Abstract
Background
Mild Cognitive Impairment (MCI) is frequently a precursor to dementia, affecting aspects of cognition such as language, thinking, or memory. Lifestyle interventions are increasingly studied as potential means to slow the progression from MCI to dementia.
Objective
A systematic review was conducted to investigate the effectiveness of home-based lifestyle interventions in reducing cognitive decline in older adults with MCI.
Methods
A systematic review of randomized controlled trials (RCTs) was conducted to identify home-based lifestyle interventions for individuals with MCI from 1980 to 2023. These interventions were either single-component or multi-component and included diet, physical activity, stress-reduction, or cognitive stimulation treatments to assess their impact on cognition. We performed a comprehensive search in the PubMed, Web of Science, Google Scholar, Embase, and MEDLINE databases.
Results
From 320 abstracts, 20 (6.25%) studies met the criteria for inclusion, with five multi-component and fifteen single-component studies. Eighteen home-based lifestyle interventions for MCI patients were focused on physical activity, diet, and/or cognitive training, while two studies were identified that incorporated stress reduction training as a method to improve cognitive function. Nineteen studies reported significant improvements in cognitive performance between the experimental and control groups post-intervention for at least one aspect of cognition. Four studies reported nonsignificant improvements in cognitive function between the two groups for at least one area of cognition.
Conclusions
Home-based lifestyle interventions have the potential to improve cognition in elderly patients with MCI. However, future RCTs with larger sample sizes and longer intervention durations are needed to confirm these findings.
Similar content being viewed by others
Introduction
Mild Cognitive Impairment (MCI) is an intermediate stage between normal aging and early dementia [1]. MCI is characterized by cognitive decline that can affect a person’s ability to perform everyday activities, such as the ability to remember important information or to attend appointments, complete complex tasks, understand written or verbal information, and problem-solving. MCI can be further categorized as amnestic MCI, which predominately affects memory, or as non-amnestic MCI, which affects areas of cognition other than memory. Globally, the prevalence of MCI among community-dwelling elderly aged 50 years and older is more than 15% [2]. Approximately 46% of people with MCI develop dementia within 3 years compared to only 3% of the similar age population [3]. Effective, non-pharmacological strategies to delay or prevent cognitive decline in older adults are an area of active research. Fortunately, evidence indicates that nonpharmacological interventions can improve cognition in older adults [4]. One meta-analysis of 28 studies and 2711 participants concluded that multidomain and nonpharmacological interventions were more strongly associated with improving memory, verbal fluency, executive function, and global cognition in older adults with MCI than single-domain interventions [4]. Traditionally, cognitive interventions have been in-person or group-based at a designated study location, such as a clinic. However, this usually requires a time commitment from participants to travel to the study site, and clinic logistics of space and personnel. 17% of elderly patients over the age of 65 are home-bound and unable to access services to support their health [5].
Home-based interventions have the potential to offer multiple advantages for participants compared to in-person approaches, such as reduced costs in terms of traveling, more accessibility, and potentially more anonymity [6]. Home-based interventions are feasible alternatives that would allow older adults the potential to improve their cognition from the convenience of their homes and have risen in prominence in recent years, especially during the COVID-19 pandemic [7]. However, there is sparse reviews or guidelines available that describes the effectiveness of home-based lifestyle interventions for patients with MCI. Therefore, the purpose of this systematic review is to identify the prevalence and effectiveness of home-based lifestyle interventions (i.e., diet, physical activity, stress reduction, cognitive training) on cognitive function in older adults with MCI.
Methods
Study selection criteria and search strategy
Randomized controlled trial (RCT) studies that included participants with MCI were included in this systematic review. The inclusion criteria also required that the interventions have lifestyle-based components, specifically diet, physical activity, stress reduction, or cognitive training. PubMed, Web of Science, Embase, Google Scholar, and MEDLINE were the databases used the complete this search. Studies from 1980 to 2023 were included. The year 1980 was set as a lower limit because the term “MCI” was introduced in the 1980s by Reisberg and colleagues to identify the transitional cognitive stage from normal aging to dementia [8]. We restricted our analyses to those published in English. The databases were searched using the following keywords: “mild cognitive impairment,” cognition, “cognitive function”, “physical activity,” “board games,” diet, stress, AND (RCT OR randomized OR controlled trial OR intervention) AND (home-based OR web-based). Interventions were classified as home-based if they partially or wholly occurred at the participant’s home. RCTs that evaluated consequences of lifestyle interventions on cognition were included. We also included studies that were pilot in nature.
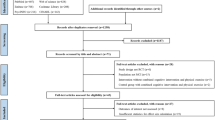
Records were identified via database searching of the previously mentioned keywords and duplicates were removed. All titles and abstracts were analyzed for potential eligibility during the first round of screening. Papers were included if they (1) examined the effect of at least one type of lifestyle intervention (diet, physical activity, stress reduction, or cognitive training) on cognition, (2) included only individuals with MCI, (3) were RCTs, (4) were conducted from 1980 to 2023, and (5) had the intervention carried out at patients’ homes. Individuals with dementia or Alzheimer’s were excluded from this review, as well as study protocol articles. All potentially eligible articles were then retrieved in full text and further included or excluded based on the criteria mentioned above. Twenty studies met our eligibility criteria and were included in this review. In addition, data on the year of publication, setting and population, intervention and control groups, total sample size, outcome of intervention, and p-values were extracted to provide supporting information for this review. All data were independently extracted and assessed by two authors to minimize bias. Any discrepancies involved in selecting the studies to be included in this review were resolved by consensus or by an adjudicator (Dr. Kulshreshtha) if needed. Study information was extracted and stored in EndNote. Results of the literature search were tabulated and displayed using a PRISMA Flow Diagram. Details of individual studies included in the review were displayed via a table. Meta-analysis was not employed because studies were too dissimilar to each other in terms of sample size, study population, and intervention components. Sensitivity analyses were also not utilized in this review. The study adheres to PRISMA guidelines (http://www.prisma-statement.org/) for reporting systematic reviews.
Results
Figure 1 presents the literature search and study selection process, resulting in twenty studies from different countries being included in the final analysis. Five of these were multi-component and fifteen were single-component studies. Table 1 shows specific details about each study included in this systematic review, including the population and setting, intervention duration and type, total sample size, control groups, outcomes, and p-values. Two studies focused on MCI individuals with specific clinical circumstances (i.e., HIV or obesity) [9, 10]. Furthermore, three studies focused exclusively on individuals with amnestic mild cognitive impairment (aMCI) [11,12,13]. Individual studies were evaluated for bias and study quality was graded by reviewers.
Multi-component interventions
Multi-component interventions were defined as including two or more lifestyle modifications from the following categories: diet, physical activity, stress reduction, and cognitive training. The database search found five studies that included multi-component interventions [10, 16, 17, 22, 24]. Only two studies were identified that included stress reduction training as a method to improve cognitive function, and they were both part of a larger multi-component study [16, 22].
Out of the total twenty interventions analyzed, nineteen reported significant improvements in cognitive function between the experimental and control groups for at least one aspect of cognition. Four of these were multicomponent interventions [10, 16, 17, 22]. Yu et al. reported that participants in a strength-based and empowerment program, which includes cognitive and stress adaptation training, had improvements in their Mini-Mental State Examination (MMSE) scores compared to the control group of usual care provided by the elderly (p < 0.001) [16]. Dannhauser et al. found that a three-component intervention composed of physical activity, group-based cognitive stimulation, and individual cognitive stimulation resulted in significant improvements in working memory [17]. A four-component intervention by Fotuhi et al. found that physical fitness education, education about Mediterranean diets and omega-3 supplements, meditation and stress reduction training, and cognitive training programs resulted in significant improvements in cognitive function (p < 0.05) [22]. Horie et al. studied the impact of physical activity encouragement and nutrition counselling and found improvements in global cognition compared to the control group (p < 0.0001) [10].
Single-component interventions
The fifteen single-component interventions all found significant improvements in at least one area of cognitive function, in which six studied the effect of diet, two studied the impact of physical activity, and seven analyzed the effect of cognitive training. Manenti et al. studied the effect of face-to-face cognitive virtual reality rehabilitation system and cognitive stimulation on cognitive function and found that they had improvements in memory, language and visuo-constructional abilities compared to face-to-face treatment as usual [14]. Lee et al. found that a home-based robot cognitive intervention resulted in improvements in spatial working memory (p = 0.037) but not in paired associates learning (p = 0.744) or rapid visual information processing (p = 0.0366) [15]. Frain et al. utilized a computerized cognitive training program and found significant improvements in total Montreal Cognitive Assessment (MoCA) scores compared to control (p = 0.04) [9]. Jeong et al. studied a group-based cognitive intervention (GCI) and home-based cognitive intervention (HCI) and found that compared to the control which received neither intervention, subjects in both intervention groups had improvements in cognition, with the benefits of cognitive intervention persisting for at least another 6 months after the study (p = 0.01 and p = 0.02) [11]. Sungkarat et al. found that tai chi exercises helped improve logical memory (p = 0.006) [12]. Suzuki et al. also studied physical activity and found that a structured exercise program had improvements in logical memory of immediate recall (p = 0.03) and letter verbal fluency test (p = 0.02) [13]. Boespflug et al. studied the effect of blueberry diet supplementation on blood oxygen level-dependent (BOLD) signal on neural activity. They found increased BOLD activation in the left interior parietal lobe, left pre-central gyrus, and left middle frontal gyrus during working memory load conditions (p < 0.01) [18]. Bo et al. studied n-3 polyunsaturated fatty acids supplementation to the diet. Participants demonstrated improvements in multiple areas of cognition, specifically total Basic Cognitive Aptitude Tests (BCAT) scores, space imagery efficiency, working memory, and perceptual speed (p < 0.01). Desideri et al. found that the time required to complete Trail Making Test A and B was significantly lower in subjects assigned to drinking coca drinks with high or intermediate flavanol levels (p < 0.05) compared to those assigned to low flavanols [20]. Fortier et al. found that subjects who drank a ketogenic drink with medium chain triglycerides had improvements in free and cued recall (p = 0.047) and verbal fluency (p = 0.033) [21]. Hwang et al. studied the effect of Lactobacillus plantarum C29-fermented soybean (DW2009) as a nutritional supplement on cognition and found improvements in combined cognitive functions and the attention domain (p = 0.02) in the experimental group compared to control group [23]. Rondanelli et al. found that those who supplemented their diet with an oily emulsion of docosahexaenoic acid (DHA)-phospholipids containing melatonin and tryptophan had improvements in MMSE scores (p < 0.001) and semantic verbal fluency (p < 0.06) [25]. Ma et al. studied the effect of playing an assortment of board games on cognitive function and found improvements in attention as demonstrated by increases in MMSE-K and MoCA-K scores [26]. Lim et al. found that individuals participating in cognitive training through a serious game demonstrated immediate improvement in MMSE-K (p = 0.001), MoCA-K (p = 0.01), and SVFT scores (p = 0.044), with effects continuing one month post-intervention [27]. Baik et al. analyzed the effect of a home-based computerized cognitive training intervention called Neuro-World, and determined there were improvements in MoCA scores (p < 0.01), digit span test results (p = 0.000), and semantic word fluency test results (p = 0.004) [28].
Four studies reported no significant differences in cognitive performance between the experimental and control groups for at least one aspect of cognition, of which only Köbe et al.’s study was multi-component [15, 18, 19, 24]. One study’s experimental group had omega-3 fatty acid (FA) supplementation, aerobic exercise, and cognitive stimulation whereas the control group had omega-3 FA supplementation and non-aerobic exercise [24]. No significant changes in memory (p = 0.635), executive function (p = 0.160), sensorimotor speed (p = 0.345) and attention (p = 0.656) were found in both groups after correction for multiple-comparisons [24]. Boespflug et al. studied the effect of blueberry diet supplementation on blood oxygen level-dependent (BOLD) signal on neural activity. There was no clear evidence of an enhancement in working memory post-intervention [18]. Another study analyzed the impact of a home-based robot cognitive intervention versus a control group with no cognitive intervention [15]. After the 4-week intervention, there was no significant difference between the two groups in paired associates learning (p = 0.744) or rapid visual information processing (p = 0.366) [15]. Bo et al. studied n-3 polyunsaturated fatty acids supplementation to the diet. There was no significant improvement in recognition memory or mental arithmetic efficiency (p > 0.05) [19].
Discussion
In our comprehensive review, we identified five multi-component and fifteen single-component home-based intervention studies from our twenty total eligible research papers. Of the five multi-component studies, four indicated the effectiveness of home-based lifestyle interventions in enhancing cognitive function within at least one cognitive domain, whereas only one demonstrated no significant change in at least one aspect of cognition after the intervention. All the fifteen single-component interventions found improvements in cognitive function within at least one cognitive domain. Six studied the effect of diet, two studied the impact of physical activity, and seven analyzed the effect of cognitive training.
There is a dearth of multi-component lifestyle interventions that fit within our search criteria. Research examining the impact of stress reduction training is particularly scarce and was not analyzed as single components; rather, they were included only in two multi-component studies. Four studies demonstrated no significant change in at least one aspect of cognition after the intervention, with only one being multi-component [15, 18, 19, 24]. Of these four studies, two focused solely on dietary interventions, one focused solely on cognitive interventions, and one studied a multidomain intervention consisting of dietary, cognitive, and physical activity interventions. It is worth noting that among the two dietary interventions that concluded no significant change in at least one aspect of cognition, there were still improvements in other areas of cognitive function, specifically in neural responses, working memory, space imagery efficiency, and perceptual speed [18, 19].
Most of the studies had web-based components in addition to home-based, such as the use of robots or online applications. The use of web-based health interventions in chronic disease management has revolutionized the field of healthcare. These interventions offer several advantages over traditional interventions, particularly in terms of improving accessibility, convenience, and user engagement. With virtual health interventions, patients can access their healthcare from anywhere and at any time, which can lead to better adherence to treatment and improved health outcomes. Moreover, these interventions offer the potential for continuous monitoring and feedback, which can help to optimize the intervention and provide personalized care. These advantages are particularly relevant in the context of MCI as it often affects older adults, who may have limited mobility and may face challenges in accessing traditional healthcare settings. By providing interventions through mobile devices, virtual interventions can overcome these barriers and provide older adults with a convenient and accessible way to manage their cognitive impairment.
It is important to note that the penetration of mobile technology among older adults may be lower compared to younger populations. However, over the past decade and with COVID-19 pandemic, an increasing number of elderly individuals have used telehealth and mobile devices from their home for their healthcare needs [29]. Thus, it is essential to assess the penetration of mobile-based interventions among older adults and to ensure that the interventions are designed in a way that is accessible and user-friendly for this population. Additionally, it is important to consider the unique challenges faced by older adults in terms of cognitive and physical abilities, and to design interventions that are tailored to their needs.
Although limited, there are existing systematic reviews that detail the effect of lifestyle interventions on cognition of older adults with MCI [4]. However, these studies did not include RCTs that are specifically home-based. Thus, more research is needed to analyse how home-based interventions can impact cognition and address this gap in the scientific literature. This is particularly important for the very elderly as they frequently have barriers for transportation and the ones living in rural areas with limited access to healthcare facilities for in-person interventions.
Our systematic review is dependent on the quality of the contributing studies and has a few limitations. Some of the studies focused only on MCI participants while two other studies targeted MCI individuals with specific clinical circumstances of HIV or obesity. The results from these two studies may not be as applicable to individuals with MCI in general. Furthermore, a few of the studies (n = 6) had a smaller sample size of 25 people or less or were of short duration of 4 weeks or less (n = 4), which could have affected the reliability of the results.
Conclusion
Our systematic review suggests that home-based lifestyle interventions focusing on diet, physical activity, stress reduction, and cognitive training can help combat cognitive decline and improve brain function. Since MCI is often a precursor to more serious forms of dementia, there is a need for effective lifestyle interventions that can be conveniently performed from home via telemedicine or other accessible formats. More robust RCTs with larger sample sizes and longer duration are needed to provide stronger evidence of the effectiveness of these interventions on specific cognitive domains and which components of lifestyle are most beneficial. Home-based interventions have the potential to slow cognitive decline and provide access to lifestyle support for the growing elderly population in US and globally.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- aMCI:
-
amnestic mild cognitive impairment
- BCAT:
-
Basic Cognitive Aptitude Tests
- BOLD:
-
blood oxygen level-dependent
- DHA:
-
docosahexaenoic acid
- FA:
-
fatty acid
- GCI:
-
group-based cognitive intervention
- HCI:
-
home-based cognitive intervention
- MCI:
-
Mild Cognitive Impairment
- MMSE:
-
Mini-Mental State Examination
- MMSE:
-
K-Mini-Mental State Examination Korean version
- MoCA:
-
Montreal Cognitive Assessment
- MoCA:
-
K-Montreal Cognitive Assessment Korean version
- RCT:
-
Randomized controlled trial
- SVFT:
-
Sematic Verbal Fluency Task
References
Van der Mussele S et al. Mar., Behavioral symptoms in mild cognitive impairment as compared with Alzheimer’s disease and healthy older adults, (in eng), Int J Geriatr Psychiatry, vol. 28, no. 3, pp. 265–75, 2013, https://doi.org/10.1002/gps.3820.
Bai W et al. Worldwide prevalence of mild cognitive impairment among community dwellers aged 50 years and older: a meta-analysis and systematic review of epidemiology studies, (in eng), Age Ageing, vol. 51, no. 8, Aug 2 2022, https://doi.org/10.1093/ageing/afac173.
Tschanz JT et al. Conversion to dementia from mild cognitive disorder: the Cache County Study, (in eng), Neurology, vol. 67, no. 2, pp. 229–34, Jul 25 2006, https://doi.org/10.1212/01.wnl.0000224748.48011.84.
Salzman T, Sarquis-Adamson Y, Son S, Montero-Odasso M, Fraser S. Associations of Multidomain Interventions With Improvements in Cognition in Mild Cognitive Impairment: A Systematic Review and Meta-analysis, (in eng), JAMA Netw Open, vol. 5, no. 5, p. e226744, May 2 2022, https://doi.org/10.1001/jamanetworkopen.2022.6744.
Qiu WQ, et al. Physical and mental health of homebound older adults: an overlooked population, (in eng). J Am Geriatr Soc. Dec 2010;58(12):2423–8. https://doi.org/10.1111/j.1532-5415.2010.03161.x.
Heber E et al. The Benefit of Web- and Computer-Based Interventions for Stress: A Systematic Review and Meta-Analysis, (in eng), J Med Internet Res, vol. 19, no. 2, p. e32, Feb 17 2017, https://doi.org/10.2196/jmir.5774.
Bernini S, et al. Cognitive telerehabilitation for older adults with neurodegenerative diseases in the COVID-19 era: a perspective study, (in eng). Front Neurol. 2020;11:623933. https://doi.org/10.3389/fneur.2020.623933.
Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution, (in eng). J Intern Med. Mar 2014;275(3):214–28. https://doi.org/10.1111/joim.12190.
Frain JA, Chen L. Examining the effectiveness of a cognitive intervention to improve cognitive function in a population of older adults living with HIV: a pilot study, (in eng), Ther Adv Infect Dis, vol. 5, no. 1, pp. 19–28, Jan 2018, https://doi.org/10.1177/2049936117736456.
Horie NC, et al. Cognitive effects of Intentional Weight loss in Elderly obese individuals with mild cognitive impairment, (in eng). J Clin Endocrinol Metab. Mar 2016;101(3):1104–12. https://doi.org/10.1210/jc.2015-2315.
Jeong JH, et al. Group- and home-based cognitive intervention for patients with mild cognitive impairment: a Randomized Controlled Trial. Psychother Psychosom. 2016;85(4):198–207. https://doi.org/10.1159/000442261.
Sungkarat S, Boripuntakul S, Chattipakorn N, Watcharasaksilp K, Lord SR. Effects of Tai Chi on Cognition and fall risk in older adults with mild cognitive impairment: a Randomized Controlled Trial, (in English). J Am Geriatr Soc Article vol. 2017;65(4):721–7. https://doi.org/10.1111/jgs.14594.
Suzuki T, et al. Effects of multicomponent exercise on cognitive function in older adults with amnestic mild cognitive impairment: a randomized controlled trial. (in eng) BMC Neurol. Oct 31 2012;12:128. https://doi.org/10.1186/1471-2377-12-128.
Manenti R et al. Effectiveness of an Innovative Cognitive Treatment and Telerehabilitation on Subjects With Mild Cognitive Impairment: A Multicenter, Randomized, Active-Controlled Study, (in eng), Front Aging Neurosci, vol. 12, p. 585988, 2020, https://doi.org/10.3389/fnagi.2020.585988.
Lee EH et al. Four-Week, Home-Based, Robot Cognitive Intervention for Patients with Mild Cognitive Impairment: a Pilot Randomized Controlled Trial, (in eng), Dement Neurocogn Disord, vol. 19, no. 3, pp. 96–107, Sep 2020, https://doi.org/10.12779/dnd.2020.19.3.96.
Yu DS-F, Li PW-C, Zhang F, Cheng S-T, Ng TK, Judge KS. The effects of a dyadic strength-based empowerment program on the health outcomes of people with mild cognitive impairment and their family caregivers: a randomized controlled trial. Clin Interv Aging. 2019;14:1705–17. https://doi.org/10.2147/CIA.S213006.
Dannhauser TM, Cleverley M, Whitfield TJ, Fletcher BC, Stevens T, Walker Z. A complex multimodal activity intervention to reduce the risk of dementia in mild cognitive impairment–ThinkingFit: pilot and feasibility study for a randomized controlled trial, (in eng), BMC Psychiatry, vol. 14, p. 129, May 5 2014, https://doi.org/10.1186/1471-244x-14-129.
Boespflug EL et al. Enhanced neural activation with blueberry supplementation in mild cognitive impairment, (in eng), Nutr Neurosci, vol. 21, no. 4, pp. 297–305, May 2018, https://doi.org/10.1080/1028415x.2017.1287833.
Bo Y et al. The n-3 Polyunsaturated Fatty Acids Supplementation Improved the Cognitive Function in the Chinese Elderly with Mild Cognitive Impairment: A Double-Blind Randomized Controlled Trial, (in eng), Nutrients, vol. 9, no. 1, Jan 10 2017, https://doi.org/10.3390/nu9010054.
Desideri G et al. Benefits in cognitive function, blood pressure, and insulin resistance through cocoa flavanol consumption in elderly subjects with mild cognitive impairment: the Cocoa, Cognition, and Aging (CoCoA) study, (in eng), Hypertension, vol. 60, no. 3, pp. 794–801, Sep 2012, https://doi.org/10.1161/hypertensionaha.112.193060.
Fortier M, et al. A ketogenic drink improves cognition in mild cognitive impairment: results of a 6-month RCT, (in eng). Alzheimers Dement. Mar 2021;17(3):543–52. https://doi.org/10.1002/alz.12206.
Fotuhi M et al. A Personalized 12-week Brain Fitness Program for Improving Cognitive Function and Increasing the Volume of Hippocampus in Elderly with Mild Cognitive Impairment, (in eng), J Prev Alzheimers Dis, vol. 3, no. 3, pp. 133–137, 2016, https://doi.org/10.14283/jpad.2016.92.
Hwang YH et al. Efficacy and Safety of Lactobacillus Plantarum C29-Fermented Soybean (DW2009) in Individuals with Mild Cognitive Impairment: A 12-Week, Multi-Center, Randomized, Double-Blind, Placebo-Controlled Clinical Trial, (in eng), Nutrients, vol. 11, no. 2, Feb 1 2019, https://doi.org/10.3390/nu11020305.
Köbe T et al. Combined omega-3 fatty acids, aerobic exercise and cognitive stimulation prevents decline in gray matter volume of the frontal, parietal and cingulate cortex in patients with mild cognitive impairment, NeuroImage, vol. 131, pp. 226–238, 2016/05/01/ 2016, https://doi.org/10.1016/j.neuroimage.2015.09.050.
Rondanelli M et al. Effects of a diet integration with an oily emulsion of DHA-phospholipids containing melatonin and tryptophan in elderly patients suffering from mild cognitive impairment, (in eng), Nutr Neurosci, vol. 15, no. 2, pp. 46–54, Mar 2012, https://doi.org/10.1179/1476830511y.0000000032.
Ma S-R, Cho B-J, Song B-K. Effects of Home-based board games programs on cognition and depression for elderly with mild cognitive impairment-pilot study. Indian J Public Health Res Dev. 08/01 2018;9:546. https://doi.org/10.5958/0976-5506.2018.00790.8.
Lim EH et al. Effects of Home Based Serious Game Training (Brain Talk™) in the Elderly With Mild Cognitive Impairment: Randomized, a Single-Blind, Controlled Trial, (in eng), Brain Neurorehabil, vol. 16, no. 1, p. e4, Mar 2023, https://doi.org/10.12786/bn.2023.16.e4.
Baik JS, et al. Effects of Home-based computerized cognitive training in Community-Dwelling adults with mild cognitive impairment. IEEE J Translational Eng Health Med. 2024;12:97–105. https://doi.org/10.1109/JTEHM.2023.3317189.
Choi NG, DiNitto DM, Marti CN, Choi BY. Telehealth Use among older adults during COVID-19: associations with Sociodemographic and Health characteristics, Technology device ownership, and Technology Learning, (in eng). J Appl Gerontol. Mar 2022;41(3):600–9. https://doi.org/10.1177/07334648211047347.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Institute on Aging (grant number K23AG066931). The funding source had no role in the conceptualization; study design; collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
C. Z. completed the manuscript writing, analyzed and interpreted the data from the RCTs reviewed, and prepared the figures and tables. A. K developed the idea and provided guidance regarding the literature review and manuscript writing. D.A.R. helped with conceptualization, writing the manuscript, and interpreting the data from the RCTs that were reviewed. R. J help with manuscript review and final edits. All authors read and reviewed the manuscript draft and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zou, C., Amos-Richards, D., Jagannathan, R. et al. Effect of home-based lifestyle interventions on cognition in older adults with mild cognitive impairment: a systematic review. BMC Geriatr 24, 200 (2024). https://doi.org/10.1186/s12877-024-04798-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04798-5