Abstract
Background
The association between functional capacity and the subsequent risk of nutritional deterioration is yet to be understood. The purpose of this study was to elucidate the relationship between functional capacity, comprising instrumental activities of daily living (IADL), intellectual activity, and social function, and future decline in nutritional status.
Methods
The current study is a two-year prospective cohort study. A total of 468 community-dwelling older adults without nutritional risks were enrolled. We used the Mini Nutritional Assessment Screening Form. Functional capacity, including IADL, intellectual activity, and social function, was assessed using the Tokyo Metropolitan Institute of Gerontology Index of Competence at baseline. The nutritional status was reassessed at a 2-year follow-up. Risk ratios (RR) of functional capacity for the incidence of nutritional decline were estimated.
Results
Low functional capacity was significantly associated with future deterioration of nutritional status (RR 1.12, 95% confidence interval [CI] 1.02–1.25). Of the subdomains of functional capacity, IADL decline (adjusted RR 2.21, 95% CI 1.18–4.13) was an independent risk factor for the incidence of nutritional risk. Intellectual and social activities were not significant.
Conclusion
Decline in functional capacity, especially IADL, is a risk factor for future deterioration in nutritional status. Further studies are required to elucidate the effect of interventions for IADL decline on maintaining nutritional status in older adults.
Similar content being viewed by others
Background
Good nutrition is a key factor in the aging process and a considerable contributor to healthy aging, helping to maintain favorable health and reducing the risk of chronic disease[1, 2]. Malnutrition is associated with significantly increased morbidity and impaired functional ability[3]. Consequently, individuals who are malnourished or at risk of malnutrition exhibit higher mortality rates compared to those who are well-nourished [4, 5]. Earlier studies conducted in older adults demonstrated that 5–10% of them were malnourished and 30–50% were categorized as at risk of malnutrition, even in community settings[6,7,8]. In addition, its prevalence in nursing homes or hospital settings is higher than that in community[8]. Malnutrition is a serious problem that threatens the health of many older adults.
Nutritional decline has been linked to several chronic diseases, depressive symptoms, loneliness, and functional dependency among community-dwelling older adults[9,10,11,12]. Systematic reviews examining risk factors for malnutrition in older adults have indicated that polypharmacy, cognitive decline, oral dysphagia, poor appetite, and edentulousness were also related to the deterioration of nutritional status[13, 14]. Identifying risk factors for worsening nutritional status enables healthcare professionals to provide preventive approaches to malnutrition in older populations.
Functional capacity is a crucial aspect of maintaining independent living among older adults. Lawton’s model conceptualizes functional capacity as comprising three subdomains: instrumental activities of daily living (IADL), intellectual activity, and social function[15]. Decreased IADLs, including shopping, meal preparation, and public transportation, may negatively contribute to the nutritional status of older people. Intellectual activities, including reading newspapers or books, and interest in health may also associated with maintaining the nutritional status in older adults.
However, it remains unclear whether functional capacity is associated with future nutritional risk. Furthermore, it is unclear which subdomains of functional capacity are closely associated with nutritional status. A previous review examining the association between IADL and malnutrition concluded that sufficient evidence was unavailable due to the lack of studies[14]. This understanding would facilitate the formulation of a preventive strategy aimed at reducing the nutritional risk or prevalence of malnutrition among older adults. The purpose of this study was to elucidate the association between functional capacity and a future decline in nutritional status and to determine which domains of functional capacity predict it.
Methods
Study design and participants
This study was a prospective cohort study. Baseline data were collected from 2015 to 2017. The population’s average age in the area was higher than the national average, with 31.4% of individuals being aged 65 or older. Participants were recruited for the study through community advertising, placement of posters at hospital, and verbal announcements made by medical personnel. The 2-year follow-up assessment was performed to determine the frequency of decline in the nutritional status.
The targeted population were individuals who were not at nutritional risk or malnourished according to the Mini Nutritional Assessment Screening Form (MNA-SF). The inclusion criteria consisted of: (1) age ≥ 65 years and (2) normal nutritional status. The exclusion criteria were as follows: (1) Moderate to severe cognitive impairment assessed by a Mini-Mental State Examination (MMSE) score of < 21 [16] and (2) incomplete data.
During the initial stage, a total of 844 individuals participated in the baseline assessment, out of which 724 met the inclusion criteria (120 out of 844 were at nutritional risk or were malnourished). Twelve people were excluded due to cognitive decline or missing data. Of 712 people, 244 were excluded due to the missing information regarding nutritional status at the follow-up assessment. The 468 participants were included in the analysis.
Nutritional assessment
A clinical dietitian assessed the nutritional status using the MNA-SF tool, which comprises six inquiries covering appetite, weight loss, mobility, psychological stress, neuropsychological issues, and body mass index (BMI). The scoring of MNA-SF ranges from 0 to 14, with patients falling into three categories: “normal nutritional status” (scores 12–14), “at nutritional risk” (scores 8–11), or “malnourishment” (scores 0–7)[2, 17].
Functional capacity
At the baseline assessment, the participants’ functional capacity was assessed using the Tokyo Metropolitan Institute of Gerontology Index of Competence (TMIG-IC) questionnaire[18]. This questionnaire includes three competence subdomains, namely IADL, intellectual activity, and social function. Each subdomain is scored on a scale ranging from 0 to 5 for IADL, 0 to 4 for intellectual activity, and 0 to 4 for social function. The IADL subdomain assesses the participant’s ability to utilize public transport independently, shop for essential items, prepare meals independently, pay bills, and manage banking without assistance. The intellectual activity subdomain evaluates the participant’s capability to complete pension forms, read newspapers, read books or magazines, and exhibit an interest in news stories or television programs that pertain to health-related subjects. The social function subdomain assesses the participant’s ability to visit friends at their residence, advise family or friends, ability to visit ill friends, and communicate with younger individuals. The total maximum score for the TMIG-IC questionnaire was 13 points, with higher scores indicating better functioning. The definition of impairments in each functional capacity was based on scores that were lower than the maximum possible score[19].
Other variables
The age, sex, comorbidities, and education of the participants were self-reported. The Barthel index was used to evaluate the function of basic ADLs[20]. Additionally, the Geriatric Depression Scale (GDS) [21] was employed to assess depressive symptoms. Venous blood was collected during the interviews, and serum was prepared from the blood.
Outcome measure
The main outcome was the nutritional status assessed using the MNA-SF score. Participants were re-assessed for nutritional status during the 2-year follow-up, and were classified as either maintaining a normal nutritional status (scores 12–14) or declined nutritional status, which indicates nutritional risk or malnourishment (scores < 12), to determine the temporal association between functional capacity and nutritional status. As an additional analysis, we focused on the subdomains of functional capacity, consisting of IADL, intellectual activity, and social activity. Then, we conducted an exploratory analysis to determine which sub-items in the MNA mainly deteriorated.
Statistical analysis
We assessed the differences in baseline characteristics between the maintained nutritional status group and the declined nutritional status group (MNA-SF scores < 12) during the 2-year follow-up using appropriate statistical tests based on the nature of the variables. Selection bias was assessed by comparing baseline characteristics in participants who were successfully followed up and non-followed after 2 years.
We used a modified Poisson regression model[22] to calculate the risk ratio (RR) and 95% confidence interval (CI) of functional capacity for the decline in nutritional status. First, functional capacity assessed by TMIG-IC, as a continuous variable, was included as an independent variable. The TMIG-IC score was then transformed so that higher scores indicated lower function. Second, three subdomains of functional capacity, IADL, intellectual activity, and social activity, were entered as independent variables as binomial data[19] in the different models. As adjusted variables, age and sex were selected as basic demographics (Model 2). For the adjusted variables, age and sex were selected as basic demographics (Model 2). Additionally, the MMSE score, GDS score, number of comorbidities, and medications were selected as potential confounders that could influence the association between functional capacity and nutritional status [23,24,25,26,27,28] (Model 3). Then, we assessed these associations in subitems of the MNA-SF to determine the detailed association between functional capacity and MNA-SF. The change in the MNA score during the 2-year follow-up was then entered as the dependent variable. IBM SPSS ver. 24 (IBM Japan Ltd., Tokyo, Japan) was utilized to analyze the data. The level of statistical significance was set at P < 0.05.
Results
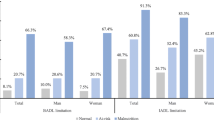
Participants’ characteristics at baseline are shown according to the maintained nutritional status group and declined nutritional status group during the 2-year follow-up (Table 1). At the 2-year follow-up, 49 (10%) of 468 declined nutritional status and 419 (90%) were maintained (Table 1). Of the participants with nutritional decline, 45 were categorized as at risk and 4 as malnutrition. The frequencies of participants with decreased scores on each question in the MNA-SF at the 2-year follow-up were as follows: Appetite: 26 (5.6%), Weight loss: 42 (9.0%), Mobility: 1 (0.2%), Psychological stress: 26 (5.6%), Neuropsychological problems or acute disease: 3 (0.6%), and BMI: 75 (16%). According to the results of the assessment of selection bias (see Appendix Table), non-follow-up participants had low cognitive function, intellectual activity, and physical functioning.
By comparing the baseline characteristics between each nutritional group during the 2-year follow-up, there were significant differences in body weight, BMI, osteoporosis, GDS, IADL, and intellectual activity (Table 1).
Modified Poisson regression showed that low functional capacity was a significant risk factor for deterioration of nutritional status during the 2-year follow-up (crude RR 1.12, 95% CI 1.02–1.25, fully adjusted RR 1.12, 95% CI 1.01-1.23) (Table 2). A secondary analysis using the subdomains of functional capacity showed that reduced IADL (crude RR 2.22, 95% CI 1.21–4.08, fully adjusted RR 2.21, 95% CI 1.18–4.13) was an independent risk factor for the development of nutritional risk. The decreased intellectual activity was not significant slightly for the future decline in nutritional status (crude RR 1.83, 95% CI 0.97–3.39, fully adjusted RR 1.79, 95% CI 0.97–3.32), and declined social activity was also not associated with it (crude RR, 1.43; 95% CI 0.75–2.74, fully adjusted RR 1.28, 95% CI, 0.638–2.55). In our Poisson regression model with binomial independent variables, the calculated statistical power for examining the association of IADL decline, intellectual activity decline, and social role decline with nutritional risk was 0.607, 0.411, and 0.147, respectively.
Of the sub-items in the MNA-SF, weight loss was the most sensitive outcome related to functional capacity (Table 3).
Discussion
This prospective cohort study investigated the temporal relationship between functional capacity and future deterioration of nutritional status. A decline in functional capacity was related to the development of nutritional risks. Among the subdomains of functional capacity, the decline in IADL was a significant risk factor for the deterioration of nutritional status. Of the sub-items in the MNA-SF, weight loss appeared to be the most sensitive factor.
Functional capacity, especially IADL, was associated with future deterioration in nutritional status. Although cross-sectional relationships have been reported, it was unclear whether the decline in IADL preceded the deterioration in nutritional status. IADL includes shopping for daily necessities and meal preparation, paying bills, and using public transport. Some earlier studies have cross-sectionally shown the relationship between limited IADL and nutritional risk[11, 29,30,31], and contributions of IADL to good nutritional status have been mentioned. The ability to shop is an important aid in maintaining good nutrition, and difficulty with transportation is a significant barrier [29, 30, 32]. Difficulty in meal preparation can be a key factor in malnutrition, especially in healthy older adults[31, 32]. In the present study, weight loss seemed to be the sensitive subitem of the MNA-SF. Considering these results, one could hypothesize that a decrease in functional capacity, including IADL, contributes to weight loss, thereby leading to a decline in nutritional status. However, the significant association we observed between functional capacity and weight loss became somewhat less significant in the fully adjusted model. As such, we were unable to reach a definitive conclusion.
The temporal association between intellectual activity and nutritional status was not statistically confirmed, although consistent trends were observed. Cognitive decline affects daily functional status, which can lead to dependence and decreased oral intake[33] and is also associated with nutritional status[11]. The present study focused on the independent risk of intellectual activity for nutritional status by adjusting for cognitive function, and it was not significant. Intellectual activities include the capacity to gather information related to health topics, which represents health literacy[34]. A higher health literacy contributes to better nutritional quality[35]. Hence, we hypothesized that intellectual activity could be related to a reduction in the risk of nutritional decline. It seems difficult to conclude the direct association of that activity with future nutritional status based on the current results.
Social functioning did not contribute to preventing the decline in nutritional status. When the social aspects of eating are considered, food consumption may increase, thereby improving nutritional status[36]. Loss of family or friends is negatively associated with intake[37]. Fewer friends, loneliness, and the death of a spouse increase the risk of protein-energy malnutrition[14]. Despite the relationship between social aspects and nutritional factors, no such association was found in this study. The questionnaire used in the current study included only limited aspects of social factors, such as visiting friends and advice to someone, which might bring different results to those of earlier studies.
Malnutrition is associated with the incidence of IADL disability, including basic ADL[38]. Our results, coupled with the association, implicate a hypothetical model wherein nutritional status and IADL could be interinfluenced. The current investigation, being an observational study, might have bias and unknown confounding variables; as a result, it is important to interpret the causal connections between IADL and malnutrition with caution. Nevertheless, the possibility that maintaining IADL or assistance as functional capacity can contribute to the prevention of nutritional deterioration seems logical and should be considered.
The current study has some limitations. First, a few participants dropped out of the 2-year follow-up assessments. Indeed, non-followed participants presented lower cognitive function and intellectual activity than the follow-up participants, which may have involved a selection bias. However, this difference was marginal. Therefore, we considered that the risk of serious selection bias was not high. Second, we treated nutritional risk (MNA-SF scores from 8 to 11) or malnutrition (scores from 0 to 7) as indicators of nutritional deterioration, without using a full version of MNA. Therefore, the current results cannot definitively conclude that decreased functional capacity is associated with the onset of malnutrition. Third, the statistical power by the post-hoc analysis was not high, which suggesting that larger sample size could have potentially yielded more significant results. Hence, future studies with larger sample sizes may help to strengthen these findings. Fourth, since this study is observational, not intervention, we can’t r assert any causal associations.
Conclusions
Our study underscores that a decline in functional capacity, especially IADL, is a risk factor for future deterioration of nutritional status. Among the sub-items of the MNA-SF, weight loss appears to be a sensitive domain. Further studies are required to elucidate the effects of interventions for IADL decline on maintaining nutritional status in older adults.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IADL:
-
instrumental activities of daily living
- RR:
-
Risk ratio
- CI:
-
confidence interval
- MNA-SF:
-
Mini Nutritional Assessment Screening Form
- MMSE:
-
Mini-Mental State Examination
- BMI:
-
body mass index
- TMIG-IC:
-
Tokyo Metropolitan Institute of Gerontology Index of Competence
- GDS:
-
Geriatric Depression Scale
References
Zhao W, Ukawa S, Okada E, Wakai K, Kawamura T, Ando M, Tamakoshi A. The associations of dietary patterns with all-cause mortality and other lifestyle factors in the elderly: an age-specific prospective cohort study. Clin Nutr. 2019;38(1):288–96.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, Compher C, Correia I, Higashiguchi T, Holst M, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64.
Amaral TF, Matos LC, Teixeira MA, Tavares MM, Alvares L, Antunes A. Undernutrition and associated factors among hospitalized patients. Clin Nutr. 2010;29(5):580–5.
Dent E, Visvanathan R, Piantadosi C, Chapman I. Nutritional screening tools as predictors of mortality, functional decline, and move to higher level care in older people: a systematic review. J Nutr Gerontol Geriatr. 2012;31(2):97–145.
Söderström L, Rosenblad A, Thors Adolfsson E, Bergkvist L. Malnutrition is associated with increased mortality in older adults regardless of the cause of death. Br J Nutr. 2017;117(4):532–40.
Johansson Y, Bachrach-Lindström M, Carstensen J, Ek A-C. Malnutrition in a home-living older population: prevalence, incidence and risk factors. A prospective study. J Clin Nurs. 2009;18(9):1354–64.
Guyonnet S, Rolland Y. Screening for Malnutrition in Older People. Clin Geriatr Med. 2015;31(3):429–37.
Kaiser MJ, Bauer JM, Rämsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony PS, Charlton KE, Maggio M, et al. Frequency of Malnutrition in older adults: a multinational perspective using the Mini Nutritional Assessment. J Am Geriatr Soc. 2010;58(9):1734–8.
Mastronuzzi T, Paci C, Portincasa P, Montanaro N, Grattagliano I. Assessing the nutritional status of older individuals in family practice: evaluation and implications for management. Clin Nutr. 2015;34(6):1184–8.
Iizaka S, Tadaka E, Sanada H. Comprehensive assessment of nutritional status and associated factors in the healthy, community-dwelling elderly. Geriatr Gerontol Int. 2008;8(1):24–31.
Saka B, Kaya O, Ozturk GB, Erten N, Karan MA. Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin Nutr. 2010;29(6):745–8.
Ferdous T, Cederholm T, Razzaque A, Wahlin A, Nahar Kabir Z. Nutritional status and self-reported and performance-based evaluation of physical function of elderly persons in rural Bangladesh. Scand J Public Health. 2009;37(5):518–24.
Fávaro-Moreira NC, Krausch-Hofmann S, Matthys C, Vereecken C, Vanhauwaert E, Declercq A, Bekkering GE, Duyck J. Risk factors for Malnutrition in older adults: a systematic review of the literature based on Longitudinal Data. Adv Nutr. 2016;7(3):507–22.
van der Pols-Vijlbrief R, Wijnhoven HA, Schaap LA, Terwee CB, Visser M. Determinants of protein-energy malnutrition in community-dwelling older adults: a systematic review of observational studies. Ageing Res Rev. 2014;18:112–31.
Lawton MP. Assessing the competence of older people, Research Planning and Action for the Elderly: the power and potential of Social Science. New York: Human Sciences Press; 1972.
Perneczky R, Wagenpfeil S, Komossa K, Grimmer T, Diehl J, Kurz A. Mapping scores onto stages: mini-mental state examination and clinical dementia rating. Am J Geriatr Psychiatry. 2006;14(2):139–44.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56(6):M366–372.
Koyano W, Shibata H, Nakazato K, Haga H, Suyama Y. Measurement of competence: reliability and validity of the TMIG Index of competence. Arch Gerontol Geriatr. 1991;13(2):103–16.
Sakurai R, Yasunaga M, Murayama Y, Ohba H, Nonaka K, Suzuki H, Sakuma N, Nishi M, Uchida H, Shinkai S, et al. Long-term effects of an intergenerational program on functional capacity in older adults: results from a seven-year follow-up of the REPRINTS study. Arch Gerontol Geriatr. 2016;64:13–20.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5.
Sugishita K, Sugishita M, Hemmi I, Asada T, Tanigawa T. A validity and reliability study of the Japanese Version of the geriatric Depression Scale 15 (GDS-15-J). Clin gerontologist. 2017;40(4):233–40.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6.
El Zoghbi M, Boulos C, Awada S, Rachidi S, Al-Hajje A, Bawab W, Saleh N, Salameh P. Prevalence of malnutrition and its correlates in older adults living in long stay institutions situated in Beirut, Lebanon. J Res Health Sci. 2014;14(1):11–7.
Fishman P. Detecting malnutrition’s warning signs with simple screening tools. Geriatrics. 1994;49(10):39–42. 345; quiz 346-347.
Peres K, Helmer C, Amieva H, Orgogozo JM, Rouch I, Dartigues JF, Barberger-Gateau P. Natural history of decline in instrumental activities of daily living performance over the 10 years preceding the clinical diagnosis of dementia: a prospective population-based study. J Am Geriatr Soc. 2008;56(1):37–44.
Amasene M, Medrano M, Echeverria I, Urquiza M, Rodriguez-Larrad A, Diez A, Labayen I, Ariadna BB. Malnutrition and poor physical function are Associated with higher Comorbidity Index in hospitalized older adults. Front Nutr. 2022;9:920485.
Ho C, Feng L, Fam J, Mahendran R, Kua EH, Ng TP. Coexisting medical comorbidity and depression: multiplicative effects on health outcomes in older adults. Int Psychogeriatr. 2014;26(7):1221–9.
Jyrkka J, Mursu J, Enlund H, Lonnroos E. Polypharmacy and nutritional status in elderly people. Curr Opin Clin Nutr Metab Care. 2012;15(1):1–6.
Han Y, Li S, Zheng Y. Predictors of nutritional status among community-dwelling older adults in Wuhan, China. Public Health Nutr. 2009;12(8):1189–96.
Callen BL, Wells TJ. Views of community-dwelling, old-old people on barriers and aids to nutritional health. J Nurs scholarship: official publication Sigma Theta Tau Int Honor Soc Nurs. 2003;35(3):257–62.
Ulger Z, Halil M, Kalan I, Yavuz BB, Cankurtaran M, Gungor E, Ariogul S. Comprehensive assessment of malnutrition risk and related factors in a large group of community-dwelling older adults. Clin Nutr. 2010;29(4):507–11.
Donini LM, Scardella P, Piombo L, Neri B, Asprino R, Proietti AR, Carcaterra S, Cava E, Cataldi S, Cucinotta D, et al. Malnutrition in elderly: social and economic determinants. J Nutr Health Aging. 2013;17(1):9–15.
Claggett MS. Nutritional factors relevant to Alzheimer’s disease. J Am Diet Assoc. 1989;89(3):392–6.
Iwasa H, Masui Y, Inagaki H, Yoshida Y, Shimada H, Otsuka R, Kikuchi K, Nonaka K, Yoshida H, Yoshida H, et al. Assessing competence at a higher level among older adults: development of the Japan Science and Technology Agency Index of competence (JST-IC). Aging Clin Exp Res. 2018;30(4):383–93.
Kuczmarski MF, Adams EL, Cotugna N, Pohlig RT, Beydoun MA, Zonderman AB, Evans MK. Health literacy and Education Predict Nutrient Quality of Diet of socioeconomically diverse, urban adults. J Epidemiol Prev Med 2016, 2(1).
Cassens D, Johnson E, Keelan S. Enhancing taste, texture, appearance, and presentation of pureed food improved resident quality of life and weight status. Nutr Rev. 1996;54(1 Pt 2):51–4.
Amarantos E, Martinez A, Dwyer J. Nutrition and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):54–64.
Wei K, Nyunt MSZ, Gao Q, Wee SL, Ng TP. Long-term changes in nutritional status are associated with functional and mortality outcomes among community-living older adults. Nutrition. 2019;66:180–6.
Acknowledgements
We acknowledge Ayumi Tanigaki, Haruka Goto, and Mariko Oka for their contributions to data collection.
Funding
This work was supported by JSPS KAKENHI [Grant numbers: JP16KT0012, JP19K19723 and 22K11136]. The funding sources had no role in the design of the study, collection, analysis, interpretation of data, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
KN and KS2 were involved in the original conception and design of this study. Data acquisition was conducted by KN, TK, MI, MG, KT, RM, HK, YW, ST, and KS. KN, TK, and KS2 conducted the statistical analysis and interpretation of the data. KN, TK, MI, MG, and KS2 drafted the manuscript. KT, RM, HK, YW, ST, and KS1 ST, and KS1 critically revised the manuscript for intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to patriciate
The ethics review board of Hyogo College of Medicine (No. Rinhi 0342) approved this research, and it was conducted following the principles of the Declaration of Helsinki. Before the study began, participants were given both oral and written explanations about the study and provided written informed consent.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nagai, K., Komine, T., Ikuta, M. et al. Decline of instrumental activities of daily living is a risk factor for nutritional deterioration in older adults: a prospective cohort study. BMC Geriatr 23, 480 (2023). https://doi.org/10.1186/s12877-023-04185-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04185-6