Abstract
Background
In aged society, health policies aimed at extending healthy life expectancy are critical. Maintaining physical activity is essential to prevent the deterioration of body functions. Therefore, it is important to understand the physical activity levels of the target age group and to know the content and intensity of the required physical activity quantitatively. Especially we focused the role of non-exercise activity thermogenesis and sedentary time, which are emphasized more than the introduction of exercise in cases of obesity or diabetes.
Methods
A total of 193 patients from 25 institutions were included. Participants underwent a locomotive syndrome risk test (stand-up test, 2-step test, and Geriatric Locomotive Function Scale-25 questionnaire) and were classified into three stages. Physical activity was quantitatively monitored for one week with 3-axial accelerometer. Physical activity was classified into three categories; (1) Sedentary behavior (0 ∼ ≤ 1.5 metabolic equivalents (METs)), (2) Light physical activity (LPA:1.6 ∼ 2.9 METs), and (3) Moderate to vigorous physical activity (MVPA: ≥3 METs). We investigated the relationship between physical activity, including the number of steps, and the stages after gender- and age- adjustment. We also investigated the relationship between social isolation using Lubben’s Social Network Scale (LSNS), as social isolation would lead to fewer opportunities to go out and less outdoor walking.
Results
Comparison among the three stages showed significant difference for age (p = 0.007) and Body Mass Index (p < 0.001). After gender-and age-adjustment, there was a significant relation with a decrease in the number of steps (p = 0.002) and with MVPA. However, no relation was observed in sedentary time and LPA. LSNS did not show any statistically significant difference. Moderate to high-intensity physical activity and the number of steps is required for musculoskeletal disorders. The walking, not sedentary time, was associated to the locomotive stages, and this finding indicated the importance of lower extremity exercise.
Conclusions
Adjusting for age and gender, the number of steps and moderate to vigorous activity levels were necessary to prevent worsening, and there was no effect of sedentary behavior. Merely reducing sedentary time may be inadequate for locomotive disorders. It is necessary to engage in work or exercise that moves lower extremities more actively.
Similar content being viewed by others
Background
In aged society, health policies aimed at extending so-called “healthy life expectancy” are essential [1]. A main contributing factor is increasing or at least maintaining the physical activity of the target age group. Physical activity is vital for maintaining the quality of life of older adults. Many studies have explored this topic and reported the importance of physical activity in reducing the deterioration of multiple body functions, mainly for motor functions, but also for many other bodily functions [2].
Recently, great progress has been made in our understanding of physical activity, and quantitative measurements of physical activity have garnered attention. However, unlike the dosage and usage of drugs, the required content of applicable programs that modify lifestyles or physical activity has not yet been identified. Therefore, it is vitally important to quantitatively understand the details of the physical activity levels of the target age group and the content to which they can be improved their health level [3].
There are many methods for measuring the amount of physical activity, but none of them individually enables optimal detection of all facets of physical activity. Therefore, a multimodal, combined approach of self-reported and device-based methods, such as questionnaires and accelerometers, is recommended [4, 5].
Whether the total energy expenditure is high or low depends on physical activity [6]. Physical activity excluding resting metabolic rate and meal-induced thermogenesis can be further divided into exercise and non-exercise activity thermogenesis (NEAT), which refers to the energy consumed in daily activities that are not considered as exercises [7, 8]. Most of the physical activity is NEAT as a reality, which corresponds to daily life activities such as housework, office work, standing, sitting, and climbing stairs in a short period of time rather than exercise itself.
In recent years, the role of NEAT has attracted attention when discussing the amount of physical activity [7, 9]. NEAT-level energy consumption greatly affects physical activity related to obesity or diabetes, so we focused on relationship between such sedentary behavior and the degree of locomotive disorders.
The ultimate aim of our study as a prospective cohort is to quantify the minimal level of physical activity required using quantitative measurement of daily physical activity. However, in the current study using the baseline data of the participants, we tried to examine the situation of people with locomotive problems by quantitatively measuring physical activity.
Rather than simply aiming to increase physical activity, we set as a hypothesis that lifestyle improvements such as a decrease in sedentary time and a reduction in social isolation, as described in DM, etc., might have a significant impact on locomotive disorders.
The purpose of the study was to examine the relationship between (A) quantitative measurement of physical activities using 3-axial accelerometer and social isolation check with a questionnaire and (B) locomotive syndrome stages by motor function tests and GLFS-25 questionnaire.
Methods
This study was originally part of a prospective cohort, and a cross-sectional study using the baseline data.
Participants
Participants were recruited as outpatients from 25 facilities attended by the members of the Japanese Clinical Orthopedic Association (See Acknowledgements). Participants were recruited from March to July 2022.
Inclusion criteria
-
1.
Age; more than 50 years old; both gender.
-
2.
Outpatients of orthopedic clinics under orthopedic management.
-
3.
Able to complete the locomotive syndrome risk test (stand-up test, 2-step test, and the Geriatric Locomotive Function Scale-25 (GLFS-25) questionnaire).
-
4.
Consent to measure the physical activity with a 3 -axis accelerometer for one week.
The locomotive syndrome risk test was performed on the day the participant visited the medical facilities, and 3-axial accelerometer data were measured in the following one week.
Exclusion criteria
-
1.
Inability to stand up from a chair or bed.
-
2.
Disability in walking or locomotion because of brain disease requiring treatment at the time of entry.
-
3.
Severe pulmonary, renal, coronary, or hepatic disease.
-
4.
Mental illness.
-
5.
Past history of stroke within the preceding 6 months.
-
6.
Past history of myocardial infarction within the preceding 6 months.
-
7.
Past history of fracture of a lower extremity within the preceding 6 months.
-
8.
Current treatment for acute trauma.
-
9.
Other reasons determined by the attending physician.
Physical activity sensor system
Device: 3-axial accelerometer
A 3-axial accelerometer (Active style Pro HJA-750 C; OMRON Co., Kyoto, Japan) was used in this study. The data logger held the memory stock and then analyzed the body movement using an application program, which is a unique algorithm of data processing to distinguish between walking and daily activities [10, 11] (Fig. 1).
The device extracted daily activity records and separated a total of 12 types of activities; comprising five types of daily activities like dish washing and seven types of walking/running activities including ascending/descending stairs. In addition, in the discrimination method, the acceleration detected on each axis is passed through a high-pass filter to cut the low frequency range of less than 0.7 Hz., and the cut off value for discrimination of household and locomotive activities was set at 1.16 of the ratios of unfiltered to filtered total acceleration. It has been reported that the device enables to almost 98.7% correct discrimination [11].
Data acquisition and analysis
The device detected acceleration at 32 Hz and estimated Metabolic Equivalents (METs) from the average synthetic acceleration every 1 min. This information, output from the software created by the manufacturer was used as a quantitative measurement of daily activity and its content according to total energy consumption. We treat a 0 METs as not detected acceleration (no movement for 1 min); namely sitting and motionless, rather than not wearing the device. Sixty minutes or more of continuous non-activity (0 METs) is included not in sedentary time but in non-wearing time.
The parameters obtained were walking expressed as the number of steps and the time in minutes (finally converted to METs hour) of the categorized physical activity levels.
The algorithm classified accelerometric data into the following three categories; one sedentary time and two physical activities.
-
Sedentary behavior (min): 0 ∼ ≤ 1.5 METs.
-
Light physical activities (LPA: METs hour): 1.6 ≤ ∼ ≤ 2.9 METs.
-
Moderate to vigorous physical activity (MVPA: METs hour): 3 ≤ ∼ METs.
Physical activity monitors cannot detect posture itself but rather detect movement and estimate the amount of exercise. Therefore, it is not strictly possible to tell whether 1.5 METs or less with accelerometer is sitting or not. Time with very low levels of activity that do not involve movement is measured as sedentary time. Since the calculated amount of physical activity for sitting may be 0 METs, it cannot be expressed in units of hour, and expressed in min.
In the measurement of activity in this study, sedentary time includes 0 METs and is considered inactive time, although this does not necessarily mean sedentary time in the strict sense. In other words, sitting is considered physical inactivity, and LPA or above is considered physical activity.
Sensor measuring method
The device was attached vertically at the right pelvic region of the participants and maintained for the entire day except while sleeping and taking a bath.
After wearing the accelerometer for one week, the device was collected by their attending physicians. Confirming the recording status/min, the data that fulfilled the required wearing time; (≥ 400 min/day and ≥ 5 days/week) were used for analysis.
In this study data acceptance condition was set to 400 min/day, which is slightly less than 10 h/day previously used [12]. It is because there were several dropouts in those with locomotive syndrome stage 3 from a previous pilot study, we set in to collect data even if the amount of activity is low.
Participants were requested to log their activities as a diary to improve adherence and quickly respond to equipment problems such as battery failure.
Assessment for locomotive function
The GLFS-25 is a self-administered questionnaire consisting of 25 items [13]. These 25 items are graded on a 5-point scale from no impairment (0 points: not difficult to do) to severe impairment (4 points: difficult to perform), and then arithmetically added to produce a total score (minimum 0 and, maximum 100).
Participants were requested to complete the GLFS-25 questions. The reliability and validity of the GLFS-25 have been certified [13], and the national standard value of the GLFS-25 score has already been reported [14].
Based on the measured locomotive syndrome risk tests, the corresponding GLFS-25 scores were assigned to Locomotive syndrome stage 1, 2, and 3 and stage 0 (reference stage) [15].
-
(Locomotive syndrome stage 0 = GLFS-25 score: ≤6)
-
Locomotive syndrome stage 1 = GLFS-25 score: 7 ∼ 15.
-
Locomotive syndrome stage 2 = GLFS-25 score: 16 ∼ 23.
-
Locomotive syndrome stage 3 = GLFS-25: score ≥ 24.
Social isolation
Lubben’s Social Network Scale (LSNS) [16] shortened Japanese version [17], which is validated by a group of Japanese researchers, was used to assess social isolation. On Lubben’s scale, a cut-off value of < 12 points indicated social isolation [16].
Statistical analysis
The t-test and analyses of variance were performed for comparison of means among two groups and three groups, respectively. Fisher’s exact test was performed for comparison of proportions. Analysis of covariance method was conducted for calculating gender- and age- adjusted means and their comparisons. The Tukey-Kramer method was used for multiple comparisons of each pair of means among three groups. Linear regression is used for trend testing of continuous variables (means), and logistic regression is used for trend testing of binary variables (proportions) as trend tests.
Since Fisher’s exact test does not always require an approximation to a chi-square distribution, we considered the exact test to be the best analysis for our sample size.
Data analyses were performed using SAS, version 9.4. Software (SAS Institute, Cary, NC, USA).
Results
Demographic data of the participants
A total 193 participants (men: 45, women: 148; age distribution: 52 ∼ 90 years old) joined in this study. However, three did not have complete data, one case was against the age requirement, and out of the remaining 189 participants, five were classified as locomotive syndrome stage 0; therefore, physical activity was analyzed for 184 cases, considering the current study aim.
The locomotive grade categories were distributed as follows: Locomotive syndrome stage 1 (n = 63: mean age: 71.6 years (SD = 7.9 years)), stage 2 (n = 62: 73.9 (SD = 8.1)), stage 3 (n = 59: 76.2 (SD = 8.0)).
GLFS-25 scores compared to the national norm
Figure 2 shows the distribution of participants in this study on the GLFS-25 national norm by gender. Our sample is like the national norm in terms of the degree of locomotive function, and it is the age group where symptoms start to become apparent in terms of age.
Standing position of the current samples in the national standard values of GLFS-25. National standard values of the GLFS-25 Standing position of the current samples. (taken from reference #14 with permission). The figure shows the distribution of participants according to the GLFS-25 national norm by gender
Analyses among locomotive categories
There is no significant difference between gender and locomotive syndrome stage according to Fisher’s exact test (p = 0.904), but increasing age has a significant difference with the stages (p = 0.007) (Table 1).
Analysis was conducted for calculating gender- and age-adjusted means and their comparisons among locomotive syndrome stages. There were significant differences in body weight (p = 0.015) and Body Mass index (p = < 0.001) between locomotive syndrome stage 1 and stages 2 or 3 (Table 1). Weight gain indicates the progress of mobility function decline.
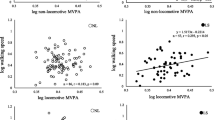
The worsening locomotive syndrome stage was significantly related to a decrease in the numbers of steps (p = 0.002). Sedentary activity (activity of 0 ∼ 1.5 METs) was not significantly associated to the locomotive syndrome stages (p = 0.240).
On the other hand, there are different trends in the amount of physical activity in terms of activity categories; the analysis of covariance gave a p-value of 0.056, but the trend test gave a p-value of 0.016, and the multiple comparisons among the locomotive syndrome stages was statistically significant for MVPA, but not significant for LPA (p = 0.654) (Table 2).
Adjusting for age and gender, the number of steps and moderate to vigorous activity (MVPA) levels were related to worsening of locomotive syndrome stages, but there was no effect of sedentary behavior.
Social isolation was observed in 50 participants, but not identified in 134. There were no differences in age (Welch’s t-test) and gender (Fisher’s exact test).
There was no difference in the physical activity categories, and the number of steps yielded also no statistical difference (Table 3).
Social isolation assessed by LSNS did not show any statistically significant difference among physical activity level.
Discussion
Contrary to the study’s hypothesis, reducing sedentary time or social isolation do not related to locomotive syndrome stages. It seems that different interventions from obesity or diabetes are required for locomotive function. Ensuring that the number of steps and the amount of activity above a certain level of intensity could lead to improvement of the stages.
Based on these results, the following considerations may be necessary to interpret our results.
Significance of non-exercise activity thermogenesis (NEAT) in physical activity
Generally, total daily energy expenditure can be divided into three main components; basal metabolic rate (approximately 60% or 50 ∼ 70%), diet-induced thermogenesis (approximately 10%), and the cost of physical activity (approximately 30% or 20 ∼ 40%), both heat-produced exercise (planned) and NEAT (unplanned) [18, 19].
The basal metabolic rate depends on body size, and diet-induced thermogenesis depends on dietary intake; therefore, intra-individual variability is low. But individual differences in NEAT were very large, and physical activities other than walking were performed more frequently than walking itself.
Activities that fall under NEAT are considered to have an intensity of exercise of “less than 3 METs” [18], so we focused on sitting time, light physical activity, and the degree of locomotion.
Even if we do not exercise regularly, we can engage in a lot of physical activity, such as housework or any activity other than sedentary time [19]. Therefore, social isolation or loneliness must be considered in terms of physical activity [20].
Walking (numbers of steps) and sedentary behavior
Sedentary behavior or sitting duration is closely related to obesity and other risk factors for metabolic abnormalities as well as social participation [21]. Traditionally, walking (number of steps) has been treated as an easy-to-understand index that represents the amount of physical activity. However, the concept of NEAT emphasizes the importance of more diverse activities, such as housework.
The method of evaluating physical activity and sedentary behavior using accelerometers has enabled the division of activity time by intensity (e.g., METs for sedentary behavior, LPA, and MVPA) as the equipment progresses [22].
LPA in daily life and sedentary behavior account for much of the activity time during the day and LPA is expected to affect health. In addition, the longer the duration of LPA, the shorter the sedentary time, indicating a trade-off. Accurate evaluation of LPA is important to determine the actual state of physical activity and sedentary behavior [23].
It has been reported recently that patients with metabolic syndrome can improve their status by changing their sitting time to other activities, even if they do not exercise [19, 24].
However, the results of our study were correlated with step count and moderate to vigorous physical activity, which are suggesting that different approaches may be required to manage locomotor disorders and metabolic syndromes. It is necessary to engage in the exercises that moves the lower extremities more actively than only altering behaviors or habits.
Categorization of physical activity in accelerometer measurement and its accuracy
Quantitative assessment of physical activity has been widely applied, especially in epidemiological research on obesity and diabetes. Because questionnaire surveys cannot adequately capture such inter-individual differences, epidemiological studies should use objective and accurate methods such as accelerometers [25]. However, as already mentioned, the accuracy of measurements is highly dependent on the analysis algorithm used [26].
Several reports indicate that inconsistent results among various devices are inevitable; underestimated or overestimated [27]. It has been highlighted that a single estimation formula based on the number of counts has limitations [28, 29]. Moreover, it has been reported that machine learning can measure energy consumption and physical activity duration for each intensity more accurately than conventional methods that convert acceleration data (number of counts) into energy consumption [30, 31]. An attempt was also made to use the pattern recognition method of machine learning classification [31].
It might be necessary to use rigorous experiment of exercise metabolism using such high-technology to determine the threshold of METs for locomotive syndrome.
Limitation of the study
This is a study to analyze the baseline data as part of a prospective cohort study. We conducted a one-week quantitative physical activity survey, which is basically a cross-sectional study. This research is not a rigorous measurement experiment but multi-person measurement data in the field to find the current status. At this moment the determination of a necessary activity level is not established yet.
As another important limitation of accelerometer, it is difficult to divide standing and sitting properly [23]. We would expect that many elderly people spend their work time sitting like desk work of office workers. And current available sensor is not waterproof and unable to record swimming, or aqua exercise, or bathing. Probably the technology could be advanced, but the challenge is whether the acceleration can be well measured to distinguish sitting from standing postures.
It is reported that physical activity fluctuates seasonally [32], and this survey was conducted in the spring to summer, and therefore, did not include snowy winter. In addition, there is a possibility that the opportunity to go out and behavior patterns have changed due to the COVID-19 pandemic. These issues should be considered in future research.
Participants’ orthopedic diagnosis was not examined at this time. We knew the diagnoses (often multiple) of participants under health insurance, but did not know which diseases were active at the time of participation, and we did not control the diagnosis in the study. The status of participants’ locomotor function is compared with the national norm of GLFS-25.
Conclusions
Comparison among the three stages showed significant difference for age and Body Mass Index. Adjusting for age and gender, the number of steps and moderate to vigorous activity levels were required to prevent worsening, and there was no effect of sedentary behavior.
Merely reducing sedentary time or altering behaviors, which are able to improve glucose metabolism, may be inadequate for locomotive disorders. It is necessary to engage in work or exercise that moves lower extremities more actively.
Data availability
The corresponding author has full access to all study data and assumes final responsibility for the decision to submit for publication. Additional data are available via e-mail: akai-masami@iuhw.ac.jp.
Abbreviations
- ADL:
-
Activities of daily living
- GLFS-25:
-
Geriatric Locomotive Function Scale-25
- LSNS:
-
Lubben’s Social Network Scale
- LPA:
-
Light physical activity
- METs:
-
Metabolic equivalents
- MVPA:
-
Moderate to vigorous physical activity
- NEAT:
-
Non-exercise activity thermogenesis
- SD:
-
Standard deviation
- SE:
-
Standard error
References
Healthy life expectancy extension plan. Ministry of Health, Labor and Welfare (mhlw.go.jp) (in Japanese). https://www.mhlw.go.jp/content/12601000/000514142.pdf. Accessed 29 November 2023.
World Health Organization. Global recommendations on physical activity for health. Genève: World Health Organization. 2010. https://www.who.int/publications/i/item/9789241599979. Accessed 29 November 202
Wen CP, Wai JPM, Tsai MK, Yang YC, Cheng TYD, Lee M-C, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378(9798):1244–53.
Freedson P, Bowles HR, Troiano R, Haskell W. Assessment of physical activity using wearable monitors: recommendations for monitor calibration and use in the field. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S1–4.
Matthews CE, Hagströmer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S68–76.
Westerterp KR. Exercise, energy balance and body composition. Eur J Clin Nutr. 2018;72(9):1246–50.
Levine JA, Eberhardt NL, Jensen MD. Role of nonexercise activity thermogenesis in resistance to fat gain in humans. Science. 1999;283(5399):212–4.
Levine JA, Lanningham-Foster LM, McCrady SK, Krizan AC, Olson LR, Kane PH, et al. Interindividual variation in posture allocation; possible role in human obesity. Science. 2005;307(5709):584–6.
Wijndaele K, Westgate K, Stephens SK, Blair SN, Bull FC, Chastin SFM, et al. Utilization and harmonization of adult accelerometry data: review and expert consensus. Med Sci Sports Exerc. 2015;47(10):2129–39.
Oshima Y, Kawaguchi K, Tanaka S, Ohkawara K, Hikihara Y, Ishikawa-Takata K, et al. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture. 2010;31(3):370–4.
Ohkawara K, Oshima Y, Hikihara Y, Ishikawa-Takata K, Tabata I, Tanaka S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br J Nutr. 2011;105(11):1681–91.
Honda T, Narazaki K, Chen T, Nishiuchi H, Nofuji Y, Matsuo E, et al. Association between tri-axial accelerometer-derived sedentary time and obesity in a Japanese community-dwelling older population (in Japanese). Res Exerc Epidemiol. 2014;16(1):24–33.
Seichi A, Hoshino Y, Doi T, Akai M, Tobimatsu Y, Iwaya T. Development of a screening tool for risk of locomotive syndrome in the elderly: the 25-question geriatric locomotive function scale. J Orthop Sci. 2012;17(2):163–72.
Yamada K, Ito YM, Akagi M, Chosa E, Fuji T, Hirano K, et al. Reference values for the locomotive syndrome risk test quantifying mobility of 8681 adults aged 20–89 years: a cross-sectional nationwide study in Japan. J Orthop Sci. 2020;25(6):1084–92.
Locomotive syndrome risk test. Geriatric locomotive function scale – 25. Locomotive Syndrome Prevention Awareness Official Site by the Japanese Orthopedic Association (in Japanese). https://locomo-joa.jp/check/test/locomo25.html. Accessed 29 November 2023.
Lubben JE, Blozik E, Gillmann G, Iliffe S, von Renteln Kruse W, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46(4):503–13.
Kurimoto A, Awata S, Ohkubo T, Tsubota-Utsugi M, Asayama K, Takahashi K, et al. Reliability and validity of the Japanese version of the abbreviated Lubben Social Network Scale. Nippon Ronen Igakkai Zasshi (Japanese J Geriatrics) (in Japanese). 2011;48(2):149–57.
Ravussin E, Bogardus C. A brief overview of human energy metabolism and its relationship to essential obesity. Am J Clin Nutr. 1992;55(1):S242–5.
Ravussin E. A NEAT way to control weight? Science. 2005;307(5709):530–1.
Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013;110(15):5797–801.
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk of disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32.
Yonemoto K, Honda T, Kishimoto H, Yoshida D, Hata J, Mukai N, et al. Longitudinal changes of physical activity and sedentary time in the middle-aged and older Japanese population: the Hisayama Study. J Phys Act Health. 2019;16(2):165–71.
Honda T, Chen S, Yonemoto K, Kishimoto H, Chen T, Narazaki K, et al. Sedentary bout durations and metabolic syndrome among working adults: a prospective cohort study. BMC Public Health. 2016;16(1):888.
Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–13.
Dohrn I-M, Gardiner PA, Winkler E, Welmer A-K. Device-measured sedentary behavior and physical activity in older adults differ by demographic and health-related factors. Eur Rev Aging Phys Act. 2020;17:8.
Sasai H, Hikihara Y, Okazaki K, Nakata Y, Ohkawara K. Overview of physical activity assessments by accelerometer-based activity monitors and their potential application for physical activity promotion. (in Japanese). Res Exerc Epidemiol. 2015;17(1):6–18.
Dyrstad SM, Hansen BH, Holme IM, Anderssen SA. Comparison of self-reported versus accelerometer-measured physical activity. Med Sci Sports Exerc. 2014;46(1):99–106.
Migueles JH, Cadenas-Sanchez C, Ekelund U, Delisle Nyström C, Mora-Gonzalez J, Löf M, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–45.
Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64.
Ellis K, Kerr J, Godbole S, Staudenmayer J, Lanckriet G. Hip and wrist accelerometer algorithms for free-living behavior classification. Med Sci Sports Exerc. 2016;48(5):933–40.
Kerr J, Patterson RE, Ellis K, Godbole S, Johnson E, Lanckriet G, et al. Objective assessment of physical activity: classifiers for public health. Med Sci Sports Exerc. 2016;48(5):951–7.
Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JH, Blair SN, et al. Patterns of sedentary behavior in US Middle-Age and older adults: the REGARDS Study. Med Sci Sports Exerc. 2016;48(3):430–8.
Acknowledgements
We thank all the attending physicians, their staffs, and patients who willingly participated in this study. The following 25 hospitals and clinics were involved in this project; Arai Orthopedics, Gomibuchi Orthopedic Clinic, Hasegawa Orthopedic Clinic, Hashiguchi Orthopedic Clinic, Higashi Sapporo Ooyama Orthopedics, Kato Orthopedics, Kawamura Orthopedics, Kigawa Clinic, Kijima Central Hospital, Kita Chiba Orthopedic Makuhari Clinic, Kuga Clinic, Kunisaki Orthopedics, Matubara Rheumatology and Orthopedics, Mirai Tana orthopedic Clinic, Murai Orthopedics, Narushima Orthopedic Clinic, Nikaidou Clinic, Nishimoto Orthpedics, Okumura Orthopedics, Ono Orthopedic Clinic, Sameshima Orthopedics, Tachibana Orthopedics, Tanabe Orthopedic Clinic, Watanabe Orthopedic Clinic, Yourou Orthopedic Clinic.
Funding
This study was a part of the 2020 Special project of the Japanese Society for Musculoskeletal Medicine (Recipient: Hideki Tanabe). The fund provided mainly served to cover the fees for consumable research supplies, such as accelerometers.
Author information
Authors and Affiliations
Contributions
All authors designed, conducted, analyzed, interpreted the present study, and participated in the data analysis and reporting stage of this manuscript. The corresponding author attests that all listed authors meet the authorship criteria and that any others meeting the criteria have not been omitted. HT, KH, and MA prepared the study protocols. HT received funding, and organized the study network, recruited the participants, and measured the outcome in their outpatient clinics. KY performed the data analysis. MA prepared the first draft, and all authors contributed to the writing, and have seen and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research regulations, and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all participants, and the Institutional Review Board of the Japanese Clinical Orthopedic Association (#2021-01) approved all study protocols.
Consent for publication
Not applicable. The manuscript contains neither identifiable information nor images of participants. This paper has not been published elsewhere nor is under consideration for publication. All authors agree to submit the manuscript and to transfer copyright to the publisher, if the manuscript is accepted.
Competing interests
The corresponding author (MA) is a member of the Editorial Board of BMC geriatrics. But we declare that the rest of the authors have no conflict of interest.
Device status/Drug statement
The 3-axial accelerometer (Active style Pro HJA-750 C; OMRON Co., Kyoto, Japan) used is commonly available as a health-related device.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tanabe, H., Akai, M., Hayashi, K. et al. Relationship between quantitative physical activity and deterioration of locomotive function: a cross-sectional study using baseline data from a cohort. BMC Geriatr 24, 601 (2024). https://doi.org/10.1186/s12877-024-04995-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04995-2