Abstract
Background
Machine learning-based prediction models have the potential to have a considerable positive impact on geriatric care.
Design
Systematic review and meta-analyses.
Participants
Older adults (≥ 65 years) in any setting.
Intervention
Machine learning models for predicting clinical outcomes in older adults were evaluated. A random-effects meta-analysis was conducted in two grouped cohorts, where the predictive models were compared based on their performance in predicting mortality i) under and including 6 months ii) over 6 months.
Outcome measures
Studies were grouped into two groups by the clinical outcome, and the models were compared based on the area under the receiver operating characteristic curve metric.
Results
Thirty-seven studies that satisfied the systematic review criteria were appraised, and eight studies predicting a mortality outcome were included in the meta-analyses. We could only pool studies by mortality as there were inconsistent definitions and sparse data to pool studies for other clinical outcomes. The area under the receiver operating characteristic curve from the meta-analysis yielded a summary estimate of 0.80 (95% CI: 0.76 – 0.84) for mortality within 6 months and 0.81 (95% CI: 0.76 – 0.86) for mortality over 6 months, signifying good discriminatory power.
Conclusion
The meta-analysis indicates that machine learning models display good discriminatory power in predicting mortality. However, more large-scale validation studies are necessary. As electronic healthcare databases grow larger and more comprehensive, the available computational power increases and machine learning models become more sophisticated; there should be an effort to integrate these models into a larger research setting to predict various clinical outcomes.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Older adults aged ≥ 65 years are the highest healthcare consumers, accounting for the largest and disproportionate share of hospitalisations and in-hospital deaths [1]. Moreover, this population demonstrates the highest prevalence of multimorbidity [2], emphasizing the importance of optimised clinical care and healthcare resource allocation.Traditional statistical methods for predicting clinical outcomes in this age group have limitations due to their parsimonious nature and predetermined modelling assumptions. Conversely, machine learning, which employs algorithms to analyse extensive datasets and generate predictions based on pre-set criteria, does not share these drawbacks [3].
The application of machine learning in geriatric medicine is already evidentin multiple clinical areas such as cancer diagnosis [4], predicting falls [5], mortality [6], and other therapeutic areas [7,8,9,10]. However, these applications predominantly underwent internal validation, with limited exposure in real-world clinical settings. Some recent exceptions that applied machine learning models validated in external clinical cohorts are in predicting real-time emergency department visits [11], pain perception in older adults with cognitive impairment [12] and the risk of myeloid neoplasms [13].
Despite the aforementioned progress, a comprehensive overview that synthesis these findings is lacking. To the authors' knowledge, this is the first systematic literature review and meta-analysis focused on the use of machine learning to predict clinical outcomes in the older adult demographic (≥ 65 years). While a previous review addressed machine learning in geriatric care for chronic diseases, it lacked the depth and did not include a meta-analysis [14]. Existing studies often emphasise diagnostic applications, yet literature that predicts relevant clinical outcomes those that can directly enhance geriatric care and influence prescribing policies is limited.
The potential applications of machine learning in geriatrics are vast. It could transform care by forecasting frailty [15] enabling proactive clinical interventions or adjusting treatment courses. For example, heart failure risk predictions might guide clinical decisions to mitigate adverse outcomes in this frail population. Notably, falls are a significant concern, with around a third of those aged > 65 years experiencing at least one accidental fall annually, resulting in injuries for 20% and hospitalisation for 5% [16]. Early identification of high-risk individuals could trigger preventive strategies, decreasing fall incidences. Another promising area is in predicting adverse drug reactions in older adults on polypharmacy, a situation often overlooked. Anticipating these reactions might influence modfications and optimisation in therapy, reducing potential harm.
In light of the potential applications of machine learning to improve geriatric care, this review aims to bridge the gap in the literature by offering a comprehensive examination of machine learning's role in predicting clinical outcomes for older adults, particularly those ≥ 65 years, considering their increased healthcare utilisation and the scarcity of research tailored to this cohort.
Methods
This systematic review was conducted after the study protocol was registered with PROSPERO (CRD42021295956).
Search strategy
For this systematic review and meta-analysis, studies describing the use of machine learning models in predicting clinical outcomes in older adults (≥ 65 years) were assessed for the performance of machine learning models in predicting clinical outcomes in older adults (≥ 65 years old). The literature databases included in the study were PubMed, Embase, Web of Science core collection, Web of Science BIOSIS citation index, Scopus and ProQuest, using keywords in titles, abstracts, and index terms. This systematic review and meta-analysis used all relevant literature published in English up to the 28th of February, 2023. All studies were uploaded to EndNote Version 9 for duplicate removal. After removing the duplicates, the remaining studies were uploaded to Covidence software for abstract screening, full-text review, data extraction and quality assessment. The complete search strategy can be viewed in Supplementary Information Table 1.
Inclusion and exclusion criteria
Predefined criteria were established for the inclusion and exclusion of studies. Regarding the participants, only older adults (years of age ≥ 65) were included. Studies concerning adult-only populations, animal studies, and pre-term populations were excluded. Regarding the intervention, studies which applied machine learning-based clinical prediction algorithms in older adults were included. Any synonyms for machine learning, such as “deep learning” or “statistical learning”, were included. The application of machine learning to non-clinical settings, the application of machine learning solely to images and/or signals, and studies that did not use machine learning were excluded. Regarding comparators, studies concerning machine learning vs other machine learning methods, machine learning vs traditional statistical, clinical prediction tools, and machine learning vs the unaided clinician were included. Studies utilising only traditional statistical prediction tools or unassisted clinician performance alone were excluded. Regarding the type of study, cohort studies (retrospective and prospective), cross-sectional studies and grey literature about the implementation of machine learning in clinical prediction tools in the geriatric setting were included. Narrative reviews, letters, abstracts only, corrigendum, no full-text available studies, and practice guidelines were excluded.
Study selection process
The entire study review process, except duplicate removal, was conducted in Covidence software. RO conducted title and abstract screening and the full-text review. During the full-text review, a 10% sample of studies was blindly assessed by RO, SR, and PN to generate an agreement score, Cohen’s kappa score. Agreement reached 99.29%, and Cohen’s kappa score, 0.89, signifying almost perfect agreement.
Data extraction and model performance
The data was extracted via Covidence into an Excel spreadsheet by RO and verified by SR and PN. The following items were extracted: Title, authors, in-text reference, journal, country, study design, participants/datasets used, participants/datasets sample size, primary outcome, machine learning approach, model assessment metric, statistical methods, study limitations, participant missing data, reasons for missing data. Corresponding authors of five original articles were contacted due to missing data, and one clarifying response was received. Papers for which a response was not received [17,18,19,20] were excluded from the meta-analysis. Studies which did not qualify for the meta-analysis underwent a narrative description.
The performance of a model is most commonly assessed via several performance metrics such as the Area Under the Receiver Operator Characteristic Curve (AUC-ROC), c-statistic, accuracy, F1 score, sensitivity, specificity, Positive Predictive Value (PPV), and Negative Predictive Value (NPV) [21]. It should be noted that assessing any given model using multiple metrics is generally recommended, ensuring a comprehensive analysis, as each metric has its limitations.
PROBAST quality and risk of bias assessment
The Prediction model study Risk Of Bias Assessment Tool (PROBAST) was used to assess the quality of the studies included in this systematic literature review. PROBAST assesses both the risk of bias and concerns of applicability of a study aiming to develop, validate or update a multivariable diagnostic or prediction model. It is a tool suitable for the assessment of studies that utilise machine learning to predict clinical outcomes. PROBAST utilises four steps; step 1, in which the assessor specifies their systematic review question, step 2, in which the assessor classified the type of prediction model evaluation, step 3, in which the assessor judges the risk of bias and applicability within the model and step 4 in which the assessor passes their overall judgement on the model. RO and SR carried out the PROBAST risk of bias assessment, with PN as a tie-break.
Statistical analyses
We conducted a random-effects meta-analysis using JASP software [22] based on the DerSimonian Laird model. Forest and funnel plots were also generated via JASP. In instances where the 95%CI for AUC-ROC results were absent, we estimated them. When only sensitivity and specificity were provided, we approximated an AUC-ROC value for a single point. Depending on the ROC curve type, the AUCmax can be approximated as the mean of the maximum and minimum areas.The formulas for approximations of 95%CI, single point AUC-ROC, AUCmax and the deviations from the PROSPERO protocol can be seen in Supplementary Information Appendix 1: Methods (cont).
Results
Study identification
The search identified 11,185 studies. After removing duplicates, 5,227 studies underwent title and abstract screening. From the title and abstract screen, 1,662 studies progressed to full-text review, and 3,565 were considered irrelevant. From the full-text review, 37 studies progressed to data extraction, and 1,625 were excluded. The reasons for exclusion were the wrong patient population (n = 1,340), wrong intervention (n = 119), wrong study design (n = 90), wrong outcomes (n = 39), conference abstract (n = 23), review article (n = 11), letter to the editor (n = 2), study protocol (n = 1). Figure 1 shows the study selection flowchart.
Study characteristics
The characteristics of the studies included in this review are summarised in Table 1. Most studies (n = 16) originated from the USA, with the remaining studies originating from various EU countries as well as Taiwan, Japan, China and Iceland. All studies were published between 1994–2023, with the majority of studies published in the last five years (n = 29). The data was mainly acquired from EHRs (n = 20). The majority of studies were of a retrospective design. The most common study design was retrospective cohort studies (n = 20), and the least common study design was a descriptive study, longitudinal prospective study and retrospective case–control study (n = 1 each). There was a large variation in sample sizes, ranging from 15 to 1,214,489 patients. All studies concerned exclusively patients aged ≥ 65 years.
Outcomes
The primary outcome varied across studies, with most (n = 14) predicting a mortality outcome. Other commonly reported outcomes included clinical care admission/readmission (n = 4), delirium (n = 2) and survival (n = 2). Due to a limited number of studies, a meta-analysis was only performed for the mortality outcome, split into mortality within 6 months and mortality within a period longer than 6 months.
Quality assessment
All studies included in this systematic review were evaluated for risk of bias and concerns regarding applicability using the PROBAST tool. Overall, the risk of bias in the majority of studies was considered low. The number of participants was a concern, with some studies utilising the data of fewer than 100 participants (n = 4). Models built on such a small number of participants are unsuitable for external validation. Additionally, the current guidelines for reporting machine learning studies are unclear. Many studies are not accurately reporting key information about the model development or internal validation procedures. A summary table of the results from the PROBAST assessment can be seen in Supplementary Information Table 2.
ML models
A wide variety of machine learning approaches were used across the studies. The most common machine learning approaches utilised included Random Forest (RF) (n = 12), logistic regression (n = 11), decision trees (n = 7), XGBoost (n = 5) and Artificial Neural Network (ANN) (n = 3).
ML model performance and evaluation
All studies utilised a classical approach for appraising the performance of the model. Most commonly, AUC-ROC was utilised in 28 studies. Other commonly used methods for appraising performance included sensitivity (n = 13), specificity (n = 13), accuracy (n = 8), Root Mean Square Error (RMSE) (n = 2), Mean Square Error (MSE) (n = 1), and F1 values (n = 1).
Meta-analysis
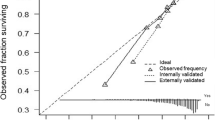
Eight studies were included in the meta-analysis, which was split into two groups. Studies were grouped by the outcome (mortality) and compared based on the AUC-ROC. The summative results can be seen in Figs. 2A, B and 3A, B. Typically AUC-ROC values between 1—0.9 are considered ‘excellent’, 0.9—0.8 ‘good’, 0.8–0.7 ‘fair’, 0.7–0.6 ‘poor’, and 0.6–0.5 ‘failed’. The highest AUC-ROC were recorded by Gomes et al., 2021, where ANN, Support Vector Machine (SVM) and RF models were applied to predict all-cause intrahospital mortality after Transcatheter Aortic Valve Implantation (TAVI). The most effective model was RF with an AUC-ROC of 0.97 [95%CI: 0.95–0.98], followed by ANN (AUC-ROC of 0.96 [95%CI: 0.94–0.97]) and SVM (AUC-ROC of 0.94 [95%CI: 0.91–0.96]) [33]. Interestingly, the summary estimates for both meta-analyses were comparable, 0.80 [95%CI 0.76–0.84] for 6 months or less and 0.81 [95% CI 0.76–0.86] for 6 months or more. The models presented by Diaz-Ramirez et al., 2021 showed the lowest AUC-ROC readings from the meta-analysis, ranging from an AUC-ROC of 0.66 for predicting mortality using the intersection method to 0.72 for predicting mortality using the full method model [27]. Several studies, such as Duarte et al., 2015 [28], Sancarlo et al., 2012 [44] and Pilotto et al., 2010 [41] showed a large variety of AUC-ROC results. The complete key for Fig. 2 can be seen in Supplementary Information Appendix 2.
Predictive model methods (mortality—within 6 months)
Pilotto et al., 2010 applied Multidimensional Prognostic Index (MPI) to predict 1-month mortality in 376 patients with a diagnosis of heart failure split into cohorts by sex. Traditional regression model scores were also calculated. However, MPI performed best, reaching an AUC-ROC of 0.80 in women and 0.83 in men [41]. In a study by Sancarlo et al., 2012 MPI was used to predict 1-month and 6-month all-cause mortality. MPI showed significantly high discriminatory power with AUC-ROC of 0.819, 0.799, respectively [44]. Duarte et al., 2015 describe the Patient-Reported Outcome Mortality Prediction Tool (PROMPT) in predicting 6-month mortality. Patients were split into derivation/validation cohorts. PROMPT achieved similar AUC-ROC readings in both cohorts, 0.75 and 0.73, respectively. The authors concluded that PROMPT demonstrates good discrimination but poor calibration in independent heterogeneous datasets [28].
Predictive model methods (mortality—over 6 months)
In the meta-analysis predicting mortality over 6 months, the top three models were from Gomes et al., 2021: RF (AUC-ROC 0.97), SVM (AUC-ROC 0.94), and ANN (AUC-ROC 0.96) to predict intrahospital mortality post-TAVI with 451 patients using 83 features. When restricted to 50 baseline features, performance dropped: AUC-ROC 0.81, 0.83, and 0.72, respectively. Traditional logistic risk scores lagged, scoring AUC-ROC 0.64 and 0.65 [33]. This suggests more input features improve AUC-ROC, but the study's limited patient sample limits its generalisability. Verdu-Rotellar et al., 2022, with a sample size of 811, applied multivariable logistic regression to predict risk in heart failure patients, attaining AUC-ROC scores of 0.73 and 0.89 in validation and derivation cohorts, respectively [50].
Parenica et al., 2012 used the EuroScore on small TAVI and TAVI + SAVR cohorts of 29 and 42 patients respectively, achieving AUC-ROC 0.885 and 0.817 [40]. Morris et al., 2020 designed a two-tiered mortality prediction system: qEMAT (on presentation) and fEMAT (post-radiologic evaluation). Both scored AUC-ROC of 0.80 and 0.85 in respective cohorts. In an external dataset, qEMAT recorded AUC-ROC 0.82 [38]. Sancarlo et al., 2012's MPI model for 12-month mortality had AUC-ROC 0.770, a slight decrease from their short-term mortality predictions [44]. Diaz-Ramirez et al., 2021 evaluated various Bayesian models, with the 'Full Method' showing the best performance at AUC-ROC 0.72. The 'Intersection method' scored the lowest, at AUC-ROC 0.66 [27].
Funnel plots for the studies included in the meta-analysis show the variability of individual studies (standard error) versus the mean effect size, as seen in Figs. 4 and 5. For both meta-analyses, there is good symmetry in the unweighted and multiplicative overdispersion plots, with an equal dispersion of studies below and above the mean. Moreover, some studies fall outside the funnel in the unweighted and multiplicative overdispersion plots, indicating publication bias. It must be noted that Egger’s test [53] is less precise in detecting bias, given the small number of studies, particularly in the meta-analyses concerning mortality within 6-months. Prediction intervals (95% PI) can be seen in Figs. 2B and 3B. 95% PI values are useful because there is uncertainty associated with a single point value, to sum up the performance of a machine learning model. A range is much more useful when anticipating how a future prediction might perform. A 95% PI of over 0.6 on the lower bound and 0.8 on the upper bound in both meta-analyses suggest that the performance of the model in a validation study is expected to be good.
Descriptive analysis of studies not included in the meta-analysis
Studies excluded from the meta-analysis also provide valuable information about the use of machine learning in predicting clinical outcomes. These studies were included in the meta-analysis because they aimed to predicts outcomes other than mortality but were too few in quantity to incorporate into a meta-analysis and directly compare the effect sizes. For a tabular representation of study characteristics, please see Table 1. Studies by Abdul-Ghaffar et al., 2020 [20], Das et al., 2003 [17], Fransvea et al., 2022 [31], Maurer et al., 2023 [37], Suzuki et al., 2020 [18], Venturini et al., 2021 [19], Ghotra et al., 2020 [54] and Han et al., 2012 [34] concerned mortality outcomes, but missing information prevented us from utilising these studies in the meta-analysis. The studies in this section have been grouped by primary outcome.
Studies predicting mortality outcomes
Abdul Ghaffar et al., 2020 combined decision trees, ensembles, logistic regression and deep nets into a single OptiML model to predict in-hospital mortality outcomes in post-TAVI patients. For 30-day cardiovascular mortality, the phenogroup data combined with the Society of Thoracic Surgeons (STS) score improved discriminatory power compared to the STS score alone (AUC-ROC 0.96 vs 0.80). In conclusion, the group showed that applying OptiML could identify patients at higher risk of various types of mortality post Tpost-TAVI [20]. Das et al., 2003 compared an ANN model with a BLEED model for the prediction of death, recurrent bleeding, and therapeutic interventions for the control of haemorrhage. The ANN model significantly outperformed the BLEED model in terms of accuracy for predicting death (97% vs 70%), recurrent bleeding (93% vs 73%) and need for interevention (93% vs 70%) during the external validation. The ANN model showed good discriminatory power and was concluded to have benefits for risk stratification in these populations [17]. Fransvea et al., 2022 predicted 30-day mortality using five machine learning models; elastic net, SVM, KNN, decision tree, multilayer perceptron. The best performance was observed using the multilayer perceptron model, attaining an accuracy of 94.9% and outperforming traditionally used approaches [31]. Han et al., 2012 developed a PROMPT model for the prediction of 6-month mortality in community-dwelling older adults. At 10%-70% cutpoints, PROMPT achieved a sensitivity of 0.80%-83.4%. The models’ discriminatory power was further supported by the fact that over half of patients with estimated 6-month mortality > 30% died within a 12-month follow-up period [34]. Maurer et al., 2023 performed an external validation of a Predictive OpTimal Trees in Emergency Surgery Risk (POTTER) model, predicting 30-day mortality. POTTER is available as a mobile telephone app and outperforms all traditional risk prediction approaches. The model achieved a c-statistic of 0.80, with its worst performance in the ≥ 80 years cohort (c-statistic = 0.71) and its best in the 65–74 years cohort (c-statistic = 0.84). The group concluded that POTTER could be useful in emergency surgery departments [37]. Suzuki et al., 2020 developed a multiple logistic regression model to predict 180-day all-cause mortality. The model showed good discriminatory power with a c-statistic of 0.820. The group remarked on the models’ potential application in deciding the direction of therapy, palliative care or hospital referrals [18]. Thongprayoon et al., 2023 utilised a clustering approach (unsupervised consensus clustering) to allocate patients and their post-transplant outcomes, such as mortality, graft failure and acute allgraft rejection. Graphical mean cluster consensus scores suggest good model performance [47]. Venturini et al., 2021 developed five tree models designed for the prediction of various clinical outcomes, including mortality, intensive care unit admission and intensive care unit discharge. The accuracy scores recorded were as follows; conditional RF (0.70), RF (0.79), ordinal forest (0.77), partitional tree (0.65), and conditional inference tree (0.79). While these results show good discriminatory power, external validation is needed before implementation into clinical care [19].
Studies predicting hospitalisation, admission, and transfer outcomes
Belmin et al., 2022 utilised a previously developed machine learning algorithm to predict emergency department admissions using questionnaire data collected during home visits, achieving a sensitivity of 83%. The system was successfully implemented, and the group concluded that it could have a use in lowering the number of emergency department visits within the study cohort [11]. Bories et al., 2022 built three machine learning models to predict hospitalisation for bleeding effects. The RF, XGBoost, and Support Vector Machine achieved predictive accuracy of 0.64, 0.68 and 0.64, respectively, in a sample of 7,462 participants [23]. Considine et al., 2019 utilised multivariable logistic regression to predict emergency interhospital transfer from subacute to acute care in a cohort of 1717 participants. The model achieved a median AUC of 0.77. The group concluded that while the results from the model are encouraging, further development and testing is necessary before implementing for external validation [26]. Friz et al., 2022 developed four machine learning models with good discriminatory power to predict 30-day readmission; adaptive boosting (AUC = 0.803), gradient boosting (AUC-ROC = 0.782), XGBoost (AUC-ROC = 0.776), RF (AUC-ROC = 0.786). All four models outperformed the traditionally used LACE index, which achieved an AUC of 0.504; however, they require external validation before introducing into a clinical setting [32]. Ren et al., 2022 developed an RF model for predicting various hospital complications within 30 days of admission and investigating feature importance from three traditionally used risk scores [43]. Sax et al., 2021 developed five machine learning models to predict serious adverse events within 30 days of emergency department admission. Logistic regression, Least Absolute Shrinkage and Selection Operator (LASSO), decision tree, RF, and XGBoost models achieved c-statistic of 0.80, 0.80, 0.65, 0.83, 0.85, respectively. The group concluded that using machine learning is an improvement on using traditional approaches [45]. Zarkowsky et al., 2021 developed a multivariable statistical model and a multilayer perceptron to predict the appropriateness of short-stay discharge and survival at 30 days. Bootstrap model validation with 1000 repetitions generated an AUC-ROC of 0.71. The study found that selecting patients for short-stay discharge is possible without risk to the patient [51].
Studies predicting cardiovascular outcomes
Chung et al., 2020 developed two ANN models to predict i) favourable/poor clinical outcome ii) modified Rankin Scale at 3 months in a sample of participants with acute ischemic stroke. Both models performed well, predicting clinical outcomes with an AUC-ROC of 0.974 and predicting modified Rankin Scale at 3 months with a low error, MSE = 0.24. In conclusion, the group showed the usefulness of these two ANN models and remarked that they could benefit clinicians, assisting with therapeutic decision-making. It should be noted that this analysis included only 31 participants [25]. Falsetti et al., 2021 developed an XGBoost model for the prediction of 3 clinical outcomes, all three models showing good discriminatory power: stroke/transient ischaemic attack (AUC-ROC = 0.931), therapeutic failure (AUC-ROC = 0.974), and major bleeding (AUC-ROC = 0.930). The models outperformed traditional risk scores, and the group concluded that the study was a big step in the instrumentation of machine learning in a larger clinical setting [29]. Velagapudi et al., 2021 developed and optimised five machine learning model classifiers to predict thrombolysis in cerebral infarction on first pass. Logistic regression, RF, SVM, Naïve Bayes and XGBoost performed to an AUC of 0.657, 0.659, 0.642, 0.599 and 0.599, respectively. The authors remark that given the improved predictive power, ease of integration with new data and generalisability, machine learning approaches are preferred to traditional approaches for studying clinical outcomes in stroke populations [48]. Zhou et al., 2021 developed six machine learning models to predict heart failure by identifying participant subgroups at high risk of death. Kernel partial least squares with the genetic algorithm (GA-KPLS), RF, LASSO, ridge regression, logistic regression and SVM achieved AUC-ROC results of 0.995, 0.646, 0.774, 0.734, 0.591, and 0.929, respectively. The results achieved with the GA-KPLS and SVM models are particularly high compared to others, which could be explained by a small participant count of just 149. The authors concluded that while the performance of the models was encouraging, external validation in another dataset/in a live clinical setting is required [52].
Studies predicting other clinical outcomes
Bowen et al., 2021 used a multilevel mixed model to predict pain perception in the last 7 days. The model included 58 continuous features and showed that poor sleep is highly associated with pain perception in the last 7 days. It should be noted that a sample size of just 15 community-dwelling older adults was used in this study, which is a significant limiting factor when considering how generalisable the results are in the larger geriatric care setting [12]. Chen et al., 2020 predicted survival in patients with early-stage uterine papillary serous carcinoma using a proportional subdistribution hazards regression predictive model. The model showed great risk stratification ability as the participants placed in the high-risk-of-death group had higher incidence of death (p < 0.001). The group concluded that the model showed promising results [24]. Ford et al., 2021 developed three models (logistic regression, naïve Bayes, RF) to detect dementia in patients where the symptoms were identified in primary care, but a formal diagnosis was not made. All three models achieved similar AUC-ROC results in the range of 0.87–0.90 with coded variables and 0.90–0.94 when keywords were added. The study showed the benefit of using machine learning for the retrospective diagnosis of dementia, assuring that records are up to date and that good quality of care is provided to patients [30]. Ko et al., 2014 aimed to develop two machine learning models, decision trees and linear discriminant analysis, to classify colonoscopy indications from EHR data. The overall accuracy for classifying colonoscopy indication was 71%, 73%, and 68% for decision trees, linear discriminant analysis model 1 and linear discriminant analysis model 2, respectively. The study concluded that while these results are promising, external validation is necessary before deploying in clinical care [35]. Li Kuan Ong et al., 2023 developed three multivariate analysis models to predict the risk of late genitourinary toxicity in older adults with prostate cancer receiving radiotherapy. Models 1, 1a and 2 achieved AUC of 0.63, 0.64, and 0.81, respectively [36]. Ocagli et al., 2021 developed an RF model to predict 4AT delirium scores. The RF model predicted 4AT scores with an RMSE of 3.29. The study showed that RF is a valid method for predicting 4AT scores and assessing the factors associated with delirium [39]. Pompei et al., 1994 aimed to develop and validate a logistic regression model for predicting the risk of delirium by classifying participants into one of three ascending risk groups. The model achieved good discriminatory power with AUC-ROC of 0.74 [42]. Rossi et al., 2021 defined a multivariable Cox analysis predictive model to stratify patients into three groups based on the risk of developing myeloid neoplasms. The model achieved c-index scores of 0.851 and 0.889 in the internal and external validation cohorts. These results, coupled with a reasonable sample size of 1,794 patients, suggest a good generalisability of the results [13]. Shardell et al., 2021 predicted sex-specific serum 25-hydroxyvitamin D thresholds that best discriminated incident slow gait using weighted decision trees [46]. Venerito et al., 2022 developed three machine learning approaches to predict a 3-month giant cell arthritis flare-up. RF outperformed logistic regression and decision trees, with accuracy scores of 71.4%, 70.4%, and 62.9%, respectively. AUC-ROC RF outperformed logistic regression and decision trees 0.76, 0.73, and 0.65, respectively. The authors concluded that their approach is highly reproducible and capable of being a benefit to a clinician caring for an older adult [49].
Discussion
Our review identified 37 studies which utilised a machine learning approach to predict a clinical outcome in adults aged ≥ 65 years. The two-grouped meta-analysis consisted of a total of eight studies using different machine learning models to predict mortality within 6 months in the first group and mortality within a period over 6 months for the second group. Supported by an AUC-ROC summary estimate of 0.80 (95% CI: 0.76 – 0.84) for mortality within 6 months and 0.81 (95% CI: 0.76 – 0.86) for mortality over 6 months, we found that machine learning models display good discriminatory power in predicting mortality. While the future of utilising machine learning in geriatric care looks favourable, caution must be applied before proclaiming it the new gold standard. This systematic literature review and meta-analysis identified some key issues facing machine learning applications in geriatric settings.
First, many studies have very low numbers of participants, some as low as under 100 participants. Machine learning models benefit greatly from large datasets numbering thousands of observations, with a low percentage of missing data. Second, many studies are utilising datasets of participants with varying levels of heterogeneity. Studies which use highly heterogeneous populations cannot be generalised to the general population of older adults. Third, most studies do not validate their findings externally. External validation studies incorporating a large number of participants are necessary before machine learning can be applied in the wider geriatric care setting. Fourth, ideally, machine learning models could be applied to any Electronic Healthcare Record (EHR)/clinical database and make live predictions as new data is introduced. However, this will prove challenging since many EHR differ fundamentally in data structures. Therefore, EHRs and clinical databases must be standardised to utilise these approaches fully. Fifth, some machine learning algorithms require much larger amounts of high-quality data to make accurate predictions than traditional statistical approaches. Sixth, most machine learning algorithms need to be optimised, and the optimal model tuning would be user dependent, which may introduce additional challenges in assessing each model’s performance and risk of bias. Finally, we found significant inconsistencies in reporting machine learning study findings. Many studies report limited information on model development and performance metrics with no insights into 95% CI. We recommend that journals specialising in this niche take special care in encouraging authors to be detailed in reporting their model development approach and encourage them to supply a full view of model performance metrics.
In 2020, a systematic literature review was carried out by Choudhury et al. 2020, in which the authors identified 35 eligible studies concerning machine learning in geriatric care for chronic diseases. Similar to the findings in this review, the group concluded that while the applications of machine learning in geriatric settings look promising, more validation studies are needed, and machine learning needs to be standardised and tailored to geriatric settings carefully [14].
Limitations and strengths
Our approach has several limitations. First, the search was limited to English, meaning relevant literature in other languages was not considered. Second, the review could have missed some studies due to unusual terminology. To mitigate this, significant time was spent identifying all synonyms of keywords and working with an experienced subject librarian when designing the search strategy. Third, due to limited literature in the field, only eight studies were included in the meta-analysis. Fourth, there is much heterogeneity between the patients from the studies included in the meta-analysis, and several patients had co-morbidities such as heart failure. Additionally, we could not calculate an I2 due to the studies failing to report the standard error. Fifth, we could only pool studies by one outcome (mortality) as there were inconsistent definitions and sparse data to pool studies for other clinical outcomes. Further to this point, further grouping of patients into cohorts with similar comorbidities is necessary but was not carried out as part of this meta-analysis, given the limited number of papers. Grouping patients into such cohorts would greatly improve the generalisability of our results. Sixth, inconsistent reporting of the model development process and inconsistent reporting of model performance meant that some studies appropriate for meta-analysis were not included. For instance, not all performance metrics can be converted to AUC-ROC, especially without specific data on the number of subjects in the derivation/validation cohorts. Finally, the predictions were performed on retrospective data, mostly from electronic health records; validating these models on prospectively collected data from other sources is critical for reproducibility. Our study’s strengths include following PRISMA guidelines, having our protocol approved and registered by PROSPERO, using Covidence software (increased rigour, accurate documentation), using a highly appropriate quality of study tool (PROBAST) and utilising multiple literature databases.
Conclusion
Given the vast amounts of clinical data collected from patients, there is considerable potential in utilising machine learning in predicting clinical outcomes in older adults. This review showed that machine learning models exhibit high discriminatory power, often outperforming traditional statistical approaches. It should also be considered that as datasets become larger and machine learning models become more sophisticated, their performance will increase further. As this field of research develops, we believe it is crucial that specific attention is dedicated to a comprehensive model performance analysis for each model. More large-scale validation studies are needed to show that machine learning can predict clinical outcomes in older adults underrepresented in our findings, such as predicting risk factors for dementia, identifying risk factors for multimorbidity, and screening subgroups of older adults vulnerable to falls and fractures.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- 95% CI:
-
95% Confidence Interval
- 95% PI:
-
95% Prediction Interval
- ACS-NSQIP:
-
ACS National Surgical Quality Improvement Program
- ADHERE:
-
Acute Decompensated Heart Failure National Registry
- AIS:
-
Acute Ischemic Stroke
- ANN:
-
Artificial Neural Network
- ANOVA:
-
Analysis of Variance
- AUC:
-
Area Under the Curve
- AUC-ROC:
-
Area Under the Receiver Operator Characteristic (ROC) Curve
- baBIC:
-
Best Average Bayesian Information Criterion
- CORI :
-
Clinical Outcomes Research Initiative
- CPRD:
-
Clinical Practice Research Datalink
- EFFECT:
-
Enhanced Feedback for Effective Cardiac Treatment
- EHR:
-
Electronic Healthcare Record
- fEMAT:
-
Full Elderly Mortality After Trauma
- GA-KPLS :
-
Kernel partial least squares with the genetic algorithm
- HRS:
-
Health and Retirement Study
- LASSO:
-
Least Absolute Shrinkage and Selection Operator
- MHOS :
-
Medicare Health Outcomes Survey
- MPI:
-
Multidimensional Prognostic Index
- mRS:
-
Modified Rankin Scale
- MSE:
-
Mean Square Error
- NPV:
-
Negative Predictive Value
- NYHA:
-
New York Heart Association
- OPTN:
-
Organ Procurement and Transplantation Network
- POTTER:
-
Predictive OpTimal Trees in Emergency Surgery Risk
- PPV:
-
Positive Predictive Value
- PROBAST:
-
Prediction model study Risk Of Bias Assessment Tool
- PROMPT:
-
Patient-Reported Outcome Mortality Prediction Tool
- qEMAT:
-
Quick Elderly Mortality After Trauma
- RF:
-
Random Forest
- RMSE:
-
Root Mean Square Error
- SAVR:
-
Surgical Aortic Valve Replacement
- SEER :
-
Surveillance, Epidemiology, and End Results
- STS:
-
Society of Thoracic Surgeons
- SVM:
-
Support Vector Machine
- TAVI:
-
Transcatheter Aortic Valve Implantation
- TIA:
-
Transient Ischaemic Attack
- UNOS:
-
United Network for Organ Sharing
References
Dixon T, Shaw M, Frankel S, Ebrahim S. Hospital admissions, age, and death: retrospective cohort study. BMJ. 2004;328(7451):1288.
Kingston A, Robinson L, Booth H, Knapp M, Jagger C, Project M. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018;47(3):374–80.
Ley C, Martin RK, Pareek A, Groll A, Seil R, Tischer T. Machine learning and conventional statistics: making sense of the differences. Knee Surg Sports Traumatol Arthrosc. 2022;30(3):753–7.
Capper D, Jones DTW, Sill M, Hovestadt V, Schrimpf D, Sturm D, et al. DNA methylation-based classification of central nervous system tumours. Nature. 2018;555(7697):469–74.
Nait Aicha A, Englebienne G, van Schooten KS, Pijnappels M, Krose B. Deep Learning to Predict Falls in Older Adults Based on Daily-Life Trunk Accelerometry. Sensors (Basel). 2018;18(5):1654.
Tedesco S, Andrulli M, Larsson MA, Kelly D, Alamaki A, Timmons S, et al. Comparison of Machine Learning Techniques for Mortality Prediction in a Prospective Cohort of Older Adults. Int J Environ Res Public Health. 2021;18(23):12806.
Hu Z, Qiu H, Wang L, Shen M. Network analytics and machine learning for predicting length of stay in elderly patients with chronic diseases at point of admission. BMC Med Inform Decis Mak. 2022;22(1):62.
Ming C, Viassolo V, Probst-Hensch N, Dinov ID, Chappuis PO, Katapodi MC. Machine learning-based lifetime breast cancer risk reclassification compared with the BOADICEA model: impact on screening recommendations. Br J Cancer. 2020;123(5):860–7.
Yokoyama S, Hamada T, Higashi M, Matsuo K, Maemura K, Kurahara H, et al. Predicted Prognosis of Patients with Pancreatic Cancer by Machine Learning. Clin Cancer Res. 2020;26(10):2411–21.
Clayton EA, Pujol TA, McDonald JF, Qiu P. Leveraging TCGA gene expression data to build predictive models for cancer drug response. BMC Bioinformatics. 2020;21(Suppl 14):364.
Belmin J, Villani P, Gay M, Fabries S, Havreng-Thery C, Malvoisin S, et al. Real-world Implementation of an eHealth System Based on Artificial Intelligence Designed to Predict and Reduce Emergency Department Visits by Older Adults: Pragmatic Trial. J Med Internet Res. 2022;24(9):e40387.
Bowen ME, Ji X, Griffioen MA. Poor Sleep Predicts Increased Pain Perception Among Adults With Mild Cognitive Impairment. Nurs Res. 2021;70(4):310–6.
Rossi M, Meggendorfer M, Zampini M, Tettamanti M, Riva E, Travaglino E, et al. Clinical relevance of clonal hematopoiesis in persons aged over 80 years. Am Soc Hematol. 2021;138:2093–105.
Choudhury A, Renjilian E, Asan O. Use of machine learning in geriatric clinical care for chronic diseases: a systematic literature review. JAMIA Open. 2020;3(3):459–71.
Aponte-Hao S, Wong ST, Thandi M, Ronksley P, McBrien K, Lee J, et al. Machine learning for identification of frailty in Canadian primary care practices. Int J Popul Data Sci. 2021;6(1):1650.
Abell JG, Lassale C, Batty GD, Zaninotto P. Risk Factors for Hospital Admission After a Fall: A Prospective Cohort Study of Community-Dwelling Older People. J Gerontol A Biol Sci Med Sci. 2021;76(4):666–74.
Das A, Ben-Menachem T, Cooper GS, Chak A, Sivak MV, Gonet JA, et al. Prediction of outcome in acute lower-gastrointestinal haemorrhage based on an artificial neural network: internal and external validation of a predictive model. Lancet. 2003;362(9392):1261–6.
Suzuki S, Motoki H, Kanzaki Y, Maruyama T, Hashizume N, Kozuka A, et al. A Predictive Model for 6-Month Mortality in Elderly Patients with Heart Failure. Int Heart J. 2020;61(2):325–31.
Venturini S, Orso D, Cugini F, Crapis M, Fossati S, Callegari A, et al. Classification and analysis of outcome predictors in non-critically ill COVID-19 patients. Intern Med J. 2021;51(4):506–14.
Abdul Ghffar Y, Osman M, Shrestha S, Shaukat F, Kagiyama N, Alkhouli M, et al. Usefulness of Semisupervised Machine-Learning-Based Phenogrouping to Improve Risk Assessment for Patients Undergoing Transcatheter Aortic Valve Implantation. Am J Cardiol. 2020;136:122–30.
Hicks SA, Strumke I, Thambawita V, Hammou M, Riegler MA, Halvorsen P, et al. On evaluation metrics for medical applications of artificial intelligence. Sci Rep. 2022;12(1):5979.
Team J. JASP (Version 0.16.3)[Computer software]. JASP Team; 2022.
Bories M, Bouzille G, Cuggia M, Le Corre P. Drug-Drug Interactions with Oral Anticoagulants as Potentially Inappropriate Medications: Prevalence and Outcomes in Elderly Patients in Primary Care and Hospital Settings. Pharmaceutics. 2022;14(7):1410.
Chen L, Liu X, Li M, Wang S, Zhou H, Liu L, et al. A novel model to predict cancer-specific survival in patients with early-stage uterine papillary serous carcinoma (UPSC). Cancer Med. 2020;9(3):988–98.
Chung CC, Chen YC, Hong CT, Chi NF, Hu CJ, Hu HH, et al. Artificial neural network-based analysis of the safetand efficacy of thrombolysis for ischemic stroke in older adults in Taiwan. Neurology Asia. 2020;25(2):109–17. https://hub.tmu.edu.tw/en/publications/artificial-neural-network-based-analysis-of-the-safetand-efficacy.
Considine J, Street M, Bucknall T, Rawson H, Hutchison AF, Dunning T, et al. Characteristics and outcomes of emergency interhospital transfers from subacute to acute care for clinical deterioration. Int J Qual Health Care. 2019;31(2):117–24.
Diaz-Ramirez LG, Lee SJ, Smith AK, Gan S, Boscardin WJ. A Novel Method for Identifying a Parsimonious and Accurate Predictive Model for Multiple Clinical Outcomes. Comput Methods Programs Biomed. 2021;204:106073.
Duarte CW, Black AW, Murray K, Haskins AE, Lucas L, Hallen S, et al. Validation of the Patient-Reported Outcome Mortality Prediction Tool (PROMPT). J Pain Symptom Manage. 2015;50(2):241-7 e6.
Falsetti L, Rucco M, Proietti M, Viticchi G, Zaccone V, Scarponi M, et al. Risk prediction of clinical adverse outcomes with machine learning in a cohort of critically ill patients with atrial fibrillation. Sci Rep. 2021;11(1):18925.
Ford E, Sheppard J, Oliver S, Rooney P, Banerjee S, Cassell JA. Automated detection of patients with dementia whose symptoms have been identified in primary care but have no formal diagnosis: a retrospective case-control study using electronic primary care records. BMJ Open. 2021;11(1):e039248.
Fransvea P, Fransvea G, Liuzzi P, Sganga G, Mannini A, Costa G. Study and validation of an explainable machine learning-based mortality prediction following emergency surgery in the elderly: A prospective observational study. Int J Surg. 2022;107:106954.
Polo Friz H, Esposito V, Marano G, Primitz L, Bovio A, Delgrossi G, et al. Machine learning and LACE index for predicting 30-day readmissions after heart failure hospitalization in elderly patients. Intern Emerg Med. 2022;17(6):1727–37.
Gomes B, Pilz M, Reich C, Leuschner F, Konstandin M, Katus HA, et al. Machine learning-based risk prediction of intrahospital clinical outcomes in patients undergoing TAVI. Clin Res Cardiol. 2021;110(3):343–56.
Han PK, Lee M, Reeve BB, Mariotto AB, Wang Z, Hays RD, et al. Development of a prognostic model for six-month mortality in older adults with declining health. J Pain Symptom Manage. 2012;43(3):527–39.
Ko CW, Dominitz JA, Neradilek M, Polissar N, Green P, Kreuter W, et al. Determination of colonoscopy indication from administrative claims data. Med Care. 2014;52(4):e21–9.
Li Kuan Ong A, Knight K, Panettieri V, Dimmock M, Kit Loong Tuan J, Qi Tan H, et al. Predictors for late genitourinary toxicity in men receiving radiotherapy for high-risk prostate cancer using planned and accumulated dose. Phys Imaging Radiat Oncol. 2023;25:100421.
Maurer LR, Chetlur P, Zhuo D, El Hechi M, Velmahos GC, Dunn J, et al. Validation of the Al-based Predictive OpTimal Trees in Emergency Surgery Risk (POTTER) Calculator in Patients 65 Years and Older. Ann Surg. 2023;277(1):e8–15.
Morris RS, Milia D, Glover J, Napolitano LM, Chen B, Lindemann E, et al. Predictors of elderly mortality after trauma: A novel outcome score. J Trauma Acute Care Surg. 2020;88(3):416–24.
Ocagli H, Bottigliengo D, Lorenzoni G, Azzolina D, Acar AS, Sorgato S, et al. A Machine Learning Approach for Investigating Delirium as a Multifactorial Syndrome. Int J Environ Res Public Health. 2021;18(13):7105.
Parenica J, Nemec P, Tomandl J, Ondrasek J, Pavkova-Goldbergova M, Tretina M, et al. Prognostic utility of biomarkers in predicting of one-year outcomes in patients with aortic stenosis treated with transcatheter or surgical aortic valve implantation. PLoS One. 2012;7(12):e48851.
Pilotto A, Addante F, Franceschi M, Leandro G, Rengo G, D’Ambrosio P, et al. Multidimensional Prognostic Index based on a comprehensive geriatric assessment predicts short-term mortality in older patients with heart failure. Circ Heart Fail. 2010;3(1):14–20.
Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK. Delirium in Hospitalized Older Persons: Outcomes and Predictors. J Am Geriatr Soc. 1994;42(8):809–15.
Ren SS, Zhu MW, Zhang KW, Chen BW, Yang C, Xiao R, et al. Machine Learning-Based Prediction of In-Hospital Complications in Elderly Patients Using GLIM-, SGA-, and ESPEN 2015-Diagnosed Malnutrition as a Factor. Nutrients. 2022;14(15):3035.
Sancarlo D, Pilotto A, Panza F, Copetti M, Longo MG, D’Ambrosio P, et al. A Multidimensional Prognostic Index (MPI) based on a comprehensive geriatric assessment predicts short- and long-term all-cause mortality in older hospitalized patients with transient ischemic attack. J Neurol. 2012;259(4):670–8.
Sax DR, Mark DG, Huang J, Sofrygin O, Rana JS, Collins SP, et al. Use of Machine Learning to Develop a Risk-Stratification Tool for Emergency Department Patients With Acute Heart Failure. Ann Emerg Med. 2021;77(2):237–48.
Shardell M, Cappola AR, Guralnik JM, Hicks GE, Kritchevsky SB, Simonsick EM, et al. Sex-specific 25-hydroxyvitamin D threshold concentrations for functional outcomes in older adults: PRoject on Optimal VItamin D in Older adults (PROVIDO). Am J Clin Nutr. 2021;114(1):16–28.
Thongprayoon C, Jadlowiec CC, Mao SA, Mao MA, Leeaphorn N, Kaewput W, et al. Distinct phenotypes of kidney transplant recipients aged 80 years or older in the USA by machine learning consensus clustering. BMJ Surg Interv Health Technol. 2023;5(1):e000137.
Velagapudi L, Mouchtouris N, Schmidt RF, Vuong D, Khanna O, Sweid A, et al. A Machine Learning Approach to First Pass Reperfusion in Mechanical Thrombectomy: Prediction and Feature Analysis. J Stroke Cerebrovasc Dis. 2021;30(7):105796.
Venerito V, Emmi G, Cantarini L, Leccese P, Fornaro M, Fabiani C, et al. Validity of Machine Learning in Predicting Giant Cell Arteritis Flare After Glucocorticoids Tapering. Front Immunol. 2022;13:860877.
Verdu-Rotellar JM, Abellana R, Vaillant-Roussel H, Gril Jevsek L, Assenova R, Kasuba Lazic D, et al. Risk stratification in heart failure decompensation in the community: HEFESTOS score. ESC Heart Fail. 2022;9(1):606–13.
Zarkowsky DS, Nejim B, Hubara I, Hicks CW, Goodney PP, Malas MB. Deep Learning and Multivariable Models Select EVAR Patients for Short-Stay Discharge. Vasc Endovascular Surg. 2021;55(1):18–25.
Zhou L, Guo Z, Wang B, Wu Y, Li Z, Yao H, et al. Risk Prediction in Patients With Heart Failure With Preserved Ejection Fraction Using Gene Expression Data and Machine Learning. Front Genet. 2021;12:652315.
Matthias Egger GDS, Martin Schneider, Christoph Minder. Bias in meta-analysis detected by a simple geographical test. British Medical Journal. 1997;315:629–34.
Ghotra AS, Monlezun DJ, Boone D, Jacob R, Poosti K, Loghin C, et al. Outcomes of Patients Undergoing Transcatheter Aortic Valve Implantation With Incidentally Discovered Masses on Computed Tomography. Am J Cardiol. 2020;132:114–8.
Acknowledgements
We thank Tamsin Riley, the subject librarian for Pharmacy and Pharmacology at the University of Bath, for assisting in designing the literature search strategy.
Funding
URSA (University Research Studentship Award) at the University of Bath.
Author information
Authors and Affiliations
Contributions
Search strategy design; RO. Abstract Screen; RO. Full-text screen; RO, SR, PN. Quality assessment and risk of bias assessment; RO and SR, with PN as tie-break. Manuscript writing; RO under the guidance of SR and PN. Final editing; RO under the guidance of SR and PN. All authors critically reviewed the content of the literature review and approved its final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Information Appendix 1. Methods (cont). Supplementary Information Appendix 2. A key for Figure. 2 detailing the characteristics of the studies included in the meta analysis. Supplementary Information Table 1. Full search strategy. Supplementary Information Table 2. PROBAST assessment. Supplementary Information Appendix 3. PRISMA checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Olender, R.T., Roy, S. & Nishtala, P.S. Application of machine learning approaches in predicting clinical outcomes in older adults – a systematic review and meta-analysis. BMC Geriatr 23, 561 (2023). https://doi.org/10.1186/s12877-023-04246-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04246-w