Abstract
Objectives
Relatively little is known about the lived experiences of older adults during the COVID-19 pandemic. We systematically review the international literature to understand the lived experiences of older adult’s experiences during the pandemic.
Design and methodology
This study uses a meta-ethnographical approach to investigate the included studies. The analyses were undertaken with constructivist grounded theory.
Results
Thirty-two studies met the inclusion criteria and only five papers were of low quality. Most, but not all studies, were from the global north. We identified three themes: desired and challenged wellbeing; coping and adaptation; and discrimination and intersectionality.
Overall, the studies’ findings were varied and reflected different times during the pandemic. Studies reported the impact of mass media messaging and its mostly negative impact on older adults. Many studies highlighted the impact of the COVID-19 pandemic on participants' social connectivity and well-being including missing the proximity of loved ones and in consequence experienced an increase in anxiety, feeling of depression, or loneliness. However, many studies reported how participants adapted to the change of lifestyle including new ways of communication, and social distancing. Some studies focused on discrimination and the experiences of sexual and gender minority and ethnic minority participants. Studies found that the pandemic impacted the participants’ well-being including suicidal risk behaviour, friendship loss, and increased mental health issues.
Conclusion
The COVID-19 pandemic disrupted and impacted older adults’ well-being worldwide. Despite the cultural and socio-economic differences many commonalities were found. Studies described the impact of mass media reporting, social connectivity, impact of confinement on well-being, coping, and on discrimination. The authors suggest that these findings need to be acknowledged for future pandemic strategies. Additionally, policy-making processes need to include older adults to address their needs. PROSPERO record [CRD42022331714], (Derrer-Merk et al., Older adults’ lived experiences during the COVID-19 pandemic: a systematic review, 2022).
Similar content being viewed by others
Introduction
In March 2020 the World Health Organisation declared a pandemic caused by the virus SARS-CoV2 (COVID-19) [1]. At this time 118,000 cases in 114 countries were identified and 4,291 people had already lost their lives [2]. By July 2022, there were over 5.7 million active cases and over 6.4 million deaths [2]. Despite the effort to combat and eliminate the virus globally, new variants of the virus are still a concern. At the start of the pandemic, little was known about who would be most at risk, but emerging data suggested that both people with underlying health conditions and older people had a higher risk of becoming seriously ill [3]. Thus, countries worldwide imposed health and safety measures aimed at reducing viral transmission and protecting people at higher risk of contracting the virus [4]. These measures included: national lockdowns with different lengths and frequencies; targeted shopping times for older people; hygiene procedures (wearing masks, washing hands regularly, disinfecting hands); restricting or prohibiting social gatherings; working from home, school closure, and home-schooling.
Research suggests that lockdowns and protective measures impacted on people’s lives, and had a particular impact on older people. They were at higher risk from COVID-19, with greater disease severity and higher mortality compared to younger people [5]. Older adults were identified as at higher risk as they are more likely to have pre-existing conditions including heart disease, diabetes, and severe respiratory conditions [5]. Additionally, recent research highlights that COVID-19 and its safety measures led to increased mental health problems, including increased feelings of depression, anxiety, social isolation, and loneliness, potentially cognitive decline [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Other studies reported the consequences of only age-based protective health measures including self-isolation for people older people (e.g. feeling old, losing out the time with family) [23,24,25,26,27,28,29,30].
Over the past decade, the World Health Organisation (WHO) has recognised the importance of risk communication within public health emergency preparedness and response, especially in the context of epidemics and pandemics. Risk communication is defined as “the real-time exchange of information, advice and opinions between experts or officials, and people who face a threat (hazard) to their survival, health or economic or social well-being” ([31], p5). This includes reporting the risk and health protection measurements through media and governmental bodies. Constructing awareness and building trust in society are essential components of risk communication [32]. In the context of the pandemic, the WHO noted that individual risk perception helped to prompt problem-solving activities (such as wearing face masks, social distancing, and self-isolation). However, the prolonged perception of pandemic-related uncertainty and risk could also lead to heightened feelings of distress and anxiety [31, 33], see also [34,35,36,37].
This new and unprecedented disease provided the ground for researchers worldwide to investigate the COVID-19 pandemic. To date (August 2022), approximately 8072 studies have been recorded on the U.S. National Library of Medicine ClinicalTrials.gov [38] and 12002 systematic reviews have been registered at PROSPERO, concerning COVID-19. However, to our knowledge, there is little known about qualitative research as a response to the COVID-19 pandemic and how it impacted older adults’ well-being [39]. In particular, little is known about how older people experienced the pandemic. Thus, our research question considers: How did older adults experience the COVID-19 pandemic worldwide?
We use a qualitative evidence synthesis (QES) recommended by Cochrane Qualitative and Implementation Methods Group to identify peer-reviewed articles [40]. This provides an overview of existing research, identifies potential research gaps, and develops new cumulative knowledge concerning the COVID-19 pandemic and older adults’ experiences. QES is a valuable method for its potential to contribute to research and policy [41]. Flemming and Noyes [40] argue that the evidence synthesis from qualitative research provides a richer interpretation compared to single primary research. They identified an increasing demand for qualitative evidence synthesis from a wide range of “health and social professionals, policymakers, guideline developers and educationalists” (p.1).
Methodology
A systematic literature review requires a specific approach compared to other reviews. Although there is no consensus on how it is conducted, recent systematic literature reviews have agreed the following reporting criteria are addressed [42, 43]: (a) a research question; (b) reporting database, and search strategy; (c) inclusion and exclusion criteria; (d) reporting selection methods; (e) critically appraisal tools; (f) data analysis and synthesis. We applied these criteria in our study and began by registering the research protocol with Prospero [44].
Protocol
The study is registered at Prospero [44]. This systematic literature review incorporates qualitative studies concerning older adults’ experiences during the COVID-19 pandemic.
Search strategy
The primary qualitative articles were identified via a systematic search as per the qualitative-specific SPIDER approach [45]. The SPIDER tool is designed to structure qualitative research questions, focusing less on interventions and more on study design, and ‘samples’ rather than populations, encompassing:
-
S-Sample. This includes all articles concerning older adults aged 60 + [1].
-
P-Phenomena of Interest. How did older adults experience the COVID-19 pandemic?
-
D-Design. We aim to investigate qualitative studies concerning the experiences of older adults during the COVID-19 pandemic.
-
E-Evaluation. The evaluation of studies will be evaluated with the amended Critical Appraisal Skills Programme CASP [46].
-
R-Research type Qualitative
Information source
The following databases were searched: PsychInfo, Medline, CINAHL, Web of Science, Annual Review, Annual Review of Gerontology, and Geriatrics. A hand search was conducted on Google Scholar and additional searches examined the reference lists of the included papers. The keyword search included the following terms: (older adults or elderly) AND (COVID-19 or SARS or pandemic) AND (experiences); (older adults) AND (experience) AND (covid-19) OR (coronavirus); (older adults) AND (experience) AND (covid-19 OR coronavirus) AND (Qualitative). Additional hand search terms included e.g. senior, senior citizen, or old age.
Inclusion and exclusion criteria
Articles were included when they met the following criteria: primary research using qualitative methods related to the lived experience of older adults aged 60 + (i.e. the experiences of individuals during the COVID-19 pandemic); peer-reviewed journal articles published in English; related to the COVID-19 pandemic; empirical research; published from 2020 till August 2022.
Articles were excluded when: papers discussed health professionals’ experiences; diagnostics; medical studies; interventions; day-care; home care; or carers; experiences with dementia; studies including hospitals; quantitative studies; mixed-method studies; single-case studies; people under the age of 60; grey literature; scoping reviews, and systematic reviews. We excluded clinical/care-related studies as we wanted to explore the everyday experiences of people aged 60 + . Mixed-method studies were excluded as we were interested in what was represented in solely qualitative studies. However, we acknowledge, that mixed-method studies are valuable for future systematic reviews.
Meta-ethnography
The qualitative synthesis was undertaken by using meta-ethnography. The authors have chosen meta-ethnography over other methodologies as it is an inductive and interpretive synthesis analysis and is uniquely “suited to developing new conceptual models and theories” ([47], p 2), see also [48]. Therefore, it combines well with constructivist grounded theory methodology. Meta-ethnography also examines and identifies areas of disagreements between studies [48].
This is of particular interest as the lived experiences of older adults during the COVID-19 pandemic were likely to be diverse. The method enables the researcher to synthesise the findings (e.g. themes, concepts) from primary studies, acknowledging primary data (quotes) by “using a unique translation synthesis method to transcend the findings of individual study accounts and create higher order” constructs ([47], p. 2). The following seven steps were applied:
-
1.
Getting started (identify area of interest). We were interested in the lived experiences of older adults worldwide.
-
2.
Deciding what was relevant to the initial interest (defining the focus, locating relevant studies, decision to include studies, quality appraisal). We decided on the inclusion and exclusion criteria and an appropriate quality appraisal.
-
3.
Reading the studies. We used the screening process described below (title, abstract, full text)
-
4.
Determining how the studies were related (extracting first-order constructs- participants’ quotes and second-order construct- primary author interpretation, clustering the themes from the studies into new categories (Table 3).
-
5.
Translating the studies into one another (comparing and contrasting the studies, checking commonalities or differences of each article) to organise and develop higher-order constructs by using constant comparison (Table 3). Translating is the process of finding commonalities between studies [48].
-
6.
Synthesising the translation (reciprocal and refutational synthesis, a lines of argument synthesis (interpretation of the relationship between the themes- leads to key themes and constructs of higher order; creating new meaning, Tables 2, 3),
-
7.
Expressing the synthesis (writing up the findings) [47, 48].
Screening and Study Selection
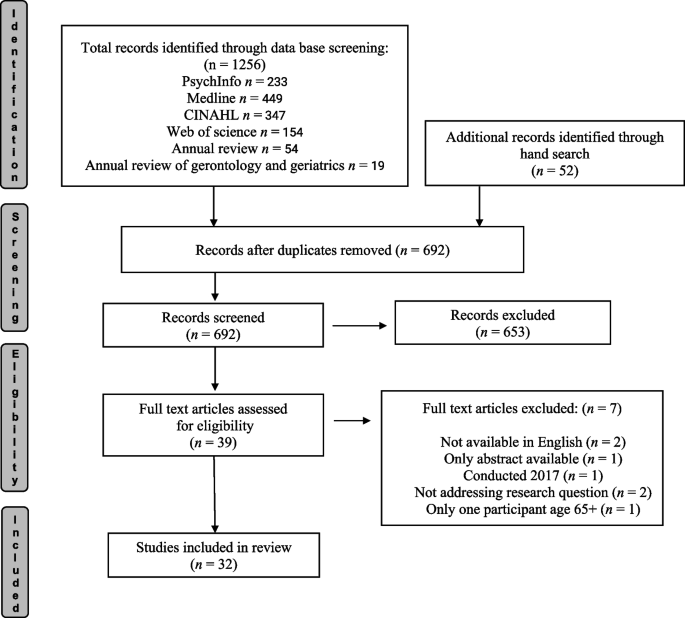
A 4-stage screening protocol was followed (Fig. 1 Prisma). First, all selected studies were screened for duplicates, which were deleted. Second, all remaining studies were screened for eligibility, and non-relevant studies were excluded at the preliminary stage. These screening steps were as follows: 1. title screening; 2. abstract screening, by the first and senior authors independently; and 3. full-text screening which was undertaken for almost all papers by the first author. However, 2 papers [9, 23] were assessed independently by LS, LR, and LMM to avoid a conflict of interest. The other co-authors also screened independently a portion of the papers each, to ensure that each paper had two independent screens to determine inclusion in the review [49]. This avoided bias and confirmed the eligibility of the included papers (Fig. 1). Endnote reference management was used to store the articles and aid the screening process.
Prisma flow diagram adapted from Page et al. [50]. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71)
Data extraction
After title and abstract screening, 39 papers were selected for reading the full article. 7 papers were excluded after the full-text assessment (1 study was conducted in 2017, but published in 2021; 2 papers were not fully available in English, 2 papers did not address the research question, 1 article was based on a conference abstract only, 1 article had only one participant age 65 +).
The full-text screening included 32 studies. All the included studies, alongside the CASP template, data extraction table, the draft of this article, and translation for synthesising the findings [47, 48] were available and accessible on google drive for all co-authors. All authors discussed the findings in regular meetings.
Quality appraisal
A critical appraisal tool assesses a study for its trustworthiness, methodological rigor, and biases and ensures “transparency in the assessment of primary research” ([51], p. 5); see also [48,49,50,51,52,53]. There is currently no gold standard for assessing primary qualitative studies, but different authors agreed that the amended CASPS checklist was appropriate to assess qualitative studies [46, 54]. Thus, we use the amended CASP appraisal tool [42]. The amended CASP appraisal tool aims to improve qualitative evidence synthesis by assessing ontology and epistemology (Table 1 CASP appraisal tool).
A numerical score was assigned to each question to indicate whether the criteria had been met (= 2), partially met (= 1), or not met (= 0) [54]; see also [55]. The score 16 – 22 are considered to be moderate and high-quality studies. The studies scored 15 and below were identified as low-quality papers. Although we focus on higher-quality papers, we did not exclude papers to avoid the exclusion of insightful and meaningful data [42, 48, 52,53,54,55,56,57]. The quality of the paper was considered in developing the evidence synthesis.
We followed the appraisal questions applied for each included study and answered the criteria either ‘Yes’, ‘Cannot tell’, or ‘No’. (Table 1 CASP appraisal criteria). The tenth question asking the value of the article was answered with ‘high’ of importance, ‘middle’, or low of importance. The new eleventh question in the CASP tool concerning ontology and epistemology was answered with yes, no, or partly (Table 1).
Data synthesis
The data synthesis followed the seven steps of Meta-Ethnography developed by Noblit & Hare [58], starting the data synthesis at step 3, described in detail by [47]. This encompasses: reading the studies; determining how the studies are related; translating the studies into one another; synthesis the translations; and expressing synthesis. This review provides a synthesis of the findings from studies related to the experiences of older adults during the COVID-19 pandemic. The qualitative analyses are based on constructivist grounded theory [59] to identify the experiences of older adults during the COVID-19 pandemic (non-clinical) populations. The analysis is inductive and iterative, uses constant comparison, and aims to develop a theory. The qualitative synthesis encompasses all text labelled as ‘results’ or ‘findings’ and uses this as raw data. The raw data includes participant’s quotes; thus, the synthesis is grounded in the participant's experience [47, 48, 60, 61]. The initial coding was undertaken for each eligible article line by line. Please see Table 2 Themes per author and country. Focused coding was applied using constant comparison, which is a widely used approach in grounded theory [61]. In particular, common and recurring as well as contradicting concepts within the studies were identified, clustered into categories, and overarching higher order constructs were developed [47, 48, 60] (Tables 2, 3, 4).
Findings
We identified twenty-seven out of thirty-two studies as moderate-high quality; they met most of the criteria (scoring 16/22 or above on the CASP; [54]. Only five papers were identified as low qualitative papers scoring 15 and below [71, 73, 74, 86, 91]. Please see the scores provided for each paper in Table 4. The low-quality papers did not provide sufficient details regarding the researcher’s relationship with the participants, sampling and recruitment, data collection, rigor in the analysis, or epistemological or ontological reasoning. For example, Yildirim [91] used verbatim notes as data without recording or transcribing them. This article described the analytical process briefly but was missing a discussion of the applied reflexivity of using verbatim notes and its limitations [92].
This systematic review found that many studies did not mention the relationship between the authors and the participant. The CASP critical appraisal tool asks: Has the relationship between the researcher and participants been adequately considered? (reflecting on own role, potential bias). Many studies reported that the recruitment was drawn from larger studies and that the qualitative study was a sub-study. Others reported that participants contacted the researcher after advertising the study. One study Goins et al., [72] reported that students recruited family members, but did not discuss how this potential bias impacted the results.
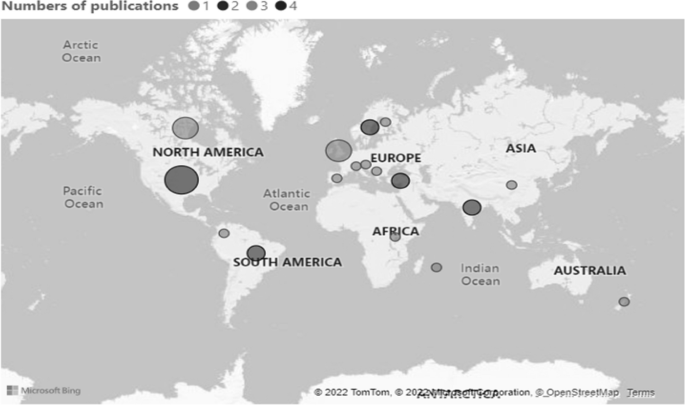
Our review brings new insights into older adults’ experiences during the pandemic worldwide. The studies were conducted on almost all continents. The majority of the articles were written in Europe followed by North America and Canada (4: USA; 3: Canada, UK; 2: Brazil, India, Netherlands, Sweden, Turkey 2; 1: Austria, China, Finland, India/Iran, Mauritius, New Zealand, Serbia, Spain, Switzerland, Uganda, UK/Ireland, UK/Colombia) (see Fig. 2). Note, as the review focuses on English language publications, we are unable to comment on qualitative research conducted in other languages see [72].
The characteristics of the included studies and the presence of analytical themes can be found in Table 4. We used the following characteristics: Author and year of publication, research aims, the country conducted, Participant’s age, number of participants, analytical methodology, CASP score, and themes.
We identified three themes: desired and challenged wellbeing; coping and adaptation; discrimination and intersectionality. We will discuss the themes in turn.
Desired and challenged wellbeing
Most of the studies reported the impact of the COVID-19 pandemic on the well-being of older adults. Factors which influenced wellbeing included: risk communication and risk perception; social connectivity; confinement (at home); and means of coping and adapting. In this context, well-being refers to the evidence reported about participants' physical and mental health, and social connectivity.
Risk perception and risk communication
Politicians and media transmitted messages about the response to the pandemic to the public worldwide. These included mortality and morbidity reports, and details of health and safety regulations like social distancing, shielding- self-isolation, or wearing masks [34,35,36,37]. As this risk communication is crucial to combat the spread of the virus, it is also important to understand how people perceived the reporting during the pandemic.
Seven studies reported on how the mass media impacted participants' well-being [23, 67, 68, 70, 72, 81, 85]. Sangrar et al. [68] investigated how older adults responded to COVID-19 messaging: “My reaction was to try to make sure that I listen to everything and [I] made sure I was aware of all the suggestions and the precautions that were being expressed by various agencies …”. (p. 4). Other studies reported the negative impact on participants' well-being of constant messaging and as a consequence stopped watching the news to maintain emotional well-being [3, 67, 68, 70, 72, 81, 85]. Derrer-Merk et al. [23] reported one participant said that “At first, watching the news every day is depressing and getting more and more depressing by the day, so I’ve had to stop watching it for my own peace of mind” (p. 13). In addition, news reporting impacted participants’ risk perception. For example, “Sometimes we are scared to hear the huge coverage of COVID-19 news, in particular the repeated message ‘older is risky’, although the message is useful.” ([81], p5).
Social connectivity
Social connectivity and support from family and community were found in fourteen of the studies as important themes [9, 62, 66,67,68, 75,76,77,78,79,80, 83, 84, 90].
The impact of COVID-19 on social networks highlighted the diverse experiences of participants. Some participants reported that the size of social contact was reduced: “We have been quite isolated during this corona time” ?([80], p. 3). Whilst other participants reported that the network was stable except that the method of contact was different: “These friends and relatives, they visited and called as often as before, but of course, we needed to use the telephone when it was not possible to meet” ([77], p. 5). Many participants in this study did not want to expand their social network see also [9, 77,78,79]. Hafford-Letchfield et al. [76] reported that established social networks and relationships were beneficial for the participants: “Covid has affected our relationship (with partner), we spend some really positive close time together and support each other a lot” (p. 7).
On the other hand, other studies reported decreases of, and gaps in, social connectedness: “I couldn’t do a lot of things that I’ve been doing for years. That was playing competitive badminton three times a week, I couldn’t do that. I couldn’t get up early and go volunteer in Seattle” [9, 67, 75]. A loss of social connection with children and grandchildren was often mentioned: “We cannot see our grandchildren up close and personal because, well because they [the parents] don’t want us, they don’t want to risk our being with the kids … it’s been an emotional loss exacerbated by the COVID thing” ([68] p.10); see also [9, 67, 78]. On the contrary, Chemen & Gopalla [66] note that those older adults who were living with other family members reported that they were more valued: “Last night my daughter-in-law thanked me for helping with my granddaughter” (p.4).
Despite reports of social disconnectedness, some studies highlighted the importance of support from family members and how support changed during the COVID-19 pandemic [9, 62, 81, 83, 90]. Yang et al. [90] argued that social support was essential during the Lockdown in China: “N6 said: ‘I asked my son-in-law to take me to the hospital” (p. 4810). Mahapatra et al. [81] found, in an Indian study, that the complex interplay of support on different levels (individual, family, and community) helped participants to adapt to the new situation. For example, this participant reported that: “The local police are very helpful. When I rang them for something and asked them to find out about it, they responded immediately” (p. 5).
Impact of confinement on well being
Most articles highlighted the impact of confinement on older adults’ well-being [9, 62, 63, 65, 67, 69, 70, 72, 75, 77,78,79, 81,82,83, 85, 89, 90].
Some studies found that participants maintained emotional well-being during the pandemic and it did not change their lifestyle [79, 80, 82, 83, 89, 92]: “Actually, I used this crisis period to clean my house. Bookcases are completely cleaned and I discarded old books. Well, we have actually been very busy with those kind of jobs. So, we were not bored at all” ([79], p. 5). In McKinlay et al. [82]’s study, nearly half of the participants found that having a sense of purpose helped to maintain their well-being: “You have to have a purpose you see. I think mental resilience is all about having a sense of purpose” (p. 6).
However, at the same time, the majority of the articles (12 out of 18) highlighted the negative impact of confinement and social distancing. Participants talked of increased depressive feelings and anxiety. For example, one of Akkus et al.’s [62] participants said: “... I am depressed; people died. Terrible disease does not give up, it always kills, I am afraid of it …” (p. 549). Similarly, one of Falvo et al.’s [67] participants remarked: “I am locked inside my house and I am afraid to go out” (p. 7).
Many of the studies reported the negative impact of loneliness as a result of confinement on participants’ well-being including [69, 70, 72, 78, 79, 90, 93]. Falvo et al. [67] reported that many participants experienced loneliness: “What sense does it make when you are not even able to see a family member? I mean, it is the saddest thing not to have the comfort of having your family next to you, to be really alone” (p. 8).
Not all studies found a negative impact on loneliness. For example, a “loner advantage” was found by Xie et al. ([82], p. 386). In this study participants found benefits in already being alone “It’s just a part of who I am, and I think that helps—if you can be alone, it really is an asset when you have to be alone” ([82], p. 386).
Bundy et al. [80] investigated loneliness from already lonely older adults and found that many participants did not attribute the loneliness to the pandemic: “It’s not been a whole lot, because I was already sitting around the house a whole lot anyway ( …). It’s basically the same, pretty well … I’d pretty well be like this anyway with COVID or without COVID” (p. 873) (see also [83]).
A study from Serbia investigated how the curfew was perceived 15 months afterward. Some participants were calm: “I realized that … well … it was simply necessary. For that reason, we accepted it as a measure that is for the common good” ([70], p.634). Others were shocked: “Above all, it was a huge surprise and sort of a shock, a complete shock because I have never, ever seen it in my life and I felt horrible, because I thought that something even worse is coming, that I even could not fathom” ([70], p. 634).
The lockdowns brought not only mental health issues to the fore but impacted the physical health of participants. Some reported they were fearful of the COVID-19 pandemic: “... For a little while I was afraid to leave, to go outside. I didn’t know if you got it from the air” ([75]. p. 6). Another study reported: “It’s been important for me to walk heartily so that I get a bit sweaty and that I breathe properly so that I fill my lungs—so that I can be prepared—and be as strong as possible, in case I should catch that coronavirus” ([77], p. 9); see also [70, 78, 82, 85].
Coping and adaptation
Many studies mentioned older adults’ processes of coping and adaptation during the pandemic [63, 64, 68, 69, 72, 75, 79, 81, 85, 87,88,89,90].
A variety of coping processes were reported including: acceptance; behavioural adaptation; emotional regulation; creating new routines; or using new technology. Kremers et al. [79] reported: “We are very realistic about the situation and we all have to go through it. Better days will come” (p. e71). Behavioural adaptation was reported: “Because I’m asthmatic, I was wearing the disposable masks, I really had trouble breathing. But I was determined to find a mask I could wear” ([68], p. 14). New routines with protective hygiene helped some participants at the beginning of the pandemic to cope with the health threat: “I am washing my hands all the time, my hands are raw from washing them all the time, I don't think I need to wash them as much as I do but I do it just in case, I don’t have anybody coming in, so there is nobody contaminating me, but I keep washing” ([69], p. 4391); see also [72]. Verhage et al. [87] reported strategies of coping including self-enhancing comparisons, distraction, and temporary acceptance: “There are so many people in worse circumstances …” (p. e294). Other studies reported how participants used a new technology: “I have recently learned to use WhatsApp, where I can make video phone calls.” ([88], p. 163); see also [89].
Discrimination -intersectionality (age and race/gender identity)
Seven studies reported ageism, racism, and gender discrimination experienced by older adults during the pandemic [23, 63, 67, 70, 76, 84, 88].
Prigent et al. [84], conducted in a New Zealand study, found that ageism was reciprocal. Younger people spoke against older adults: “why don’t you do everyone a favour and drop dead you f******g b**** it’s all because of ones like you that people are losing jobs” (p. 11). On the other hand, older adults spoke against the younger generation: “Shame to see the much younger generations often flout the rules and generally risk the gains made by the team. Sheer arrogance on their part and no sanctions applied” (p.11). Although one study reported benevolent ageism [23] most studies found hostile ageism [23, 63, 67, 70, 76, 84]. One study from Canada exploring 15 older adult’s Chinese immigrants’ experiences reported racism as people around them thought they would bring the virus into the country. The negative impact on existing friendships was told by a Chinese man aged 69 “I can tell some people are blatantly despising us. I can feel it. When I talked with my Caucasian friends verbally, they would indirectly blame us for the problem. Eventually, many of our friendships ended because of this issue” ([88], p161). In addition, this study reported ageism when participants in nursing homes felt neglected by the Canadian government.
Two papers reported experiences of sexual and gender minorities (SGM) (e.g. transgender, queer, lesbian or gay) and found additional burdens during the pandemic [63, 76]. People experienced marginalisation, stereotypes, and discrimination, as well as financial crisis: “I have faced this throughout life. Now people look at me in a way as if I am responsible for the virus.” ([63], p. 6). The consequence of marginalisation and ignorance of people with different gender identities was also noted by Hafford- Letchfield et al. [76]: “People have been moved out of their accommodation into hotels with people they don't know …. a gay man committed suicide, community members know of several that have attempted suicide. They are feeling pretty marginalised and vulnerable and you see what people are writing on the chat pages” (p.4). The intersection of ageism, racism, and heterosexism and its negative impact on people’s well-being during the pandemic reflects additional burden and stressors for older adults.
Discussion
This systematic literature review is important as it provides new insights into the lived experiences of older adults during the COVID-19 pandemic, worldwide. Our study highlights that the COVID-19 pandemic brought an increase in English-written qualitative articles to the fore. We found that 32 articles met the inclusion criteria but 5 were low quality. A lack of transparency reduces the trustworthiness of the study for the reader and the scientific community. This is particularly relevant as qualitative research is often criticised for its bias or lack of rigor [94]. However, their findings are additional evidence for our study.
Our aim was to explore, in a systematic literature review, the lived experiences of older adults during the COVID-19 pandemic worldwide. The evidence highlights the themes of desired and challenged wellbeing, coping and adaptation, and discrimination and intersectionality, on wellbeing.
Perceived risk communication was experienced by many participants as overwhelming and anxiety-provoking. This finding supports Anwar et al.’s [37] study from the beginning of the pandemic which found, in addition to circulating information, that mass media influenced the public's behaviour and in consequence the spread of disease. The impact can be positive but has also been revealed to be negative as well. They suggest evaluating the role of the mass media in relation to what and how it has been conveyed and perceived. The disrupted social connectivity found in our review supports earlier studies that reported the negative impact of people’s well-being [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28] at the beginning of the pandemic. This finding is important for future health crisis management, as the protective health measures such as confinement or self-isolation had a negative impact on many of the participants’ emotional wellbeing including increased anxiety, feelings of depression, and loneliness during the lockdowns. As a result of our review, future protective health measures should support people’s desire to maintain proximity with their loved ones and friends. However, we want to stress that our findings are mixed.
The ability of older adults to adapt and cope with the health crisis is important: many of the reported studies noted the diverse strategies used by older people to adapt to new circumstances. These included learning new technologies or changing daily routines. Politicians and the media and politicians should recognise both older adults' risk of disease and its consequences, but also their adaptability in the face of fast-changing health measures. This analysis supports studies conducted over the past decades on lifespan development, which found that people learn and adapt livelong to changing circumstances [95,96,97].
We found that discrimination against age, race, and gender identity was reported in some studies, in particular exploring participants’ experiences with immigration backgrounds and sexual and gender minorities. These studies highlighted the intersection of age and gender or race and were additional stressors for older adults and support the findings from Ramirez et al. [98] This review suggests that more research should be conducted to investigate the experiences of minority groups to develop relevant policies for future health crises.
Our review was undertaken two years after the pandemic started. At the cut-off point of our search strategy, no longitudinal studies had been found. However, in December 2022 a longitudinal study conducted in the USA explored older adult’s advice given to others [99]. They found that fostering and maintaining well-being, having a positive life perspective, and being connected to others were coping strategies during the pandemic [100]. This study supports the results of the higher order constructs of coping and adaptation in this study. Thus, more longitudinal studies are needed to enhance our understanding of the long-term consequences of the COVID-19 pandemic. The impact of the COVID-19 restrictions on older adults’ lives is evident. We suggest that future strategies and policies, which aim to protect older adults, should not only focus on the physical health threat but also acknowledge older adults' needs including psychological support, social connectedness, and instrumental support. The policies regarding older adult’s protections changed quickly but little is known about older adults’ involvement in decision making [100]. We suggest including older adults as consultants in policymaking decisions to ensure that their own self-determinism and independence are taken into consideration.
There are some limitations to this study. It did not include the lived experiences of older adults in care facilities or hospitals. The studies were undertaken during the COVID-19 pandemic and therefore data collection was not generally undertaken face-to-face. Thus, many studies included participants who had access to a phone, internet, or email, others could not be contacted. Additionally, we did not include published papers after August 2022. Even after capturing the most commonly used terms and performing additional hand searches, the search terms used might not be comprehensive. The authors found the quality of the papers to be variable, and their credibility was in question. We acknowledge that more qualitative studies might have been published in other languages than English and were not considered in this analysis.
To conclude, this systematic literature review found many similarities in the experiences of older adults during the Covid-19 pandemic despite cultural and socio-economic differences. However, we stress to acknowledge the heterogeneity of the experiences. This study highlights that the interplay of mass media reports of the COVID-19 pandemic and the policies to protect older adults had a direct impact on older adults’ well-being. The intersection of ‘isms’ (ageism, racism, and heterosexism) brought an additional burden for some older adults [98]. These results and knowledge about the drawbacks of health-protecting measures need to be included in future policies to maintain older adults’ well-being during a health crisis.
Availability of data and materials
The systematic literature review is based on already published articles. And all data analysed during this study are included in this manuscript. No additional data was used.
References
World Health Organisation (WHO): WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. Retrieved from https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
WorldOMeter: Coronavirus toll update: Cases & deaths by country. 2022. Worldometers. https://www.worldometers.info/coronavirus/.
World Health Organisation (WHO): Coronavirus disease. 2022. https://www.who.int/health-topics/coronavirus#tab=tab. Aaccessed 5 Oct 2022.
Ayouni I, Maatoug J, Dhouib W, Zammit N, Fredj SB, Ghammam R, Ghannem H. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015.
Cerasoli B. The frail future of geriatrics. Lancet Healthy Longev. 2020;1(1):e11.
Allen K-A, Arslan G, Craig H, Arefi S, Yaghoobzadeh A, Sharif Nia H. The psychometric evaluation of the sense of belonging instrument (SOBI) with Iranian older adults. BMC Geriatr. 2021;21(1):211.
Bailey L, Ward M, DiCosimo A, Baunta S, Cunningham C, Romero-Ortuno R, Kenny RA, Purcell R, Lannon R, McCarroll K, et al. Physical and mental health of older people while cocooning during the COVID-19 pandemic. QJM. 2021;114(9):648–53.
Dahlberg L. Loneliness during the COVID-19 pandemic. Aging Ment Health. 2021;25(7):1161–4.
Derrer-Merk E, Ferson S, Mannis A, Bentall R, Bennett KM. Older people's family relationships in disequilibrium during the COVID-19 pandemic. What really matters? Ageing Soc. 2022:1–18.
Derrer-Merk E, Ferson S, Mannis A, Bentall RP, Bennett KM. Belongingness challenged: Exploring the impact on older adults during the COVID-19 pandemic. PLoS ONE. 2022;17(10):e0276561.
Heidinger T, Richter L. The effect of COVID-19 on loneliness in the elderly. An empirical comparison of pre-and peri-pandemic loneliness in community-dwelling elderly. Front Psychol. 2020;11:(585308).
Richter L, Heidinger T. Hitting close to home: the effect of COVID-19 illness in the social environment on psychological burden in older adults. Front Psychol. 2021;12:(737787).
Krendl AC, Perry BL. The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e53–8.
Litwin, H., & Levinsky, M. Social networks and mental health change in older adults after the Covid-19 outbreak. Aging Ment Health. 2021:1–6. https://doi.org/10.1080/13607863.2021.1902468.
De Pue S, Gillebert C, Dierckx E, Vanderhasselt MA, De Raedt R, Van den Bussche E. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Sci Rep. 2021;11(1):4636.
Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, Patel R, Aggarwal CS, Vunnam R, Sahu N, Bhatt D, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–9.
Smith M, Steinman L, Casey E. Combatting social isolation among older adults in a time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health. 2020;8:403.
Cohn-Schwartz E, Finlay JM, Kobayashi LC. Perceptions of societal ageism and declines in subjective memory during the COVID-19 pandemic: longitudinal evidence from US adults aged ≥55 years. J Soc Issues. 2022;78(4):924–38.
Tsoukalis-Chaikalis N, Demsia S, Stamatopoulou A, Chaniotis D, Tel Nu. Systematic Mapping Study of Covid-19 Psychological Impact. 2021;15(3):820.
van Gerwen M, Alsen M, Little C, Barlow J, Genden E, Naymagon L, Tremblay D. Risk factors and outcomes of COVID-19 in New York City; a retrospective cohort study. J Med Virol. 2021;93(2):907–15.
Victor CR, Rippon I, Barreto M, Hammond C, Qualter P. Older adults’ experiences of loneliness over the lifecourse: an exploratory study using the BBC loneliness experiment. Arch Gerontol Geriatr. 2022;102:104740.
Vrach IT, Tomar R. Mental health impacts of social isolation in older people during COVID pandemic. Prog Neurol Psychiatry. 2020;24(4):25–9.
Derrer-Merk E, Reyes-Rodriguez M-F, Salazar A-M, Guevara M, Rodríguez G, Fonseca A-M, Camacho N, Ferson S, Mannis A, Bentall RP, et al. Is protecting older adults from COVID-19 Ageism? A comparative cross-cultural constructive grounded theory from the United Kingdom and Colombia. J Soc Issues. 2022;78(4):900–23.
Lytle A, Levy SR. Reducing ageism toward older adults and highlighting older adults as contributors during the COVID-19 pandemic. J Soc Issues. 2022;78(4):1066–84.
McDarby M, Ju CH, Picchiello MC, Carpenter BD. Older adults’ perceptions and experiences of ageism during the COVID-19 pandemic. J Soc Issues. 2022;78(4):939–64.
Drury L, Abrams D, Swift HJ. Intergenerational contact during and beyond COVID-19. J Soc Issues. 2022;78(4):860–82.
Kanık B, Uluğ ÖM, Solak N, Chayinska M. “Let the strongest survive”: Ageism and social Darwinism as barriers to supporting policies to benefit older individuals. J Soc Issues. 2022;00:1–25.
Spaccatini F, Giovannelli I, Pacilli MG. “You are stealing our present”: Younger people's ageism towards older people predicts attitude towards age-based COVID-19 restriction measures. J Soc Issues. 2022;78(4):769–89.
Sutter A, Vaswani M, Denice P, Choi KH, Bouchard H, Esses VM. Ageism toward older adults during the COVID-19 pandemic: Intergenerational conflict and support. J Soc Issues. 2022;78(4):815–41.
Swift H, Chasteen A. Ageism in the time of COVID-19. Group Process Intergroup Relat. 2021;24:246–52.
World Health Organisation (WHO): Risk Communication in times of an epidemic or pandemic. Asset paper series Epidemics and Pandemics: 2017. https://www.who.int/emergencies/risk-communicationsWHORCaCERaoSAo.
Bailey A, Harris MA, Bogle D, Jama A, Muir SA, Miller S, Walters CA, Govia I. Coping with COVID-19: health risk communication and vulnerable groups. Disaster Med Public Health Prep. 2021;17:e22.
Li X, Lyu H. Epidemic risk perception PS, and mental health during COVID-19 pandemic: a moderated mediating model. Front Psychol. 2021;11:563741. https://doi.org/10.3389/fpsyg.2020.563741.
Sandman P M & American Industrial Hygiene Association: Responding to community outrage: strategies for effective risk communication. American Industrial Hygiene Association. 2003.
Sandman, P M. Introduction and orientation index. https://www.psandman.com/index-intro.htm. Retrieved 13 October 2022.
Anderson M, Pitchforth E, Asaria M, Brayne C, Casadei B, Charlesworth A, Coulter A, Franklin BD, Donaldson C, Drummond M, et al. LSE-Lancet Commission on the future of the NHS: re-laying the foundations for an equitable and efficient health and care service after COVID-19. Lancet. 2021;397(10288):1915–78.
Anwar A, Malik M, Raees V, Anwar A. Role of mass media and public health communications in the COVID-19 pandemic. Cureus. 2020;12(9):e10453.
U.S. National Library of Medicine: COVID-19 - Search Details - ClinicalTrials.gov: Clinicaltrials.gov 2022. Retrieved October 13, 2022, from https://clinicaltrials.gov/ct2/results/details?cond=COVID-19.
Tremblay S, Castiglione S, Audet L-A, Desmarais M, Horace M, Peláez S. Conducting qualitative research to respond to COVID-19 challenges: reflections for the present and beyond. Int J Qual Methods. 2021;20:16094069211009680.
Flemming K, Noyes J. Qualitative evidence synthesis: where are we at? Int J Qual Methods. 2021;20:1609406921993276.
Booth A. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev. 2016;5(1):74.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203.
Phillips V, Barker E. Systematic reviews: structure, form and content. J Perioper Pract. 2021;31(9):349–53.
Derrer-Merk E, Soulsby L, Reyes Rodriguez M, Ferson S, Mannis A, Bennett KM. Older adults' lived experiences during the COVID-19 pandemic: a systematic review. 2022. PROSPERO 2022 CRD42022331714. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022331714.
Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22:1435–43.
Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci. 2020;1(1):31–42.
Sattar R, Lawton R, Panagioti M, Johnson J. Meta-ethnography in healthcare research: a guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv Res. 2021;21(1):50.
Soundy A, Heneghan NR. Meta-ethnography. Int Rev Sport Exerc Psychol. 2022;15(1):266–86.
Fallon V, Groves R, Halford JCG, Bennett KM, Harrold JA. Postpartum anxiety and infant-feeding outcomes: a systematic review. J Hum Lact. 2016;32(4):740–58.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583.
Tod D, Booth A, Smith B. Critical appraisal. Int Rev Sport Exerc Psychol. 2022;15(1):52–72.
Morse J. Why the Qualitative Health Research (QHR) review process does not use checklists. Qual Health Res. 2021;31(5):819–21.
Munthe-Kaas HM, Glenton C, Booth A, Noyes J, Lewin S. Systematic mapping of existing tools to appraise methodological strengths and limitations of qualitative research: first stage in the development of the CAMELOT tool. BMC Med Res Methodol. 2019;19(1):113.
Njau B, Covin C, Lisasi E, Damian D, Mushi D, Boulle A, Mathews C. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Public Health. 2019;19(1):1289.
Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care. Worldviews Evid Based Nurs. 2016;13(3):241–9.
Soilemezi D, Linceviciute S. Synthesizing qualitative research: reflections and lessons learnt by two new reviewers. Int J Qual Methods. 2018;17(1):1609406918768014.
Booth A. Harnessing energies, resolving tensions: acknowledging a dual heritage for qualitative evidence synthesis. Qual Health Res. 2019;29(1):18–31.
Carroll C, Booth A. Quality assessment of qualitative evidence for systematic review and synthesis: Is it meaningful, and if so, how should it be performed? Res Synth Methods. 2015;6(2):149–54.
Charmaz K. Constructing Grounded Theory. 2nd ed. London: Sage; 2014.
Toye F, Seers K, Allcock N, Briggs M, Carr E, Barker K. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 2014;14(1):80.
Noblit GW, Hare RD. Meta-ethnography: synthesizing qualitative studies. California: Sage Publications Ltd; 1988.
Akkus Y, Parlak A, Karacan Y, Karatay G. Perceptions and experiences of older people regarding the COVID-19 pandemic process: a phenomenological study. Turk Geriatri Dergisi. 2021;24:546–56.
Banerjee D, Rao TSS. “The Graying Minority”: lived experiences and psychosocial challenges of older transgender adults during the COVID-19 pandemic in India, A qualitative exploration. Front Psychiatry. 2021;11:604472.
Brooke J, Jackson D. Older people and COVID-19: Isolation, risk and ageism. J Clin Nurs. 2020;29(13-14):2044–6.
Bundy H, Lee HM, Sturkey KN, Caprio AJ. The lived experience of already-lonely older adults during COVID-19. Gerontologist. 2021;61(6):870–7.
Chemen S, Gopalla YN. Lived experiences of older adults living in the community during the COVID-19 lockdown - The case of mauritius. J Aging Stud. 2021;57:100932.
Falvo I, Zufferey MC, Albanese E, Fadda M. Lived experiences of older adults during the first COVID-19 lockdown: a qualitative study. PLoS ONE. 2021;16(6):e0252101.
Fiocco AJ, Gryspeerdt C, Franco G. Stress and adjustment during the COVID-19 pandemic: a qualitative study on the lived experience of Canadian older adults. Int J Environ Res Public Health. 2021;18(24):12922.
Fristedt S, Carlsson G, Kylén M, Jonsson O, Granbom M. Changes in daily life and wellbeing in adults, 70 years and older, in the beginning of the COVID-19 pandemic. Scand J Occup Ther. 2022;29(6):511–21.
Gazibara T, Maksimovic N, Dotlic J, Jeremic Stojkovic V, Cvjetkovic S, Milic M. Experiences and aftermath of the COVID-19 lockdown among community-dwelling older people in Serbia: a qualitative study. J Eval Clin Pract. 2022;28(4):631–40.
Giebel C, Ivan B, Ddumba I. COVID-19 public health restrictions and older adults’ well-being in Uganda: psychological impacts and coping mechanisms. Clin Gerontol. 2022;45(1):97–105.
Goins RT, Anderson E, Minick H, Daniels H. Older adults in the United States and COVID-19: a qualitative study of perceptions, finances, coping, and emotions. Front Public Health. 2021;9:660536.
Gomes MACFC, Fontenele NAO, Galindo Neto NM, Barros LM, Frota NM. Elderly people’s experience facing social isolation in the COVID-19 pandemic. Rev Rene. 2021;22:e69236. https://doi.org/10.15253/2175-6783.20212269236.
Gonçalves AR, Barcelos JLM, Duarte AP, Lucchetti G, Gonçalves DR. Silva e Dutra FCM, Gonçalves JRL: Perceptions, feelings, and the routine of older adults during the isolation period caused by the COVID-19 pandemic: a qualitative study in four countries. Aging Ment Health. 2022;26(5):911–8.
Greenwood-Hickman MA, Dahlquist J, Cooper J, Holden E, McClure JB, Mettert KD, Perry SR, Rosenberg DE. “They’re Going to Zoom It”: a qualitative investigation of impacts and coping strategies during the COVID-19 pandemic among older adults. Front Public Health. 2021;9:679976.
Hafford-Letchfield T, Toze M, Westwood S. Unheard voices: a qualitative study of LGBT+ older people experiences during the first wave of the COVID-19 pandemic in the UK. Health Soc Care Community. 2022;30(4):e1233–43.
Huntley R, Bratt AS. An interpretative phenomenological analysis of the lived experiences of older adults during the covid-19 pandemic in sweden. Nordic Psychol. 2022;75(1)3–19.
Jiménez-Etxebarria E, Bernaras Iturrioz E, Jaureguizar J. Impact of the COVID-19 pandemic as perceived by older people in Northern Spain. Psychol Res Behav Manag. 2021;14:1789–803.
Kremers EM, Janssen JHM, Nieuwboer MS, Olde Rikkert MGM, Peeters GMEE. The psychosocial adaptability of independently living older adults to COVID-19 related social isolation in the Netherlands: a qualitative study. Health Soc Care Community. 2022;30(1):e67–74.
Kulmala J, Tiilikainen E, Lisko I, Ngandu T, Kivipelto M, Solomon A. Personal social networks of community-dwelling oldest old during the Covid-19 pandemic—A qualitative study. Front Public Health. 2021;9:1–10.
Mahapatra P, Sahoo KC, Desaraju S, Pati S. Coping with COVID-19 pandemic: reflections of older couples living alone in urban Odisha India. Prim Health Care Res Dev. 2021;22:e64.
McKinlay AR, Fancourt D, Burton A. A qualitative study about the mental health and wellbeing of older adults in the UK during the COVID-19 pandemic. BMC Geriatr. 2021;21(1):1–10.
Pfabigan J, Wosko P, Pichler B, Reitinger E, Pleschberger S. Under reconstruction: the impact of COVID-19 policies on the lives and support networks of older people living alone. Int J Care Caring. 2022;6(1-2):211–28.
Prigent C, Morgan T, Wiles J, Morgan K, Williams L, Gott M. Intergenerational tension or cohesion during the covid-19 pandemic?: A letter-writing study with older new zealanders. J Intergenerational Relationsh. 2022;20(4):386–405.
Sangrar R, Porter MM, Chesser S. Exploring the interpretation of COVID-19 messaging on older adults. Experiences of vulnerability. Can J Aging Rev Can Vieil. 2021;40(4):533–42.
Sattari S, Billore S. Bring it on Covid-19: being an older person in developing countries during a pandemic. Working Older People. 2020;24(4):281–91.
Verhage M, Thielman L, Kock L, Lindenberg J. Coping of older adults in times of COVID-19: considerations of temporality among dutch older adults. J Gerontol B. 2021;76(7):e290–9.
Wang Q, Liu JKK, Walsh CA. Identities: experiences and impacts of the COVID-19 pandemic from the perspectives of older Chinese immigrants in Canada. China J Soc Work. 2021;14(2):153–71.
Xie B, Shiroma K, De Main AS, Davis NW, Fingerman K, Danesh V. Living through the COVID-19 pandemic: community-dwelling older adults’ experiences. J Aging Soc Policy. 2021;33(4–5):380–97.
Yang Q, Wang Y, Tian C, Chen Y, Mao J. The Experiences of Community-dwelling older adults during the COVID-19 lockdown in Wuhan: a qualitative study. J Adv Nurs (John Wiley & Sons, Inc). 2021;77(12):4805–14.
Yıldırım H. Psychosocial status of older adults aged 65 years and over during lockdown in Turkey and their perspectives on the outbreak. Health Soc Care Community. 2022;30(3):899–907.
Hill Z, Tawiah-Agyemang C, Kirkwood B, Kendall C. Are verbatim transcripts necessary in applied qualitative research: experiences from two community-based intervention trials in Ghana. Emerg Themes Epidemiol. 2022;19(1):5.
Giles D. Performed across Europe and written up in English: the double challenge for qualitative psychologists. Qual Res Psychol. 2019;16(3):503–7.
Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ. 2010;74(8):141.
Nikitin J, Freund A. The Adaptation Process of Aging. The Cambridge Handbook of Successful Aging. Chapter: 17. Cambridge University Press. 2019. p. 281–98.
Deimling GT, Kahana B, Bowman KF, Schaefer ML. Cancer survivorship and psychological distress in later life. Psychooncology. 2002;11(6):479–94.
Baltes PB, Staudinger UM, Lindenberger U. Lifespan psychology: theory and application to intellectual functioning. Annu Rev Psychol. 1999;50:471–507.
Ramirez L, Monahan C, Palacios-Espinosa X, Levy SR. Intersections of ageism toward older adults and other isms during the COVID-19 pandemic. J Soc Issues. 2022;78(4):965–90.
Van Vleet B, Fuller HR, Hofmann B, Huseth-Zosel A. Untapped insight: a longitudinal qualitative analysis of older adults’ advice during the COVID-19 pandemic. Innov Aging. 2022;6(7):igac071.
Gietel-Basten S, Matus K, Mori R. COVID-19 as a trigger for innovation in policy action for older persons? Evid Asia Policy Soc. 2022;41(1):168–86.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Elfriede Derrer-Merk contributed to the design, analysis, and writing the draft. Maria-Fernanda Rodriguez-Reyes contributed to the analysis, revised the draft, and approved the submission. Laura K. Soulsby contributed to the analysis, revised the draft, and approved the submission. Louise Roper contributed to the analysis, revised the draft, and approved the submission. Kate M. Bennett contributed to the design, analysis, writing the draft, and approved the submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Derrer-Merk, E., Reyes-Rodriguez, MF., Soulsby, L.K. et al. Older adults’ experiences during the COVID-19 pandemic: a qualitative systematic literature review. BMC Geriatr 23, 580 (2023). https://doi.org/10.1186/s12877-023-04282-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04282-6