Abstract
Background
It is essential to assess the need for palliative care and the life prognosis of elderly nursing home residents with an advanced chronic condition, and the NECPAL ICO-CCOMS©4.0 prognostic instrument may be adequate for both purposes. The objective of this study was to examine the predictive capacity of NECPAL, the Palliative Prognosis Index, and the PROFUND index in elderly residents with advanced chronic condition with and without dementia, comparing their results at different time points.
Methods
This prospective observational study was undertaken in eight nursing homes, following the survival of 146 residents with advanced chronic condition (46.6% with dementia) at 3, 6, 12, and 24 months. The capacity of the three instruments to predict mortality was evaluated by calculating the area under the receiver operating characteristic curve (AUC), with 95% confidence interval, for the global population and separately for residents with and without dementia.
Results
The mean age of residents was 84.63 years (± 8.989 yrs); 67.8% were female. The highest predictive capacity was found for PROFUND at 3 months (95%CI: 0.526–0.756; p = 0.016), for PROFUND and NECPAL at 12 months (non-significant; AUC > 0.5), and NECPAL at 24 months (close-to-significant (AUC = 0.624; 95% CI: 0.499–0.750; p = 0.053). The highest capacity at 12 months was obtained using PROFUND in residents with dementia (AUC = 0.698; 95%CI: 0.566–0.829; p = 0.003) and NECPAL in residents without dementia (non-significant; AUC = 0.649; 95%CI: 0.432–0.867; p = 0.178). Significant differences in AUC values were observed between PROFUND at 12 (p = 0.017) and 24 (p = 0.028) months.
Conclusions
PROFUND offers the most accurate prediction of survival in elderly care home residents with advanced chronic condition overall and in those with dementia, especially over the short term, whereas NECPAL ICO-CCOMS©4.0 appears to be the most useful to predict the long-term survival of residents without dementia. These results support early evaluation of the need for palliative care in elderly care home residents with advanced chronic condition.
Similar content being viewed by others
Introduction
The World Health Organization [1] has called for the implementation of an integrated care model for patients with chronic disease, combining specific therapy to prolong life with palliative care to relieve pain and suffering. Palliative care becomes more important with the progression of disease and is traditionally offered in its final stages, at the end of life. The integrated model is particularly designed for patients with long-term chronic diseases, including chronic obstructive pulmonary disease (COPD), heart or kidney failure, or neurodegenerative disease [1,2,3]. A key issue raised by this model is the timing of palliative care delivery [4, 5]. This challenge is addressed in the Catalan care model for patients with chronic diseases [6] by differentiating among complex chronicity, advanced chronic condition ( ACC), and terminal stage.
The life prognosis of patients is evidently crucial information; however, if it is the sole parameter considered, it might be erroneously concluded that palliative care is only necessary in the terminal stage of disease. Over the past few years, instruments have been developed to combine life prognosis estimation with the identification of palliative care needs [5, 7,8,9], yielding a more profound and realistic perspective [8,9,10,11]. Among these, NECPAL ICO-CCOMS© [12] represented a major advance by allowing identification of palliative needs of individuals defined as having advanced complex care disease (ACD). The current version (3.1) includes the question “Would you be surprised if the patient died over the next year?” for subjective assessment of the prognosis [11, 13, 14] as well as nine items on physical and psychosocial needs. Version 4.0 of this instrument was recently developed [8, 9, 15], preserving the “surprise” question and considering six of the same parameters to classify three prognostic stages for estimating patient survival. This version was tested in patients with different diseases in various clinical settings and offered a good prediction of survival at 24 months [9]. However, its performance has not been compared with that of other instruments used in patients with chronic disease, such as the Palliative Prognostic Index (PPI) [16] or PROFUND index [17,18,19]. It is also important to select instruments for prognostic estimation according to the disease and setting of patients [9, 16, 20,21,22]. This process is of particular interest in people with dementia, given the need to act early in accordance with the preferences of patients and to minimize invasive procedures at the end of life [23,24,25,26,27,28,29,30,31,32]. However, generic and nonspecific life prognosis evaluation tools have not demonstrated good predictive capacity in individuals with dementia [8, 9, 20].
Nursing home residents include many elderly individuals with dementia, which predisposes sufferers to institutionalization [33,34,35,36]. Reports on the prevalence of people with dementia in European nursing homes have ranged between 85.2% in Austria and 51.8% in Germany [37, 38]. In Spain, cognitive impairment was detected in 56.4% of residents of Andalusian nursing homes [10]. In general, nursing homes have only limited material, human, and training resources to meet the considerable demand for palliative care [39,40,41]; nevertheless, specific instruments may be required for residents with dementia, whose needs for palliative care may differ from those of residents without this condition [42].
The application of instruments with prognostic value that consider the presence of cognitive impairment and complex chronic disease can be crucial for planning the care of residents, and it is necessary to verify the most appropriate instrument for this purpose.
This article aimed to compare the capacity of three widely used prognostic instruments (NECPAL4.0, PPI, and PROFUND) to predict the survival of elderly nursing home residents with ACC over the short- and long-term, considering the presence/absence of diagnosed dementia.
Methodology
Design
This prospective observational study was performed in nursing homes, following the survival of study participants at 3, 6, 12, and 24 months.
Participants and data gathering
The study population comprised residents of eight nursing homes in Granada and Jaen (Southern Spain) who participated in the Nursing Homes End of Life Program (NU-HELP) [10, 43]. Nurses with more than 6 months’ work experience and specifically trained in data gathering selected 20 residents at each center who had no end date for their stay in the home and met the following criteria of the Spanish Society of Palliative Care (SECPAL) for ACC [44]: the presence of advanced, progressive, and incurable disease with no reasonable possibility of therapeutic response; the presence of numerous conditions or intense, multiple, multifactorial, and changing symptoms; the cause of major emotional impact on patients, family members, and staff; and/or life expectancy of ≤ 6 months.
The designated nurses gathered data between March 2019 and March 2022, recording the survival of residents at 3, 6, 12, and 24 months post-enrolment. The research team were available by telephone to provide the nurses with any specific or complementary information required and made periodic visits to the centers to monitor the process. Informed consent was obtained from all participants in the study, being provided by representatives or appointed relatives of the residents with dementia. Out of the total of 160 residents selected for study, consent was not given by 11 residents or representatives, leaving a final sample of 149 residents.
Variables and instruments
Table 1 reports information on the different instruments employed in this study. The main outcome variable was survival at 3, 6, 12, and 24 months post-enrolment.
Data analysis
Quantitative variables were expressed as means with standard deviations and categorical variables as absolute frequencies and percentages. Variables were non-normally distributed according to the Kolmogorov-Smirnov test; therefore, non-parametric tests were applied, using the chi-square or Fisher test to verify independence among categorical variables and the Mann-Whitney U test to evaluate the association between independent samples (patients with and without dementia). The predictive capacity of the instruments for mortality was evaluated by calculating the area under the receiver operating characteristic curve (AUC) with 95% confidence interval. Analysis was performed for the global population and separately for residents with and without dementia. IBM SPSS v.25 © (IBM Corporation, Armonk, NY) was used for data analyses, considering p ≤ 0.05 to be significant.
Ethical oversight
All participants or appointees (for patients with cognitive impairment) signed their informed consent. The study was approved by the Research Ethics Committee (AP-0105-2016), and data were treated in accordance with national data protection regulations [46, 47].
Results
Description of participants
Among the 149 residents selected from the NUHELP project [43], 146 had all records required for analyses (Fig. 1); the three residents (2%) with incomplete records were excluded from the study, leaving a final sample of 146 residents, including 68 (46.6%) with dementia.
The mean age of residents was 84.63 ± 8.989 years, and 99 were female (67.8%). After dementia (n = 68, 46.6%), the second most prevalent condition was chronic heart disease (CHD) (n = 57, 39%). Seventy-nine residents (54.1%) had ACD according to NECPAL ICO-CCOMS© 3.1. The mean PPI score was 2.53 (± 2.578), i.e., 42% of individuals with similar characteristics could be expected to die within six months (180 days). The mean PROFUND index score was 8.99 ± 3.996, indicating a mean expected survival of 9.3 months post-assessment.
Residents with and without dementia only significantly differed in the percentage with cancer (p < 0.001) COPD (p < 0.001), or CHD (p < 0.001), with CHD being the most prevalent comorbidity in both groups. They did not significantly differ in prognostic instrument scores or percentage with ACD by NECPAL (Table 2). Table 3 shows the survival stages of residents with ACD (n = 79) according to NECPAL-ICO-CCOMS©4.0.
Comparison of mortality prediction between residents with and without Dementia
Fifty-six residents (38.4%) died during the follow up. The mean survival of deceased residents was 373.5 ± 222.328 days, with no significant differences between those with and without dementia. Thirty of these deaths (20.5% of total sample) occurred within 12 months. At the end of the follow-up, 45.6% of residents with dementia and 32.1% of those without dementia had died, although this difference was only statistically significant at three months (p = 0.004), when no deaths were recorded among residents without dementia (Table 4).
The majority of residents with ACC who had died were in survival stage II by NECPAL4.0 at three months (n = 18, 32.1%), while their mean PPI score was 2.55 (± 2.621) and mean PROFUND score 9.16 (± 4.080). Results of these instruments did not differ between deceased residents with and without dementia except for a close-to significant difference (p = 0.051) in PROFUND score (Table 4).
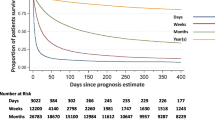
Mortality prediction capacity of tools. ROC curves
For the global sample, all three instruments had an AUC > 0.5 at three months. The best result was obtained with PROFUND at three months (95%CI: 0.526–0.756; p = 0.016) and again, although without statistical significance, at six months, (p = 0.106), while both PROFUND and NECPAL4.0 had an AUC > 0.5 at 12 months but without statistical significance (p = 0.310 and p = 0.212, respectively). All three instruments had an AUC > 0.5 at 24 months, when the best result was obtained using NECPAL, with a close-to-significant result (AUC = 0.624; 95%CI: 0.499–0.750; p = 0.053) (Fig. 2).
Among the residents with dementia, the highest AUC value was obtained with the PROFUND index at all time points, reaching statistical significance at 12 months (AUC = 0.698; 95%CI: 0.566–0.829; p = 0.003). Among those without dementia, the highest value was observed with NECPAL4.0 at 12 months (AUC = 0.649; 95%CI: 0.432–0.867; p = 0.178), although statistical significance was not reached. Residents with and without dementia significantly differed in AUC values for PROFUND at 12 (p = 0.017) and 24 (p = 0.028) months (Fig. 3). Data on the ROC curves of instruments for accumulated time periods are included as supplementary material. ROC curves of instruments at the different measurement time points for all patients who died and for those with and without dementia are given as supplementary material.
Discussion
This study compared the predictive capacity of the new version 4.0 of the NECPAL instrument [8, 9, 15], PROFUND index [17, 18], and PPI [16, 48] at four time points (3, 6, 12, and 24 months) in a sample of elderly nursing home residents with ACC with and without dementia. Higher predictive capacities were found for NECPAL4.0 and PROFUND according to the presence/absence of dementia and measurement time point.
The age and sex profiles of the residents were similar to those in previous studies of this type in the nursing home setting [37, 49,50,51,52,53,54,55]. The percentage of residents classified with ACD by NECPAL3.1 was somewhat lower than described by Martínez-Muñoz [56] but higher than reported by da Costa et al. [57]. The percentage of residents with positive responses to the “surprise” question was higher than in previous studies that included this item in the study of other instruments [54, 55].
Similar proportions of residents with ACC were in NECPAL survival stages I and II and only a small proportion in stage III, implying a lower median survival (3.6 months). A higher proportion of patients were in stage III in the investigation by Calsina-Berna et al. [58], which included a larger percentage of patients receiving palliative care; however, few studies have been published on this issue, which warrants further research.
PROFUND results [7, 18] were in agreement with the findings by Da Costa et al. [57] and Moretti et al. [19] of a high or very high risk of mortality (≥ 7 points) in most residents. With regard to PPI findings, a mean of 4.5 points was obtained by Nieto-Martín et al. [16], indicating a worse survival than predicted in the present series.
There was a lower percentage of deaths in the present study than in some other studies of residents with dementia [23, 59, 60], although these only reported the mortality for periods < 12 months. Studies in nursing homes with a 24-month follow-up by Turrillas et al. [9] and Martínez-Muñoz et al. [56] observed a higher mortality rate (43% and 52.74%, respectively) at 24 months in comparison to the present series (38.4% ). Most residents who died within two years had dementia. Bernabeu-Wittel et al. [17] described the presence of dementia as a predictor of mortality and included it in the PROFUND index. In general, the instruments under study described a worse prognosis for the residents with versus without dementia, although dementia often coexists with other diseases that might affect the prognosis.
In the global sample, the highest AUC was obtained at 3 and 6 months using the PROFUND index [17, 18], with statistical significance, while the highest AUC at 24 months was obtained with NECPAL4.0, with a close-to-significant result, supporting data in the validation study for this instrument [9].
PROFUND obtained higher AUC values in the patients with versus without dementia, reaching statistical significance at 12 and 24 months. This might be attributable to the inclusion of a specific analytical parameter (hemoglobin < 10 g/dL) known to predict a worse prognosis and improve the prognostic accuracy in patients with different diseases, including dementia. NECPAL4.0 showed higher AUC values for the residents without dementia, in line with the finding by the original validation study of a worse predictive capacity in patients with versus without dementia [9]. The lowest AUC values were observed with PPI [16] at all follow-up times, and no statistically significant results were observed.
Strengths and limitations
A larger sample of residents would have increased the statistical power, thereby improving the detection of statistical significance in trends identified in the present study. A further limitation was the lack of data on comorbidities in the groups with and without dementia, which should be provided separately in future studies, given that dementia is frequently accompanied by other diseases that can affect the prognosis. Only patients diagnosed with dementia were considered for this study. It should be considered for results interpretation that residents who have undiagnosed dementia or have some cognitive impairment have been excluded in the analysis. It should also be taken into account that part of the survival follow-up coincided with the COVID19 pandemic, although the nursing homes reported that none of the residents in the study died from this cause.
Conclusions
According to these findings, PROFUND is the best instrument to predict survival in nursing home residents with ACC in general and in those with dementia, especially over the short term, whereas NECPAL4.0 offers the best performance in residents without dementia and over the long term (≥ 24 months). Hence, these instruments complement each other in terms of type of resident and time scale. NECPAL4.0 not only covers a longer time period than PROFUND but also offers information on the palliative needs of residents, helping nursing homes to prioritize resources for their adequate care.
A nursing home policy to estimate the prognosis of elderly people with ACC facilitates the early implementation of palliative care and supports multidimensional evaluation, advanced care planning, and resource management.
Combined evaluation of the care needs and the prognosis of residents provides a global view, whereas consideration of the prognosis alone may lead to the erroneous conclusion that palliative care is only necessary during the final stages of disease.
The detection of palliative care needs and application of a prognostic instrument with good predictive capacity in residents with dementia can improve their palliative care, reducing differences with dementia-free residents with ACC.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
References
Organización M, de la Salud OMS. Cuidados paliativos [Internet]. Organizacion mundial de la salud. 2020 [cited 2022 Aug 23]. Available from: https://www.who.int/es/news-room/fact-sheets/detail/palliative-care.
Blay C, Limón E. Bases para un modelo catalán de atención a las personas con necesidades complejas [Internet]. Vol. 6, Generalitat de Catalunya. Programa de prevenció i atenció a la cronicitat. 2017. Available from: http://salutweb.gencat.cat/web/.content/home/ambits_tematics/linies_dactuacio/model_assistencial/atencio_al_malalt_cronic/documents/bases_modelo_personas_complejidad_v_6.pdf.
Consejería de Salud y Familia. Cuidados Paliativos. Proceso Asistencial Integrado [Internet]. 2019. Available from: http://hdl.handle.net/10668/3026.
Boyd M, Frey R, Balmer D, Robinson J, McLeod H, Foster S, et al. End of life care for long-term care residents with Dementia, chronic Illness and cancer: prospective staff survey. BMC Geriatr. 2019;19(1):1–9.
Thomas K, Wilson JA, Team GSF. The Gold Standards Framework - Proactive Identification Guidance (PIG). 2016;6:2. Available from: https://www.goldstandardsframework.org.uk/cd-content/uploads/files/PIG/NEW PIG – 20.1.17 KT vs17.pdf.
Boyd K, Murray SA. Recognising and managing key transitions in end of life care. BMJ. 2010;341(7774):649–52.
The Gold Standards Framework. The GSF Prognostic Indicator Guidance. End Life Care [Internet]. 2010;4(1):62–4. Available from: http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/EOLC-prognostic-indicator-guide.pdf.
Gómez-Batiste X, Turrillas P, Tebé C, Calsina-Berna A, Amblàs-Novellas J. NECPAL tool prognostication in advanced chronic Illness: a rapid review and expert consensus. BMJ Support Palliat Care. 2020;12(e1):1–11.
Turrillas P, Peñafiel J, Tebé C, Amblàs-Novellas J, Gómez-Batiste X. NECPAL prognostic tool: a palliative medicine retrospective cohort study. BMJ Support Palliat Care. 2021;1–10.
Esteban-Burgos AA, Lozano-Terrón MJ, Puente-Fernandez D, Hueso-Montoro C, Montoya-Juárez R, García-Caro MP. A new approach to the identification of palliative care needs and advanced chronic patients among nursing home residents. Int J Environ Res Public Health. 2021;18(6):1–14.
Gómez-Batiste X, Martínez-Muñoz M, Blay C, Amblàs J, Vila L, Costa X, et al. Utility of the NECPAL CCOMS-ICO© tool and the Surprise question as screening tools for early palliative care and to predict mortality in patients with advanced chronic conditions: a cohort study. Palliat Med. 2017;31(8):754–63.
Gómez-Batiste X, Martínez-Muñoz M, Blay C, Amblàs J, Vila L, Costa X, et al. Identifying patients with chronic conditions in need of palliative care in the general population: development of the NECPAL tool and preliminary prevalence rates in Catalonia. BMJ Support Palliat Care. 2013;3(3):300–8.
Carvalho JR, Vasconcelos M, Marques da Costa P, Marinho RT, Fatela N, Raimundo M, et al. Identifying palliative care needs in a Portuguese liver unit. Liver Int. 2018;38(11):1982–7.
de la Rica Escuín ML. Necesidad de atención paliativa a residentes institucionalizados con enfermedades crónicas evolutivas con pronóstico de vida limitado. Med Paliativa [Internet]. 2016;23(4):183–91. https://doi.org/10.1016/j.medipa.2014.04.004.
Gómez-Batiste X, Turrillas P, Tebé C, Calsina-Berna A, Amblàs-Novellas J. NECPAL tool prognostication in advanced chronic Illness: a rapid review and expert consensus. BMJ Support Palliat Care. 2022;12(e1):e10–e20. https://doi.org/10.1136/bmjspcare-2019-002126.
Nieto Martín MD, Bernabeu Wittel M, De La Higuera Vila L, Mora Rufete A, Barón Franco B. Ollero Baturone M. Recalibración Del Palliative Prognostic Index en pacientes con enfermedades médicas avanzadas. Rev Clin Esp. 2013;213(7):323–9.
Bernabeu-Wittel M, Ollero-Baturone M, Moreno-Gaviño L, Barón-Franco B, Fuertes A, Murcia-Zaragoza J et al. Development of a new predictive model for polypathological patients. The PROFUND index. Vol. 22, European Journal of Internal Medicine. 2011. p. 311–7.
Bernabeu-Wittel M, Moreno-Gaviño L, Ollero-Baturone M, Barón-Franco B, Díez-Manglano J, Rivas-Cobas C, et al. Validation of PROFUND prognostic index over a four-year follow-up period. Eur J Intern Med. 2016;36:20–4.
Moretti D, Buncuga MG, Laudanno CD, Quiñones ND, Scolari Pasinato CM, Rossi FE. Índice PROFUND Y Valoración Global Subjetiva. Valor pronóstico en pacientes pluripatológicos internados. Med (B Aires). 2020;80(6):622–32.
Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012;307(2):182–92. https://doi.org/10.1001/jama.2011.1966.
Zucchelli A, Vetrano DL, Grande G, Calderón-Larrañaga A, Fratiglioni L, Marengoni A, et al. Comparing the prognostic value of geriatric health indicators: a population-based study. BMC Med. 2019;17(1):1–10.
Bergstraesser E, Thienprayoon R, Brook LA, Fraser LK, Hynson JL, Rosenberg AR, et al. Top ten tips palliative care clinicians should know about prognostication in children. J Palliat Med. 2021;24(11):1725–31.
Loizeau AJ, Shaffer ML, Habtemariam DA, Hanson LC, Volandes AE, Mitchell SL. Association of prognostic estimates with burdensome interventions in nursing home residents with advanced Dementia. JAMA Intern Med. 2018;178(7):922–9.
Almagro P, Ponce A, Komal S, de la Asunción Villaverde M, Castrillo C, Grau G, Simon L, de la Sierra A. Multimorbidity gender patterns in hospitalized elderly patients. PLoS ONE. 2020;15(1):e0227252. https://doi.org/10.1371/journal.pone.0227252. PMID: 31990911; PMCID: PMC6986758.
Brown MA, Sampson EL, Jones L, Barron AM. Prognostic indicators of 6-month mortality in elderly people with advanced Dementia: a systematic review. Palliat Med. 2013;27(5):389–400.
Kusumastuti S, Hoogendijk EO, Gerds TA, Lund R, Mortensen EL, Huisman M et al. Do changes in frailty, physical functioning, and cognitive functioning predict mortality in old age? Results from the Longitudinal Aging Study Amsterdam. BMC Geriatr [Internet]. 2022;22(1):1–10. https://doi.org/10.1186/s12877-022-02876-0.
Palacio GC, Krikorian A, Gómez-Romero MJ, Limonero JT. Resilience in caregivers: a systematic review. Am J Hosp Palliat Med. 2020;37(8):648–58.
Overbeek FCMS, Goudzwaard JA, van Hemmen J, van Bruchem-Visser RL, Papma JM, Polinder-Bos HA, Mattace-Raso FUS. The Multidimensional Prognostic Index predicts mortality in older outpatients with cognitive decline. J Clin Med. 2022;11(9):2369. https://doi.org/10.3390/jcm11092369.
Blay C, Martori JC, Limón E, Oller R, Vila L, Gómez-Batiste X. Busca tu 1%: prevalencia y mortalidad de una cohorte comunitaria de personas con enfermedad crónica avanzada y necesidades paliativas. Vol. 51, Atención Primaria. 2019. p. 71–9.
Gómez-Batiste X, Martínez-Muñoz M, Blay C, Amblàs J, Vila L, Costa X, et al. Prevalence and characteristics of patients with advanced chronic conditions in need of palliative care in the general population: a cross-sectional study. Palliat Med. 2014;28(4):302–11.
de Miguel C, Ruiz S, de la Uz A, Merino E, Gutierrez A, Sanz L et al. ¿Son complejos los pacientes atendidos por unidades de cuidados paliativos domiciliarias? Med Paliativa. 2018;25(1):7–16. https://doi.org/10.1016/j.medipa.2016.06.003.
Murray SA, Kendall M, Mitchell G, Moine S, Amblàs-Novellas J, Boyd K. Palliative care from diagnosis to death. BMJ. 2017;356:j878. https://doi.org/10.1136/bmj.j878.
Hajek A, Luppa M, Brettschneider C, van der Leeden C, van den Bussche H, Oey A, et al. Correlates of institutionalization among the oldest old—evidence from the multicenter AgeCoDe-AgeQualiDe study. Int J Geriatr Psychiatry. 2021;36:1095–102.
Villars H, Gardette V, Frayssignes P, Deperetti E, Perrin A, Cantet C et al. Predictors of nursing home placement at 2 years in Alzheimer’s Disease: a follow-up survey from the THERAD study. Vol. 37, Int J Geriatr Psychiatry. 2022.
Toot S, Swinson T, Devine M, Challis D, Orrell M. Causes of nursing home placement for older people with Dementia: a systematic review and meta-analysis. Int Psychogeriatr. 2017;29(2):195–208.
Longitudinal. Predictors of Institutionalization in Old Age _ Enhanced Reader.pdf.
Auer SR, Höfler M, Linsmayer E, Beránková A, Prieschl D, Ratajczak P, et al. Cross-sectional study of prevalence of Dementia, behavioural symptoms, mobility, pain and other health parameters in nursing homes in Austria and the Czech Republic: results from the DEMDATA project. BMC Geriatr. 2018;18(1):1–13.
Hoffmann F, Kaduszkiewicz H, Glaeske G, van den Bussche H, Koller D. Prevalence of Dementia in nursing home and community-dwelling older adults in Germany. Aging Clin Exp Res. 2014;26(5):555–9.
Reitinger E, Froggatt K, Brazil K, Heimerl K, Hockley J, Kunz R, et al. Palliative care in long-term care settings for older people: findings from an EAPC taskforce. Eur J Palliat Care. 2013;20(5):251–3.
López Domínguez J, Puig Llobet M, Rodríguez Ávila N, Lluch Canut MT, Ferré Grau C. Roldán Merino J. El Cuidado De las personas mayores al final de la vida en instituciones geriátricas. Revisión bibliográfica Presencia. 2014;10(20).
Froggatt KA, Moore DC, Van den Block L, Ling J, Payne SA, Arrue B, et al. Palliative Care implementation in Long-Term Care facilities: European Association for Palliative Care White Paper. J Am Med Dir Assoc. 2020;21(8):1051–7.
Puente-Fernández D, Campos-Calderón CP, Esteban-Burgos AA, Hueso-Montoro C, Roldán-López CB, Montoya-Juárez R. Palliative care symptoms, outcomes, and interventions for chronic advanced patients in Spanish nursing homes with and without Dementia. Int J Environ Res Public Health. 2020;17(5).
Mota-Romero E, Esteban-Burgos AA, Puente-Fernández D, García-Caro MP, Hueso-Montoro C, Herrero-Hahn RM, et al. Nursing Homes End of Life care program (NUHELP): developing a complex intervention. BMC Palliat Care. 2021;20(1):98.
Sociedad Española de Cuidados Paliativos (SECPAL). Guía de Cuidados Paliativos Sociedad Española de Cuidados Paliativos SECPAL. Sociedad Española de Cuidados Paliativos. 2018. Available from: www.secpal.com.
Gómez-Batiste X, Amblàs J, Costa X, Espaulella J, Lasmarías C, Ela S et al. Recomendaciones para la atención integral e intregrada de personas con enfermedades o condiciones crónicas avanzadas y pronóstico de vida limiatado en servicios de salud y sociales: NECPAL CCOMS-ICO© 3.1 (2017). 2017.
Reglamento (UE). 2016/679 del Parlamento Europeo y del Consejo de 27 de abril de 2016 relativo a la protección de las personas físicas en lo que respecta al tratamiento de datos personales y a la libre circulación de estos datos y por el que se deroga la Directiva 95/46/CE.
Gobierno de España. Ley Orgánica 3/2018, de 5 de diciembre, de Protección de Datos Personales y garantía de los derechos digitales. [Internet]. BOE-A-2018-16673. 2018 [cited 2023 Jan 15]. p. 119788–11985. Available from: https://www.boe.es/buscar/act.php?id=BOE-A-2018-16673.
Liu Y, Su L, Wang Y, Liu S, Dong B. The application of the palliative prognostic index in predicting the life expectancy of patients in palliative care: a systematic review and meta-analysis. Aging Clin Exp Res [Internet]. 2018;30(12):1417–28. https://doi.org/10.1007/s40520-018-0928-7.
Monacelli F, Tafuro M, Molfetta L, Sartini M, Nencioni A, Cea M, et al. Evaluation of prognostic indices in elderly hospitalized patients. Geriatr Gerontol Int. 2017;17(6):1015–21.
Blay C, Martori JC, Limon E, Oller R, Vila L, Gómez-Batiste X. Find your 1%: prevalence and mortality of a community cohort of people with advanced chronic disease and palliative needs. Aten Primaria [Internet]. 2019;51(2):71–9. https://doi.org/10.1016/j.aprim.2017.07.004.
de la Escuín M. R. Necesidad de atención paliativa a residentes institucionalizados con enfermedades crónicas evolutivas con pronóstico de vida limitado. Med Paliativa [Internet]. 2014;(xx). Available from: http://www.sciencedirect.com/science/article/pii/S1134248X1400086X.
Puente-Fernández D, Campos-Calderón CPCP, Esteban-Burgos AAAA, Hueso-Montoro C, Roldán-López CBCB, Montoya-Juárez R. Palliative care symptoms, outcomes, and interventions for chronic advanced patients in Spanish nursing homes with and without Dementia. Int J Environ Res Public Health. 2020;17(5):1–12.
Martinsson L, Lundström S, Sundelöf J. Better quality of end-of-life care for persons with advanced Dementia in nursing homes compared to hospitals: a Swedish national register study. BMC Palliat Care. 2020;19(1):1–9.
Liyanage T, Mitchell G, Senior H. Identifying palliative care needs in residential care. Aust J Prim Health. 2018;24(6):524–9.
Hermans K, Cohen J, Spruytte N, Van Audenhove C, Declercq A. Palliative care needs and symptoms of nursing home residents with and without Dementia: a cross-sectional study. Geriatr Gerontol Int. 2017;17(10):1501–7.
Martínez-Muñoz M. Identifying individuals with advanced chronic conditions who may benefit from an early palliative care approach predictive models. University of Vic – Central University of Catalonia ‘QUALY’; 2016.
da Costa E, Robles MJ, Sánchez-Rodríguez MD, Vázquez-Ibar O, Miralles R. Prognostic value of assessment tools on elderly patients with chronic advanced Disease and end of life, admitted to an intermediate care centre. Rev Esp Geriatr Gerontol. 2018;53(2):77–80.
Calsina-Berna A, Martinez-Muñoz M, Bardés Robles I, Beas Alba E, Madariaga Sánchez R, Alentorn XGB. Intrahospital Mortality and Survival of patients with Advanced Chronic illnesses in a Tertiary Hospital identified with the NECPAL CCOMS-ICO© Tool. J Palliat Med. 2018;21(5):665–73.
Rauh SP, Heymans MW, Van Der Maaden T, Mehr DR, Kruse RL, De Vet HCW, et al. Predicting mortality in nursing home residents with Dementia and Pneumonia treated with antibiotics: validation of a prediction model in a more recent Population. Journals Gerontol - Ser A Biol Sci Med Sci. 2019;74(12):1922–8.
Braggion M, Pellizzari M, Basso C, Girardi P, Zabeo V, Lamattina MR et al. Overall mortality and causes of death in newly admitted nursing home residents. Aging Clin Exp Res [Internet]. 2020;32(2):275–80. https://doi.org/10.1007/s40520-019-01441-x.
Acknowledgements
Results belong to one of the objectives for a Doctoral Thesis study of the Clinical Medicine and Public Health Doctoral Program of the University of Granada. We would like to thank all the participants and professionals who participated.
Funding
This study has been partially funded by Consejería de Salud, Junta de Andalucía (Fundación Pública Andaluza Progreso y Salud, Proyecto AP-0105-2016).
Author information
Authors and Affiliations
Contributions
Conceptualization, R.M.-J., C.H.-M., E.M-R. and M.G.-C.; methodology, R.M.-J., C.H.-M., E,M-R., A, E-B., and M.P.G.-C.; formal analysis, A.A.E.-B., C.H.-M., and M.P.G.-C.; data curation, E.M-R., A.A.E.-B., R.M.-J., writing—original draft preparation, A.A.E.-B., R.M.-J., C.H.-M., X.G-B., and M.P.G.-C.; writing—review and editing, A.A.E.-B., R.M.-J., C.H.-M., E.M-R., X.G-B., and M.P.G.-C. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research Ethics Committee for the Andalusian Public Health System in Granada (reference number: AP-0105-2016, date of approval: 28 June 2017). Informed consent was obtained from all subjects involved in the study. At all times these data were separated from the questionnaire answers in order to protect the participants’ anonymity, in accordance with Organic Law 3/2018, of 5 December, on Personal Data Protection and Safeguards for Digital Rights.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Esteban-Burgos, A.A., Hueso-Montoro, C., Mota-Romero, E. et al. The prognostic value of the NECPAL instrument, Palliative Prognostic Index, and PROFUND index in elderly residents of nursing homes with advanced chronic condition. BMC Geriatr 23, 715 (2023). https://doi.org/10.1186/s12877-023-04409-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04409-9