Abstract
Objective
Improving care transitions for older adults can reduce emergency department (ED) visits, adverse events, and empower community autonomy. We conducted an inductive qualitative content analysis to identify themes emerging from comments to better understand ED care transitions.
Methods
The LEARNING WISDOM prospective longitudinal observational cohort includes older adults (≥ 65 years) who experienced a care transition after an ED visit from both before and during COVID-19. Their comments on this transition were collected via phone interview and transcribed. We conducted an inductive qualitative content analysis with randomly selected comments until saturation. Themes that arose from comments were coded and organized into frequencies and proportions. We followed the Standards for Reporting Qualitative Research (SRQR).
Results
Comments from 690 patients (339 pre-COVID, 351 during COVID) composed of 351 women (50.9%) and 339 men (49.1%) were analyzed. Patients were satisfied with acute emergency care, and the proportion of patients with positive acute care experiences increased with the COVID-19 pandemic. Negative patient comments were most often related to communication between health providers across the care continuum and the professionalism of personnel in the ED. Comments concerning home care became more neutral with the COVID-19 pandemic.
Conclusion
Patients were satisfied overall with acute care but reported gaps in professionalism and follow-up communication between providers. Comments may have changed in tone from positive to neutral regarding home care over the COVID-19 pandemic due to service slowdowns. Addressing these concerns may improve the quality of care transitions and provide future pandemic mitigation strategies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Older adults are frequent users of emergency departments (EDs) [1, 2]. Two-thirds of ED visits among older adults result in discharge back to the community [3]. Care transitions from the ED are critical moments where vulnerable older adults are at high risk of discharge-related adverse events, which can result in unplanned readmissions and loss of physical, functional, and/or cognitive capacity [3, 4]. Care transitions include sets of actions, both before and after a hospital or ED stay, put in place to ensure the continuity of care [5, 6]. Care transitions are frequent from the ED and represent an important opportunity for quality improvement [7]. They are also costly, necessitating investment of time and resources from clinicians and informal caregivers [8].
The COVID-19 pandemic has also been devastating for older adults’ care transitions [9]. COVID-19 has disproportionately affected older adults with higher risks of complications and mortality [10]. Fear of contracting the virus and preventative measures to reduce their risk of infection have also led to their social isolation [11]. Care transitions during the pandemic have been complicated by the lack of qualified personnel, care transition nurses and social workers being called upon to manage COVID-19 units, caregivers being asked to stay away from hospitals and caregivers becoming ill themselves [12].
Studies published before the pandemic have documented patients’ views about post-ED discharge outcomes [13], but to our knowledge few studies have documented the impact of the pandemic on patients’ experience about their care transitions to improve care transitions in the post-COVID-19 period [14]. Tailoring care transition interventions to the needs of patients, especially those with multi-morbidity, by paying attention to their lived care experiences can help co-create interventions that are patient-oriented and contribute to better outcomes [15]. While some care transition studies have employed patient-centered outcomes [16,17,18,19,20,21,22,23] none have studied interventions that were patient-oriented. Using comments provided by patients, we may be able to identify paths to developing patient-oriented interventions in older adults to improve care transition interventions. The goal of this study was to better understand patients’ care transition experiences that could be used in designing future patient-oriented interventions to improve care transitions in the post-COVID-19 context.
Methodology
Study design and context
Using an inductive approach with no a-priori coding scheme [24, 25], we designed this qualitative descriptive study to analyze data collected directly from older patients having experienced care transition before and during pandemic. This study was nested within the LEARNING WISDOM (Supporting the Creation of a LEARNing INteGrated Health System to Mobilize Context-adapted Knowledge With a Wiki Platform to Improve the Transitions of Frail Seniors From Hospitals and Emergency Departments to the cOMmunity) longitudinal cohort study [26]. We followed the Standards for Reporting Qualitative Research (SRQR) to report our results [27]. The protocol for this study was approved by the Centre intégré de santé et de services sociaux de Chaudière-Appalaches (CISSS-CA) Ethics Review Committee (project #2018 − 462, 2018-007). The LEARNING WISDOM cohort included older adults who underwent a transition of care following a visit to one of the four EDs in the CISSS-CA (Québec, Canada) between January 2019 and December 2021. The CISSS-CA is an integrated health organization consisting of four acute care hospitals (Hôtel-Dieu de Lévis (HDL), Hôpital de Montmagny (HDM), Hôpital de Saint-Georges (HSG), Hôpital de Thetford-Mines (HTM)). The HDL is a university-affiliated teaching hospital receiving 70,000 visits to the ED annually. The other three sites each receive 30,000 annual ED visits.
Selection of participants
The LEARNING WISDOM cohort included patients discharged from one of the four EDs before the COVID-19 pandemic and throughout waves one through five of the pandemic in Québec [28]. Recruitment for the LEARNING WISDOM cohort finished on December 21, 2021. Participants were aged 65 years or older and had been discharged back to the community from the ED observation unit. In the four participating EDs, patients triaged to an observation unit are still considered outpatients being considered for admission to hospital or discharge with primary or specialist care follow-up if needed. Patients triaged to a stretcher in the observation unit are often put on close monitoring. Patients only seen in the ambulatory care section of the ED, admitted to hospital, transferred to another hospital, or transferred to a long-term care center were excluded. Participants having already participated in our study were also excluded. Patients had to be able to understand French and provide informed consent. For the full duration of the study recruitment period, at each participating hospital, a list of eligible discharged patients was generated each day. Patients were called using a computer-generated randomized list for each day of the month and patients were contacted in order until three to five patients were enrolled that day.
Data collection
As part of a continuous quality improvement project lead by the CISSS-CA participants were contacted by telephone between 24 h and up to seven days after ED discharge, to administer the three-item Care Transitions Measure (CTM-3) [29] (Appendix A), a validated questionnaire that assesses the patient’s opinion about the quality of their care transition [30]. The CTM-3 has three items that investigate three different domains related to the quality of care transitions after discharge from hospital: (1) Whether the patient and family’s preferences were accounted for in the care plan; (2) Whether patients understood their role in self-management after discharge; and (3) Whether patients were briefed on their medications and how to use them before discharge. Patients are asked to qualify their level of agreement with each of the three CTM-3 items (strongly disagree; disagree; agree; strongly agree, missing (don’t know/don’t remember/not applicable)). After completing the CTM-3, patients were then invited to participate in a more in-depth research interview in the following days.
During this second call, patients were required to summarize—in their own words—their understanding of the study to consent, based on the Nova Scotia Criteria [31]. We then asked participants to report on their care transition experience from the ED to home using a structured interview with closed-ended questions and one open-ended response question. We collected sociodemographic information including age, sex, race, language, educational level, family income, pre-consultation living situation, and reason for ED consultation and one single open-ended question asking about their care transition experiences. Patients were asked: Do you have any details to provide related to your experience of transition from emergency care to returning to your living environment? Patients answered in as much or as little detail as they wished. We instructed research professionals to collect patients’ comments on all issues concerning their care transitions even if patients commented on their care before arrival to the ED, during their ED stay or after their ED discharge. Our rationale was that elderly patients’ complete care experience during their whole journey to and from the ED, and during their ED stay are important to understand when planning care transition quality improvement interventions.
We refer to these open-ended responses hereafter as comments. A member of the research team asserted the patient’s consent, administered questionnaires, and were instructed to immediately record key elements of each patient’s response to the open-ended question (including important verbatim excerpts) in REDCap (Research Electronic Data Capture [32, 33]). These research professionals were MD students, PhD students in psychology, and research nurses who were trained by the research team coordinator to conduct the interviews and collect important verbatims. This training involved role-playing, simulated calls between the data collection trainees, and direct observation of the first calls until the data collection procedure was respected. Although we did not audio record the calls or produce verbatim transcripts for each call, research professionals were instructed to capture the key open-ended comments made by each patient in short sentences and support these comments with verbatim quotes whenever possible. This data collection process was authorized by the Director of Nursing and the Professional Services Director. Care partners did not provide comments analyzed in this study, nor were they interviewed as proxies to capture patients’ individual care transition experience. The data were anonymized, and a single unique numerical identifier was created for each participant. The CTM-3 in addition to the open-ended question in French and translated in English for this article are presented in Appendix A.
Quantitative analyses
We used descriptive statistics to present the number of participants who responded to each response category (strongly disagree, disagree, agree, strongly agree, missing (don’t know/don’t remember/not applicable) stratified by pandemic period (pre vs. during COVID-19). To calculate individual CTM-3 scores, we used a linear transformation of its four-point response structure (strongly disagree = 1 point; disagree = 2 points; agree = 3 points; strongly agree = 4 points) to create a CTM-3 score ranging from 0 to 100 [34]. Patients with “missing” results were excluded from analyses and the score was simply calculated by adding the sum of the scores from each item divided by the number of questions answered. We compared mean CTM-3 scores for pre vs. during COVID-19 participants using an independent t-test. We also conducted X 2 analyses comparing dichotomous CTM-3 responses for both periods. Values labelled as “missing” were not included in the X 2 analyses.
Qualitative analyses
Our analysis plan followed an inductive content analysis approach, which consisted of iteratively developing codes used to label the data during the process of coding, based on the content of the data set [35, 36]. This approach is well suited to analyzing comments, consisting of interpreting not just the content of the text, but also the interrelations between themes and concepts [35]. This thematic analysis was performed by two female evaluators from different scientific backgrounds (VC, experienced research professional and NG, a Master of Science candidate in epidemiology with training in mixed methods) and supervised by an experienced researcher in qualitative analyses (PMA).
Constructing the coding scheme
Patient comments were stripped of any identifying information and placed in a password-protected online collaborative spreadsheet program (Google Sheets, Google LLC, Mountain View, CA) to support thematic analysis. Both evaluators then used a basic inductive content analysis to screen all patient comments in the shared spreadsheet to identify and group overarching keywords into codes in a bottom-up fashion, and then groups of linked codes were clustered into themes. Each theme was reviewed to ensure that it reflected all its associate sub-themes. For instance, a mention of “bed sheets” in patient comments was determined to fall into a subcategory of “bedding, clothing and furniture”, which was under a larger category relating to the patient’s “conditions of stay” at the ED.
These themes and sub-themes were integrated together into a Mind Map diagram drawn with diagrams.net to guide the coding of individual comments by both evaluators. Throughout the analysis, disagreements and questions between both evaluators were validated by a third author (PMA). Pair debriefing between both evaluators, triangulation (both evaluators coded independently of one another), and expert validation by a third evaluator (PMA) minimized the influence of subjectivity and preconceptions among the coders.
Once the Mind Map diagram and coding scheme was developed to map the whole care transition continuum, both evaluators each coded an identical random sample of 40 comments to determine inter-rater reliability. Both reviewers assessed separate online spreadsheets that were then used to independently collect codes (either 1 or 0; each column indicated its own theme) indicating the presence or absence of a theme embedded in the comment. Krippendorff’s alpha coefficient [37] was then used to measure the interrater agreement between both evaluators. Krippendorff’s alpha coefficient is a reliability coefficient employed frequently in content analysis, developed to measure the agreement among codes that draw distinctions among typically unstructured phenomena. Acceptable inter-rater agreement is considered an alpha above or equal to 0.8 [37].
We then identified, through an inductive coding scheme, an emotional valence (positive, negative, or neutral) expressed by participants towards the quality of the care transitions they had experienced associated with each individual theme. We also calculated an interrater Krippendorff’s alpha reliability coefficient for the emotional valence codes. We then produced descriptive statistics for each theme stratified based on their emotional valence and by time period (before and after the start of the COVID-19 pandemic).
Sample size
For the LEARNING WISDOM cohort, our sample size for the HDL site was calculated based on measuring a daily CTM-3 [38] for five discharged patients per day from the ED aged more than 65 years. The other three sites had a planned sample size of three patients per day from June 21st, 2019, until December 21st, 2021. After collecting data between January 24th, 2019, to October 4th, 2019, at the HDL site yielding an average score of 75.1 (95% CI [67.6, 82.6]), we decreased our recruitment of five random patients per day to three patients a day—like the other three sites—because including three patients per day until the end of recruitment would be sufficient to attain sufficiently precise daily CTM-3 point estimates.
For our nested qualitative study, we selected a sample of participants’ responses using a random number generator to obtain a representative sample of participants from all periods of the three-year study (pre and during COVID-19). Two authors (VC and NG) performed the qualitative inductive content analysis using the comments from sampled participants. We coded comments placed in an online spreadsheet until we reached data saturation when additional comments did not reveal new themes [39]. For each hospital site, two authors (VC and NG) each individually coded 30 randomly selected comments (selection without replacement). After which they each individually analyzed additional randomly selected comments in rounds of 10. We considered saturation achieved when two consecutive rounds of 10 comments were completed without the emergence of a new sub-theme per site.
The impact of the COVID-19 pandemic
To analyze how the COVID-19 pandemic may have affected the experiences of older adult patients undergoing a transition of care, we split the coded comments into two groups: patients who left the ED before the onset of the COVID-19 pandemic, and patients who left the ED on or after the start of the pandemic on March 14th, 2020 [28].
Results
Figure 1 presents the flow of participants during our recruitment process. We reached data saturation after analyzing a sample of comments from 690 patients (339 pre-COVID and 351 during-COVID) composed of 351 women (50.9%) and 339 men (49.1%). Demographic characteristics of the sample are summarized in Table 1. Patients were aged 75 years on average (M = 75.7, SD = 7.2) and nearly all were Caucasian (99.9%) and spoke French as their first language (99.7%). We did not observe differences among patients included in this qualitative analysis (N = 690) versus all participants in the LEARNING WISDOM project who provided a comment but were not selected via random sampling (N = 4,312), and patients who opted not to provide a comment at all (N = 37). See Supplemental Table 2d in Appendix B. Included patients reported on average that 3.8 people (SD = 3.7) in their entourage could serve as sources of social support, and one third of patients reported having an informal caregiver (35.8%). Nearly all patients reported having access to transport for medical appointments (94.1%) and a family physician (91.6%), but only half of patients (51.7%) said they could quickly get an appointment with their family physician if needed. Patients were discharged from one of the four EDs before the COVID-19 pandemic (01/01/2019 to 12/03/2020) and throughout waves one (13/03/2020 to 11/07/2020), two (23/08/2020 to 20/03/2021), three (21/03/2021 to 17/07/2021), four (18/07/2021 to 4/12/2021) and five (5/12/2021 to 12/03/2022). Our sample included slightly more participants who were discharged from the ED after the start of the COVID-19 pandemic (N = 351, 50.8%) than before the start of the pandemic in Québec, Canada (N = 339, 49.1%). Concerning participants’ scores on the CTM-3, for each of the three questions, the majority of patients strongly agreed, or agreed with each statement. Additionally, the distribution of these responses did not statistically significantly change between the two time periods (see Table 1 and Appendix A). The mean CTM-3 scores were also both similarly high without any significant difference in both periods (see Table 1 and Appendix A).
Main themes and their sub-themes
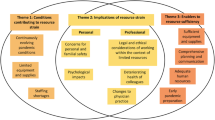
We identified four overarching themes related to transitions of care among older adult ED users, and eighteen sub-themes. Both coders obtained a Krippendorff’s alpha coefficient of 0.93 on the first round of coding, and after a discussion to resolve disagreements in codes we achieved an alpha of 0.98. These main themes were (1) care in the ED, (2) conditions of stay in the ED, (3) leaving the ED, and (4) empowering patients in their living environment. A Mind Map of all themes and their sub-themes is presented in Fig. 2.
Mind Map of the four main themes and nineteen sub-themes emerging from patients’ comments about their complete care transition continuum experience before, during and after their ED visit and discharge back to their living situations. A transversal theme, Timeliness of receiving services is also identified
Care in the ED
Quality of care was the most frequently cited main theme by patients, present in 96.6% of all comments (Fig. 3A).
This theme was related to several sub-themes: clinical interventions (cited in 79.4% of all patient comments, see Fig. 3B), communication (53.2%), professionalism (11.6%), explanations (5.2%), sense of security about care (2.3%) and finally accompaniment (1%). Clinical intervention comments reflected the quality of acute care. Communication consisted of comments citing the presence or absence of planned follow-ups or tests with specialists or outpatient clinics. For professionalism, patients reported whether the ED staff members were negligent, empathetic, dismissive, prejudiced, or did not take their complaints seriously. In the case of explanations, patients reported whether personnel took the time to meaningfully explain planned procedures and tests in plain language. Security encompassed feelings of safety and the preservation of patients’ own bodily autonomy during care. Lastly, accompaniment at the ED included comments about loved ones who stayed with and supported the patient during their ED stay.
Conditions of stay in the ED
The conditions of stay on a stretcher were the least mentioned of the main themes (2.4% of all patient comments, see Fig. 3A). Sub-themes included food, sense of security, sleeping conditions, hygiene and sanitation, privacy, and bedding (each < 1%, see Fig. 3B). For food, the commonest concerns were quality and the availability of drinking water. Sense of security about the environment referred to feeling safe during their observation in the physical ED environment. Sleeping conditions highlighted excessive light which made it difficult to rest. For hygiene and sanitation, the concerns were oriented toward inadequate cleanliness of facilities and observed inadequacies in personal protective equipment used by staff. Privacy reflected the ability to discreetly speak to staff and to attend to private matters with dignity (e.g., toileting). For bedding, patients mentioned uncomfortable furniture, bedding, bedclothes, or accommodations and whether their environment was adequately heated or cooled.
ED discharge
ED discharge was mentioned in approximately 34.3% of all main theme comments, making it the second most cited main theme (see Fig. 3A). Comments described the circumstances surrounding the conclusion of ED care and the return home. This main theme was divided into three sub-themes: departure (33.9%), the presence or absence of transport, and feelings of security or vulnerability in leaving the ED (each < 1.3%, see Fig. 3B). Here, patients mentioned whether their ED discharge was seamless, rushed or forced, at night, too slow, or if the ED had to close temporarily because the ED physician had to escort a patient during an urgent medical transfer to another hospital forcing some patients to leave consequently. Although this is a very rare situation, some smaller remote community-based hospitals have staffing issues that force them to have to close temporarily if the on-call physician needs to escort a patient in ambulance for a life-saving procedure in another hospital.
Living environment empowerment
The main theme related to services empowering older adults to stay independent at home was specified in 14.8% of all patient comments (Fig. 3A). This main theme was subdivided in the following sub-themes: home care (14.1%), domestic help, isolation, and sense of security at home (each < 1%) (Fig. 3B). Concerning home care, patients commented on interventions or services performed outside the hospital which required a specific level of training. Domestic help referred to having a person, a relative, or services for daily chores and household tasks. As for isolation, the comments concerned the potential social isolation due to patients’ absence or small social networks. The sense of security at home encompassed comments from patients about their sense of feeling safe and secure in their living environment.
Main themes were reported with similar frequency regardless of the hospital site analysed, despite differences in hospital size and the annual visit rate among the four sites (Fig. 3A). The most frequently mentioned sub-themes (mentioned > 90% of the time) for each site (Fig. 3B) were (i) clinical interventions, (ii) communications between departments, (iii) professionalism, (iv) ED discharge and (v) home care. These themes represent the most salient topics of concern among older adults undergoing care transitions. For the remaining sub-themes, we noted only anecdotal differences (< 3%) among frequencies observed between sites.
A Barplot of the relative frequency (%, y-axis) of main themes (x-axis) coded in patient comments about their care transition. B Barplot of the relative frequency (%, y-axis) of the five most common sub-themes (x-axis). The legend to the right of each plot identifies the hospital. For each bar in the plots in both figures, the numerator is equal to the number of patients that mentioned a theme or sub-theme in their comment and the denominator is equal to the total number of patients who provided a comment, at a given hospital
Timeliness of services in and after the ED
The timeliness of receiving services in and after ED care was a transversal theme affecting all our main themes and subthemes. We did not identify the timeliness of services as an individual sub-theme in each of our major themes as it affected each theme individually. For Care in the ED, time was mentioned by 76 patients (100% of comments referenced wait times) affecting all 6 related subthemes (clinical interventions, explanations, security in the ED, communications between departments, professionalism, and accompaniment). For Living environment empowerment, time was mentioned by 14 patients, affecting 3 subthemes (home care, domestic help, and isolation. e.g., waiting list for domestic or home care services). For Conditions of stay in the ED, time was mentioned by 3 patients and concerned the time to receive a service in the ED, referring to 3 subthemes (sleeping conditions, food, and hygiene, e.g., spending the night on an uncomfortable gurney in a bright hallway, waiting to have soiled protective underwear changed, and time spent without eating). For ED discharge, time was mentioned by 26 patients and concerned all 3 subthemes (departure and whether patients felt discharge was too soon or took too long, delays in receiving transportation home, and sense of security waiting to be discharged). For examples and full comments, see Appendix C.
Emotional valence
We determined an indication of the patient’s sense of emotional valence (positivity, negativity, or neutrality) associated with each comment using an inductive approach. Interrater reliability was 0.94 using Krippendorff’s alpha for this coding of emotional valence. This emotional valence was mostly influenced by patients’ assessment of the quality of care, services received, and their timeliness. The emotional valence was positive among 81% of the comments in the cohort and positive in 76% of comments mentioning wait times. There were 70 comments that mentioned timeliness of care: 58 were positive, 11 negative and 7 neutral. Among the 11 negative comments, 10 reported long wait times. Because all four hospital sites had the same top sub-themes, we compared them on the emotional valence calculated by the number of positive, neutral, and negative comments (see Fig. 4). Overall, the clinical interventions and departure were the most positively described sub-themes, whereas communication in care and professionalism were the most frequently mentioned sub-theme with a negative valence. Home care services were the services that received neutral comments the most frequently and positive comments least frequently.
Histogram representing satisfaction (%, y-axis) regarding each sub-theme. Each bar denotes the proportion of negative, positive, and neutral comments that emerged among all comments mentioning the given sub-theme. Sub-themes are presented in decreasing frequency from left to right, and sub-themes were analysed for each site separately. Only the top five most frequent sub-themes are presented. Both time periods (before the COVID-19 pandemic and during the COVID-19 pandemic) were collapsed together
Effects of the COVID-19 pandemic
The proportion of positive comments relating to communication in care before the pandemic decreased in favor of more neutral comments after the start of the pandemic (14.2% increase in neutral comments, and 26.8% reduction in positive comments). Participants appeared to be more pleased with clinical care during the pandemic than before the pandemic (26.4% increase in positive comments), as well as their experiences with departing the ED (13.8% increase in positive comments). Chi-square tests of proportions of the effect of Valence ✕ Time Period yielded statistically significant effects of emotional valence as a function of the COVID-19 pandemic for all five themes. The proportions of emotional valences before and during the pandemic are presented in Table 2.
Discussion
We sought to generate a better understanding of patient’s care transition experiences that could be used in designing future patient-oriented interventions to improve care transitions in the post-COVID-19 context. We used open-ended comments to collect the perspectives of older adults’ experiences in the ED and their subsequent care transition from the ED. We conducted a qualitative content analysis using an inductive approach to identify themes and sub-themes among these comments to record concerns of patients from four Québec hospitals. We obtained a high level of agreement between coders and a clear coding scheme [40]. We also noted the emotional valence of each theme and sub-theme embedded within patients’ comments to understand if they were satisfied or not about the care transitions they experienced.
For each site, the most frequently mentioned sub-themes (mentioned over 90% of the time) were the clinical interventions received in the ED, communications in care, professionalism, discharge from the ED, and home care. These sub-themes represent the most salient topics of concern among older adults undergoing care transitions. Overall, quality of care was reported positively but communication in care and home care were qualified as neutral. These results are similar to findings by other authors [15, 41, 42] who report that older adults who undergo transitions in care also mention the quality of care received in hospital, but that communication during ED discharge and care transition planning can be fragmented. These themes will be important to consider in designing future patient-oriented interventions to improve care transitions in the post-COVID-19 context.
In home care, the emotional valence was mostly neutral, believed to be because a service had been organized in the ED but had not yet been delivered. As such, patients could only comment on the fact that a service was to come, but not on the quality or experience of receiving that service. The proportion of positive comments relating to communication in care before the pandemic decreased in favor of more neutral comments after the start of the pandemic. This is likely because of the service slowdown hospitals experienced at the beginning of the COVID-19 pandemic [43].
Similar results were found in qualitative analyses of patient and caregiver experiences, such that transport, communication, and services at home were commonly cited themes [44]. Lapses in communication were argued to be a major barrier to successful care transitions [44, 45]. Like other authors, we have also found that patients report an overall positive perception of acute care services [46]. The COVID-19 pandemic appears to have significantly impacted patient comments in our study. In a qualitative study on care transition experiences during the COVID-19 pandemic, communication was often perceived negatively, whereas in our study communication was often addressed neutrally [47].
We also observed that communications in care and professionalism at the ED are often negatively perceived and may be important barriers to successful care transitions among older adults. When patients are asked in surveys to score their experience in the ED, other authors have found that their answers are misquoted as they attribute positive scores regarding certain aspects they also expressed negative comments about [48]. These surveys may also inadvertently influence patients’ answers which either misrepresent some aspects or overrepresent some they would otherwise not have addressed. A deeper understanding of patients’ experiences could better guide patient-centered quality improvement initiatives compared to only using quantitative satisfaction scores (e.g., CTM-3). Future work using natural language processing (NLP) [49] could also potentially offer new opportunities to analyse patient-reported qualitative comments using patients’ own vocabulary to qualify their care transitions.
Orchestrating cooperation among health workers increases patient satisfaction [50] and reduces length of hospital stay [51]. If we can ensure that older adult patients are satisfied with their care, we may reap the rewards of fewer avoidable visits to the ED [52]. The benefits of a successful care transition are not limited to individual patients as they impact on communities and caregivers. The World Health Organization’s Decade of Health Aging Report considers this a crucial holistic indicator of care transition success [53].
Patients who are satisfied with their care and feel a sense of self-efficacy tend to stay out of the hospital longer and have more favorable health outcomes [54, 55]. Even so, the causal link between discharge planning, patient satisfaction, and hospital-level outcomes is still unclear [55]. When older adults feel empowered to manage their health at home, they show greater adherence to treatment plans [56]. It stands to reason that effective care transitions must provide clear instructions and resources to empower older adults to ensure a complete transition.
The American Geriatrics Society argues that its own guidelines for an ideal geriatric ED should be tailored to each ED based upon patient needs and available resources [57]. We found that patients appear to be satisfied overall with the acute interventions they receive in the four EDs we studied, but patients report neutral and negative comments relating to communication between the acute care provider and external clinics and specialists, their departure from the ED to their living environment, and the professionalism of the staff at the ED. All these elements would help the four EDs participating in this study to develop tailored interventions aiming to improve their local care transition best practices. In addition to using validated quantitative questionnaires such as the CTM-3 to measure quality of care transitions, our study also points to the usefulness of collecting open ended qualitative data from patients after their discharge to gain additional insights to inform a model for a care transition quality improvement initiative in other EDs. For our part, the comments collected and the results from this analysis will help in the design and implementation of a patient-oriented intervention to improve care transitions at the CISSS-CA immediately and in the post-COVID-19 era.
Overall, our results indicate that all the major sub-themes that emerged in our data appear to have been influenced by COVID-19. Most notable were changes in the proportion of positive comments relating to communication in care, which shifted in tone from positive to neutral. Future pandemic mitigation strategies will have to focus on improving communication throughout the care continuum (referrals, communications between clinics or specialties, patient and caregiver empowerment), and the preservation of homecare services. Among potential patient-oriented solutions that need further investigation would be better patient-centered communication skills among health professionals [58], addressing new patient decisional needs earlier [59, 60], decreasing loneliness and social isolation [61], having a single electronic medical record shared across different care settings [62] and accessible to patients themselves [63], better virtual care services and tools [14], and more efficient knowledge mobilization and management [64].
Strengths and limitations
The strengths of our study arise from our rigorous application of qualitative methodology, the strong inter-rater agreement, and the substantial random sample size that we recruited representing patients seen pre and during COVID-19 pandemic periods at four different EDs. Our strong inter-rater reliability indicates a clear coding scheme, which we attribute to a rigorous, iterative development of the coding scheme. Our large sample size can be explained by our desire to attain saturation of themes and sub-themes at all four sites.
This study also has limitations. First is the short follow-up time after departure from the ED as patients were called to participate between 1 and 7 days following discharge. Questions were fielded as soon as possible following this post-discharge period to capitalize on the primacy of the patient’s experience. While this primacy may have been a strength, this short follow-up time may not have left sufficient time for the patient to undergo all relevant aspects of the care transition, leading to an information bias. For instance, many patients reported a planned follow-up with a specialist but had yet to attend, so this experience was coded neutrally.
Second, since all our patients were recruited after a stay in the observation unit, we may have selected patients with short door-to-first contact wait times. This may have underestimated the impact of wait times on patient’s satisfaction with care because all patients were triaged to stretchers in the ED observation unit, and not strictly ambulatory where less urgent cases wait longer to see a doctor. As such, wait times to first contact with a nurse and doctor may have been shorter than ambulatory patients. However, this is not absolute because when stretchers were full, patients remained in the waiting room [65] and overcrowding can negatively influence total length of stay in the ED. In future work, door-to-doctor time (from when a patient arrives at the ED to their first personal interaction with a doctor) could be used to corroborate patient experiences, as this metric is significantly associated with worse patient experience in discharged patients [66].
Third, a selection bias may have occurred due to the utilization of the telephone to administer our questionnaire, limiting the participation of seniors who hear less well, those who do not use the telephone, and those who do not possess a telephone. However, this also allowed us to survey patients with reduced mobility. We also note a potential social desirability bias as patients satisfied with their care may have been more willing to participate, and dissatisfied patients may have declined due to a perceived risk that they may harm their relationship with their health professional. This potential bias did not prevent us from collecting negative comments and areas for improvement.
Fourth, patient comments for this study were collected over the telephone and transcribed immediately by a research professional. We did not audio record patients’ comments. This may have introduced an information bias such that the content of comments has been interpreted by the research professional conducting the interviews. Also, patients may not have completely understood our question about care transitions and answered our questions with their overall care in mind. This might reflect itself in the themes we identified that covered many aspects of quality of care within the ED and not specific to care transitions between the ED and the community. Although this may not have been clear for patients, we also believe that including feedback from patients about the complete care transition continuum before, during and after their ED visit is crucial because poor care transitions can find their root cause in the lack of meaningful advance care planning, iatrogenic complications related to ED conditions of stay, substandard communication with caregivers during ED stay, and deficient care coordination post ED discharge. Our collection method does not appear to have influenced the length of the comments collected, as ranged from a few words up to 100 words of text. We also took care to transcribe local metaphors and idioms provided by patients to emphasize the depth of their feelings. One man described feeling like “un chien dans un jeu de quilles” [“a dog in a bowling alley” analogous to feeling like you are out of place] when he arrived at the ED for care, indicating a strong feeling of being misunderstood and unwelcome. For more examples of each theme, their translations, and definitions, see Appendix C.
Conclusion
The present study offers a holistic understanding of individual experiences at the emergency department among older adult patients. Overall, patients were satisfied by their care, but they also reported neutral and negative comments relating to communication between the acute care provider and external clinics, specialists and community services, their departure from the hospital to their living environment, and the professionalism of the staff in the emergency department. The themes identified will help design patient-oriented interventions focused on improving the quality-of-care transitions from emergency departments for older adults.
Availability of data and materials
The datasets created and analysed during the current study are available from the corresponding author on reasonable request.
References
Dufour I, Chiu Y, Courteau J, Chouinard MC, Dubuc N, Hudon C. Frequent emergency department use by older adults with ambulatory care sensitive conditions: a population-based cohort study. Geriatr Gerontol Int. 2020;20(4):317–23.
Legramante JM, Morciano L, Lucaroni F, Gilardi F, Caredda E, Pesaresi A, et al. Frequent use of Emergency Departments by the Elderly Population when Continuing Care is not well established. PLoS ONE. 2016;11(12):e0165939.
Gettel CJ, Falvey JR, Gifford A, Hoang L, Christensen LA, Hwang U, et al. Emergency Department Care Transitions for patients with cognitive impairment: a scoping review. J Am Med Dir Assoc. 2022;S1525–8610(22):00154–2.
Gabayan GZ, Asch SM, Hsia RY, Zingmond D, Liang LJ, Han W, et al. Factors associated with short-term bounce-back admissions after emergency department discharge. Ann Emerg Med. 2013;62(2):136–144e1.
Coleman EA, Boult C, American Geriatrics Society Health Care Systems Committee. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51(4):556–7.
Zurlo A, Zuliani G. Management of care transition and hospital discharge. Aging Clin Exp Res. 2018;30(3):263–70.
Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39(3):238–47.
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing Hospital Readmission: current strategies and future directions. Annu Rev Med. 2014;65:471–85.
Naylor MD, Hirschman KB, McCauley K. Meeting the Transitional Care needs of older adults with COVID-19. J Aging Soc Policy. 2020;32(4–5):387–95.
Mueller AL, McNamara MS, Sinclair DA. Why does COVID-19 disproportionately affect older people? Aging. 2020;12(10):9959–81.
Dassieu L, Sourial N. Tailoring interventions for social isolation among older persons during the COVID-19 pandemic: challenges and pathways to healthcare equity. Int J Equity Health. 2021;20(1):26.
Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or Avoidance of Medical Care because of COVID-19–Related concerns — United States, June 2020. Morb Mortal Wkly Rep. 2020;69(36):1250–7.
Vaillancourt S, Seaton MB, Schull MJ, Cheng AHY, Beaton DE, Laupacis A, et al. Patients’ perspectives on outcomes of Care after Discharge from the Emergency Department: a qualitative study. Ann Emerg Med. 2017;70(5):648–658e2.
Dassieu L, Develay E, Beauchet O, Quesnel-Vallée A, Godard-Sebillotte C, Tchouaket E et al. Implementing a telehealth support tool for community-dwelling older adults during the COVID-19 pandemic: a qualitative investigation of provider experiences. J Aging Soc Policy. 2022;1–18. Published online ahead of print.
Kuipers SJ, Cramm JM, Nieboer AP. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Serv Res. 2019;19(1):13.
Mion LC, Palmer RM, Meldon SW, Bass DM, Singer ME, Payne SMC, et al. Case finding and referral model for emergency department elders: a randomized clinical trial. Ann Emerg Med. 2003;41(1):57–68.
Miller DK, Lewis LM, Nork MJ, Morley JE. Controlled trial of a geriatric case-finding and liaison service in an emergency department. J Am Geriatr Soc. 1996;44(5):513–20.
Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department–the DEED II study. J Am Geriatr Soc. 2004;52(9):1417–23.
Guttman A, Afilalo M, Guttman R, Colacone A, Robitaille C, Lang E, et al. An emergency department-based nurse discharge coordinator for elder patients: does it make a difference? Acad Emerg Med off J Soc Acad Emerg Med. 2004;11(12):1318–27.
Basic D, Conforti DA. A prospective, randomised controlled trial of an aged care nurse intervention within the Emergency Department. Aust Health Rev Publ Aust Hosp Assoc. 2005;29(1):51–9.
Hastings SN, Heflin MT. A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med off J Soc Acad Emerg Med. 2005;12(10):978–86.
Katz EB, Carrier ER, Umscheid CA, Pines JM. Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med. 2012;60(1):12–23e1.
Kessler C, Williams MC, Moustoukas JN, Pappas C. Transitions of care for the geriatric patient in the emergency department. Clin Geriatr Med. 2013;29(1):49–69.
Glaser B, Strauss A. Discovery of grounded theory: strategies for qualitative research. New York: Routledge; 2017. p. 282.
Glaser BG. Theoretical sensitivity: advances in the methodology of grounded theory [Internet]. Mill Valley, Calif.: Sociology Press; 1978 [cited 2023 Oct 23]. 164 p. Available from: http://books.google.com/books?id=73-2AAAAIAAJ.
Archambault PM, Rivard J, Smith PY, Sinha S, Morin M, LeBlanc A, et al. Learning Integrated Health System to mobilize context-adapted knowledge with a Wiki platform to improve the transitions of Frail seniors from hospitals and emergency departments to the community (LEARNING WISDOM): protocol for a mixed-methods implementation study. JMIR Res Protoc. 2020;9(8):e17363.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med J Assoc Am Med Coll. 2014;89(9):1245–51.
Institut national de santé publique du Québec. Ligne du temps COVID-19 au Québec [Internet]. INSPQ. 2022 [cited 2022 Oct 19]. Available from: https://www.inspq.qc.ca/covid-19/donnees/ligne-du-temps.
Coleman EA. Mesures Transitoires de Soins (MTS-3) [French version of the CTM-3] [Internet]. All Tools and Resources: The Care Transitions Program. 2006 [cited 2022 Jun 6]. Available from: https://caretransitions.org/all-tools-and-resources/.
Kolk D, Kruiswijk AF, MacNeil-Vroomen JL, Ridderikhof ML, Buurman BM. Older patients’ perspectives on factors contributing to frequent visits to the emergency department: a qualitative interview study. BMC Public Health. 2021;21(1):1709.
College of Physicians and Surgeons of Nova Scotia. Professional standard and guidelines regarding informed patient consent to treatment [Internet]. Bedford, Nova Scotia, Canada. ; 2016 Dec. Available from: https://cpsns.ns.ca/wp-content/uploads/2017/10/Informed-Patient-Consent-to-Treatment.pdf.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Shadmi E, Zisberg A, Coleman EA. Translation and validation of the care transition measure into Hebrew and Arabic. Int J Qual Health Care. 2009;21(2):97–102.
Reeves S, Kuper A, Hodges BD. Qualitative research methodologies: ethnography. BMJ. 2008;337:a1020.
Lewis-Beck M, Bryman A, Liao T. Ethnographic Content Analysis. In: The SAGE Encyclopedia of Social Science Research Methods [Internet]. Thousand Oaks: SAGE Publications, Inc.; 2004 [cited 2022 Jun 30]. p. 326–326. Available from: https://sk.sagepub.com/reference/socialscience/n292.xml.
Krippendorff K. Computing Krippendorff’s Alpha-Reliability. Dep Pap ASC [Internet]. 2011; Available from: https://repository.upenn.edu/asc_papers/43.
Parry C, Mahoney E, Chalmers SA, Coleman EA. Assessing the quality of transitional care: further applications of the care transitions measure. Med Care. 2008;46(3):317–22.
Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. Tenth edition. Philadelphia: Wolters Kluwer Health; 2017. p. 784.
Krippendorff K. Content Analysis An Introduction to Its Methodology. [Internet]. 4th ed. Thousand Oaks: SAGE Publications, Incorporated; 2018 [cited 2023 Oct 23]. Available from: https://public.ebookcentral.proquest.com/choice/PublicFullRecord.aspx?p=7106785.
Leff B, Burton L, Mader S, Naughton B, Burl J, Clark R, et al. Satisfaction with hospital at Home Care. J Am Geriatr Soc. 2006;54(9):1355–63.
Leff B, Burton L, Mader SL, Naughton B, Burl J, Inouye SK, et al. Hospital at home: feasibility and outcomes of a program to provide Hospital-Level Care at Home for acutely Ill older patients. Ann Intern Med. 2005;143(11):798–808.
Hohl CM, Rosychuk RJ, Hau JP, Hayward J, Landes M, Yan JW, et al. Treatments, resource utilization, and outcomes of COVID-19 patients presenting to emergency departments across pandemic waves: an observational study by the Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN). Can J Emerg Med. 2022;24(4):397–407.
Takahashi PY, Finnie DM, Quigg SM, Borkenhagen LS, Kumbamu A, Kimeu AK, et al. Understanding experiences of patients and family caregivers in the Mayo Clinic Care Transitions program: a qualitative study. Clin Interv Aging. 2019;14:17–25.
Lagacé M, Fraser S, Ranger MC, Moorjani-Houle D, Ali N. About me but without me? Older adult’s perspectives on interpersonal communication during care transitions from hospital to seniors’ residence. J Aging Stud. 2021;57:100914.
Levine DM, Pian J, Mahendrakumar K, Patel A, Saenz A, Schnipper JL. Hospital-Level Care at Home for acutely Ill adults: a qualitative evaluation of a Randomized Controlled Trial. J Gen Intern Med. 2021;36(7):1965–73.
Ganton J, Hubbard A, Kovacs Burns K. Patients with COVID-19 share their experiences of recovering at home following hospital care transitions and discharge preparation. Health Expect Int J Public Particip Health Care Health Policy. 2022. https://doi.org/10.1111/hex.13595.
Gallan A, Girju M, Girju R. Perfect ratings with negative comments: learning from contradictory patient survey responses. Patient Exp J. 2017;4(3):15–28.
Rahimi SA, Légaré F, Sharma G, Archambault P, Zomahoun HTV, Chandavong S, et al. Application of Artificial Intelligence in Community-based primary Health Care: systematic scoping review and critical Appraisal. J Med Internet Res. 2021;23(9):e29839.
Deeter-Schmelz DR, Norman Kennedy K. Patient care teams and customer satisfaction: the role of team cohesion. J Serv Mark. 2003;17(7):666–84.
Blewett LA, Johnson K, McCarthy T, Lackner T, Brandt B. Improving geriatric transitional care through inter-professional care teams. J Eval Clin Pract. 2010;16(1):57–63.
Warren C, Lemieux AA, Phoenix Bittner N. Excellence in Population Health: a successful community-based Care transitions Program Model. Prof Case Manag. 2019;24(1):39–45.
World Health Organization. Decade of healthy ageing: baseline report [Internet]. Geneva: World Health Organization. ; 2020. Available from: https://apps.who.int/iris/handle/10665/338677.
Sarkar U, Ali S, Whooley MA. Self-efficacy as a marker of cardiac function and predictor of Heart Failure hospitalization and mortality in patients with stable coronary Heart Disease: findings from the Heart and Soul Study. Health Psychol. 2009;28(2):166–73.
Fox MT, Persaud M, Maimets I, Brooks D, O’Brien K, Tregunno D. Effectiveness of early discharge planning in acutely ill or injured hospitalized older adults: a systematic review and meta-analysis. BMC Geriatr. 2013;13:70.
Rees S, Williams A. Promoting and supporting self-management for adults living in the community with physical chronic Illness: a systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Libr Syst Rev. 2009;7(13):492–582.
Carpenter CR, Bromley M, Caterino JM, Chun A, Gerson LW, Greenspan J, et al. Optimal older adult emergency care: introducing Multidisciplinary Geriatric Emergency Department guidelines from the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine. J Am Geriatr Soc. 2014;62(7):1360–3.
Izumi SS, Caron D, Guay-Bélanger S, Archambault P, Michaels L, Heinlein J, et al. Development and evaluation of Serious Illness Conversation Training for Interprofessional Primary Care teams. J Palliat Med. 2023;26(9):1198–206.
Stacey D, Ludwig C, Archambault P, Smith M, Taljaard M, Carley M, et al. Decisions and decisional needs of canadians from all provinces and territories during the COVID-19 pandemic: Population-based cross-sectional surveys. JMIR Public Health Surveill. 2023;9:e43652.
Derrer-Merk E, Reyes-Rodriguez MF, Soulsby LK, Roper L, Bennett KM. Older adults’ experiences during the COVID-19 pandemic: a qualitative systematic literature review. BMC Geriatr. 2023;23(1):580.
Briere J, Wang SH, Khanam UA, Lawson J, Goodridge D. Quality of life and well-being during the COVID-19 pandemic: associations with loneliness and social isolation in a cross-sectional, online survey of 2,207 community-dwelling older canadians. BMC Geriatr. 2023;23(1):615.
Sudat SEK, Robinson SC, Mudiganti S, Mani A, Pressman AR. Mind the clinical-analytic gap: electronic health records and COVID-19 pandemic response. J Biomed Inform. 2021;116:103715.
Hägglund M, McMillan B, Whittaker R, Blease C. Patient empowerment through online access to health records. BMJ. 2022;378:e071531.
Said Abasse K, Toulouse-Fournier A, Paquet C, Côté A, Smith PY, Bergeron F, et al. Collaborative writing applications in support of knowledge translation and management during pandemics: a scoping review. Int J Med Inf. 2022;165:104814.
Cheng I, Lee J, Mittmann N, Tyberg J, Ramagnano S, Kiss A, et al. Implementing wait-time reductions under Ontario government benchmarks (pay-for-Results): a Cluster Randomized Trial of the Effect of a physician-nurse supplementary triage assistance team (MDRNSTAT) on emergency department patient wait times. BMC Emerg Med. 2013;13(1):17.
Nyce A, Gandhi S, Freeze B, Bosire J, Ricca T, Kupersmith E, et al. Association of Emergency Department Waiting Times with patient experience in admitted and discharged patients. J Patient Exp. 2021;8:23743735211011404.
Acknowledgements
We acknowledge the support of participating patients and their caregivers. We also thank David Buckeridge and Jean-Louis Denis for their support and expertise in planning the LEARNING WISDOM project.
Network of Canadian Emergency Researchers
Patrick Archambault, MD, MSc, Marcel Émond, MD, MSc, Eric Mercier, MD, MSc.
Funding
This study was funded by an Embedded Clinician Salary Award (ECRA) awarded to PMA from the Canadian Institutes for Health Research (CIHR) (#201603), a Fonds de recherche du Québec – Santé (FRQS) Senior Clinical Scholar Award (#283211), and a CIHR Project Grant (#378616). NG received a Master’s Award: Canada Graduate Scholarships Award (CIHR) for this work (#202112). The funding bodies had no role in the design of the study, collection, or analysis of the data, interpretation of the results, or writing of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
1. Study concept and design. 2. Acquisition of the data. 3. Analysis and interpretation of the data. 4. Drafting of the manuscript. 5. Critical revision of the manuscript for important intellectual content. 6. Statistical expertise. 7. Obtained funding. 8. Administrative, technical, or material support. 9. Study supervision. 1. VC, NG, MM, JC, JR, ÉM, IP, ST, and PMA conceptualized the study and analysis. NS and LC provided content expertise in study design and outcome selection. 2. ÉC, LL, LA, RG, PS, JR, ST, RS, and PMA collected and managed participant data. 3. VC, NG, and PMA conducted the analysis. 4. VC, NG, and PA wrote the first draft of the manuscript. 5. AAB, YC, CD, ME, RF, MSH, AL, FL, DM, DR, SS, MJS, HOW, and PMA. All authors (VC, NG, ÉC, LL, JR, MM, JC, YC, FL, MSH, LBC, AAB, NS, ÉM, CD, RF, AL, DM, DR, SS, MJS, HOW, ME, JR, IP, ST, RS, RG, LA, PYS and PMA) critically reviewed the manuscript and provided comments to improve the manuscript. All authors read and approved the final manuscript. 6. RS, ST, YC and FL provided statistical and methodological expertise. 7. AAB, YC, CD, ME, RF, MSH, AL, FL, DM, DR, SS, MJS, HOW, and PMA obtained funding for this study. 8. ÉC, LL, PYS, RG and LA provided administrative and technical support. 9. PMA is the principal investigator.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol for this study was approved by the CISSS-CA Ethics Review Committee (project #2018 − 462, 2018-007). Patients had to be able to understand French and provide informed consent. To demonstrate the capacity to provide informed consent, patients were required to summarize—in their own words—their understanding of the study to consent to, based on the Nova Scotia Criteria. Participants were also made aware that it would not be possible to identify individual participants in the published results.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Couture, V., Germain, N., Côté, É. et al. Transitions of care for older adults discharged home from the emergency department: an inductive thematic content analysis of patient comments. BMC Geriatr 24, 8 (2024). https://doi.org/10.1186/s12877-023-04482-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04482-0