Abstract
Background
With the aging population, the number of individuals with dementia in China is increasing rapidly. This community-based study aimed to investigate the prevalence and risk factors for dementia and mild cognitive impairment (MCI) among older adults in China.
Methods
In this study, 20,070 individuals aged ≥ 65 were recruited between January 1, 2022, and February 1, 2023, from ten communities in Xiamen City, China. We collected data on age, sex, level of education, and medical history, as well as global cognition and functional status. The prevalence of dementia and MCI was examined, and the risk factors for different groups were assessed.
Results
The overall prevalence of dementia and MCI was approximately 5.4% (95% confidence interval [CI], 5.1–5.7) and 7.7% (95% CI, 7.4–8.1), respectively. The results also indicated that dementia and MCI share similar risk factors, including older age, female sex, hypertension, and diabetes mellitus. Compared with individuals with no formal education, those with > 6 years of education had an odds ratio for MCI of 1.83 (95% CI, 1.49–2.25). We also found that only 5.5% of the positive participants chose to be referred to the hospital for further diagnosis and treatment during follow-up visits.
Conclusions
This study estimated the prevalence and risk factors for dementia and MCI among individuals aged ≥ 65 years in Southeast China. These findings are crucial for preventing and managing dementia and MCI in China.
Similar content being viewed by others
Background
Dementia, a common neurocognitive disorder with an insidious onset, is characterized by chronic and progressive cognitive impairment, accompanied by a decline in the ability to perform activities of daily living [1]. With an increasing aging population, the number of individuals with dementia is rapidly growing, and more than 150 million individuals worldwide are projected to have dementia by 2050 [2]. In China, approximately 10 million people currently live with dementia, and the socioeconomic cost associated with it is projected to reach $250 billion by 2020 [3]. The burden of dementia poses significant financial, social, and public health challenges worldwide. Mild cognitive impairment (MCI) is considered to be a stage between normal physiological aging and dementia, potentially progressing to dementia within 5–10 years [4]. Effective therapies for dementia are currently lacking, emphasizing the importance of primary prevention [5]. MCI is a critical interventional target for dementia. Consequently, a better understanding of MCI, including early identification, underlying etiology, risk factor definition, and available pharmacological and non-pharmacological treatments, has become an important research topic [6, 7].
Several studies have investigated the prevalence of dementia and MCI in the Chinese population. However, the results indicated significant variations across various regions of China. The findings of a cross-sectional national survey involving Chinese individuals aged ≥ 60 years indicated a prevalence of 6.0% for dementia and 15.5% for MCI [8]. Another study found the prevalence of dementia and MCI to be 8.04% and 18.76%, respectively, among Chinese individuals aged ≥ 65 years [9]. A meta-analysis reported that the prevalence of dementia in Northern China (5.4%) was higher than that in central (3.8%) and Southern China (3.7%) [10]. Furthermore, a systematic review revealed that the prevalence of MCI in Eastern China (13.14%) was lower than that in Western China (14.33%) [11]. Additionally, the risk factors for dementia have evolved over the past decade, influenced by environment, urbanization, and lifestyle changes. A previous analysis indicated that unhealthy lifestyles, including high fat intake and physical inactivity, contribute to an increased incidence of cognitive impairment [12].
In our clinical practice, we found that over 50% of the patients exhibited moderate-to-severe dementia during their initial hospital visit due to a lack of early screening [13]. Early screening and health education within communities play important roles in the early identification of dementia in older people, especially in those with limited mobility and insufficient care [14]. In community-based screening through home visits, trained professionals, such as physicians or nurses, can provide a brief cognitive assessment for the early identification of cognitive decline and improve the knowledge of preventing dementia in older adults. This study investigated the prevalence and risk factors for dementia and MCI in a large sample of individuals aged ≥ 65 years from 10 communities in Southeast China.
Methods
Participants and preparation procedure
In this cross-sectional study, we recruited participants aged ≥ 65 in Xiamen City between January 1, 2022, and February 1, 2023. We randomly selected two communities from each district (a total of ten communities) in Xiamen City. Prior to the interviews, we contacted all older people aged ≥ 65 years in this community by telephone, facilitated by community volunteers, to inquire if they were willing to participate in our survey. Subsequently, we conducted home visits to those who agreed to participate and conducted relevant interviews after obtaining signed informed consent. Four to five teams of interviewers were formed for each community, each comprising one community doctor, one community nurse, and one community staff member. Furthermore, we established a community expert panel comprising two neurologists and two neuropsychologists with expertise in cognitive impairment disorders. The expert panel and interviewers reviewed all data and assigned final diagnoses. The interviewers underwent a week-long training course covering knowledge and diagnosis of dementia and MCI, as well as assessment procedures for cognitive measurement tools. The inter-rater reliability for cognitive diagnoses and assessments needed to exceed 0.90. The expert panel conducted logic checks for inconsistencies and audits to ensure the quality of the entered data. Thus, all interviews were conducted by well-trained interviewers, with good quality control measures. The in-person interviews with the participants or their guardians were conducted at their residences through home visits. Information regarding age, sex, education level, and medical history was collected using a structured questionnaire. Thereafter, cognitive evaluations were conducted for the participants, including the Mini-Mental State Examination (MMSE) and the Clinical Dementia Rating (CDR). The functional status was assessed using the Basic Activities of Daily Living and Instrumental Activities of Daily Living scales [15]. Meanwhile, we brought portable blood pressure and blood glucose monitors to measure the participants’ blood pressure and random blood glucose levels, respectively, before the interview. Combined with medical records and testing results, when doubts about the diagnosis arose, we conducted fasting blood glucose and blood pressure exams one or two times on different days during home visits to confirm the diagnosis. Written informed consent was obtained from the participants themselves or their guardians. The study was approved by the Research Ethics Committee of the First Affiliated Hospital of Xiamen University.
Diagnosis criteria
Participants were categorized into groups representing normal cognitive function, MCI, or dementia. Normal cognitive function was defined when participants have a CDR score of 0 as well as an MMSE score > 19 for illiterate individuals, > 22 for individuals with 1–6 years of education, and > 26 for individuals with > 6 years of education. Dementia was defined when participants have a CDR score ≥ 1 as well as an MMSE score ≤ 17 for illiterate participants, ≤ 20 for participants with 1–6 years of education, and ≤ 24 for participants with > 6 years of education [16]. MCI was determined when participants have a CDR score of 0.5 as well as an MMSE score ≤ 19 for illiterate participants, ≤ 22 for participants with 1–6 years of education, and ≤ 26 for participants with > 6 years of education [17].
Statistical analysis
The prevalence of dementia or MCI, along with the 95% confidence interval (CI), was calculated for all participants and subgroups based on age, sex, and educational level. A multivariable logistic regression model was employed to identify the risk factors for dementia or MCI, including age (65–74, 75–84, and ≥ 85 years), sex, educational level, and presence of hypertension or diabetes mellitus (DM). Multivariable adjusted odds ratios (ORs), with corresponding 95% CIs, were reported. All statistical analyses were conducted using SPSS 25.0 (IBM Corp., Armonk, N.Y., USA), using two-sided statistical tests. Statistical significance was set at p < 0.05.
Results
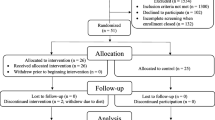
A total of 21,978 participants aged ≥ 65 years from 10 communities in Xiamen City were invited to participate in this study. Among them, 1,908 were excluded: 1,460 had incomplete or doubtful data, 293 had hearing or vision loss, and 155 withdrew their consent. Consequently, 20,070 participants were included in the final analysis. The demographic and clinical characteristics of the participants are shown in Table 1. The mean age was 73.14 ± 6.39 years, and 9,719 participants (45.7%) were males. Notably, 1,960 participants (9.8%) were uneducated, and 4,969 (24.8%) had ≤ 6 years of education. Among the 20,070 participants, we identified 1,082 (5.4%) with dementia and 1,553 (7.7%) with MCI.
The overall prevalence of dementia was estimated to be 5.4% (95% CI, 5.1–5.7). The prevalence of dementia increased with age, ranging from 3.2% (95% CI, 2.9–3.5) in the 65–74 years group to 24.5% (95% CI, 22.2–27.0) in the ≥ 85 years group (Table 2; Fig. 1). Furthermore, females, especially those in the ≥ 85 years group, demonstrated a higher prevalence of dementia than males (Table 2; Fig. 2A). The overall prevalence of MCI was 7.7% (95% CI, 7.4–8.1). Across age groups, the prevalence of MCI at 64–74 years, 75–84 years, and ≥ 85 years was 6.7%, 9.8%, and 9.6%, respectively. The results also showed that the prevalence of MCI among females aged 75–84 years was higher than that among males. In contrast, the prevalence among females aged ≥ 85 years was lower than that among males (Fig. 2B).
Table 3 shows the outcomes of the multivariable-adjusted logistic regression analyses. We found that female sex was associated with an increased risk of dementia. Compared with individuals aged 64–74 years, the OR for dementia was 2.09 (95% CI, 1.80–2.42) among those aged 75–84 years; the OR significantly increased to 10.42 (95% CI, 8.80–12.34) among those aged ≥ 85 years. Furthermore, the presence of hypertension (OR, 2.33; 95% CI, 2.05–2.65) or DM (OR, 2.32; 95% CI, 2.02–2.66) was identified as a significant risk factor for dementia. The results indicated that older age, female sex (OR, 1.22; 95% CI, 1.10–1.36), hypertension (OR, 1.66; 95% CI, 1.49–1.84), and DM (OR, 1.51; 95% CI, 1.33–1.70) were associated with an increased risk of MCI. Compared with individuals who had no formal education, the OR for MCI was 1.83 (95% CI, 1.49–2.25) among those who had received > 6 years of education. The 2,635 participants with dementia or MCI identified through screening were advised to visit the general hospital for further diagnosis and treatment. However, during follow-up visits, we observed that only 5.5% (144/2635) of the older adults with dementia or MCI opted to pursue further diagnosis and treatment at the hospital.
Discussion
Our study was based on a government project titled “Bring Tangible Benefits to the People” of Xiamen City, Fujian Province, China. The project focused on residents aged ≥ 65 years and aimed to explore the current status, including the prevalence and risk factors, of dementia and MCI in Xiamen City. According to the 2021 census, among a total population of 5.3 million in Xiamen city, 367,000 people were aged ≥ 65 years. This study enrolled 20,070 participants, constituting 5.5% of the population aged ≥ 65 years. Our results showed that the overall prevalence of dementia in Xiamen was 5.4%. A previous large-sample report for Chinese individuals aged ≥ 65 years involving 32,552 respondents in 2019 and 10,276 in 2014 indicated a 5.60% and 5.14% prevalence of dementia, respectively [18, 19]. Another study encompassing 46,011 Chinese respondents aged ≥ 60 years in 2020 reported a 6.0% prevalence of dementia [8]. Thus, the prevalence of dementia in our survey was consistent with previous findings among Chinese individuals. However, compared with the prevalence of dementia in other countries, our findings showed a significantly lower prevalence than those in Japan (11.3%) [20], Latin America and the Caribbean (10.66%) [21], South Korea (9.20%) [22], the United States (8.5%) [23], and India (7.4%) [24]. Conversely, it was higher than those reported in Benin (3.2%) [25] and Portugal (3.65%) [26]. The prevalence of dementia varies greatly among countries. Several factors were considered to contribute to these variations, such as genetic factors, sample size, diverse diagnostic criteria, and environmental risks. Moreover, we identified 1,553 individuals with MCI, yielding a prevalence of 7.7%. The prevalence of MCI ranged from 5.0 to 36.7% in different regions among individuals aged ≥ 60 years [27]. Two reports on the Chinese population aged ≥ 60 years indicated that the prevalence of MCI was 14.7% in 2018 and 15.5% in 2020 [8, 11]. Another report showed that the prevalence of MCI was 19.5% (23.4% in rural and 16.8% in urban areas) among Chinese individuals aged ≥ 65 years [28]. Our study enrolled an older and relatively less educated population. However, the estimated prevalence of dementia and MCI was lower than that of other populations outside China. This may attribute to the combined effect of multiple factors. First, it may be related to the dietary habits. The diet of the population in Southeast China is rich in vegetables, fruits, and fish, as well as low in salt and fat. Growing evidence suggests that diets rich in vegetables and low in salt and fat can be protective against cognitive decline [29]. Second, genetic factors may have contributed to these results.
Our results showed that two unmodifiable risk factors, increasing age and female sex, were associated with dementia and MCI, similar to those of another study [30]. Additionally, two modifiable risk factors, hypertension and DM, were related to dementia and MCI. Previous reports have also indicated a remarkable increase in the MCI risk among individuals with hypertension and DM [31]. Another meta-analysis suggested that DM resulted in gray matter atrophy and accelerated brain aging [32]. Moreover, hypertension and DM are associated with amyloid-β burden and contribute to the pathophysiology of MCI [33]. To date, no effective medical treatment is available for MCI. Therefore, interventions targeting modifiable risk factors are particularly crucial for preventing cognitive deterioration. Healthy lifestyles and regular use of medications to manage hypertension and DM were considered to lower the risk of developing cognitive decline [34, 35]. Meanwhile, contrary to previous studies, our results indicated that the OR for MCI in the population that had received > 6 years of education was higher than that in the population that had received no formal education. No direct correlation has been established between education level and cognitive impairment. However, individuals with higher levels of education may possess stronger learning, thinking, and problem-solving abilities. Nonetheless, highly educated individuals may experience more negative affective states, such as anxiety and depression, or have more unhealthy lifestyle habits, which may also increase the risk of cognitive impairment.
While we maintained scientific rigor throughout this study, we acknowledge several limitations. First, despite enrolling over 20,000 older people in Xiamen City, conducting similar research in more cities across Southeast China would enhance the credibility and comprehensiveness of our findings. Second, we did not classify dementia according to its etiology, such as vascular dementia or Alzheimer’s disease. Finally, compared with previous large-scale studies conducted in China, we chose two possible modifiable risk factors for analysis. At the outset of the in-person interviews, we collected the participant’s personal and medical histories, such as hypertension, DM, hyperlipidemia, heart disease, and smoking and drinking habits. However, as the interviews progressed, we discovered through quality analysis that much of the information provided by the participants was unreliable. For instance, the reliability of hyperlipidemia data was compromised due to the lack of recent blood lipid level test results for many participants in hospital records. Additionally, most participants refused to go to the hospital for examination. Therefore, we utilized portable blood pressure and glucose monitors to test the blood pressure and blood glucose levels, respectively, of the participants for the determination of hypertension and diabetes diagnoses. Furthermore, due to the older age of the participants, the information regarding their lifestyle issues was often inaccurate and ambiguous. To ensure the reliability and authenticity of the data, we chose to focus our data collection and analysis on stable and reliable factors, such as hypertension and DM.
During follow-up visits, we discovered that only 5.5% (144/2635) of the older adults with dementia or MCI opted to pursue further diagnosis and treatment at the hospital. This low referral rate among positive participants may be attributed to several reasons. One possible reason is the impact of the coronavirus disease pandemic, as patients and their family members may have feared contracting the virus when visiting the hospital. Some individuals may consider amnesia or cognitive dysfunction to be a normal aging process; hence, they were reluctant to seek medical attention. Additionally, education and knowledge about dementia and MCI have not been widely disseminated, posing challenges for family members in recognizing the detrimental effects and prognosis of cognitive impairment. Recommendations have been made to improve the referral rate of patients with cognitive impairment from the community. First, specialists in cognitive disorders from general hospitals should conduct more lectures and presentations on dementia or MCI to train doctors in the community. Moreover, government departments should implement more science education initiatives in the community to raise public awareness of cognitive disorders.
Conclusions
The estimated prevalence of dementia and MCI was 5.4% and 7.7%, respectively, among individuals aged ≥ 65 years in Southeast China. Meanwhile, our results indicated that dementia and MCI share similar risk factors, including older age, female sex, hypertension, and DM. Additionally, only 5.5% of the positive participants opted for referral to the hospital for further diagnosis and treatment during follow-up visits. These findings are crucial for preventing and managing dementia and MCI in China.
Data availability
The data are available from the corresponding author upon reasonable request.
Abbreviations
- MCI:
-
Mild cognitive impairment
- MMSE:
-
Mini-Mental State Examination
- CDR:
-
Clinical Dementia Rating
- ADL:
-
Activities of Daily Living
- DM:
-
Diabetes Mellitus
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Ji D, Chen WZ, Zhang L, Zhang ZH, Chen LJ. Gut microbiota, circulating cytokines and dementia: a mendelian randomization study. J Neuroinflammation. 2024;21(1):2.
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105–25.
Jia J, Wei C, Chen S, Li F, Tang Y, Qin W, et al. The cost of Alzheimer’s disease in China and re-estimation of costs worldwide. Alzheimers Dement. 2018;14(4):483–91.
Prestia A, Caroli A, van der Flier WM, Ossenkoppele R, Van Berckel B, Barkhof F, et al. Prediction of dementia in MCI patients based on core diagnostic markers for Alzheimer disease. Neurology. 2013;80(11):1048–56.
Grande G, Qiu C, Fratiglioni L. Prevention of dementia in an ageing world: evidence and biological rationale. Ageing Res Rev. 2020;64:101045.
Hafdi M, Hoevenaar-Blom MP, Richard E. Multi-domain interventions for the prevention of dementia and cognitive decline. Cochrane Database Syst Rev. 2021;11(11):CD013572.
Tao QQ, Cai X, Xue YY, Ge W, Yue L, Li XY, et al. Alzheimer’s disease early diagnostic and staging biomarkers revealed by large-scale cerebrospinal fluid and serum proteomic profiling. Innov (Camb). 2024;5(1):100544.
Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. 2020;5(12):e661–71.
Sun Y, Lee HJ, Yang SC, Chen TF, Lin KN, Lin CC, et al. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PLoS ONE. 2014;9(6):e100303.
Wu YT, Ali GC, Guerchet M, Prina AM, Chan KY, Prince M, et al. Prevalence of dementia in mainland China, Hong Kong and Taiwan: an updated systematic review and meta-analysis. Int J Epidemiol. 2018;47(3):709–19.
Xue J, Li J, Liang J, Chen S. The prevalence of mild cognitive impairment in China: a systematic review. Aging Dis. 2018;9(4):706–15.
Zhang YR, Xu W, Zhang W, Wang HF, Ou YN, Qu Y, et al. Modifiable risk factors for incident dementia and cognitive impairment: an umbrella review of evidence. J Affect Disord. 2022;314:160–7.
Lohmeyer JL, Alpinar-Sencan Z, Schicktanz S. Attitudes towards prediction and early diagnosis of late-onset dementia: a comparison of tested persons and family caregivers. Aging Ment Health. 2021;25(5):832–43.
Hugo J, Ganguli M. Dementia and cognitive impairment: epidemiology, diagnosis, and treatment. Clin Geriatr Med. 2014;30(3):421–42.
Jiang B, Zhou J, Li HL, Chen YG, Cheng HR, Ye LQ, et al. Mutation screening in Chinese patients with familial Alzheimer’s disease by whole-exome sequencing. Neurobiol Aging. 2019;76:e21515–21.
Li H, Jia J, Yang Z. Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis. 2016;53(2):487–96.
Jia X, Wang Z, Huang F, Su C, Du W, Jiang H, et al. A comparison of the Mini-mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for mild cognitive impairment screening in Chinese middle-aged and older population: a cross-sectional study. BMC Psychiatry. 2021;21(1):485.
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–24.
Jia J, Wang F, Wei C, Zhou A, Jia X, Li F, et al. The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. 2014;10(1):1–9.
Ohara T, Hata J, Yoshida D, Mukai N, Nagata M, Iwaki T, et al. Trends in dementia prevalence, incidence, and survival rate in a Japanese community. Neurology. 2017;88(20):1925–32.
Ribeiro F, Teixeira-Santos AC, Caramelli P, Leist AK. Prevalence of dementia in Latin America and Caribbean countries: systematic review and meta-analyses exploring age, sex, rurality, and education as possible determinants. Ageing Res Rev. 2022;81:101703.
Kim YJ, Han JW, So YS, Seo JY, Kim KY, Kim KW. Prevalence and trends of dementia in Korea: a systematic review and meta-analysis. J Korean Med Sci. 2014;29(7):903–12.
Hudomiet P, Hurd MD, Rohwedder S. Trends in inequalities in the prevalence of dementia in the United States. Proc Natl Acad Sci U S A. 2022;119(46):e2212205119.
Lee J, Meijer E, Langa KM, Ganguli M, Varghese M, Banerjee J, et al. Prevalence of dementia in India: national and state estimates from a nationwide study. Alzheimers Dement. 2023;19(7):2898–912.
Adoukonou T, Yoro-Zohoun I, Gnonlonfoun DD, Amoussou P, Takpara C, Agbetou M, et al. Prevalence of dementia among well-educated old-age pensioners in Parakou (Benin) in 2014. Dement Geriatr Cogn Disord. 2020;49(2):210–8.
Gonçalves-Pereira M, Cardoso A, Verdelho A, Alves da Silva J, Caldas de Almeida M, Fernandes A, et al. The prevalence of dementia in a Portuguese community sample: a 10/66 Dementia Research Group study. BMC Geriatr. 2017;17(1):261.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
Jia J, Zhou A, Wei C, Jia X, Wang F, Li F, et al. The prevalence of mild cognitive impairment and its etiological subtypes in elderly Chinese. Alzheimers Dement. 2014;10(4):439–47.
Dominguez LJ, Veronese N, Vernuccio L, Catanese G, Inzerillo F, Salemi G, et al. Nutrition, physical activity, and other lifestyle factors in the prevention of cognitive decline and dementia. Nutrients. 2021;13(11):4080.
Lavrencic LM, Delbaere K, Broe GA, Daylight G, Draper B, Cumming RG, et al. Dementia incidence, APOE genotype, and risk factors for cognitive decline in Aboriginal australians: a longitudinal cohort study. Neurology. 2022;98(11):e1124–36.
Zhang Y, Chen SD, Deng YT, You J, He XY, Wu XR, et al. Identifying modifiable factors and their joint effect on dementia risk in the UK Biobank. Nat Hum Behav. 2023;7(7):1185–95.
Antal B, McMahon LP, Sultan SF, Lithen A, Wexler DJ, Dickerson B, et al. Type 2 diabetes mellitus accelerates brain aging and cognitive decline: complementary findings from UK Biobank and meta-analyses. Elife. 2022;11:e73138.
van Arendonk J, Neitzel J, Steketee RME, van Assema DME, Vrooman HA, Segbers M, et al. Diabetes and hypertension are related to amyloid-beta burden in the population-based Rotterdam Study. Brain. 2023;146(1):337–48.
Kasper S, Bancher C, Eckert A, Förstl H, Frölich L, Hort J, et al. Management of mild cognitive impairment (MCI): the need for national and international guidelines. World J Biol Psychiatry. 2020;21(8):579–94.
Zhang XX, Tian Y, Wang ZT, Ma YH, Tan L, Yu JT. The epidemiology of Alzheimer’s disease modifiable risk factors and prevention. J Prev Alzheimers Dis. 2021;8(3):313–21.
Acknowledgements
The authors extend their sincere gratitude to all participants for their support and willingness to participate in this study.
Funding
This work was supported by grants from the Medical and Health Guiding Project of Xiamen City to Bin Jiang (No. 3502Z20214ZD1014), the Natural Science Foundation of Fujian Province to Bin Jiang (No. 2022J011359), and the Medical and Health Guiding Project of Xiamen City to Qi Liu (No. 3502Z20224ZD1013).
Author information
Authors and Affiliations
Contributions
B.J., Q.L., and JP.L., drafted and revised the manuscript. SN.L., HJ.W., ZW.Y., and J.W., acquired and analyzed the data. W.Z., JH.T., CH.C., and FY.L., acquired and interpreted the data. M.B., NA.X., and KM.Z., contributed to the design of the work and provided study supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was provided by the Research Ethics Committee of the First Affiliated Hospital of Xiamen University. Written informed consent was obtained from the participants themselves or their guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, B., Liu, Q., Li, JP. et al. Prevalence and risk factors for dementia and mild cognitive impairment among older people in Southeast China: a community-based study. BMC Geriatr 24, 466 (2024). https://doi.org/10.1186/s12877-024-05054-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05054-6