Abstract
Background
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can lead to multiorgan insufficiency and death, particularly among the older adults. Statins have been suggested as potentially protective drugs due to their pleotropic effects, but the actual benefit of statin use among the older population in this setting is not clear. This study aimed to evaluate the association between preadmission statin use and the presentation and clinical outcomes of hospitalized COVID-19 patients older than 70 years of age.
Methods
A historical cohort study of all patients above 70 years of age who were hospitalized with COVID-19 infection in a large academic hospital between March and August 2020 was performed. The association between preadmission statin use and patients’ presentation and adverse outcome was studied. Adverse outcome was defined as any of the following: shock, invasive or non-invasive ventilation, organ insufficiency, myocardial infarction, cerebrovascular accident, in-hospital or 30-day post-admission mortality, hospital stay longer than the median length of stay of all COVID-19 patients, referral to nursing home or rehabilitation center.
Results
Seventy-two (44%) of the 163 studied patients (median age 82 years, 45% males) had been preadmission treated with statins. The statin-treated patients (STP) had a higher prevalence of diabetes (40% vs 24%, p = 0.028) and cardiovascular disease (58% vs. 34%, p = 0.002). Seventy two percent of the STP had adverse outcome, compared to 86% of the non-STP (p = 0.033). After adjustment for potential confounders, prior statin use was associated with decreased risk for an adverse outcome (odds ratio = 0.4, 95% confidence interval 0.18–0.92, p = 0.03).
Conclusions
The preadmission use of statins was associated with a lower risk of adverse outcome in older adults hospitalized with COVID-19. Continuation of statin treatment might be implemented for risk reduction of adverse outcomes in the older population in the era of new SARS-CoV-2 variants and less effective vaccines.
Similar content being viewed by others
Background
As of March 2022, coronavirus disease-2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has affected over 470,000,000 people and caused more than 6,100,000 deaths worldwide [1]. COVID-19 may lead to multiorgan insufficiency, particularly among the older population and patients with chronic conditions, such as cardiovascular disease, chronic obstructive pulmonary disease, diabetes mellitus and obesity [2,3,4]. Older adults are generally defined as those 70 years of age and older [5], and they have an increased risk to develop atherosclerotic cardiovascular disease. Statins are the most effective treatment for primary prevention and even more significant with regard to secondary prevention of cardiovascular disease, having been shown to decrease the risk of both cerebrovascular and coronary artery disease in older adults, similar to their effects in young populations [6, 7].
A beneficial role of statins was shown in the patients with pneumonia, other infection diseases and sepsis based upon their well-established pleotropic properties [8,9,10]. The association between statins and the clinical outcomes of COVID-19 patients was recently investigated in several retrospective studies, meta-analyses and a few randomized controlled trials. Most of those studies found that statin use was associated with improved clinical outcomes, while others reported no such association and even adverse outcomes among statin users [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Although some studies included stratification according to age and showed mixed results, only one study directly addressed disease outcome specifically among hospitalized and non-hospitalized older patients, while there is no reported meta-analysis on this specific population [13]. The aim of this retrospective study was to evaluate the association between preadmission statin use and the presentation and clinical outcomes of hospitalized COVID-19 patients older than 70 years of age.
Methods
Study design and population
A historical cohort study of all patients above 70 years of age who were hospitalized with COVID-19 infection during the first wave of the pandemic and who received the same pharmacological treatments, which included steroids, was performed between March and August 2020 at the Tel Aviv Sourasky Medical Center (TASMC). TASMC is a tertiary university-affiliated 1500-bed medical center located in central Israel. Only patients with laboratory-confirmed COVID-19 infections were included in the study. Excluded from the study were patients whose data could not be accessed, as well as subjects who had end-stage/advanced malignancy, liver cirrhosis, past single or multiple organ transplantations, and those who continued care at another acute medical center. Also excluded were patients with nosocomial COVID-19 according to European Centre for Disease Prevention and Control (CDC) (i.e., diagnosed after the 7th day of hospitalization), women who were admitted to hospital to give birth and pregnant women. The study was approved by the local ethics committee (TLV-0341–20).
Data source, measurement and variables
All of the analyzed data were retrieved from the hospital database. Data on demographic parameters (age and gender), anthropometric measurements (weight and body mass index), first vital signs on emergency department admission (pulse, systolic blood pressure, diastolic blood pressure, body temperature and oxygen saturation), comorbidities, first blood test findings on emergency room admission and chronically used medications (angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, calcium channel blockers, beta blockers, diuretics, aspirin and insulin) were collected. Information on hypertension (HTN), diabetes mellitus (DM), cardiac disease, cerebrovascular disease (CVA/TIA), chronic renal failure (CRF), chronic obstructive pulmonary disease (COPD) or asthma, chronic liver disease and hypothyroidism was also recorded. Disease severity was determined using the NIH classification criteria [27].
Blood tests results included complete blood count, C-reactive protein (CRP), creatinine, and liver enzymes (alanine transaminase, aspartate transaminase, alkaline phosphatase and gamma glutamyl transferase). The estimated glomerular filtration rate was calculated with the CKD-EPI equation [28]. Shock, invasive or non-invasive ventilation, organ insufficiency, myocardial infarction or cerebrovascular accident during admission, in-hospital or 30-day post-admission mortality, hospital stay longer than the median length of all-adult COVID-19 patients’ stay and new referral to a nursing home or rehabilitation center were considered as an adverse outcome.
Laboratory methods
Blood cell counts were performed with the Beckman Coulter UniCel. Blood chemistry tests were measured by ADVIA (Siemens Healthcare Diagnostics Inc., Tarrytown, NY 10591–5097 USA) as described previously [29]. Viral respiratory infection was diagnosed by polymerase chain reaction methodology.
Statistical analysis
Sample size was calculated using a significance level of 5% and a power of 80%. We assumed that approximately 30% of the STP would have an adverse outcome compared to 55% of non-STP. In addition, a ratio of 1:1 between STP and non-STP groups was assumed, whereupon 136 individuals would be needed.
Categorical variables were described as frequency and percentage. Continuous variables were evaluated for normal distribution using histograms and Q-Q plots and reported as median and interquartile range (IQR) for readers’ ease. The Chi-square test and Fisher’s exact test were used to compare categorical variables and independents samples, and the T-test and Mann–Whitney test were applied to compare continuous variables. Due to the limited sample size and the variety of medications, the associations between medication and adverse event were included only in the univariate analysis. A multivariable logistic regression was used to identify the independent association between routine statin use and adverse outcome. The multivariable analysis included only pre-admission variables, since vital signs and blood tests at admission may represent the acute phase rather than the patient's background status. Due to the restrictions imposed by the pandemic setting, anthropometric measurements were estimated rather than precisely measured in some patients, and those parameters were not included in the multivariable analysis.
The regression included two blocks: routine statin use was entered in the first block while age, gender and all comorbidities were entered in the second block followed by the application of a backward method with the Wald test to remove variables with a p value > 0.1. All statistical tests were two-tailed, and p < 0.05 was considered statistically significant. All statistical analyses were performed with SPSS (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp.)
Results
Patients’ characteristics
A total of 163 patients met the inclusion criteria during the study period. The group's median age was 82 years and 73 (45%) were males. HTN was the most common comorbidity (n = 104, 64%), followed by cardiac disease (n = 73, 45%), DM (n = 51, 31%) and COPD/asthma (n = 33, 20%). The prevalence of other studied comorbidities was less than 20%. Forty one (25%) patients had an estimated glomerular filtration rate less than 45 mL/min/1.73m2 on admission, and the group’s median CRP was 57 mg/L. Seventy two (44%) patients used statins regularly before being admitted to the hospital, 55 (34%) used aspirin, 60 (37%) used beta blockers, 51 (31%) used calcium channel blockers and 47 (29%) used diuretics. Table 1 summarizes the patients’ characteristics.
Age and gender distribution of patients who were taking statins regularly (STP) were not significantly different from those who did not use statins (NSTP), while DM and cardiovascular disease were more common among the STP (40% vs 24% and 58% vs. 34%, respectfully). Vital signs, blood test results and the severity of COVID-19 at emergency department admission were not statistically different between the two groups. Angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, calcium channel blockers, beta blockers, diuretics and aspirin were more commonly used by patients who also used statins on a regular basis. Table 1 compares patients’ characteristics in the two groups.
Adverse outcome
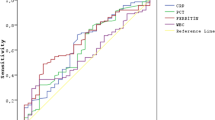
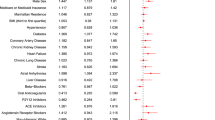
In total, 130 patients sustained an adverse outcome during hospitalization, including 10 patients with shock, 111 who were ventilated (29 invasive and 107 non-invasive), 54 with organ insufficiency and 6 with myocardial infarction or a cerebrovascular accident. Forty-seven patients died in the hospital and another 2 patients died during 30 days post-admission. In addition, 111 were hospitalized longer than the median length of stay of all-age COVID-19 patients (5 days), 7 were referred to nursing homes and 7 were referred to rehabilitation centers. Taken together, these findings revealed that 72% of the STP had an adverse outcome compared to 86% of NSTP (p = 0.033). The patients who sustained adverse events were older (median 82.7 vs 76.1 years, p = 0.011), had lower hemoglobin levels (12.5 vs. 13.8 g/dL, p = 0.005) and higher inflammatory biomarkers on admission (median WBC 7.5 vs. 6.1 K/mcL, p = 0.002, median CRP 67.1 vs 10.7, p < 0.001). Comorbidities and chronic treatments with medications other than statins were not significantly different between the patients with and those without an adverse outcome. Table 2 presents the crude association between an adverse outcome and patient characteristics. After controlling for potential confounders, prior statin use was associated with a decreased risk for an adverse outcome (odds ratio [OR] = 0.4, p = 0.03), while older age (OR = 1.07, p = 0.019) was associated with an increased risk (Fig. 1).
Discussion
COVID-19 caused by SARS-CoV-2 first appeared in late 2019 and spread rapidly, leading to a global pandemic. The older population has been reported to be at increased risk for serious outcomes in many studies. The newly developed vaccines have led to a significant reduction in morbidity and mortality, however, the appearance of the new variants elicited a significant decrease in vaccine efficacy. Statin therapy is common in the older population, especially among those with major illnesses associated with poor disease outcomes. This addition of new therapies designed to contend with an unprecedented milieu emphasizes the importance of examining the association between routine statin use and poor outcome, specifically among older COVID-19 patients. This study, therefore, aimed to evaluate the association between preadmission statin use and the presentation and clinical outcomes of hospitalized COVID-19 patients older than 70 years of age.
The results of this retrospective study suggest that although there were no significant clinical differences between the STP group and the NSTP group with regard to the severity of COVID-19 at presentation, preadmission statin use was associated with a decreased risk for an adverse outcome (OR = 0.4, 95% confidence interval [CI] 0.18–0.92, p = 0.03).
As expected, more STP presented with DM compared to NSTP (40% vs 20%, respectively) as well as with cardiovascular disease (58% vs 34%). Memel et al. described higher rates of HTN, DM, coronary artery disease, heart failure, and chronic kidney disease among 43.1% of their STP who were > 65 years of age [17]. El-Solh et al. analyzed data from the USA Department of Veterans Affairs (not all hospitalized patients): 50.2% were STP who were older than the NSTP group (68.2 vs. 58.9 years, respectively, p < 0.001) and had higher rates of HTN, DM, cardiac diseases, and chronic kidney disease [19]. De Spiegeleer et al. investigated the effects of statins on clinical outcomes of COVID-19 infection among 154 nursing home residents with a mean age of 86 years [13]. Those authors found an association between statin treatment and asymptomatic COVID-19 infection (OR 2.65; CI 1.13–6.68) among that older population. The statin-treated ones tended to have less serious clinical outcomes but not to a level of significance (OR 0.75; CI 0.24–1.87).
There are several explanations for the positive effect of statins on clinical outcome after COVID-19 infection. First, they show immune modulation and counteraction against the inflammatory response and the cytokine storm leading to the acute respiratory distress syndrome often present in viral infections. Second, stabilization by statins of the product of the MYD88 gene that regularly activates NF-κB resulting in mitigation of the inflammatory response has been reported in animal models [30,31,32,33]. Third, SARS-CoV-2 invades cells through the angiotensin-converting enzyme 2 receptor which is upregulated by statins. Fourth, statins have a role in preventing endothelial dysfunction and hypercoagulability, which are major contributors to the pathogenesis of COVID-19 [11, 12, 34]. Lastly, statins have the potential of acting against the negative effect of some of the other COVID-19 drugs on the lipid profile [35, 36].
The major strength of this study is the use of systematic electronic medical records of preadmission STP older than 70 years of age at the time of admission for COVID-19. The study was designed to include all consecutive patients that met the inclusion and exclusion criteria, thus, making selection bias unlikely to occur. All studied outcomes were fully recorded in the patients' records, and disease severity was based upon updated NIH classification [27].
Our study has a several limitations that bear mention. First, it includes a retrospective cohort of patients treated in a single medical center. Second, there is the possibility that some of the same patients were later readmitted to a different hospital, resulting in the loss of final follow-up of the patients in our database. Since the number of those latter patients is negligible, however, the influence of that caveat on the study results is likely to be small. Finally, our cohort of patients was recruited from the beginning of the pandemic period, before drugs intended to directly treat the COVID-19 patients were offered and before vaccines were available. However, those drawbacks did not prevent this cohort of patients to enable us to evaluate the association between statin use and COVID-19 severity among the older population.
In conclusion, the results of this retrospective study showed significant protective effects of statin use on adverse outcomes among older adult patients hospitalized for COVID-19, and demonstrated the importance of continuing chronic statin therapy.
Availability of data and materials
The data that support the findings of this study are available from database of the Tel Aviv Sourasky Medical Center, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Tel Aviv Sourasky Medical Center.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- STP:
-
Statin-treated patients
- NSTP:
-
Non-statin-treated patients
References
WHO Coronavirus (COVID-19) dashboard. Available from: https://covid19.who.int. Cited 2022 Mar 24.
The novel coronavirus pneumonia emergency response epidemiology team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Wkly. 2020;2(8):113–22.
Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5.
Burton JH, Young J, Bernier CA. The Geriatric ED: structure, patient care, and considerations for the emergency department geriatric unit. Int J Gerontol. 2014;8:56–9.
Horodinschi R-N, Stanescu AMA, Bratu OG, Stoian AP, Radavoi DG, Diaconu CC. Treatment with statins in elderly patients. Medicina. 2019;55:721.
Armitage J, Baigent C, Barnes E, Betteridge DJ, Blackwell L, Blazing M, et al. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407–15.
Wang CY, Liu PY, Liao JK. Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol Med. 2008;14(1):37–44.
Khan AR, Riaz M, Bin Abdulhak AA, Al-Tannir MA, Garbati MA, Erwin PJ, Baddour LM, Tleyjeh IM. The role of statins in prevention and treatment of community acquired pneumonia: a systematic review and meta-analysis. PLoS One. 2013;8(1):e52929.
Falagas ME, Makris GC, Matthaiou DK, Rafailidis PI. Statins for infection and sepsis: a systematic review of the clinical evidence. J Antimicrob Chemother. 2008;61(4):774–85.
Choi D, Chen Q, Goonewardena SN, Pachenco H, Mejia P, Smith RL, et al. Efficacy of stain therapy in patients with hospital admission for Covid-19. Cardiovasc Drugs Ther. 2022;36(6):1165–73.
Bergqvist R, Ahlqvist VH, Lundberg M, Hergens M-P, Sundström J, Bell M, et al. HMG-CoA reductase inhibitors and COVID-19 mortality in Stockholm, Sweden: A registry-based cohort study. PLOS Med. 2021;18(10): e1003820.
De Spiegeleer A, Bronselaer A, Teo JT, Byttebier G, De Tré G, Belmans L, et al. The effects of ARBs, ACEis, and statins on clinical outcomes of COVID-19 infection among nursing home residents. J Am Med Dir Assoc. 2020;21(7):909-914.e2.
Song SL, Hays SB, Panton CE, Mylona EK, Kalligeros M, Shehadeh F, et al. Statin use is associated with decreased risk of invasive mechanical ventilation in COVID-19 patients: a preliminary study. Pathogens. 2020;9(9):759.
Butt JH, Gerds TA, Schou M, Kragholm K, Phelps M, Havers-Borgersen E, et al. Association between statin use and outcomes in patients with coronavirus disease 2019 (COVID-19): a nationwide cohort study. BMJ Open. 2020;10(12):e044421.
Bikdeli B, Talasaz AH, Sharif-Kashani B, INSPIRATION-S Investigators. Atorvastatin versus placebo in patients with COVID-19 in intensive care: randomized controlled trial. BMJ. 2022;376:e068407.
Memel ZN, Lee JJ, Foulkes AS, Chung RT, Thaweethai T, Bloom PP. Association of statins and 28-day mortality rates in patients hospitalized with severe acute respiratory syndrome coronavirus 2 infection. J Infect Dis. 2022;225(1):19–29.
McAlister FA, Wang T, Wang X, Chu A, Goodman SG, van Diepen S, et al. Statins and SARS-CoV-2 infection: results of a population-based prospective cohort study of 469 749 adults from 2 Canadian provinces. J Am Heart Assoc. 2021;10(21): e022330.
El-Solh AA, Lawson Y, El-Solh DA. All-cause mortality in COVID-19 patients receiving statin therapy: analysis of veterans affairs database cohort study. Intern Emerg Med Intern Emerg Med. 2022;17(3):685–94.
Lohia P, Kapur S, Benjaram S, Mir T. Association between antecedent statin use and severe disease outcomes in COVID-19: a retrospective study with propensity score matching. J Clin Lipidol. 2021;15(3):451–9.
Oh TK, Song IA, Jeon YT. Statin Therapy and the Risk of COVID-19: A Cohort study of the national health insurance service in South Korea. J Pers Med. 2021;11(2):116.
Lee HY, Ahn J, Park J, Kyung Kang C, Won SH, Wook Kim D, et al. Beneficial effect of statins in COVID-19–related outcomes—brief report. Arterioscler Thromb Vasc Biol. 2021;41(3):e175–82.
Mitacchione G, Schiavone M, Curnis A, Arca M, Antinori S, Gasperetti A, et al. Impact of prior statin use on clinical outcomes in COVID-19 patients: data from tertiary referral hospitals during COVID-19 pandemic in Italy. J Clin Lipidol. 2021;15(1):68–78.
Vahedian-Azimi A, Mohammadi SM, Banach M, Beni FH, Guest PC, Al-Rasadi K, et al. Improved COVID-19 outcomes following statin therapy: an updated systematic review and meta-analysis. BioMed Res Int. 2021;2021: e1901772.
Wu C-C, Lee A-J, Su C-H, Huang C-Y, Islam MM, Weng Y-C. Statin use is associated with a decreased risk of mortality among patients with COVID-19. J Clin Med. 2021;10(7):1450.
Diaz-Arocutipa C, Melgar-Talavera B, Alvarado-Yarasca Á, Saravia-Bartra MM, Cazorla P, Belzusarri I, et al. Statins reduce mortality in patients with COVID-19: an updated meta-analysis of 147 824 patients. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2021;110:374–81.
National Institutes of Health (NIH). Therapeutic management of adults with COVID- 19. COVID-19 treatment guidelines. Available from: https://www.covid19treatmentguidelines.nih.gov/therapeutic-management/. Cited 2021 Mar 18.
Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, et al. Chronic kidney disease epidemiology collaboration new creatinine- and cystatin C-based equations to estimate GFR without race. N Engl J Med. 2021;385(19):1737–49.
Ziv-Baran T, Wasserman A, Goldiner I, Stark M, Shenhar-Tsarfaty S, Shapira I, et al. The association between C-reactive protein and common blood tests in apparently healthy individuals undergoing a routine health examination. Clin Chim Acta. 2020;501:33–41.
Dixon DL, Van Tassell BW, Vecchié A, Bonaventura A, Talasaz A, Kakavand H, et al. Cardiovascular considerations in treating patients with coronavirus (COVID-19). J Cardiovasc Pharmacol. 2020;75(5):359–357.
Makris D, Manoulakas E, Komnos A, Papakrivou E, Tzovaras N, Hovas A, et al. Effect of pravastatin on the frequency of ventilator-associated pneumonia and on intensive care unit mortality: open-label, randomized study. Crit Care Med. 2011;39(11):2440–6.
Pertzov B, Eliakim-Raz N, Atamna H, Trestioreanu AZ, Yahav D, Leibovici L. Hydroxymethylglutaryl-CoA reductase inhibitors (statins) for the treatment of sepsis in adults – a systematic review and meta-analysis. Clin Microbiol Infect. 2019;25(3):280–9.
Rogers AJ, Guan J, Trtchounian A, Hunninghake GM, Kaimal R, Desai M, et al. Association of elevated plasma interleukin-18 level with increased mortality in a clinical trial of statin treatment for acute respiratory distress syndrome. Crit Care Med. 2019;47(8):1089–96.
Oesterle A, Laufs U, Liao JK. Pleiotropic Effects of statins on the cardiovascular system. Circ Res. 2017;120(1):229–43.
DAD Study Group, Friis-Møller N, Reiss P, Sabin CA. Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med. 2007;356(17):1723–35.
Soubrier M, Pei J, Durand F, Gullestad L, John A. Concomitant use of statins in tocilizumab-treated patients with rheumatoid arthritis: a post hoc analysis. Rheumatol Ther. 2017;4(1):133–49.
Acknowledgements
We thank Esther Eshkol, MA, the institutional medical and scientific copyeditor, for editorial assistance.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Conceptualization: E.I., Y.V. Design: E.I., Y.V., Y.G, T.Z.B. Acquisition of data: E.I., Y.V. Statistical analysis E.I., Y.V., T.Z.B. Interpretation of data: E.I., Y.V., A.B., V.D., D.N., A.N., Y.G, T.Z.B. Manuscript writing: E.I., Y.V., A.B., V.D., D.N., A.N., Y.G, T.Z.B. Approval of the final text: All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Helsinki Medical Ethics Committee of the Tel Aviv Sourasky Medical Center provided approval to conduct this study (approval # TLV-0341–20) and waived signed informed consent since the study was based on existing databases.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Izkhakov, E., Vilian, Y., Buch, A. et al. Routine statins use is associated with less adverse outcome in patients above 70 years of age admitted to hospital with COVID-19. BMC Geriatr 23, 473 (2023). https://doi.org/10.1186/s12877-023-04183-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04183-8