Abstract
Background
Perturbation-based balance training (PBT) is an emerging intervention shown to improve balance recovery responses and reduce falls in everyday life in older adults. However, perturbation interventions were heterogeneous in nature and need improvement. This study aims to investigate the effects of a PBT protocol that was designed to address previously identified challenges of PBT, in addition to usual care, on balance control and fear of falling in older adults at increased risk of falling.
Methods
Community-dwelling older adults (age ≥ 65 years) who visited the hospital outpatient clinic due to a fall incident were included. Participants received PBT in addition to usual care (referral to a physiotherapist) versus usual care alone. PBT consisted of three 30-minute sessions in three weeks. Unilateral treadmill belt accelerations and decelerations and platform perturbations (shifts and tilts) were applied during standing and walking on the Computer Assisted Rehabilitation Environment (CAREN, Motek Medical BV). This dual-belt treadmill embedded in a motion platform with 6 degrees of freedom is surrounded by a 180° screen on which virtual reality environments are projected. Duration and contents of the training were standardised, while training progression was individualised. Fear of falling (FES-I) and balance control (Mini-BESTest) were assessed at baseline and one week post-intervention. Primary analysis compared changes in outcome measures between groups using Mann-Whitney U tests.
Results
Eighty-two participants were included (PBT group n = 39), with a median age of 73 years (IQR 8 years). Median Mini-BESTest scores did not clinically relevantly improve and were not significantly different between groups post-intervention (p = 0.87). FES-I scores did not change in either group.
Conclusions
Participation in a PBT program including multiple perturbation types and directions did not lead to different effects than usual care on clinical measures of balance control or fear of falling in community-dwelling older adults with a recent history of falls. More research is needed to explore how to modulate PBT training dose, and which clinical outcomes are most suitable to measure training effects on balance control.
Trial registration
Nederlands Trial Register NL7680. Registered 17-04-2019 – retrospectively registered. https://www.trialregister.nl/trial/7680.
Similar content being viewed by others
Introduction
Falls annually affect one in three adults over 65 years [1, 2]. In 2019, approximately 109.000 Dutch adults over 65 years visited the emergency department due to a fall incident, resulting in over 1 billion euros of direct medical costs [3]. Falls are a leading cause of injuries and hospitalization among older adults and can have many physical and psychological adverse consequences [4, 5]. The risk of falling increases with age and can increase even further in the presence of additional risk factors. An important and modifiable risk factor for falls is balance control [6, 7]. Having experienced a fall incident is another prognostic factor, which greatly increases the risk of sustaining future falls (odds ratio (OR) 2.8 for all fallers, and 3.5 for recurrent fallers) [6, 8, 9]. Consequently, older adults who have fallen are also more likely to develop fear of falling, and to experience a further decline in balance control after their fall incident [10, 11]. Since fear of falling and impaired balance control both increase the risk for falls, this illustrates how a single fall incident can cause older adults to end up in a negative cycle [10]. Given that the number of older adults is currently increasing rapidly, the burden of falls will continue to increase. Therefore, it is essential to develop interventions that make older adults more resistant to fall incidents.
Balance training is reported to effectively improve balance control and reduce fall rates in older adults by approximately 24% [12, 13]. Nonetheless, there are some drawbacks to conventional balance training interventions. Firstly, it should be understood that ‘balance control’ is an umbrella concept that can be subdivided into multiple motor skills [14], each of which is vital to perform activities of daily living. As described by Berg et al., balance control can be divided into three general categories: maintaining a position (static balance control), adjusting voluntary or anticipated movements (proactive balance control), and reacting to external or unexpected balance perturbations (reactive balance control) [15]. Conventional balance training programs do not typically address reactive balance control but focus mostly on proactive balance control [16]. However, approximately 60% of falls in older adults result from an unexpected external perturbation during walking, such as a slip or trip [17]. As the recovery actions needed to prevent such falls rely mostly on reactive balance control, the task-specificity of conventional balance training may be limited [18, 19]. Additionally, conventional balance training requires a relatively high number of training sessions to be effective, and retention of training effects is hard to accomplish [20,21,22]. As such, research to optimize balance training interventions for older adults continues.
In recent years, perturbation-based balance training (PBT) has gained increasing interest as an intervention which is more task-specific to the recovery actions needed to prevent falls from unexpected balance perturbations. PBT aims to improve reactive balance by repeatedly exposing participants to destabilizing perturbations in a safe and controlled environment. Results from two meta-analyses indicate that PBT can significantly reduce daily-life fall rates by 46% and 52%, respectively [23, 24]. Studies have also found beneficial effects of PBT on the number of laboratory-induced falls [25,26,27], various measures of balance recovery (e.g. margins of stability after perturbation or time to stabilization of center of pressure) [25, 27,28,29,30,31,32], and balance control (e.g. limits of stability, five-step test, and Berg Balance Scale (BBS)) [33,34,35,36]. Additionally, PBT may have the potential to be effective with a low training dose (one to four training sessions), which could make PBT a more efficient alternative to other interventions [37,38,39,40].
While current studies report promising results of PBT, they are heterogeneous in terms of training parameters, study populations, and outcomes. Further study is required to help develop effective training protocols that are tolerable and acceptable to the target population. To build upon the literature, this study will address some previous identified challenges of PBT. Firstly, studies have suggested that PBT training effects may be limited to the specific condition that was trained [39, 41], or only partly generalizable to different conditions [18, 42]. This is a factor that should be addressed to ensure a beneficial impact on everyday life, where falls can happen in all kinds of conditions. A potential strategy that has been proposed to improve the generalization of adaptations to PBT is to include a variety of training conditions (for example multiple perturbation types and directions) [43]. Secondly, other challenges include the physical tolerability and acceptability of PBT for older adults. Not all older adults may initially be able to tolerate the required training dose of PBT, which may lead to anxiety or inability to physically cope with the perturbations [40]. Anxiety during training is a factor that was found to limit acceptability and increase drop-out rates, and thus limit the effectiveness of PBT [32]. A proposed method to improve both physical tolerability as well as acceptability is to progressively increase training intensity (e.g. perturbation magnitude or unexpectedness) in a manner that is tailored to the individual [26, 40, 43].
In this study, we evaluate the additive effects of a three-session PBT protocol [44] that was designed to address these previously identified challenges of PBT, in addition to usual care, on balance control and fear of falling in older adults with an increased risk of falling based on a recent fall incident.
Methods
Study design and participants
A detailed description of the full study protocol was previously published [44]. In this single-blinded randomised controlled trial (RCT) PBT was offered to community-dwelling older adults (≥ 65 years). Older adults were eligible to participate in the study if they had experienced a fall in the previous three months, had therefore visited the hospital outpatient clinic, and were able to walk without a walking aid for ≥ 15 min. Exclusion criteria were diagnosis of any disease or disorder that may affect the safety of training (e.g. osteoporosis, recent fracture or severe contusion of the lower extremities, back or shoulders, or severe cardiopulmonary disease), falls caused by actions of third parties or during exercise activities, falls due to syncope, and use of medication known to increase falls risk [45]. Potential participants were also excluded if they were unable to follow instructions due to cognitive problems, unable to provide written informed consent or to communicate in Dutch. The study intervention and measurements were conducted between March 2019 and August 2021 at the physiotherapy department of the Maastricht University Medical Center, The Netherlands. Study outcomes were measured at baseline and one week post-intervention. Ethics approval was obtained from the Medical Ethics Committee azM/UM (METC18-049, Maastricht University and Maastricht University Medical Center), and the study was conducted in accordance with the declaration of Helsinki. All participants provided written informed consent.
Interventions
Participants were randomised to receive PBT as an add-on to usual care versus usual care alone.
Usual care
Usual care consisted of physiotherapy referral by the medical doctor if indicated. As in usual clinical practice, it was ultimately up to the patient to decide whether or not to visit the physiotherapist. Both the content and duration of the physiotherapy treatment could vary based on the needs of each individual patient, and were decided by the medical specialist and physiotherapist in consultation with the patient. During study visits, the outcome assessor routinely monitored if and how often each participant had visited their physiotherapist, and what components (i.e., strength training, mobility exercises, balance exercises) were included in the physiotherapy treatment.
Perturbation-based balance training
Participants referred to the experimental group received usual care as described above, and three 30-minute sessions of PBT additionally. The PBT sessions were given once a week for three consecutive weeks using the Computer Assisted Rehabilitation Environment (CAREN, MOTEK Medical BV). The CAREN is a dual-belt treadmill embedded in a motion platform with 6 degrees of freedom. The treadmill and motion platform can both provide unexpected balance perturbations, such as unilateral treadmill belt accelerations or decelerations, and platform translations and rotations in various directions. This is combined with a 180-degree screen on which a virtual reality environment is projected to make training more immersive. Participants wear a safety harness during training sessions, preventing the knees from hitting the ground in case of an unsuccessful balance recovery.
Training procedures
The first training session on the CAREN started with a familiarization procedure, where the participant could get used to the system by walking on the treadmill in the virtual environment. Participants reported a numeric rating scale (NRS) score for how comfortable they felt when walking on the CAREN before and during familiarization (0; very uncomfortable to 10; fully comfortable). If a score of 7 or higher was reached, the familiarization procedure was deemed complete. This was expected to occur within 6–7 min [46].
After this, each participants’ comfortable walking speed was determined using a ramp protocol. Subjects started walking at 0.5 m/s and speed was gradually increased until the subject said ‘stop’ when their comfortable walking speed was reached. The participant then walked unperturbed at this speed for approximately one minute to check if any adjustments needed to be made. Due to the procedures for familiarization and determining the comfortable walking speed, the total duration of the first training session could be up to 40 min.
Consecutive sessions started with a warm-up during which the participant walked unperturbed on the treadmill at their comfortable speed (determined during the first session) for approximately 3 min and got readjusted to the system. Each training session consisted of three parts: gait adaptability, static and dynamic reactive balance control (of which details are given below). During training, participants were regularly asked to rate how challenging it was to maintain their balance on an NRS score (0–10; 0 = not challenging at all, 10 = unable to maintain balance). To ensure that the training was challenging but acceptable and tolerable for each participant, the aim was to train at a difficulty level between 6 and 9 (challenging to very challenging) on the NRS. Training progression was based on these NRS scores, and each participant’s ability to manage the perturbations. Training difficulty was progressed by increasing the perturbation intensity and walking speed. During the second and final training sessions, cognitive and motor dual tasks (e.g., counting backwards in steps of 7, hitting targets in the virtual environment) could also be added to increase training difficulty. Participants were aware that there would be ‘various challenges to their balance’ during the training, and were instructed to recover their balance and to try to continue walking. Participants were naïve to the timing and the order of perturbation types that would be applied. Training adherence (number of training sessions attended and completed, reasons for missed training sessions) was monitored throughout the study, and participants were encouraged to reschedule any missed training sessions.
Gait adaptability
Participants walked in a virtual environment of a path through a forest, with various slopes and turns. Both the incline/decline of the slopes and the sharpness of the turns had a standardised starting level of 20% (out of 100%), which was then progressed in steps of 5–15%. Each 5% increase in difficulty level means an increase in the incline, decline and rotation of 0.5 degrees.
Static reactive balance
Participants stood on the CAREN while the platform and treadmill belts provided sudden perturbations. The platform could shift (move in the horizontal plane) or tilt (move into a sloping position) to anterior, posterior, left and right. The treadmill belt could unilaterally accelerate from standstill. In the second and third parts of the first training session, training difficulty started at the lowest difficulty level for each participant and could be progressed individually over 7 difficulty levels. Details on perturbation characteristics for each difficulty level were published previously [44].
Dynamic reactive balance
Participants walked on the treadmill at their comfortable walking speed, while the above-mentioned platform and treadmill perturbations were applied. The treadmill perturbations consisted of unilaterally accelerating or decelerating the treadmill belt for short periods of time (0.2–0.7 s).
Measurements
Study outcomes were measured at baseline (T0) and after 4 weeks, which was one week after the final training session for the PBT group (T1), by an outcome assessor who was blinded to treatment allocation. Demographic data (age in years, sex, body height (cm) and weight (kg)) was collected at baseline, including retrospective falls incidence over the previous 12 months. A fall was defined as ‘an event which results in a person coming to rest inadvertently on the ground or floor or lower level’ [47]. An adapted version of the ‘falls history questionnaire’ as presented in the book ‘Falls in older people: risk factors and strategies for prevention’ was used [48]. This questionnaire records if a fall has occurred in the previous 12 months, where it has happened, what the perceived cause was, and if and what kind of injuries were sustained. The outcome assessor filled in this questionnaire together with the subject to make sure that the recorded data was as comprehensive and clear as possible. Adherence to training in the PBT group was defined as attendance to the training session and completion of at least two out of three training parts.
Balance control
The main outcome in this study was balance control, assessed on the Mini-BESTest. The Mini-BESTest is a comprehensive measurement tool to assess balance in community-dwelling older adults [49]. The test is divided into four categories: anticipatory balance control (0–6 points), reactive balance control (0–6 points), sensory orientation (0–6 points) and dynamic gait (0–10 points). There are a total of 14 tasks which are scored on a three-point scale (0–2), with a total score ranging between 0 and 28 points. A higher score corresponds with better balance control. The Mini-BESTest has good reliability and validity, and a significantly smaller ceiling effect in community-dwelling older adults compared to the BBS [50, 51]. The minimal detectable change (MDC) at the 95% confidence level is 3–4 points [52,53,54]. In a study by Magnani et al., age-dependent cut-off values were determined, where scoring below a certain value was associated with an increased risk of falling in the next 6 months (area under the ROC curve 0.68–0.79); <25 points for people 60 to 69 year of age, < 23 points for 70 to 79 years, < 22 points for 80 to 89 years and < 17 points for 90 years and older [55].
Fear of falling
Fear of falling was measured with the Falls Efficacy Scale International (FES-I, Dutch version). This version of the falls efficacy scale is a 16-item questionnaire developed to determine if a person has confidence in their ability to perform a range of daily activities without falling. It has been adapted to be more suited to older adults, including a range of activities from very basic to more complex [56]. The questionnaire will be filled in by the subject with the help of the outcome assessor. Sixteen items are scored on a four-point (1–4) scale, with a maximum score of 64 points. A higher score corresponds with a greater fear of falling. Cut-off points of 16–22 points for ‘low concern’ and 23–64 points for ‘high concern’ about falling have been described [57]. The Dutch version of the FES-I has good reliability and validity and discriminative power in older adults [56,57,58,59].
Sample size and randomisation
Sample size was calculated in G*power 3.1.9.2 and was based on the primary outcome of this study, difference between group means on balance measured with the Mini-BESTest post-intervention. The effect size d (0.61) was calculated based on values from an article with a similar study population and an intervention aimed at improving dynamic balance control [52]. We assumed that changes from baseline to post-intervention would be in the favour of the PBT group. Sample size was based on a one-tailed independent samples t-test, with an α of 0.05, power (1-β) of 0.80 and allocation ratio of 1. This resulted in a required sample size of n = 72. Accounting for an expected loss to follow-up of 10%, the final sample size is n = 80. Sample size was estimated conservatively, making no assumptions about the correlation between predictors (group allocation and baseline score) added into the model and the outcome variable.
Participants were randomised using a 1:1 ratio stratified block randomisation (block sizes 2 and 4). Randomisation was stratified based on sex (male/female) and number of falls during the previous year (1 versus 2 or more falls). The randomisation sequence was generated by an independent researcher using an online random number generator. Participants were enrolled and allocated to their groups by the main researcher. Allocation was concealed by using sequentially numbered, sealed opaque envelopes. The allocation sequence list was kept in a locked drawer, which could only be accessed by the principal investigator.
Statistical analysis
Descriptive statistics are presented as means and standard deviations (SD) or as medians and interquartile ranges (IQR), depending on the normality of the data. Categorical data is presented as frequencies (n) or percentages (%). Data was analysed on an intention-to-treat basis (missing data imputed using single stochastic regression imputation). Mann-Whitney U tests were used to determine if there was a significant between-group difference in Mini-BESTest or FES-I score change between baseline and follow-up (ΔMini-BESTest or ΔFES-I, respectively). To compare proportions or percentages between groups, the chi-square test was used. A multiple regression analysis was performed to explore potential confounding variables in the association between group and ΔMini-BESTest. Variables (age, sex, previous falls, FES-I at baseline, if the participant visited a physiotherapist and if their treatment included gait/balance training between baseline and post-intervention) were added (enter method) to the model, and variables that resulted in a ≥ 10% change in the regression coefficient of the main determinant were eligible for inclusion in the model. The variable contributing the most (≥ 10%) was included in the model first, and this process was repeated for each following variable until there were no more potential confounding factors [60]. In all analyses, statistical significance was set at p < 0.05. Data was analysed using the Statistical Package for the Social Sciences version 23.0 (SPSS, Chicago, Ill., USA).
Results
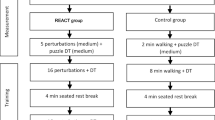
Between March 27th, 2019 and July 8th, 2021, 82 participants were included, of which 39 were randomly assigned to the PBT group (8 men, 31 women) and 43 to the control group (9 men, 34 women). The median age of the participants was 73 years (IQR 8 years). Some 49 participants experienced 1 fall during the previous year, 19 participants had fallen twice and 14 participants had fallen 3 or more times. No significant between-group differences in demographics and baseline characteristics of the participants were found (see Table 1). Six participants withdrew from the study; 2 (PBT group) due to restrictions related to the COVID-19 pandemic, 2 due to personal reasons (control group) and 2 no longer wanted to participate when they were randomised to the control group. Mini-BESTest values of five more participants (2 control and 3 PBT) are missing due to restrictions related to the COVID-19 pandemic. Figure 1 gives an overview of the flow of participants from eligibility assessment to each stage of the study.
CONSORT flow-diagram of participants. Overview of participant flow from inclusion to the final measurements, including reasons for non-inclusion or drop-outs. PBT = perturbation-based balance training. Mini-BESTest = Mini Balance Evaluation Systems Test. FES-I = Falls Efficacy Scale International. Not necessary = participant did not think they needed an intervention. Travel = participant did not want to participate due to travel issues. Burden = participant considered the time investment too high (often in combination with other treatment appointments). PBT-specific = two participants did not wish to participate for reasons related to the PBT training, specifically the safety harness. COVID-19 related = participants did not wish to participate due to the COVID-19 pandemic.
Training characteristics
Adherence to the training was 93.7% over all training sessions (104 out of 111 total scheduled sessions), of which 100 sessions were fully completed. Of the 37 participants who started PBT training, 31 (83.8%) attended all three training sessions. Six participants missed one or two training sessions, due to co-morbidities (n = 3), scheduling issues (n = 2) or feeling that their balance was too good for the training (n = 1). One participant reported a training-related adverse event of experiencing knee pain after making a misstep during the training session, which resolved without intervention within two days after the training session. Perturbation difficulty level was progressed individually, aiming to train at an NRS score of 6–9, representing the subjective experience of how challenging the perturbations were for each participant on a scale of 0 (not challenging) to 10 (unable to maintain balance). Progressing to higher perturbation difficulty levels (levels ranging from 1 (smallest perturbations) to 7 (largest perturbations)) based on this score, enabled the therapists to individualize training progression for each participant. By the end of the first session, participants on average reached perturbation difficulty levels 4 (range 2–6) and 2 (range 1–5) for standing and walking perturbations respectively (7 being the highest difficulty level). By the end of the third training session, participants on average reached level 6 (range 3–7) for standing perturbations and level 4 (range 2–7) for walking perturbations.
Assumptions
All assumptions for statistical tests were met. An analysis of standard residuals showed that the data contained one outlier on the Mini-BESTest at T1. As this score accurately reflected the performance measured for this participant, this value was not removed from the analysis.
Outcomes
Table 2 shows outcomes at baseline (T0) and post-intervention (T1) for both groups. Mini-BESTest scores at T0 and T1 are presented in Fig. 2. Baseline Mini-BESTest scores were 23 (4) points in both groups, baseline FES-I scores were 20 (8) and 20 (7) points for the control group and PBT group, respectively (median (IQR)). Median Mini-BESTest scores increased in both groups, however these change scores were not significantly different between groups (p = 0.87). No significant between-group difference in FES-I change scores was found (p = 0.85).
Multiple regression analysis was performed to explore and correct for potential interacting or confounding variables (age, sex, previous falls, FES-I at baseline, physiotherapy T0-T1 and Gait/Balance training T0-T1) in the association between group and ΔMini-BESTest, and between group and ΔFES-I. This analysis revealed that there was a significant interaction effect of age and receiving physiotherapy on the association between group and change in Mini-BESTest. Age also acted as a confounder in the relationship between group and change in FES-I. Adding these variables to the models did not result in a significant association in either model. Full regression analysis results and tables are reported in Additional file 1.
Discussion
This study evaluated the effects of a PBT protocol in addition to usual care on balance control and fear of falling in older adults with a recent history of falls. We hypothesised that the PBT group would show greater improvements compared to the control group. While median Mini-BESTest scores increased slightly in both groups, these changes were below the threshold for minimal detectable change and were not significantly different between groups. Median falls efficacy scores decreased by one point in the PBT group but not in the control group, and no significant between-group differences were found. Explorative secondary analysis revealed interactive effects of age and receiving physiotherapy on the association between group and ΔMini-BESTest, while age acted as a confounding variable on the association between group and ΔFES-I. Correction for confounding variables strengthened both associations but did not lead to a significant association with group in either.
The findings of this study do not support our hypothesis that balance control measured with the Mini-BESTest would improve significantly in the PBT group compared to the control group. Similar conclusions were drawn by recent studies comparing the effects of PBT to general balance training or multimodal physiotherapy on clinical measures of balance control (BBS, Timed Up and Go, and Dynamic Gait Index) in healthy community-dwelling older adults [61, 62]. As all participants in the present study had recently experienced one or more fall incidents, we expected that this would be reflected in their baseline values for balance control [11]. However, Mini-BESTest scores at baseline were already high, and based on these scores only approximately half (50 − 57%) of the participants were considered at increased risk for falls [55]. To our knowledge, the only studies that found significantly greater improvements in clinical measures of balance control after PBT compared to other interventions included populations with neurological conditions such as Parkinson’s disease, with notably lower scores at baseline [34, 35]. The results of this study, in line with recent literature in healthy community-dwelling older adults, did not show a significant additional effect of PBT to usual care on clinical measures of balance control in community-dwelling older adults who visit a hospital outpatient clinic due to a fall. The high Mini-BESTest scores at baseline could indicate that this outcome measure may not be sufficiently sensitive to changes in balance control in relatively healthy community-dwelling older adults. Thus, while studies have indicated that the Mini-BESTest can be useful to evaluate effects of PBT in populations with more impaired balance control, a potential avenue for future research may be to explore which clinical measures of balance control are suitable to evaluate the effects of PBT in this population.
Transfer of training adaptations to other tasks or contexts is an important challenge of PBT. Studies have shown that transfer of training adaptations can be achieved, but so far only to different conditions for a similar task. For example, studies have found transfer of PBT training adaptations after slip-perturbations on a low-friction moveable platform to a slippery floor [63], or from a treadmill to an overground surface [42], and interlimb transfer of training adaptations in the same perturbation type and context [64]. Therefore, the training protocol in the current study was designed with the aim to facilitate transfer of training adaptations by including a broader range of perturbation types and directions. However, despite each participant being able to progress to higher perturbation levels during training, this did not transfer to significant changes in overall balance control or balance recovery from lean-and-release perturbations in the reactive balance sub score measured with the Mini-BESTest. These results imply that the application of multiple perturbation types and directions in a three-session PBT protocol may not be sufficient to generate meaningful transfer to clinical measures of balance control in community-dwelling older adults with a recent history of falls. However, as development and optimization of PBT interventions are still emerging research topics, the implications of these findings for transfer of PBT training adaptations should be interpreted cautiously. For one, it should be considered which outcome measures are most suitable to measure training effects on balance control. While a clinical measure of balance control such as the Mini-BESTest may be more feasible to use in clinical practice, more subtle changes after balance training may be more accurately measured by instrumented measures (such as postural sway or gait parameters), as was demonstrated in a recent study by Hasegawa et al. [65]. More research is needed to determine which outcome measures are sufficiently sensitive to changes in balance control after training, and how they correlate with meaningful changes in balance control for everyday life.
Additionally, while studies have shown promising beneficial effects of PBT with a single or few training sessions [26, 37, 38], there are no strong guidelines on how to modulate training load to attain an optimal effect [66]. While the training dose in this study was based on a previous literature review [67], it should be considered that a higher training dose might be required to elicit adaptations on balance control that can be measured with a clinical balance test such as the Mini-BESTest. More research is needed to elucidate the training dose-response relationship of PBT, also considering the effects of factors such as perturbation intensity (high versus low or progressive intensity), transferability and retention of training adaptations.
No significant between-group differences were found in change of fear of falling measured with the FES-I. Median values at baseline were classified as ‘low concern’ based on previously determined cut-off values, and stayed the same for the control group and decreased by one point for the PBT group [57]. These findings are in line with a previous study that found no significant group-by-time interaction effects on fear of falling after PBT [68].
The results of this study show high training adherence rates, one training-related adverse event, and that increasing training difficulty was possible for each participant, confirming the feasibility of this PBT protocol for participants. However, including participants in the study proved challenging. Figure 1 shows that approximately half of the potentially eligible older adults that were approached, declined to participate. This is comparable to the median inclusion rates of 48.5% in falls prevention interventions for older adults, reported by Nyman et al. [69]. The most prevalent reasons older adults mentioned were that despite their recent fall(s), they did not see themselves as needing falls prevention or balance training, or that the burden of five study visits (including three training sessions) was too high. These reasons are also comparable to common barriers to participation in falls prevention, while only 2 potential participants indicated that they did not wish to participate for reasons specifically related to the PBT [70].
Limitations
This study was not without limitations. Firstly, restrictions related to the COVID-19 pandemic meant that some adjustments had to be made to the treatment protocol. The inclusion criterion of having experienced a fall in the previous 3 months was broadened to the previous 6 months to increase inclusion rates and reach the required sample size after a period of lockdown measures. In retrospect, this was the case for a similar number of participants in the PBT and control groups, and if this was of significant influence this would be expected to be visible from the baseline participant characteristics. The same restrictions also meant that some of the follow-up FES-I measurements had to be done over the phone, this was the case for 2 and 3 participants in the PBT and control group, respectively. This data was collected by the same outcome assessor as the baseline measurements, and did not lead to any issues. Second, while common in intervention studies, participants and therapists in the intervention group were not blinded to group allocation. However, therapists providing usual care, outcome assessors and data analysers were blinded. Additionally, the measurements were performed by a blinded outcome assessor that encouraged all participants to give their best effort. A final limitation of this study is that no direct measures of balance control in response to perturbations were applied during training. While this was a conscious choice to enable participants to focus on their training experience, it also means that direct training effects cannot be analysed from this study.
Conclusions
Participation in a PBT program that includes multiple perturbation types and directions did not lead to significantly different effects than usual care on balance control measured with the Mini-BESTest in this population of community-dwelling older adults with a recent history of falls. Fear of falling measured with the FES-I did not change in either group. More research is needed to elucidate the training dose-response relationship of PBT, and how to modulate PBT training load to attain optimal and transferrable training adaptations. Additionally, further study is needed to explore which clinical outcomes are suitable to measure PBT training effects on balance control in community-dwelling older adults.
Data Availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PBT:
-
Perturbation-based balance training
- Mini-BESTest:
-
Mini balance evaluation systems test
- FES-I:
-
Falls efficacy scale international
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- BBS:
-
Berg balance scale
- RCT:
-
Randomised controlled trial
- CAREN:
-
Computer assisted rehabilitation environment
- NRS:
-
Numeric rating scale
- T0:
-
Measurement time, baseline
- T1:
-
Measurement time, post-intervention
- SD:
-
Standard deviation
- ΔMini-BESTest :
-
Change in Mini-BESTest
- ΔFES-I :
-
Change in FES-I
References
Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age and ageing. 1990;19(2):136–41.
Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Archives of physical medicine and rehabilitation. 2001;82(8):1050–6.
Christine Stam BB. Letsels 2019 Kerncijfers Letsel Informatie Systeem. Amsterdam: VeiligheidNL; 2020. Report No.: 854 v2.
Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. Journal of gerontology. 1994;49(3):M140-7.
Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. The journals of gerontology Series A, Biological sciences and medical sciences. 1998;53(2):M112-9.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61.
Stevens JA. Falls among older adults—risk factors and prevention strategies. Journal of Safety Research. 2005;36(4):409–11.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology (Cambridge, Mass). 2010;21(5):658–68.
Lusardi MM, Fritz S, Middleton A, Allison L, Wingood M, Phillips E, et al. Determining Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta-analysis Using Posttest Probability. Journal of geriatric physical therapy (2001). 2017;40(1):1–36.
Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age and ageing. 2008;37(1):19–24.
Chu L-W, Chiu AYY, Chi I. Impact of Falls on the Balance, Gait, and activities of Daily Living Functioning in Community-Dwelling Chinese older adults. The Journals of Gerontology: Series A. 2006;61(4):399–404.
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2019(1).
Lesinski M, Hortobágyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of Balance Training on Balance performance in healthy older adults: a systematic review and Meta-analysis. Sports medicine (Auckland, NZ). 2015;45(12):1721–38.
Ragnarsdóttir M. The Concept of Balance. Physiotherapy. 1996;82(6):368–75.
Berg K. Balance and its measure in the elderly: a review. Physiotherapy Canada. 1989;41(5):240–6.
Hulzinga F, de Rond V, Vandendoorent B, Gilat M, Ginis P, D’Cruz N, et al. Repeated gait perturbation training in Parkinson’s Disease and healthy older adults: a systematic review and Meta-analysis. Frontiers in Human Neuroscience. 2021;15(611).
Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age and ageing. 1997;26(4):261–8.
Grabiner MD, Bareither ML, Gatts S, Marone J, Troy KL. Task-specific training reduces trip-related fall risk in women. Medicine and science in sports and exercise. 2012;44(12):2410–4.
Frances E Huxham PAG, Aftab E Patla. Theoretical considerations in balance assessment. Australian Journal of Physiotherapy. 2001;47:89–100.
de Vreede PL, Samson MM, van Meeteren NL, Duursma SA, Verhaar HJ. Functional-task exercise versus resistance strength exercise to improve daily function in older women: a randomized, controlled trial. Journal of the American Geriatrics Society. 2005;53(1):2–10.
Faber MJ, Bosscher RJ, Chin APMJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Archives of physical medicine and rehabilitation. 2006;87(7):885–96.
Weerdesteyn V, Rijken H, Geurts AC, Smits-Engelsman BC, Mulder T, Duysens J. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology. 2006;52(3):131–41.
Mansfield A, Wong JS, Bryce J, Knorr S, Patterson KK. Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Physical therapy. 2015;95(5):700–9.
Okubo Y, Schoene D, Lord SR. Step training improves reaction time, gait and balance and reduces falls in older people: a systematic review and meta-analysis. British journal of sports medicine. 2017;51(7):586.
Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Archives of physical medicine and rehabilitation. 2010;91(3):452–9.
Okubo Y, Sturnieks DL, Brodie MA, Duran L, Lord SR. Effect of reactive balance training involving repeated slips and trips on Balance Recovery among older adults: a Blinded Randomized Controlled Trial. The journals of gerontology Series A, Biological sciences and medical sciences. 2019;74(9):1489–96.
Wang Y, Wang S, Bolton R, Kaur T, Bhatt T. Effects of task-specific obstacle-induced trip-perturbation training: proactive and reactive adaptation to reduce fall-risk in community-dwelling older adults. Aging clinical and experimental research. 2019.
Arampatzis A, Peper A, Bierbaum S. Exercise of mechanisms for dynamic stability control increases stability performance in the elderly. Journal of biomechanics. 2011;44(1):52–8.
Bieryla KA, Madigan ML. Proof of concept for perturbation-based balance training in older adults at a high risk for falls. Archives of physical medicine and rehabilitation. 2011;92(5):841–3.
Chien J-E, Hsu W-L. Effects of dynamic perturbation-based training on Balance Control of Community-Dwelling older adults. Scientific Reports. 2018;8(1):17231.
Mansfield A, Peters AL, Liu BA, Maki BE. Effect of a perturbation-based balance training program on compensatory stepping and grasping reactions in older adults: a randomized controlled trial. Physical therapy. 2010;90(4):476–91.
Okubo Y, Brodie MA, Sturnieks DL, Hicks C, Lord SR. A pilot study of reactive balance training using trips and slips with increasing unpredictability in young and older adults: biomechanical mechanisms, falls and clinical feasibility. Clinical biomechanics (Bristol, Avon). 2019;67:171–9.
Lurie JD, Zagaria AB, Pidgeon DM, Forman JL, Spratt KF. Pilot comparative effectiveness study of surface perturbation treadmill training to prevent falls in older adults. BMC geriatrics. 2013;13:49.
Shen X, Mak MK. Technology-assisted balance and gait training reduces falls in patients with Parkinson’s disease: a randomized controlled trial with 12-month follow-up. Neurorehabilitation and neural repair. 2015;29(2):103–11.
Smania N, Corato E, Tinazzi M, Stanzani C, Fiaschi A, Girardi P, et al. Effect of balance training on postural instability in patients with idiopathic Parkinson’s disease. Neurorehabilitation and neural repair. 2010;24(9):826–34.
Protas EJ, Mitchell K, Williams A, Qureshy H, Caroline K, Lai EC. Gait and step training to reduce falls in Parkinson’s disease. NeuroRehabilitation. 2005;20(3):183–90.
Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. The journals of gerontology Series A, Biological sciences and medical sciences. 2014;69(12):1586–94.
Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip-related falls by community-dwelling adults: a prospective study. Journal of the American Geriatrics Society. 2013;61(9):1629–31.
König M, Epro G, Seeley J, Potthast W, Karamanidis K. Retention and generalizability of balance recovery response adaptations from trip perturbations across the adult life span. J Neurophysiol. 2019;122(5):1884–93.
Karamanidis K, Epro G, McCrum C, König M. Improving trip- and slip-resisting skills in older people: perturbation dose matters. Exerc Sport Sci Rev. 2020;48(1):40–7.
Dijkstra BW, Horak FB, Kamsma YP, Peterson DS. Older adults can improve compensatory stepping with repeated postural perturbations. Front Aging Neurosci. 2015;7:201.
Wang Y, Bhatt T, Liu X, Wang S, Lee A, Wang E, et al. Can treadmill-slip perturbation training reduce immediate risk of over-ground-slip induced fall among community-dwelling older adults? Journal of biomechanics. 2019;84:58–66.
Harper SA, Beethe AZ, Dakin CJ, Bolton DAE. Promoting generalized learning in Balance Recovery Interventions. Brain Sciences. 2021;11(3).
Gerards MHG, Marcellis RGJ, Poeze M, Lenssen AF, Meijer K, de Bie RA. Perturbation-based balance training to improve balance control and reduce falls in older adults – study protocol for a randomized controlled trial. BMC geriatrics. 2021;21(1):9.
Vries de O. Medicatie en valincidenten bij ouderen: een meta-analyse. Ned Tijdschr Geneeskd. 2010;154(A1669).
Meyer C, Killeen T, Easthope CS, Curt A, Bolliger M, Linnebank M, et al. Familiarization with treadmill walking: how much is enough? Scientific Reports. 2019;9(1):5232.
Organization WH. WHO Global Report on Falls Prevention in older age. France: World Health Organization; 2007.
Lord SR SC, Menz HB. Falls in older people: risk factors and strategies for Prevention. Cambridge, UK: Cambridge University Press; 2001.
Yingyongyudha A, Saengsirisuwan V, Panichaporn W, Boonsinsukh R. The Mini-Balance Evaluation Systems Test (Mini-BESTest) Demonstrates Higher Accuracy in Identifying Older Adult Participants With History of Falls Than Do the BESTest, Berg Balance Scale, or Timed Up and Go Test. Journal of geriatric physical therapy (2001). 2016;39(2):64–70.
Bán B, Rugelj D, editors. A comparison of the ceiling effect between Berg Balance Scale and Mini-BESTest in a group of balance trained community-dwelling older adults2017.
Marques A, Almeida S, Carvalho J, Cruz J, Oliveira A, Jácome C. Reliability, validity, and ability to identify fall status of the balance evaluation Systems Test, Mini-Balance evaluation Systems Test, and brief-balance evaluation Systems Test in Older People living in the community. Archives of physical medicine and rehabilitation. 2016;97(12):2166-73.e1.
Anson E, Ma L, Meetam T, Thompson E, Rathore R, Dean V, et al. Trunk motion visual feedback during walking improves dynamic balance in older adults: Assessor blinded randomized controlled trial. Gait & posture. 2018;62:342–8.
Godi M, Franchignoni F, Caligari M, Giordano A, Turcato A, Nardone A. Comparison of reliability, validity, and responsiveness of the Mini-BESTest and Berg Balance Scale in patients with Balance Disorders. Physical therapy. 2012;93.
Tsang CSL, Liao L-R, Chung RCK, Pang MYC. Psychometric Properties of the mini-balance evaluation Systems Test (Mini-BESTest) in Community-Dwelling individuals with chronic stroke. Physical therapy. 2013;93(8):1102–15.
Magnani PE, Genovez MB, Porto JM, Zanellato NFG, Alvarenga IC, Freire RC, Jr., et al. Use of the BESTest and the Mini-BESTest for Fall Risk Prediction in Community-Dwelling Older Adults Between 60 and 102 Years of Age. Journal of geriatric physical therapy (2001). 2019.
Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age and ageing. 2005;34(6):614–9.
Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age and ageing. 2010;39(2):210–6.
Helbostad JL, Taraldsen K, Granbo R, Yardley L, Todd CJ, Sletvold O. Validation of the Falls Efficacy Scale-International in fall-prone older persons. Age and ageing. 2010;39(2):259.
Kempen GI, Todd CJ, Van Haastregt JC, Zijlstra GA, Beyer N, Freiberger E, et al. Cross-cultural validation of the Falls Efficacy Scale International (FES-I) in older people: results from Germany, the Netherlands and the UK were satisfactory. Disability and rehabilitation. 2007;29(2):155–62.
Twisk JWR. Inleiding in de toegepaste biostatistiek: reed business education; 2014.
Allin LJ, Brolinson PG, Beach BM, Kim S, Nussbaum MA, Roberto KA, et al. Perturbation-based balance training targeting both slip- and trip-induced falls among older adults: a randomized controlled trial. BMC geriatrics. 2020;20(1):205-.
Lurie JD, Zagaria AB, Ellis L, Pidgeon D, Gill-Body KM, Burke C, et al. Surface perturbation training to Prevent Falls in older adults: a highly pragmatic, randomized controlled trial. Physical therapy. 2020;100(7):1153–62.
Bhatt T, Pai YC. Generalization of gait adaptation for fall prevention: from moveable platform to slippery floor. J Neurophysiol. 2009;101(2):948–57.
McCrum C, Karamanidis K, Grevendonk L, Zijlstra W, Meijer K. Older adults demonstrate interlimb transfer of reactive gait adaptations to repeated unpredictable gait perturbations. Geroscience. 2020;42(1):39–49.
Hasegawa N, Shah VV, Harker G, Carlson-Kuhta P, Nutt JG, Lapidus JA, et al. Responsiveness of Objective vs. Clinical Balance Domain Outcomes for Exercise intervention in Parkinson’s Disease. Front Neurol. 2020;11:940-.
McCrum C, Bhatt T, Gerards M, Karamanidis K, Rogers M, Lord S, et al. Perturbation-Based Balance Training: Principles, Mechanisms and Implementation in Clinical Practice2022 02-09-2022.
Gerards MHG, McCrum C, Mansfield A, Meijer K. Perturbation-based balance training for falls reduction among older adults: current evidence and implications for clinical practice. Geriatrics & gerontology international. 2017;17(12):2294–303.
Kurz I, Gimmon Y, Shapiro A, Debi R, Snir Y, Melzer I. Unexpected perturbations training improves balance control and voluntary stepping times in older adults - a double blind randomized control trial. BMC geriatrics. 2016;16:58.
Nyman SR, Victor CR. Older people’s recruitment, sustained participation, and adherence to falls prevention interventions in institutional settings: a supplement to the Cochrane systematic review. Age and ageing. 2011;40(4):430–6.
Elskamp AB, Hartholt KA, Patka P, van Beeck EF, van der Cammen TJ. Why older people refuse to participate in falls prevention trials: a qualitative study. Exp Gerontol. 2012;47(4):342–5.
Acknowledgements
The authors would like to thank all research assistants who helped with the study measurements and data collection, and all involved doctors and nurses who helped inform potential participants about the study.
Funding
The authors received no specific funding for this research.
Author information
Authors and Affiliations
Contributions
All authors were involved in the design of the study protocol. MG is the coordinating researcher, the main writer of the manuscript, involved in the data collection and training of the intervention group. RM was a major contributor in writing the manuscript and data collection, and involved in training of the intervention group. RS provided input for the writing of the manuscript and was involved in training of the intervention group. MP provided input for the writing of the manuscript and was the study doctor. RdB, KM and AL supervised the study and provided input for writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Medical Ethics Committee azM/UM (METC18-049, Medical Ethics Committee of Maastricht University and Maastricht University Medical Center), and the study was conducted in accordance with the declaration of Helsinki. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gerards, M., Marcellis, R., Senden, R. et al. The effect of perturbation-based balance training on balance control and fear of falling in older adults: a single-blind randomised controlled trial. BMC Geriatr 23, 305 (2023). https://doi.org/10.1186/s12877-023-03988-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-03988-x