviewers until they reached ≥80% agreement, after which they screened independently). Our patient partners were also invited to screen articles. Any disagreements were resolved through team discussions.
Data charting
We developed and pilot tested a standardized data abstraction form, which was iteratively revised until data abstractor pairs reached consensus on data items. Experienced reviewer pairs (IH, JS, KA, MK, JH, LP, LH, MH) abstracted data and second reviewers checked a 10% random sample of data on key study characteristics (study design, journal, year and country of conduct), population characteristics (age, sex, gender, race) and intervention characteristics: type, mode of delivery (in-person, virtual), level of interaction with the intervention (one-to-one, group-based, self-directed, pair-based or mixed); and outcomes. Although not recommended by the JBI guide [42], abstracting outcome results was relevant for this review to identify interventions that could support knowledge user decision making about social frailty interventions, and how they might be adapted during infectious disease outbreaks. We also wanted to identify which intervention should be investigated in a future systematic review.
Data analysis and synthesis
Our results were summarized descriptively according to study, patient and intervention characteristics using tables and appendices. In our data analysis and reporting, all data was disaggregated by sex and gender if reported in included studies. To organize and categorize identified interventions, we used Bunt et al’s social frailty framework [11], which highlights that the concept of social frailty needs to include not only the absence (or threat) of general and social resources that are needed to fulfill basic social needs but also the absence (or threat) of social behaviours and social activities as well as self-management abilities [11]. As such, we categorized identified interventions according to Bunt et al’s four broad domains of social frailty: (i) General resource related (“Resources that are beneficial generally, indirectly contributing to social need fulfilment” such as education, financial status, housing, living environment, basic activities of daily living, cognition, lifestyle, life events); (ii) Social resource related (“Resources that are likely to directly contribute to the fulfilment of one of more social needs “such as marital status, family ties, living children, social network size, care or help from others) [43]; (iii) Self-management (to improve an individual’s ability to manage their behaviours and emotions to benefit their overall health [44]); and (iv) Social behavioural activities (“social behaviours or activities that are performed towards social need fulfilment” such as maintenance of close relationships, social participation, volunteerism, religiosity, occupation, neighborhood involvement) [43]. The intervention categorization process involved three reviewers (IH, KA, MK), iteratively developing a codebook and definitions using content analysis [45]. If interventions were represented by overlapping domains, we categorized interventions based on the predominant component via team discussion. We used a similar procedure to organize an expected large volume of outcomes and outcome categories from our studies. If reported, we also considered differences between participants of included studies in their social frailty risk (sex, gender, advanced age, low educational level and socioeconomic status and housing) as well as how they experience social frailty [10]. To classify loneliness, social and health and well-being outcomes in identified interventions, reviewer pairs (IH, JM, KA, MK) iteratively created a codebook using content analysis [45]. Our patient partners (BL, CM, JH, LP, MH, MT) had opportunities to review and provide feedback on these documents. Interventions were classified as “effective” if they reported outcome(s) as “effective” or “statistically significant”. We used the following effect direction definitions to classify all intervention result statements: “+*” = statistically significant positive impact; “-*” = statistically significant negative impact; “+” = positive direction in impact; “-“ = negative direction in impact; “+/-“ = mixed impact; NC = no change; NA = not applicable. One reviewer (IH) applied the effect direction classification scheme, and another reviewer (MK) audited a 10% random sample of classifications. We also identified effective interventions that may be helpful during infectious disease outbreaks such as the COVID-19 pandemic. This was based on whether interventions required participants to have any physical contact or in-person interaction with another individual (i.e., whether the intervention was feasible to be delivered virtually or remotely).
Results
Literature search
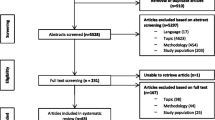
Of 31,339 records that were identified by our search strategy, we screened 20,709 titles and abstracts and 928 full-text articles. Of these, 263 studies plus 3 companion reports met the eligibility criteria and were included in our scoping review (Fig. 2).
Study characteristics
Table 1 includes the study characteristics. Of the 263 included studies, 57% were published between 2021 and 2023 followed by 31%, which were published between 2016-2020 with the earliest published in 2000. Most studies were conducted in North America (38%), followed by Europe (31%), Asia (19%%) and Australia (8%) (Fig. 3). The study designs of included studies were quasi-experimental (23%), qualitative (19%), experimental (19%) including 43 randomized controlled trials (16%), knowledge synthesis (19%), mixed- or multi-methods (16%), cross-sectional (2.7%), observational (1.5%) and cost or economic analysis (0.4%).
Population characteristics
A total of ~124,498 older adults were included among our 263 included studies representing 90% of the 495 identified interventions. Table 1 includes the participant characteristics. Of the interventions that reported on age (N=385; 78%), the largest proportion of older adults (N=156; 40.5%) had a mean age range of 70-79 years. Of 115 interventions that reported on participant sex (62%), 273 interventions (88%) included mostly female participants. Two interventions reported on gender (0.4%) and 83 interventions reported on race or ethnicity (17%). Of these, the largest proportion of interventions reported racial groups that self-identified as white (59 of 83 interventions; 71%), black (44 of 83 interventions; 53%), Latinx (28 of 83 interventions; 34%) or Asian including east, southeast and south Asian (23 of 83 interventions; 28%).
Intervention characteristics
Table 1 includes the intervention characteristics. Most of the 495 identified interventions were represented by three of the four social frailty domains [11]: 196 social resource related (40%), 157 self-management (32%), and 140 social behavioural activity interventions (28%); 2 interventions were identified from the general resource related domain (0.4 %). The largest proportion of interventions sub-categories were self-management education (21%), physical activity (9.7%) and leisure (9.7%) interventions followed by psychological self-management interventions (8.7%) and Information Communication Technology (ICT) (8.3%). The details of these intervention categories and sub-categories are in Supplement file 2. The most common mode of intervention delivery was in-person (59.5%) or virtual (35%). Participants most often interacted with interventions via group-based (48.5%) or one-to-one (27%) strategies. Intervention settings were mostly at home (47.5%) or in the community (20%).
Outcome characteristics
We identified 10 categories of outcomes (Supplement file 3): Loneliness outcomes were investigated by the largest proportion of interventions (n=312; 63%) followed by Social cohesion and connectedness (n=120; 24%), Quantity of social relationships (n=98; 20%), Social capital (n=95; 19%), Health and Wellbeing (n=83; 17%), Social engagement (n=78; 16%), Social isolation (n=75; 15%),
Social functioning and skills (n=37; 7.5%), Quality of life (n=54; 11%), and Frailty (n=5; 1%) outcomes. The highest concentration of effective interventions was found to be among loneliness outcomes (n=275), which was spread in similar proportion across the three social frailty domains: social behavioural activity (47%), self-management (43%) and social resource-related (42%).
Narrative synthesis of results
The detailed description of identified interventions and their impact across four social frailty domains are in Tables 2, 3 and 4.
Social resource-related interventions (n=196) (Table 2)
ICT-based (n=43), intergenerational (n=33), aging in place (n=31), socially assistive robots and computer agents (n=29), befriending (n=27), peer support group (n=23), mentorship, and mentorship (n=11) interventions.
ICT-based interventions included social networking platforms/apps (n=30), device-mediated communication strategies (n=9) or a combination of the two (n=2). Most of the social networking platforms/apps (70%) and device-mediated communication strategies (71%) showed non-significant improvements in social outcomes. Findings for loneliness outcomes were mixed with mostly non-significant improvement (70%) or no change (50%) for social networking platforms/apps, and non-significant improvement (71%), mixed findings (43%) or no change (14%) for device-mediated communication strategies. Intergenerational interventions included five types: strategies designed to promote or build social connections and engagement (n=12), to share experiences and memories including reminiscence therapy (n=7); community-based (n=6) or general (n=4) intergenerational programs; and interventions that promote socialization through activities and skills training (n=4). Most interventions from these five intergenerational intervention categories (range 67%-100%) significantly reduced loneliness outcomes. Similarly, most interventions across four of the five intervention categories (range 50%-100%) significantly improved health and wellbeing outcomes. Social outcomes across the five intervention categories mostly improved (range 50%-80%), but these were not significant. Aging in place interventions included home visit interventions (n=14), day care/seniors centres (n=8), telehealth interventions (n=7), and meal delivery interventions (n=4). Loneliness outcomes significantly improved in 40% of day care/seniors centre interventions, 40% of telehealth interventions, and 75% of meal delivery interventions; and no change was observed among 57% of home visit interventions. Among social outcomes, day care/seniors centres showed significant (50%) and non-significant (50%) improvement; and 44% of home visit interventions and 40% of telehealth interventions found non-significant improvement. Among health and wellbeing outcomes, most home visit or day care/seniors centre interventions (67% for both) showed significant improvement; one telehealth intervention showed non-significant improvement and meal delivery showed no change among the two interventions that investigated this outcome. Socially assistive robots (n=16) and computer agent (n=14) interventions. Among robot interventions, most reduced loneliness (67%), social (100%) and health and wellbeing (67%) outcomes non-significantly. Most computer agent interventions non-significantly improved social (83%) and wellbeing (67%) outcomes and of nine interventions that investigated loneliness outcomes, 44% significantly and 44% non-significantly showed improvement. Befriending interventions included technology mediated (n=14) and non-technology mediated (n=10) befriending interventions, and a combination of the two (n=2). None of the befriending interventions improved outcomes significantly, but most showed positive impact on loneliness (range 60%-80%), social (89%-100%) or health and wellbeing (40%-67%) outcomes regardless of whether they were mediated by technology or not. Peer support group interventions included those that were delivered in-person (n=16) or virtually (n=6). Half of in-person peer support interventions significantly reduced loneliness and health and wellbeing outcomes, and most (82%) non-significantly improved social outcomes. Most virtual peer support interventions (67%) improved social outcomes and half improved health and wellbeing outcomes but not significantly. Mentorship interventions included in-person delivered (n=8) or a combination of in-person and/or virtually delivered (n=3). Most in-person mentorship interventions (67%) significantly reduced loneliness outcomes. Of interventions that investigated social outcomes (n=3), most (75%) showed non-significant positive impact. When mentorship interventions were delivered in-person and/or virtually, findings were mixed with half of interventions finding significant improvement and half finding no change in loneliness, social or health and wellbeing outcomes.
Self-management-related interventions (n=157) (Table 3)
Self-management education (n=106), psychological self-management interventions (n=43), and social prescribing or asset-based (n=8).
Self-management education interventions included social health training (n=30), general health training (n=23), combination of technology device and Internet training (n=21), technology device training (n=16), caregiver support education (n=7), peer-based self-management education (n=5), and self-management skills training (n=4). Among social health training interventions, 70% significantly reduced loneliness and 40% significantly improved wellness outcomes, and most interventions (79%) non-significantly improved social outcomes. General health training interventions had mixed results with a third showing significant impact and 31%-40% showing no change in loneliness and social outcomes; wellness outcomes non-significantly improved in 57% of interventions. Most technology device training interventions had no change in loneliness (63%) or wellness (60%) outcomes but showed a non-significant improvement in social outcomes among 63% of interventions. 40% of caregiver support education interventions significantly reduced loneliness but showed mixed results for social and health and wellness outcomes. Among peer-based self-management education interventions, 60% non-significantly improved social outcomes and the two interventions that investigated health and wellness outcomes showed significant improvement. Most self-management skills training interventions (67%) improved social outcomes significantly but found mixed results for loneliness outcomes. Psychological self-management interventions included behavioural activation and cognitive behavioural therapy (CBT) interventions (n=22); a combination of different psychological interventions (e.g., CBT + mindfulness; music + reminiscence) (n=11), psychosocial interventions (n=5) and reminiscence therapy (n=5). Most behavioural activation or CBT interventions significantly reduced loneliness (63%) and improved health and wellbeing (67%) outcomes and half non-significantly improved social outcomes. Of interventions that included a combination of different psychological strategies, most showed positive impact for loneliness (67%) and social (60%) outcomes, but these were not significant. Among psychosocial interventions, none of the interventions showed impact in loneliness outcomes, 75% also showed no change in social outcomes but there was a non-significant improvement in health and wellbeing outcomes in two interventions. Among reminiscence therapy interventions, most (67%) significantly reduced loneliness outcomes, all interventions non-significantly improved social outcomes, and none of the three interventions that investigated health and wellness outcomes showed impact. Social prescribing or asset-based interventions included eight interventions, most of which (80%) significantly reduced loneliness and half significantly improved social outcomes; none investigated health and wellbeing outcomes.
Social behavioural activity interventions (n=140) (Table 4)
Physical activity (n=48) leisure activity (n=48), arts-based (n=27), mind-body (n=14), and spiritual (n=3) interventions.
Physical activity interventions: Among 16 technology-mediated physical activity interventions (including seven exergaming interventions), results were mixed for loneliness outcomes as 43% of interventions showed significant reduction in loneliness and 43% showed no change. For social outcomes, many interventions showed significant (40%) and non-significantly improvement, while 75% of interventions that investigated health and wellness outcomes found no change. Among physical activity interventions that were not technology mediated, some interventions investigating loneliness outcomes showed significant (36%) and non-significant (45%) improvement. Social outcomes improved non-significantly among 57% of interventions; and many interventions showed significant (50%) and non-significantly (67%) improvement in health and wellbeing outcomes. Leisure activity interventions: included group-based (n=19), self-directed (n=10), one-to-one (n=6) or mixed level of interaction (n=8) interventions. Many leisure activity interventions significantly reduced loneliness and improved health and wellbeing outcomes with group-based (43% and 55%, respectively) or self-directed (44% and 50%, respectively) interaction with the intervention. Results were mixed for strategies that were one-to-one or mixed level of interaction for loneliness and health and wellness outcomes. Social outcomes were non-significantly improved for most leisure interventions regardless of the type of interaction participants had with the intervention: group-based (55%), self-directed (50%), one-to-one (75%), mixed (71%). Arts-based interventions: included direct engagement (n=21), receptive engagement (n=3) or a combination of the two (n=2). Many arts-based interventions significantly reduced loneliness regardless of whether they were direct or receptive engagement strategies (44% and 50%, respectively). Most direct engagement in the arts strategies also improved social (71%) and health and wellbeing (75%) outcomes, but these were not significant. All the two arts-based interventions that included both direct and receptive engagement showed positive, non-significant reduction in loneliness and social outcomes. Mind-body interventions: Whether delivered in-person (n=11) or virtually (n=3), most mind-body intervention significantly reduced loneliness outcomes (44% and 67%, respectively). Among in-person strategies, most (75%) significantly improved social outcomes, and the two interventions that investigated health and wellbeing outcomes, also showed significant improvement. Spiritual interventions: Of three spiritual interventions, two significantly reduced loneliness. Social and health and wellness outcomes were mixed as one intervention significantly improved social outcomes while another showed no change in health and wellness outcomes.
General resource interventions (n=2) (Supplement Table 2)
Two interventions were identified: A single mixed method environmental study showed that renovating the neighborhood open spaces had some positive effects on social participation. The second intervention involving a hearing aid and hearing diary showed a nonsignificant decrease in loneliness from baseline to 6-month follow-up.
Interventions with potential to help older adults during isolation measures due to infectious disease outbreaks
Of the 495 interventions that were identified in our scoping review, 189 (38%) reported at least one effective loneliness, social or health and wellbeing outcome across the three social frailty domains. Of these, we identified 63 interventions (33%) that may be considered to address social frailty in older adults during infectious disease outbreaks requiring social distancing and isolation (i.e., interventions that don’t require physical contact with a person) (Table 5). Effective interventions were clustered within six intervention categories across three social frailty domains: (i) psychological self-management (n=11) and (ii) self-management education (n=9) within the self-management domain; (iii) leisure activity (n=11) and (iv) physical activity (n=8) interventions within the social behavioural activities domain; and (v) ICT (n=10) and (vi) socially assistive robots and computer agents (n=5) within the social resource domain. Loneliness outcomes were the most frequently investigated across the six intervention categories. Additionally, the highest proportion of effective interventions were those that reduced loneliness outcomes (70-100%) compared with the proportion of interventions that improved social (range 18-60%) or health and wellbeing outcomes (range 11-38%). There were two interventions categories (self-management education, leisure activity) that included interventions that had significant impact across all three outcome categories: loneliness (89% and 73% respectively), social (44% and 45%, respectively), and health and wellbeing (11%, 27%). Among 10 effective ICT-based interventions, 70% reduced loneliness outcomes and 60% improved social outcomes. Among 11 psychological self-management interventions, 82% reduced loneliness outcomes, and 18% improved social outcomes. Among five effective computer agent or robot interventions, all reduced loneliness and one improved self-rated health.
Discussion
Our scoping review identified 495 interventions across four broad domains of social frailty: social resource-, self-management-, social behaviour- and general resource-related [11] (Supplement file 2). The spread of effective interventions was nearly equal among social behaviour activity (44%) and self-management (41%) domains, followed by the social resource-related domain (33%). None of the interventions in the general resource related domain were effective. This was expected given that this category within Bunt et al’s social frailty model represents “non-specific or general resources” that fulfill social needs more indirectly and which tend to be contextual or an unmodifiable resource (e.g., educational level, income) [11, 43].
The most promising interventions were clustered around the behavioural activity and self-management domains of social frailty. Social behavioural activity interventions promote social behaviours or activities with the goal of fulfilling social needs (e.g., maintaining relationships, social participation) [43]. Most of the effective interventions in this domain were in the leisure activity (n=11) and physical activity (n=8) intervention categories. Effective leisure activities included horticulture therapy, volunteering and socializing, letter writing, and lifestyle engagement. Effective physical activities included technology-mediated (e.g., via computer, exergames) or non-technology-mediated (e.g., walking, outdoor park). Overall, both intervention categories had the greatest impact on loneliness outcomes (64% of leisure activity and 88% of physical activity interventions).
Interventions among the self-management domain aim to improve an individual’s ability to manage their behaviours, emotions and lifestyle toward improving overall health [44]. Most of the effective interventions in the self-management domain clustered within the psychological self-management (n=11) and self-management education (n=9) categories. Psychological self-management interventions included behavioural activation and CBT strategies. Self-management education interventions included skills training in general health, self-management, technology device and Internet use; and caregiver support education. Self-management strategies also had the greatest impact on loneliness outcomes as 82% of psychological and 89% of self-management education interventions significantly reduced loneliness. The positive impact of self-management interventions is not surprising given that a person’s ability to self-manage in general but particularly their social lives and activities is an important determinant of loneliness [46] and may also support healthy aging among community-dwelling older adults [47]. A person with stronger self-efficacy is more likely to do activities and to put in the effort to reach their goals [48,49,50]. Those who have higher coping self-efficacy (i.e., “a measure of self-confidence in one’s ability to effectively manage challenges using skills in problem-solving, emotional regulation, and coping through social support”) have significantly lower odds of loneliness [51]. These suggest that we need to incorporate self-efficacy skills development and as an important component of a future social frailty intervention.
We also identified several effective interventions that may be considered during isolation measures due to infectious disease outbreaks such as the COVID-19 pandemic (i.e., physical activity, leisure activity, psychological self-management, ICT, self-management education). Most of these were delivered virtually via a computer or smart device (tablet, smartphone). Although ICT and digital communication technologies offer opportunities for older adults to remain socially connected and reinforce their existing or new social connections and relationships [52], their impact has generally been mixed [27], which is consistent with our findings. Reasons for this may be that few high-quality studies investigating ICT-based interventions exist, and many ignore confounding factors such as sociodemographic data [53]. Digital technologies have become a prominent part of social contact, interactions, and communication in society, and digital social media in particular, can expedite personal interactions and contactless communication [54]. However, digital inequities among older adults can occur on multiple levels, particularly if they are economically disadvantaged. Many older adults are excluded from social networks and online connectivity because they cannot easily access the internet either because they don’t have access to computers and smart devices, or they don’t have internet connection [54, 55]. Furthermore, older adults may have differing knowledge, capacity, digital literacy, motivation and competence to access and engage with technology [55]. The COVID-19 pandemic further highlighted the depth of inequities among vulnerable populations related to gender, race, socioeconomic status, newcomer status, education social network quality and health literacy [55,56,57]. Older adults can only benefit from virtually delivered effective interventions if they have access to and can afford the technology (including the internet) and have digital literacy to benefit from services and resources, which are often only available via online government and other organization websites.
Considerations for future work in social frailty
Our scoping review results have several important considerations for future work in social frailty. First, we must ensure that a future social frailty innovation is usable, affordable, and accessible by all older adults by considering all possible inequities that they may experience. Second, a future social frailty intervention should target elements from all social frailty domains: the social resources of older adults (e.g., friendships or care from family members), their personal activities or social behaviours (e.g., social participation), as well as their self-management ability to gain or maintain their social resources and activities (e.g., their ability to make and maintain friends or to initiate social participation). Social frailty is a multidimensional concept because it’s not just about the absence of social resources or restrictions but the absence of social behaviours and social activities (e.g., maintaining cohesive relationships or social participation) as well as the absence of self-management abilities (e.g., feeling empowered or having the ability to make decision) [11]. Another important consideration is that the overall wellbeing of older adults is dependent on fulfilling needs according to their individual and personal circumstances, social resources, activities and capabilities [11, 58]. Third, we should consider social prescribing alongside self-management as these strategies can be particularly helpful for more vulnerable populations such as those with social frailty. These strategies can support self-management by connecting older adults to non-clinical supports in their communities [59]. Of the eight social prescribing interventions that we identified, 80% significantly reduced loneliness and 50% significantly reduced social outcomes. Lastly, social frailty is an important risk factor for developing physical frailty in non-frail older adults [60]. As older adults increasingly rely on their informal social relationships for well-being (e.g., family and friends), it may be more prudent to address social frailty directly, which has the potential to improve outcomes across other frailty types (e.g., physical and psychological) in addition to the overall frailty state [61]. People with stronger compared with weaker social relationships have a 50% increased likelihood of survival [62], and as the number and types of social activities increases, so does social participation and positive self-perceived health [63]. This means that social frailty doesn’t have to be an inevitable part of aging.
Strengths and limitations
Our study used rigorous scoping review methods adhering to JBI guidelines [36]. We identified 189 social frailty interventions from 263 included studies that were reported as effective, and a subset of 63 interventions that may be feasible to be adapted during infectious disease outbreaks requiring further social isolation and distancing (Table 5). To our knowledge, this is the first scoping review of social frailty interventions grounded in theory [11]. Existing reviews focus on investigating the prevalence of social frailty [20] or focusing only on technology-based interventions [29, 52, 64] or on specific aspects of social frailty outcomes (loneliness, social isolation or vulnerability [27, 28, 30]. An important gap was that none of the 495 identified interventions were designed for social frailty and only one intervention measured social frailty as an outcome [65]. Our study also had some limitations. We identified a large number of interventions with considerable heterogeneity in the type of identified interventions and outcomes. It was also challenging to organize outcomes because they were inconsistently defined (e.g., social participation, social isolation, social vulnerability, social connectivity). To overcome this challenge, reviewer pairs (IH, JM, KA, MK) iteratively created a codebook for classifying outcomes using qualitative content analysis [45] (Supplement file 3).
Conclusions
Our scoping review identified promising interventions for socially frail older adults with self-management- and social behavioural activity-related strategies showing the highest rates of significantly positive impacts on loneliness, social, health and wellbeing outcomes. We also identified that psychological self-management, self-management education, leisure activity, physical activity, ICT and socially assistive robots and computer agent interventions delivered mostly virtually would be most feasible to help older adults during isolation measures due to infectious disease outbreaks such as the COVID-19 pandemic.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- OSF:
-
Open Science Framework
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping reviews
- CADTH:
-
Canadian Agency for Drugs and Technologies in Health
- PICOS:
-
Population, Intervention, Comparator/Context, Outcomes, Study design
- JBI:
-
Joanna Briggs Institute
- ICT:
-
Information Communication Technology
- RCT:
-
Randomized Controlled Trial
- CBT:
-
Cognitive Behavioural Therapy
- ICT:
-
Information Communication Technology
References
Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults–present status and future implications. Lancet. 2015;385(9967):563–75.
Statistics_Canada. Canada Yearbook. Seniors. 2012; http://www.statcan.gc.ca/pub/11-402-x/2012000/chap/seniors-aines/seniors-aines-eng.htm. Accessed February 2020.
Kehler DS, Ferguson T, Stammers AN, et al. Prevalence of frailty in Canadians 18–79 years old in the Canadian Health Measures Survey. BMC Geriatrics. 2017;17(1):28.
Ament BHL, de Vugt ME, Verhey FRJ, Kempen GIJM. Are physically frail older persons more at risk of adverse outcomes if they also suffer from cognitive, social, and psychological frailty? Eur J Ageing. 2014;11(3):213–9.
Gobbens RJ, van Assen MA, Luijkx KG, Schols JM. The predictive validity of the Tilburg Frailty Indicator: disability, health care utilization, and quality of life in a population at risk. Gerontologist. 2012;52(5):619–31.
Markle-Reid M, Browne G. Conceptualizations of frailty in relation to older adults. J Adv Nurs. 2003;44(1):58–68.
Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Frail elderly. Identification of a population at risk. Tijdschr Gerontol Geriatr. 2007;38(2):65-76.
Freitag S, Schmidt S. Psychosocial Correlates of Frailty in Older Adults. Geriatrics. 2016;1:26.
Chen Yi-Ru R, Schulz PJ. The effect of information communication technology interventions on reducing social isolation in the elderly: A systematic review. 2016;18(1): e18.
Bessa B, Ribeiro O, Coelho T. Assessing the social dimension of frailty in old age: A systematic review. Arch Gerontol and Geriatr. 2018;78:101–13.
Bunt S, Steverink N, Olthof J, van der Shans C, Hobbelen J. Social frailty in older adults: a scoping review. Eur J Aging. 2017;1(12):323.
MacLeod S, Musich S, Hawkins K, Alsgaard K, Wicker ER. The impact of resilience among older adults. Geriatr Nurs. 2016;37(4):266–72.
Jeste DV, Savla GN, Thompson WK, et al. Association between older age and more successful aging: critical role of resilience and depression. Am J Psychiatry. 2013;170(2):188–96.
Gale C, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English Longitudinal Study of Ageing. Age and Ageing. 2018;47:392–7.
Andrew MK. Frailty and Social Vulnerability. Interdiscip Top Gerontol Geriatr. 2015;41:186–95.
Lee Y, Chon D, Kim J, Ki S, Yun J. The predictive value of social frailty on adverse outcomes in older adults living in the community. Journal of the American Medical Directors Association. 2020;21(10):1464–9.
Henry JD, Coundouris SP, Mead J, Thompson B, Hubbard RE, Grainger SA. Social frailty in late adulthood: social cognitive and psychological well-being correlates. J Gerontol B Psychol Sci Soc Sci. 2023;78(1):87–96.
Ma L, Sun F, Tang Z. Social Frailty is Associated with Physical Functioning, Cognition, and Depression, and Predicts Mortality. J Nutr Health Aging. 2018;22(8):989–95.
Yamada M, Arai H. Social frailty predicts incident disability and mortality among community-dwelling Japanese older adults. Journal of the American Directors Association. 2018;19(12):1099–103.
Zhang ZM, Cao S, Gao M, Ziao S, Xie X, Wu X. The prevalence of social frailty among older adults: A systematic review and meta-analysis. JAMDA. 2023;24:29–37.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104(2):368504211019854.
Goto T, Kishimoto T, Fujiwara S, Shirayama Y, Ichikawa T. Social frailty as a predictor of all-cause mortality and functional disability: a systematic review and meta-analysis. Nature Scientific Reports. 2024;14:3410.
Tsutsumimoto K, Doi T, Nakakubo S, et al. Impact of Social Frailty on Alzheimer’s Disease Onset: A 53-Month Longitudinal Cohort Study. J Alzheimers Dis. 2019;70(2):585–93.
Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–70.
Yoo M, Kim S, Kim BS, et al. Moderate hearing loss is related with social frailty in a community-dwelling older adults: The Korean Frailty and Aging Cohort Study (KFACS). Arch Gerontol Geriatr. 2019;83:126–30.
Chen WY, Huang XH, Pu YH, Xu JX, Gao JL. Relationship between social frailty and quality of life in community elderly. Geriatr Health Care. 2022;28(1):30–4.
Hoang P, King JA, Moore S, Moore K, Reich K, Sidhu H, Tan CV, Whaley C, McMillan J. Interventions associated with reduced loneliness and social isolation in older adults: A systematic review and meta-analysis. JAMA Network Open. 2022;5(10):e2236676.
Williams CYK, Townson AT, Kapur M, Ferreira AF, Nunn R, Galante V, Gentry S, Usher-Smith JA. Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: A rapid systematic review. PLoS ONE. 2021;16(2): e0247139.
Mah J, Rockwood K, Stevens S, Keefe J, Andrew MK. Do interventions reducing social vulnerability improve health in community dwelling older adults? A systematic review. Clinical Interventions in Aging. 2022;17:447–65.
Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26(2):147–57.
ZhaoJ, Liu YWJ, Tyrovolas S, Mutz J. Exploring the concept of psychological frailty in older adults: a systematic scoping review. JCE 2023;159:300-308.
Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011;27(1):1–15.
Lebrasseur A, Fortin-Bedard N, Lettre J, Raymond E, Bussieres EL, Lapierre N, Faieta J, Vincent C, Duchesne L, Ouellet MC, Gagnon E, Tourigny A, Lamontagne ME, Routhier F. Impact of the COVID-19 pandemic on older adults: Rapid Review. JMIR Aging. 2021;4(2): e26474.
World Health Organization (WHO). Health care considerations for older people during COVID-19 pandemic. WHO. Available at: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/technical-guidance/health-care-considerationsfor-older-people-during-covid-19-pandemic (2020).
Losada-Baltar A, Jimenez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro MDS, Fernandes-Pires J, Marquez-Gonzalez M. "We Are Staying at Home." Association of Self-perceptions of Aging, Personal and Family Resources, and Loneliness With Psychological Distress During the Lock-Down Period of COVID-19. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e10–e16.
Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18:2119–26.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 guideline statement. J Clin Epidemiol. 2016 Jul; 75:406. http://www.sciencedirect.com/science/article/pii/S0895435616000585
Kastner M, Wilczynski NL, Walker-Dilks C, McKibbon KA, Haynes RB. for the Hedges Team. Age-specific Search Strategies for MEDLINE JMIR. 2006;8(4): e25.
CADTH. Grey Matters: a practical tool for searching health-related grey literature | CADTH.ca. 2015; https://www.cadth.ca/resources/finding-evidence/grey-matters. Accessed February 2020.
Stone PW. Popping the (PICO) question in research and evidence-based practice. Appl Nurs Res. 2002;15(3):197–8.
Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC, Evans C, de Moraes EB, Godfrey CM, Pieper D, Saran A, Stern C, Munn Z. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. 2023;21(3):520–32.
Pek K, Chew J, Lim JP, Yew S, Tan CN, Yeo A, Ding YY, Lim WS. Social Frailty is Independently Associated with Mood, Nutrition, Physical Performance, and Physical Activity: Insights from a Theory-Guided Approach. International Journal of Environmental Research and Public Health. 2020;17:4239.
Lin, C.E., Wood, J.J. (2013). Self-management Interventions. In: Volkmar, F.R. (eds) Encyclopedia of Autism Spectrum Disorders. Springer, New York, NY.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nursing. 2008;62(1):107–15.
Nieboer AP, Hajema K, Murray Gramm J. Relationships of self-management abilities to loneliness among older people: a cross-sectional study. BMC Geriatrics. 2020;20:184.
Gramm JM, Twisk J, Nijboer AP. Self-management abilities and frailty are important for healthy aging among community-dwelling older people; a cross-sectional study. BMJ Geriatrics. 2014;14:28.
Steverink N, Lindenberg S, Slaets JP. How to understand and improve older people’s self-management of well-being. Eur J Ageing. 2005;2:235–44.
Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37(2):122–47.
Cramm JM, Strating MMH, de Vreede PL, Steverink N, Nieboer AP. Development and validation of a short version of the self-management ability scale (SMAS). Health Qual Life Outcomes. 2012;10:9.
Lee JW, Nersesian PV, Suen JJ, Mensah Cudjoe TK, Gill J, Stanton SL, Hlasek MD. Loneliness is associated with lower coping self-efficacy among older adults. J App Gerontol. 2023;42(2):270–9.
Balki E, Hayes N, Holland C. Effectiveness of Technology Interventions in Addressing Social Isolation, Connectedness, and Loneliness in Older Adults: Systematic Umbrella Review. JMIR Aging. 2022;5(4): e40125.
Jones RB, Ashurst EJ, Atkey J, Duffy B. Older People Going Online: Its Value and Before-After Evaluation of Volunteer Support. J Med Internet Res. 2015;17(5): e122.
Van Dijk J, Hacker K. The Digital Divide as a Complex and Dynamic Phenomenon. The Information Society. 2003;19:315–26.
Beaunoyer E, Dupere S, Guitton MJ. COVID-19 and digital inequalities: reciprocal impacts and mitigation strategies. Computers in Human Behaviour. 2020;111: 106424.
Khunti K, Platt L, Routen A, Abbasi K. Covid-19 and ethnic minorities: an urgent agenda for overdue action. BMJ. 2020;69:m2503.
Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8(6):547.
Steverink N, Lindenberg S. Which social needs are important for subjective well-being? What happens to them with aging? Psychol Aging. 2006;21:281–90.
Mulligan K, Khiung S, Bloch G, Park G, Richter A, Stebbins L, Talat S. Social Prescribing in Canada: A Tool for Integrating Health and Social Care for Underserved Communities. Healthcare Quarterly. 2023;25(4):17–22.
Makizako H, Shimada H, Doi T, Tsutsumimoto K, Hotta R, Nakakubo S, Makino K, Lee S. Social Frailty Leads to the Development of Physical Frailty among Physically Non-Frail Adults: A Four-Year Follow-Up Longitudinal Cohort Study. Int J Environ Res Public Heal. 2018;15:490.
Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Towards an integral conceptual model of frailty. J Nutr Health Aging. 2010;14(3):175–81.
Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLOS Medicine. 2010;7(7): e1000316.
Gilmour H. Social participation and the health and well-being of Canadian seniors. Health Reports, 2012;23, 4.
Choi HK, Lee SH. Trends and effectiveness of ICT interventions for the elderly to reduce loneliness: A systematic review. Healthcare. 2021;9:293.
Ožić S, Vasiljev V, Ivković V, Bilajac L, Rukavina T. Interventions aimed at loneliness and fall prevention reduce frailty in elderly urban population. Medicine (Baltimore). 2020;99(8): e19145.
Acknowledgements
The authors would like to thank Divya Mathura for her assistance in updating the scoping review.
Funding
The authors received funding for this work from the Canadian Institutes of Health Research grant (#:172657).
Author information
Authors and Affiliations
Contributions
The study was designed by MK, JHL, SS. Articles were screened by IH, JH, JM, JS, KA, LH, LP, MM, MK, data charted by IH, JS, KA, MK, JH, LP, LH, MH, data analyzed and synthesized by IH, KA, MK, BL, CM, JH, LP, MH, MT and tables and figures prepared by MK, IH and JM. All authors contributed to the interpretation of findings, and contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kastner, M., Herrington, I., Makarski, J. et al. Interventions that have potential to help older adults living with social frailty: a systematic scoping review. BMC Geriatr 24, 521 (2024). https://doi.org/10.1186/s12877-024-05096-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05096-w