Abstract
Background
Identifying people with early and late onset of chronic conditions might help target the subpopulations that are more vulnerable to negative mental, physical and functional health outcomes. The current study aimed to examine the association of early and late onset of chronic single and multiple morbidities with self-perceived physical and mental health, functional limitations and physical inactivity among older Indian adults.
Methods
Cross-sectional study was conducted using data from the Longitudinal Ageing Study in India (LASI) Wave 1 (2017–2018). The total sample size for the present study was 31,386 older adults age 60 years or older. Multivariable binary logistic regression analysis was used to establish the association between the outcomes (poor perceived physical/mental health, functional difficulty and physical inactivity) and explanatory variables (early [ = < 50 years of age] and late [> 50 years]) onset of chronic illnesses such as hypertension, diabetes, heart attack, heart disease, stroke, cancer, lung disease, arthritis, osteoporosis and psychiatric disease).
Results
Overall, 24.21% of the sample population had poor self-perceived physical health, whereas 8.67% of participants had poor self-perceived mental health. The prevalence of difficulty in ADL, difficulty in IADL, and physical inactivity was 23.77%, 48.36%, and 68.9%, respectively. Odds of poor perceived mental health were higher for the respondents with early as well as late onset of hypertension, stroke, and arthritis; while individuals with late onset of diabetes, and heart disease had higher odds of poor perceived mental health than those without chronic disease. Individuals with early onset of single morbidity were more likely to report ADL difficulty (adjusted odds ratio [AOR]: 1.33, confidence interval [CI]: 1.06–1.67); while those with late onset of single (AOR: 1.34, CI: 1.17–1.53) and multimorbidity (AOR: 1.91, CI: 1.63–2.24) were more likely to report ADL difficulty compared with individuals without morbidity. Individuals with early as well as late-onset of multimorbidity had more than two times higher odds of reporting poor physical health, poor mental health and IADL difficulty compared with individuals without chronic disease.
Conclusions
The present study revealed that early and/or late onset of chronic single and/or multiple morbidities significantly predicted poor self-perceived physical and mental health, functional limitations and physical inactivity among older Indian adults. The findings further suggest that late onset of chronic diseases such as cancer and stroke and multi-morbidity had stronger associations with physical inactivity that may help identify high risk groups for screening and support.
Similar content being viewed by others
Background
Chronic diseases represent the leading cause of mortality worldwide, and most deaths from chronic diseases occur in middle-to-low-income nations [1]. Due to changes in lifestyle and dietary habits, the prevalence of chronic conditions has become a major public health concern across the globe. In India, individuals aged 45 years and above accounted for more than half of the burden of non-communicable diseases (NCDs) [2]. Chronic conditions are associated with poor lifestyles in old age [3, 4]. Additionally, it has been shown to have negative consequences on functional, psychological, and cognitive health, mortality rates, and healthcare spending. [5,6,7,8].
Importantly, chronic diseases have been shown to be associated with the self-perceived physical health of older individuals. Existing literature suggests that having a single long-term disease or the number of diseases has a negative impact on older people’s rating of physical health [9,10,11]. The studies, however, highlight that multiple diseases can have a greater impact on the perceived health of individuals because of subjective representation and consequences of multiple illnesses, unlike single disease [12,13,14]. There is also ample evidence of the relationship between chronic diseases and mental illnesses. The number of chronic diseases modify the physiology of the brain and lead to mental illness, just as having a mental illness increases the likelihood of having comorbid diseases [15]. On the other hand, interactions between age and chronic diseases show that people who have chronic illnesses early in life are likely to have more depressive symptoms than people who get illnesses later in life. Likewise, disability increases depression symptoms when it occurs earlier in life [16]. According to one comparative study of symptoms and risk factors in the early and late onset of depression, vascular diseases were found to be associated with the late onset of depression [17].
The risk of psychological distress is higher among long-term cancer survivors. Additionally, people with comorbid illnesses and those who had trouble doing any IADLs were far more likely to have serious psychological distress (SPD). Compared to responders who had never been diagnosed with cancer, long-term cancer survivors had a significantly greater prevalence of SPD [18]. Although the majority of long-term cancer survivors successfully adjust to life after cancer and may even have positive psychological effects from dealing with their cancer [19,20,21]. Cancer diagnosis and treatment outcomes can have an impact on a person’s physical and psychological well-being. In addition to delayed physical effects that manifest many years after the end of therapy, cancer treatment can also result in immediate physical deficiencies [22,23,24]. Similarly, in comparison to people without respiratory disease, those with respiratory disease appear to have a higher prevalence of comorbid depression [25].
In a previous study, it was reported that increased chances of functional impairment were more associated with cancer, diabetes, and incontinence in males aged 70–79 years, whereas pulmonary illness and diabetes were found to be strongly associated in women [26]. Chronic multimorbidity decreases older persons’ likelihood of having better physical functioning [27]. Arthritis, diabetes, cardiovascular disease, osteoporosis, lung diseases, and high blood pressure are the most prevalent illnesses associated with functional limitation [28,29,30]. According to Klijis et al., cardiovascular and musculoskeletal diseases were associated with impairment in activities of daily living and instrumental activities of daily living among older people [29]. Similarly, among Brazilian older adults, stroke, hypertension, diabetes, and arthritis were the most prevalent chronic condition for disability [28]. Finally, older people with chronic conditions such as diabetes, high blood pressure, heart disease, stroke and cancer and other mental illnesses were more likely to report physical inactivity [31], and studies suggest that targeting people with chronic diseases will reduce the impact of physical inactivity on other health outcomes [32, 33].
Therefore, identifying people with early and late onset of chronic conditions might help target the subpopulations that are more vulnerable to negative mental, physical and functional health outcomes. Especially, early/late onset of chronic diseases and associated adverse health outcomes necessitates effective treatment approaches. Understanding the linkage between the age of onset of diseases and health outcomes is crucial to address patient concerns, develop personalized treatment strategies and support tailored to patients with early and late onset of chronic disease and multimorbidity, and implement evidence-based interventions to optimize outcomes not only in terms of disease treatment but also considering quality of life, physical, mental and functional outcomes. Thus, the current study aimed to examine the association of early and late onset of chronic single and multiple morbidities with self-perceived physical and mental health, functional limitations and physical inactivity among older Indian adults.
Methods
Data
Data from the survey of the Longitudinal Ageing Study in India (LASI) Wave 1 (2017–2018) were considered for the current analysis. The survey collected information on the health, economic, social, and demographic aspects of India’s ageing population as well as its consequences. The LASI is a nationally representative survey that included 72,250 individuals who were 45 years of age or older along with their spouses (irrespective of age) in all Indian states and union territories of India except Sikkim. The LASI employs a multistage stratified area probability cluster sampling to select the eventual units of observation. The LASI provides information on chronic health conditions, biomarkers, symptom-based health conditions, and functional and mental health. The LASI survey was carried out using a three-stage sampling design and a four-stage sampling design in rural areas and urban areas, respectively. In each state/UT, Primary Sampling Units (PSUs) were chosen in the first stage, while villages in rural areas and wards in urban areas were chosen in the selected PSUs in the second stage. Households were selected from each identified village in the third stage; however, sampling in urban areas required an additional stage, which comprised the randomly selecting one Census Enumeration Block (CEB) in each urban area. From each CEB, households were selected in the fourth stage. The main goal was to select a representative sample at each stage of sample selection.
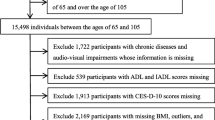
The LASI used computer-assisted personal interview (CAPI) technology for the data collection. This method required field teams to be outfitted with laptop computers pre-loaded with survey questions asked of respondents in a face-to-face interview. The report contains considerable information on the survey’s design, data collection, and methodology. The data are available at The Gateway to Global Aging Data (https://g2aging.org/ ). The present study is based on eligible respondents who are aged 60 years and above. The total sample size for the present study after dropping the missing cases (n = 78) was 31,386 older adults aged 60 years or older (Fig. 1).
Measures
Outcome variables
Poor perceived physical health
Poor self-rated health (SRH) was available on a scale of five, which represents good (very good, good, fair) and poor (poor and very poor). Further, poor SRH was coded as yes and no.
Poor perceived mental health
Poor perceived mental health was assessed using the Short Form Composite International Diagnostic Interview (CIDI-SF) with a cut-off score of 3 or more on the scale of 0–10. This scale is widely used in population-based health surveys [34]. The scale is a fully-structured diagnostic interview based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for major depressive episode and validated in field settings especially by non-clinicians in general population surveys and in cross-cultural settings [35,36,37]. Perceived mental health was coded as “good” and “poor”.
Difficulty in activities of daily living - ADL
Difficulty in activities of daily living (ADL) included having any difficulty with the following six activities: (a) walking across a room, (b) dressing, (c) bathing, (d) eating, (e) getting in and out of bed, and (f) toileting. Responses for the six items (1 = yes; 0 = no) were summed (range: 0–6) (alpha value for internal consistency was 0.87). Older individuals who struggled with any activity for more than three months were labeled “having difficulties” and otherwise “no.”
Difficulty in instrumental activities of daily living – IADL
Difficulty in instrumental activities of daily living (IADL) was assessed by asking respondents to indicate the difficulty they encounter when performing the following seven activities: grocery shopping, preparing meals, making phone calls, taking medication, doing household chores, managing finances, and getting oneself to an otherwise unfamiliar location [34] (alpha value for internal consistency was 0.88). Each item response was coded as 0 for “no difficulty” or 1 for “any difficulty.” Those who reported trouble with any of these activities for more than three months were labeled “having difficulty.” Otherwise, they were categorized as having “no difficulty.” ADL and IADL are considered as measures of functional health and a prolonged difficulty in any of the items refer to individuals’ dependence on others and/or instrumental devices [38, 39].
Physical inactivity
Physical activity included vigorous activities such as running or jogging, swimming, going to a health center or gym, cycling, or digging with a spade or shovel, heavy lifting, chopping, farm work, fast bicycling, and cycling with loads; and moderate activities such as playing outdoor games, sports, exercises, jogging and doing yoga. Those who reported none of the respective activities at least once in a week (responses were every day, more than once a week, once a week, one to three times in a month and hardly ever or never) were categorised into yes representing physical inactivity and otherwise no [40]. These measurements of physical activity were adopted from other aging surveys such as the US Health and Retirement Study (HRS) and the China Health, Aging, and Retirement Longitudinal Study (CHARLS) to enable cross-country comparisons and the list of activities was modified to the Indian context to include those that are common in the country.
Main explanatory variable
The main explanatory variable was self-reported age at onset of chronic illnesses among older adults. The variable was categorized into ‘early-onset’ and ‘late-onset’ of each chronic disease, ‘early onset of single morbidity’, ‘early onset of multimorbidity’, ‘late onset of single morbidity, and ‘late onset of multimorbidity’. The age at onset of each chronic diseases was categorized into ‘early-onset’ with a cut-off of 50 years or early ( = < 50 years of age), and ‘late-onset’ if diagnosed after the age of 50 years (> 50 years of age). In the study, respondents were asked, “Has any health professional ever diagnosed you with the following diseases?”. The diseases were: (1) Hypertension; (2) Diabetes; (3) Heart attack or myocardial infarction; (4) Chronic heart diseases; (5) Stroke; (6) Cancer; (7) Chronic lung diseases; (8) Arthritis or rheumatism; (9) Osteoporosis or other bone/joint diseases; and (10) Psychiatric disease. Respondents were also asked following questions for specific disease, “When you were first diagnosed with particular disease?” The responses, from which the age at onset of each chronic disease was estimated, were in years (in exact year when the disease was diagnosed), before a particular number of years (year at respondents’ birth plus number of years), and in respondent’s age at the time of diagnosis (current year during survey subtracted by age at diagnosis).
Other covariates
Age was coded as 60–69 years, 70–79 years, and 80 + years. Sex was coded as male and female. Education was recoded as no formal education, primary, secondary, and higher. Marital status was coded as currently in a union, and currently not a union. Living arrangements were coded as living alone, living with spouse and other living arrangements. Working status was coded as never worked, currently working, currently not working, and retired. Alcohol use, smoking tobacco, and chewing tobacco were coded as ‘no’ and ‘yes’. The BMI was computed by dividing the weight (in kilograms) by the square of the height (in meters). BMI was coded according to the criteria of the World Health Organisation’s classification; as underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obesity (≥ 30.0 kg/m2). The monthly per capita expenditure quintile or consumption quintile was categorized into five quintiles, poorest, poor, middle, rich, and richest. Religion was categorized as Hindu, Muslim, Christian, and Others. The social group (caste) was categorized as Scheduled Castes (SC), Scheduled Tribes (ST), Other Backward Classes (OBC), and others. The ‘other’ category in caste is identified as having high social status. The place of residence was coded as urban, and rural. The regions were categorized as North, Central, East, Northeast, West, and South.
Analysis
Bivariate analysis (cross-tabulation) and Chi-square test was conducted to examine the prevalence of early and late onset of chronic conditions and their associations with the selected variables. Additionally, multivariable binary logistic regression analysis [41] was used to establish the association between the outcomes (poor perceived physical/mental health, functional difficulty and physical inactivity) and explanatory variables.
The binary logistic regression model is usually put into a more compact form as follows:
The parameter \({\beta }_{0}\) estimates the log odds of outcome variables for the reference group, while \(\beta\) estimates the maximum likelihood, the differential log odds of outcome variables associated with a set of predictors X, as compared to the reference group. The survey weights were applied during the analysis to account for sample clustering and present population estimates. All the analyses were conducted using Stata version 15.1 [42].
Results
Table 1 presents the socio-demographic characteristics of the study participants. A proportion of 10.77% of the participants were in the age group of 80 years or older in this study. About 52.02% of the sample population were females. A large proportion of the sample of female, male and overall participants (69.72%, 36.29%, and 53.68% respectively) had no education. Moreover, majority of male, female and overall sample population belonged to rural areas (66.7%, 65.06%, and 65.87% respectively).
Table 2 and Table 3 present the percentage distribution of older adults by early and late onset of chronic conditions by background characteristics. A total of 4.54% of the sample population had early onset of hypertension, whereas 27.99% had late onset of hypertension. On the other hand, 2.29% of the participants had early onset of diabetes, whereas 11.91% had late onset of diabetes. The prevalence of early onset of lung disease and arthritis was 1.46% and 1.64% respectively; whereas the prevalence of late onset of lung disease and arthritis was 6.95% and 14.28% respectively. A total of 7.29% of the participants had late onset of CVD (heart attack, heart disease, and stroke).
Figure 2 depicts the prevalence of health outcomes in this study. Overall, 24.21% of the sample population had poor self-perceived physical health, whereas 8.67% of participants had poor self-perceived mental health. The prevalence of difficulty in ADL, difficulty in IADL, and physical inactivity was 23.77%, 48.36%, and 70.41% respectively. Further, Fig. 3 presents the prevalence of adverse health outcomes by early/late onset of single and multimorbidity status among older adults. Older adults with early and late onset of multimorbidity had higher prevalence of all the adverse health outcomes in this study.
Table 4 presents the multivariable logistic regression estimates of physical, mental and functional health outcomes by early and late onset of all morbidity in this study. Respondents with late onset of all chronic diseases were significantly associated with poor perceived physical health; while those with early onset of hypertension (adjusted odds ratio [AOR]: 1.60, confidence interval [CI]: 1.11–2.32), heart attack (AOR: 2.65, CI: 1.22–5.78), lung disease (AOR: 3.18, CI: 2.33–4.34), psychiatric diseases (AOR: 3.44, CI: 1.72–6.88), and arthritis (AOR: 2.58, CI: 1.92–3.46) were more likely to have poor perceived physical health than those without any chronic disease. Individuals with late onset of cancer were more likely to have poor perceived physical health (AOR: 2.62, CI: 1.58–4.36) than those without chronic disease.
The odds of poor perceived mental health were higher for the respondents with early as well as late onset of hypertension, stroke, and arthritis. Individuals with early onset of hypertension (AOR: 1.79, CI: 1.23–2.61), stroke (AOR: 3.39, CI: 1.52–7.56), and arthritis (AOR: 2.12, CI: 1.42–3.18) had 1.7, 3.3 and 2.1 times higher odds of poor perceived mental health, respectively than those without any morbidity. The result also presents that individuals with late onset of hypertension (AOR: 1.69, CI: 1.45–1.97), stroke (AOR: 2.32, CI: 1.61–3.35), arthritis (AOR: 1.34, CI: 1.11–1.62), diabetes (AOR: 1.27, CI: 1.01–1.59), heart attack (AOR: 1.66, CI: 1.09–2.52) and heart disease (AOR: 1.48, CI: 1.01–2.18) had higher odds of poor perceived mental health as compared to those without chronic disease.
Individuals with early onset of heart attack (AOR: 2.23, CI: 1.01–4.90) and arthritis (AOR: 2.38, CI: 1.71–3.31) had more than two times higher odds of reporting ADL difficulty, while those with early onset of heart disease (AOR: 3.65, CI: 1.29–10.30), stroke (AOR: 3.76, CI: 1.48–9.54), and osteoporosis (AOR: 3.92, CI: 1.65–9.32) were having more than three times higher odds of reporting ADL difficulty than those with no morbidity. Similarly, the result indicated that participants with late onset of hypertension (AOR: 1.33, CI: 1.18–1.51) and stroke (AOR: 2.22, CI: 1.72–2.87) had higher odds of suffering from ADL difficulty than the respondents without any morbidity. Individuals with late-onset of arthritis, osteoporosis, and psychiatric diseases had higher odds of ADL than those without any morbidity.
Individuals with early as well as late onset of diabetes, hypertension, arthritis, and osteoporosis were more likely to have difficulty in IADL. Participants with early onset of hypertension (AOR: 1.74, CI: 1.12–2.71), diabetes (AOR: 1.95, CI: 1.16–3.29), and arthritis (AOR: 1.98, CI: 1.43–2.74) had higher odds of IADL difficulty. Additionally, respondents with early onset of heart disease (AOR: 4.30, CI: 1.88–9.87), stroke (AOR: 3.48, CI: 1.47–8.19), and osteoporosis (AOR: 2.09, CI: 1.09–4.02) were having more than 4.3, 3.4, and 2 times higher odds of IADL difficulty, respectively, than those with no morbidity. Moreover, individuals with late onset of hypertension, diabetes, arthritis, osteoporosis, lung disease, and heart disease were more likely to have difficulty in IADL, while those with late onset of stroke (AOR: 2.97, CI: 2.20–4.01) and psychiatric disease (AOR: 2.95, CI: 2.29–3.81) had more than two times higher odds of IADL disability compared to those without any chronic condition.
Respondents with late onset of stroke (AOR: 1.58, CI: 1.09–2.30) and chronic lung disease (AOR: 1.23, CI: 1.01–1.49) were more likely to be physically inactive than the respondents without any morbidity. Further, individuals with late onset of cancer had more than two times (AOR: 2.04, CI: 1.02–4.11) higher odds of being physically inactive than those with no morbidity.
Table 5 presents the multivariable logistic regression estimates of physical, mental and functional health outcomes by early and late onset of single and multimorbidity. The odds of poor perceived physical health, poor perceived mental health, and IADL difficulty increased as chronic conditions increased from single to multimorbidity in early as well as late onset. Individuals with early onset of single morbidity were more likely to report poor perceived physical health (AOR: 1.72, CI: 1.30–2.27)), poor perceived mental health (AOR: 1.41, CI: 1.07–1.85), ADL difficulty (AOR: 1.33, CI: 1.06–1.67) and IADL disability (AOR: 1.40, CI: 1.08–1.82); while those with early onset of multimorbidity had more than two times higher odds of poor perceived physical health (AOR: 2.17, CI: 1.01–4.69), poor perceived mental health (AOR: 2.31, CI: 1.32–4.06) and IADL disability (AOR: 2.57, CI: 1.63–4.05) than individuals without chronic condition.
Similarly, participants with late onset of single morbidity had higher odds of poor perceived physical health, poor perceived mental health, ADL and IADL difficulty, whereas individuals with late onset of multimorbidity were more likely to report poor perceived physical health (AOR: 3.44, CI: 2.97–3.98), poor perceived mental health (AOR: 2.21, CI: 1.83–2.67), physical inactivity (AOR: 1.17, CI: 1.01–1.37), ADL (AOR: 1.91, CI: 1.63–2.24), and IADL difficulty (AOR: 2.08, CI: 1.81–2.40) than those without chronic disease. Individuals with early as well as late-onset of multimorbidity had more than two times higher odds of reporting poor physical health, poor mental health and difficulty in IADL compared with individuals without chronic disease.
Discussion
Given the paucity of research on interactions between age and chronic diseases with major health outcomes, the current study aimed to examine the association of early and late onset of chronic single and multiple morbidities with self-perceived physical and mental health, functional limitations and physical inactivity among older Indian adults. The study found that the odds of poor perceived physical health, poor perceived mental health, and functional difficulty increased as chronic conditions increased from single to multimorbidity in case of both early as well as late onset of chronic conditions. Also, respondents with late onset of stroke and arthritis had higher odds of all the selected adverse physical, mental and functional health outcomes.
Multimorbidity and single chronic conditions are correlated with subjective health expressed as self-perceived health [9, 10]. Our research also suggested a significant relationship between self-perceived health and the early and late onset of various chronic diseases such as hypertension, heart disease, stroke, cancer, lung disease and arthritis. A study conducted by Griffith et al. (2019) reported that multimorbidity was associated with disability and self-rated physical health [43]. This finding may partially be explained by the reduced quality of life due to the long term care needs associated with chronic conditions among individuals [44]. Given the differential impact of chronic diseases on self-perceived health across various socio-demographic groups [45,46,47], complex needs of multimorbid older patients should be prioritized in policies. Prior study has also suggested that self-perceived health, which is responsive to chronic diseases or multimorbidity, can be considered a proxy for health biomarkers and a barometer of physiologic conditions [48].
Furthermore, recent studies among older Indian also revealed that the number of chronic conditions are positively associated with functional difficulty [49, 50] and higher prevalence of depression [51]. Concordantly, the present study found that individuals with early as well as late onset of multimorbidity had higher odds of poor perceived metal health and difficulty in IADL compared to those without any chronic conditions. Another previous study focusing on the age of onset of chronic conditions found that individuals with early onset multimorbidity or both early and late multimorbidity were more likely to have physical disability, poor perceived general and mental health and physical frailty [52]. Similarly, our study revealed that individuals with early onset of single morbidity were more likely to report ADL difficulty. These findings corroborate the evidence of a scoping review on the consequences of chronic diseases associated with old age [53]. Being unable to perform simple tasks might cause elderly individuals to become isolated and lose confidence [54]. Numerous studies have demonstrated that being able to perform a variety of tasks, such as obtaining food and cooking, gives older persons a pleasant sense of independence [55].
The finding presents that the late onset of chronic conditions is associated with poor perceived mental health among older adults is in concordance with findings from previous studies. The psychological dimensions of chronic conditions are frequently ignored when medical care is considered. Patients with chronic diseases frequently need to adjust their ambitions, way of life, and professions. Many people refuse to acknowledge their situation before coping with it. However, some people have prolonged distress and may develop psychiatric illnesses, most frequently anxiety or depression [56]. Our study has further revealed that the odds of poor perceived mental health were higher for the respondents with early as well as late onset of hypertension, arthritis and stroke and late onset of diabetes, in line with previous research findings. A study has underlined that due to fluctuations in blood sugar, whether high or low, a person may experience several significant symptoms, including mood swings [57]. According to another study, after a stroke, the brain’s neuroplasticity has been found to either speed up recovery or cause unanticipated behavioural changes that result in mental diseases [58]. Depression, anxiety, exhaustion, sleep difficulties, and emotionalism are among the mental diseases that are frequently linked to stroke [59]. Moreover, our study also explored that late onset of psychiatric disease and both early and late onset of hypertension, diabetes, arthritis, heart diseases, and stroke had higher odds of IADL. In line with the present study, previous studies have demonstrated that hypertension, diabetes, arthritis, stroke, and psychiatric diseases have positive association with IADL [29, 60,61,62].
Physical activity is an established but notably under-utilized health promotion strategy. Unsurprisingly, verifying the previous findings, the present study observed that individuals with chronic diseases are at a greater risk of physical inactivity, which may contribute to some of the harmful effects of chronic conditions [63]. Evidence has highlighted that physical activity partially mediates the effect of chronic diseases on a number of health outcomes essential to the quality of life [33]. Besides, regular physical activity improves muscle strength and postural balance [64], reduces the risk of depression [65] and cognitive impairment [66], which directly help older persons maintain their mobility and also has indirect benefits, including lowering the risk of fractures and falls [67,68,69]. Similarly, physical activity can play an important role to reduce the risk of multimorbidity among those who are overweight/obese and those who have an at-risk waist circumference or at-risk waist-hip ratio [70]. Therefore, we recommend paying closer attention to physical activity as a potential health promotion strategy for older persons with chronic diseases.
Policy implications and direction for future research
The findings of this study revealed that individuals with early and late onset of chronic diseases, and multimorbidity had higher likelihoods of experiencing adverse health outcomes such as poor perceived physical and mental health, functional limitations and physical inactivity. This emphasizes the importance of public health support to young adults diagnosed with chronic diseases and multiple chronic conditions to prevent adverse health consequences as they grow older. Healthcare professionals can benefit from gaining a deeper understanding of the specific combinations of early or late onset of chronic diseases and multimorbidity that have varying levels of impact on physical, mental and functional outcomes among older adults.
Patients diagnosed with early-onset of hypertension, diabetes, lung disease, cardiovascular diseases, arthritis, and psychiatric diseases face distinct challenges throughout the disease trajectory. Healthcare professionals should emphasize on prevention, early detection of chronic disease and early interventions to reduce disease burden and improve health outcomes. By recognizing and addressing these conditions and age at the onset, clinicians can provide more comprehensive and effective care for older adults. Promoting awareness among individuals about possible adverse health outcomes of early and late onset chronic diseases and multmorbidity, encouraging them to seek medical assessment, and actively participating in screening programs are essential for improving early detection of chronic disease. Moreover, additional longitudinal research is necessary to understand the impact of early and late onset chronic diseases and multimorbidity on the health outcomes.
Limitations and strength of the study
Our study has certain limitations to be mentioned. Firstly, due to the data’s cross-sectional nature, we cannot verify the causality in the observed associations. Secondly, classifications of chronic illnesses lack independence. For example, people who have had a stroke are also more prone to developing cardiovascular diseases. Thirdly, self-report of chronic diseases may subject to reporting bias. Lastly, our analyses did not consider several other chronic diseases that could affect older person’s quality of life, such as epilepsy and migraine headaches. The large nationally representative sample of older adults is one of the study’s strengths. Also, it is the first study that has specifically examined the association of early and late onset of chronic single and multiple morbidities with major health outcomes.
Conclusions
The present study revealed that early and/or late onset of chronic single and/or multiple morbidities significantly predicted poor self-perceived physical and mental health, functional limitations and physical inactivity among older Indian adults. Findings imply that identifying people with early and late-onset chronic conditions might help target the subpopulations more vulnerable to negative mental, physical and functional health outcomes. The findings further suggest that late onset of chronic diseases such as cancer and stroke and multi-morbidity had significant associations with physical inactivity that may help identify high risk groups for screening and support. Further studies are needed to determine the types of interventions most beneficial for older adults with specific chronic conditions for improving mental, physical and functional health outcomes.
Data availability
The data are available at The Gateway to Global Aging Data (https://g2aging.org/ ).
References
Anderson E, Durstine JL. Physical activity, exercise, and chronic diseases: a brief review. Sports Med Health Sci. 2019;1:3–10.
Chatterji S, Kowal P, Mathers C, et al. The health of aging populations in China and India. Health Aff. 2008;27:1052–63.
Fortin M, Haggerty J, Almirall J, et al. Lifestyle factors and multimorbidity: a cross sectional study. BMC Public Health. 2014;14:1–8.
Mini GK, Thankappan KR. Pattern, correlates and implications of non-communicable disease multimorbidity among older adults in selected indian states: a cross-sectional study. BMJ open. 2017;7:e013529.
Fortin M, Lapointe L, Hudon C, et al. Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes. 2004;2:1–12.
Koné Pefoyo AJ, Bronskill SE, Gruneir A, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15:1–11.
Pati S, Swain S, Metsemakers J, et al. Pattern and severity of multimorbidity among patients attending primary care settings in Odisha, India. PLoS ONE. 2017;12:e0183966.
Su P, Ding H, Zhang W, et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016;16:1–7.
Caramenti M, Castiglioni I. Determinants of Self-Perceived Health: the importance of Physical Well-Being but also of Mental Health and Cognitive Functioning. Behav Sci. 2022;12:498.
Toci E, Burazeri G, Jerliu N, et al. Health literacy, self-perceived health and self-reported chronic morbidity among older people in Kosovo. Health Promot Int. 2015;30:667–74.
Bonner WIA, Weiler R, Orisatoki R, et al. Determinants of self-perceived health for Canadians aged 40 and older and policy implications. Int J Equity Health. 2017;16:1–9.
Haseen F, Adhikari R, Soonthorndhada K. Self-assessed health among thai elderly. BMC Geriatr. 2010;10:1–9.
Sun W, Watanabe M, Tanimoto Y, et al. Factors associated with good self-rated health of non-disabled elderly living alone in Japan: a cross-sectional study. BMC Public Health. 2007;7:1–9.
Machón M, Vergara I, Dorronsoro M, et al. Self-perceived health in functionally independent older people: associated factors. BMC Geriatr. 2016;16:1–9.
Snoek FJ, Bremmer MA, Hermanns N. Constructs of depression and distress in diabetes: time for an appraisal. Lancet Diabetes Endocrinol. 2015;3:450–60.
Schnittker J. Chronic illness and depressive symptoms in late life. Soc Sci Med. 2005;60:13–23.
Baldwin RC, Tomenson B. Depression in later life: a comparison of symptoms and risk factors in early and late onset cases. Br J Psychiatry. 1995;167:649–52.
Hoffman KE, McCarthy EP, Recklitis CJ, et al. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169:1274–81.
Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychol. 2006;25:47.
Bellizzi KM, Blank TO. Cancer-related identity and positive affect in survivors of prostate cancer. J Cancer Survivorship: Res Pract. 2007;1:44–8.
Park CL, Helgeson VS. Introduction to the special section: growth following highly stressful life events–current status and future directions. J Consult Clin Psychol. 2006;74:791.
Davies SM. Subsequent malignant neoplasms in survivors of childhood cancer: Childhood Cancer Survivor Study (CCSS) studies. Pediatr. Blood Cancer. 2007;48:727–30.
Ness KK, Oakes JM, Punyko JA, et al. Prevalence of the metabolic syndrome in relation to self-reported cancer history. Ann Epidemiol. 2005;15:202–6.
Pacey AA. Fertility issues in survivors from adolescent cancers. Cancer Treat Rev. 2007;33:646–55.
Goodwin RD, Scheckner B, Pena L, et al. A 10-year prospective study of respiratory disease and depression and anxiety in adulthood. Ann Allergy Asthma Immunol. 2014;113:565–70.
Kim I-H. Age and gender differences in the relation of chronic diseases to activity of daily living (ADL) disability for elderly South Koreans: based on representative data. J Prev Med Public Health. 2011;44:32–40.
Parmar MC, Saikia N. Chronic morbidity and reported disability among older persons from the India Human Development Survey. BMC Geriatr. 2018;18:1–12.
Costa Filho AM, Mambrini JV, de Malta M et al. DC, Contribution of chronic diseases to the prevalence of disability in basic and instrumental activities of daily living in elderly Brazilians: the National Health Survey (2013). Cad Saude Publica; 34.
Klijs B, Nusselder WJ, Looman CW, et al. Contribution of chronic disease to the burden of disability. PLoS ONE. 2011;6:e25325.
Yokota RT, de Heyden C, Nusselder J. Impact of chronic conditions and multimorbidity on the disability Burden in the older Population in Belgium. J Gerontol: Series A. 2016;71:903–9.
Everson-Hock ES, Green MA, Goyder EC, et al. Reducing the impact of physical inactivity: evidence to support the case for targeting people with chronic mental and physical conditions. J Public Health. 2016;38:343–51.
Ashe MC, Miller WC, Eng JJ, et al. Older adults, chronic disease and leisure-time physical activity. Gerontol. 2009;55:64–72.
Sawatzky R, Liu-Ambrose T, Miller WC, et al. Physical activity as a mediator of the impact of chronic conditions on quality of life in older adults. Health Qual Life Outcomes. 2007;5:1–11.
International Institute for Population Sciences (IIPS), MoHFW NPHCE, et al. Longitudinal ageing study in India (LASI) Wave 1. India: Mumbai; 2020.
Trainor K, Mallett J, Rushe T. Age related differences in mental health scale scores and depression diagnosis: adult responses to the CIDI-SF and MHI-5. J Affect Disord. 2013;151:639–45.
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–38.
Dang L, Dong L, Mezuk B. Shades of blue and gray: a comparison of the center for epidemiologic studies depression scale and the composite international diagnostic interview for assessment of depression syndrome in later life. Gerontol. 2020;60:e242–53.
Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc.
Muhammad T, Rashid M, Zanwar PP. Examining the association of pain and pain frequency with self-reported difficulty in activities of Daily Living (ADL) and instrumental activities of Daily Living (IADL) among community-dwelling older adults: findings from the longitudinal aging study in India. J Gerontol: Series B 2023; gbad085.
Cramm JM, Lee J. Smoking, physical activity and healthy aging in India. BMC Public Health. 2014;14:1–7.
Osborne J, King JE. Binary logistic regression. Best Practices in quantitative methods. SAGE Publications, Inc., 2011, 358–84.
StataCorp L. Stata statistical software: Release 15 (2017). College Station, TX: StataCorp LP.
Griffith LE, Gilsing A, Mangin D, et al. Multimorbidity Frameworks Impact Prevalence and Relationships with patient-important outcomes. J Am Geriatr Soc. 2019;67:1632–40.
Lima MG, Barros MB, de César A. Impact of chronic disease on quality of life among the elderly in the state of São Paulo, Brazil: a population-based study. Rev Panam Salud Publica. 2009;25:314–21.
Akhtar SN, Saikia N, Muhammad T. Self-rated health among older adults in India: Gender specific findings from National Sample Survey.
Mandal B, Pradhan KC, Mohanty P, et al. Migration status, physical limitations and associated self-rated health: a study of older indian adults. BMC Geriatr. 2023;23:1–16.
Muhammad T, Maurya P. Gender differences in the association between perceived income sufficiency and self-rated health among older adults: a population-based study in India. J Women Aging 2021; 1–14.
Marques A, Peralta M, Gouveia ÉR, et al. Physical activity buffers the negative relationship between multimorbidity, self-rated health and life satisfaction. J Public Health. 2018;40:e328–35.
Sharma P, Maurya P, Muhammad T. Number of chronic conditions and associated functional limitations among older adults: cross-sectional findings from the longitudinal aging study in India. BMC Geriatr. 2021;21:1–12.
Patel P, Muhammad T, Sahoo H. Morbidity status and changes in difficulty in activities of daily living among older adults in India: a panel data analysis. PLoS ONE. 2022;17:e0269388.
Meher T, Muhammad T, Gharge S. The association between single and multiple chronic conditions and depression among older population in India: a comparative study between men and women. Int J Geriatr. Psychiatry; 37.
Nicholson K, Griffith LE, Sohel N, et al. Examining early and late onset of multimorbidity in the canadian longitudinal study on aging. J Am Geriatr Soc. 2021;69:1579–91.
Maresova P, Javanmardi E, Barakovic S et al. Consequences of chronic diseases and.pdf. BMC Public Health.
Byeon H, Koh HW. The relationship between communication activities of daily living and quality of life among the elderly suffering from stroke. J Phys Therapy Sci. 2016;28:1450–3.
Furuta M, Komiya-Nonaka M, Akifusa S, et al. Interrelationship of oral health status, swallowing function, nutritional status, and cognitive ability with activities of daily living in japanese elderly people receiving home care services due to physical disabilities. Commun Dent Oral Epidemiol. 2013;41:173–81.
Harari H. Estructura de quarks y leptones. Investigación y Ciencia (Scientific American). 1983;JUNIO:1–5.
Muijs LT, Racca C, de Wit M, et al. Glucose variability and mood in adults with diabetes: a systematic review. Endocri Diabetes Metab. 2021;4:1–11.
Huang CCY, Ma T, Roltsch Hellard EA, et al. Stroke triggers nigrostriatal plasticity and increases alcohol consumption in rats. Sci Rep. 2017;7:1–13.
Naghavi FS, Koffman EE, Lin B, et al. Post-stroke neuronal circuits and mental illnesses. Int J Physiol Pathophysiol Pharmacol. 2019;11:1–11.
Quiñones AR, Markwardt S, Botoseneanu A. Multimorbidity combinations and disability in older adults. J Gerontol A Biol Sci Med Sci. 2016;71:823–30.
van Gool CH, Kempen GIJM, Penninx BWJH, et al. Impact of depression on disablement in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Soc Sci Med. 2005;60:25–36.
Zambon S, Siviero P, Denkinger M, et al. Role of Osteoarthritis, Comorbidity, and Pain in determining functional Limitations in older populations: European Project on Osteoarthritis. Arthritis Care Res (Hoboken). 2016;68:801–10.
US Centers for Disease Control and Prevention. Physical activity and health: A report of the Surgeon General. http://www.cdc.gov/nccdphp/sgr/pdf/execsumm.pdf.
Harridge SD, Lazarus NR. Physical activity, aging, and physiological function. Physiol. 2017;32:152–61.
Ku P-W, Fox KR, Chen L-J, et al. Physical activity and depressive symptoms in older adults: 11-year follow-up. Am J Prev Med. 2012;42:355–62.
Kumar M, Srivastava S, Muhammad T. Relationship between physical activity and cognitive functioning among older indian adults. Sci Rep. 2022;12:2725.
Campbell AJ. Preventing fractures by preventing falls in older women. CMAJ. 2002;167:1005–6.
Muhammad T, Maurya P, Sharma P. Prevalence and correlates of bone and joint diseases and its association with falls among older adults in India: evidence from LASI, 2017–18. Geriatr Nurs. 2021;42:1143–50.
Srivastava S, Muhammad T. Prevalence and risk factors of fall-related injury among older adults in India: evidence from a cross-sectional observational study. BMC Public Health. 2022;22:550.
Srivastava S, KJ VJ, Dristhi D, et al. Interaction of physical activity on the association of obesity-related measures with multimorbidity among older adults: a population-based cross-sectional study in India. BMJ open. 2021;11:e050245.
Acknowledgements
The Longitudinal Aging Study in India Project is funded by the Ministry of Health and Family Welfare, Government of India, the National Institute on Aging (R01 AG042778, R01 AG030153), and United Nations Population Fund, India.
Funding
No funding was received for the study.
Author information
Authors and Affiliations
Contributions
Conceived and designed the research paper: WA and TM; analyzed the data: TM; Wrote the manuscript: WA, KM and TM. All authors read, reviewed and approved the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study is based on secondary data from a survey which was approved by the “Indian Council of Medical Research (ICMR) Ethics Committee in January 2017 and written and oral informed consent was obtained from the participants and/or their guardians.” All methods were carried out in accordance with relevant guidelines and regulations and in accordance with the World Medical Association Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ahmed, W., Muhammad, T. & Muneera, K. Prevalence of early and late onset of chronic diseases and multimorbidity and its association with physical, mental and functional health among older Indian adults. BMC Geriatr 23, 563 (2023). https://doi.org/10.1186/s12877-023-04264-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04264-8