Abstract
Objective
The GERONTACCESS trial evaluated the utility and cost-effectiveness of a gerontological telemedicine (TLM) programme for preventing unplanned hospitalisation of residents living in nursing homes (NHs) in regions lacking medical facilities and/or qualified medical providers (“medical deserts”).
Design
GERONTACCESS was a 12-month, multicentre, prospective cluster-randomised trial conducted in NHs. The intervention group underwent TLM assessments every 3 months. The control group received the usual care. In both groups, comprehensive on-site assessments were conducted at baseline and the final visit. Care requirements were documented throughout the study.
Setting and participants
NH residents aged ≥ 60 years with multiple chronic diseases.
Methods
The study outcomes were the proportion of patients who experienced avoidable and unplanned hospitalisation, and the incremental cost savings per quality-adjusted life years from baseline to the 12-month follow-up.
Results
Of the 426 randomised participants (mean ± standard deviation age, 87.2 ± 7.6 years; 311 [73.0%] women), 23.4% in the intervention group and 32.5% in the control group experienced unplanned hospitalisation (odds ratio [OR] = 0.73, 95% confidence interval [CI] 0.43 to 0.97; p = 0.034). Each avoided hospitalisation in the intervention group saved $US 3,846.
Conclusions and implications
The results of GERONTACCESS revealed that our gerontological, preventative TLM program significantly reduced unplanned hospitalisations. This innovative intervention limited disease progression and promoted a healthy lifestyle among NH residents.
Trial registration
Clinicaltrials.gov, NCT02816177, registered June 28, 2016.
Similar content being viewed by others
Introduction
Populations are aging worldwide; the number of people aged over 80 years will increase threefold over the next three decades [1]. Elderly people may suffer from various combinations of geriatric syndromes, disabilities, and comorbidities. Nursing home (NH) residents are particularly likely to be transferred to an emergency department (ED), which is associated with adverse events, functional decline, and death [2,3,4,5]. Hospitalisation exposes frail residents to unnecessary health risks [6, 7]. Moreover, as many as two-thirds of nursing transfers to the hospital may be avoidable [8]. One major reason for unnecessary hospital transfers is the lack of qualified physicians and advanced practice providers available to guide medical care and advance care planning in residents living NHs [9].
One motivation for improved telehealth to NHs: is if hospitalisations were reduced, then, total system cost would be reduced through preventing the most expensive service, hospitalisations. Telemedicine (TLM) provides greater access to specialist care [10]. Many studies have demonstrated the utility of TLM for monitoring chronic conditions [11], dermatological issues [12], dental health [13], and geriatric health problems [14, 15]. The GERONTACCESS primary aim was to improve care plans and prevent development of geriatric syndromes and chronic diseases decompensation in order to reduce hospital transfers. The Comprehensive Geriatric Assessment (CGA), as a validated tool, improves the outcomes of older adults [16, 17]. Our systematic, preventative geriatric TLM assessment program (GTLM) with a follow-up component provided geriatric care expertise to NHs lacking resident geriatricians. The primary objective of the GERONTACCESS study was to evaluate the utility and cost-effectiveness of a 12-month GTLM program for reducing unplanned hospitalisation of residents of NHs with limited access to geriatric expertise.
Methods
Study design and population
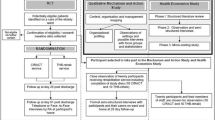
The GERONTACCESS study, Clinicaltrials.gov, NCT02816177, registered 28/06/2016, was a prospective, multicentre, cluster-randomised, open-label trial with a control arm (usual care) and an interventional arm (GTLM program) conducted from July 2016 to January 2018 in Nouvelle Aquitaine area, France. The unit of randomisation was the NH. NHs in the intervention group implemented the GTLM program for management of multiple chronic conditions, whereas NHs in the control group managed these conditions via usual care. Nine of the twelve initially selected non-profit NHs were finally included in medical desert areas (average capacity was 77 residents (min 60, max 111)). No geriatrician was present onsite. There were four NHs in the intervention group and five in the control group. All participants have been admitted for long-term care accommodation, they were aged 60 years and over; and had at least two chronic diseases. The inclusion and follow-up procedures are shown in Fig. 1. Written informed consent was obtained from all participants or their legal representatives.
Intervention
Telemedicine for the intervention group
The NHs in the intervention group received funding from the France Public Health Ministry to equip themselves with telemedicine tools as part of this experiment to optimize access to care. In accordance with French law, we used the secure TELEmedicine Aquitaine (TELEA) platform, which is specifically for the Nouvelle-Aquitaine region. TELEA ensures the security of patient and nurse data, and stores all informed consent forms and clinical files. A geriatrician can write a TLM report using the TELEA platform and send it via a secure messaging system to a physician. The equipment used during the GERONTACCESS study included a videoconferencing system, high-resolution camera (to aid wound care), mobile camera (to record residents as they walked around a room), stethoscope, electrocardiograph, and combined otoscope/dermatoscope.
Intervention
The intervention involved an initial teleconsultation within 10 days of inclusion. During this first teleconsultation a care plan was agreed upon by the resident, geriatrician, and NH staff and sent to attending physician. Three follow-up preventative teleconsultations were performed at 3, 6, and 9 months later with a mini-CGA to screen the geriatric syndromes and readjust the care plan as necessary. Teleconsultation were mostly conducted in early afternoon and they lasted 15 to 30 min. If necessary, the following connected devices were used. The stethoscope for a cardiac auscultation, a camera for the oral examination and sometimes the 'EKG' for an electrocardiogram for the follow-up of coronary disease or cardiac rhythm or conduction disorders. These examinations aim to limit avoidable non-programmed hospitalisations by avoiding decompensation of comorbidities. Unplanned teleconsultations could be requested by NH staff at any time. All treating physicians were at liberty to disregard the geriatrician’s advice.
Control group
In the control NHs, residents received the usual physician care.
Outcome measures and data collection
The primary outcome was the proportion of residents experiencing unplanned hospitalisation (defined as hospitalisation due to degeneration of a condition identified at baseline, or an emergency department admission followed by hospitalisation) during the 12-month study period. The secondary endpoint (both arms) was the number of unplanned hospitalisations (medical or surgical) during the same period. A face-to-face evaluation using the CGA was performed by the geriatrician of the mobile team at baseline and 12 months thereafter. Medico-economic data were collected every month.
Economic evaluation
Only direct costs were assessed (as recommended by the French National Authority for Health [HAS]) [18]. The calculation method, data sources, and expenses incurred by the health insurance provider and healthcare system are shown in Tables 1 and 2. Costs and programme utility were evaluated over 1 year, and an incremental cost-effectiveness ratio (ICER) was calculated. Bootstrapping was used to quantify variability among the costs and outcomes. Furthermore, 1,000 matched estimates of the average incremental costs and outcomes in each group were plotted on a cost-effectiveness plane.
Sample size
We performed a superiority test; based on an alpha risk of 5%, beta risk of 10%, estimated annual hospital admission incidence of 30% [19], and 25% reduction in the risk of admission, a minimum of 388 subjects (194 per group) were required. We added a 10% margin to account for non-evaluable subjects; thus, 428 subjects were needed (214 per group). All calculations were performed using nQuery Advisor ver. 7.0 software.
Statistical analysis
Data are presented as mean ± standard deviation (SD) or percentages, as appropriate. We used linear mixed regression models to compare quantitative outcome variables. Logistic models were used if the outcomes were binary, using patient as a fixed effect and NH as a random effect. Changes in utility were compared by analysis of covariance (ANCOVA), adjusting for the baseline and mean scores for each NH. The level of significance was set to 5%, and all analyses were performed on an intention-to-treat basis. R software (R Development Core Team, Vienna, Austria) was used for the data analysis.
Results
Of the 426 patients (Figs. 1 and 2), 214 and 212 were assigned to the intervention and control groups, respectively; 53 (25%) and 50 (24%), respectively, had been hospitalised the year before inclusion. Among the patients for whom the cost of care was evaluated, 73% were female (mean age, 87 years). Patient baseline characteristics are shown in Table 1. In terms of health insurance costs, the average total in the intervention group was $US 1,900 ± 3,040 and $US 2,250 ± 3,450 in the control group (p = 0.27). The total costs included consultations/teleconsultations, emergency department admissions followed by a hospitalisation and/or unplanned hospitalisations, and transportation costs. The mean number of consultations by a referring physician was 16.4 ± 6.94 in the intervention group and 15.1 ± 5.55 in the control group (p = 0.04). In the intervention group, 631 teleconsultations were performed during the scheduled TLM visits. Very few unscheduled teleconsultations were conducted: 2 with geriatrician and 8 with other specialists (dermalogist, psychiatrician and psychogeriatrian). The average number of TLM procedures in the intervention group was 3 ± 1.02. In terms of hospitalisation, 14% of the intervention group and 10% of the control group were admitted to emergency department without hospitalisation during the follow-up period (p = 0.314).
Effectiveness analysis
The proportion of unplanned hospitalisations was 23.4% (50 residents) in the intervention group and 32.5% (69 residents) in the control group (odds ratio = 0.73; 95% confidence interval [CI] 0.43 to 0.97; p = 0.034). During the 12-month follow-up, 61 unplanned hospitalisations occurred in the intervention group versus 93 in the control group. The mean number of theses unplanned hospitalisations was 0.285 ± 0.563 in the intervention group and 0.443 ± 0.78 in the control group; the difference of 0.158 was not significant (p = 0.17). The mean number of consultations/patients during the study was 16.4 ± 6.94 in the intervention group and 15.1 ± 5.55 in the control group. Forty (19%) deaths occurred in the intervention group, compared to forty-three (20%) in the control group (p = 0.68).
Cost-effectiveness
The incremental cost saving was $3,846 for each avoided hospitalisation in the intervention group (Tables 3 and 4). The scatterplot of the 1,000 ICERs calculated during the bootstrap analysis, indicate that 86% of the points felt within the southwestern quadrant of the cost-effectiveness plane, i.e. the intervention was dominant (less costly and less unplanned hospitalization) (Fig. 3).
Discussion
We performed a trial to evaluate the utility and cost-effectiveness of a GTLM programme. The programme reduced the proportion of NH residents admitted to the hospital, but did not reduce the number of hospitalisations. Three important points for NH residents and policymakers emerged. First, the GTLM programme provides remote geriatric expertise. Although the CGA has been validated for use in routine geriatric care [20,21,22], we found that on-site administration of the CGA by a geriatrician was valuable. In contrast to assessments made prior to an emergency department transfer [23], the CGA was performed in the resident’s normal environment under stress-free conditions in this study. A holistic, personalized, and adaptable care plan was then initiated, in consultation with the NH staff tasked with implementing it. The subsequent teleconsultations evaluated geriatric syndromes every 3 months, thereby enhancing anticipatory care to help avoid unplanned hospitalisations caused by complications of chronic multimorbidities or the worsening of a condition. The proportion of residents who avoided unplanned hospitalisation was significantly greater in the intervention group even if some of them experienced multiple hospitalisations in intervention group. In this study, the rate of mortality was not significant between the two groups. Those results are similar to those observed in literature [24]. However, the GTLM programme increased general practitioner consultations and seemed to increase emergency department visits without hospitalisation probably linked to the excessive medicalization of residents. Then it was not designed to manage emergencies, and there was no significant group difference in emergency department admissions.
Due to the robustness of the study design, the evidence regarding the utility of GTLM can be considered strong. If TLM includes a primary care consultation, the likelihood of hospital transfer is reduced [25]. We found that each hospitalisation avoided in the intervention group saved Medicare costs in the amount of $US 3,846. This does not include investment in technology, because it is part of a systematic allocation that is now basically free to all NHs. The telemedicine has not generated any new costs and is included in the current care covered by the health insurance. Then, costs for technology solution for TLM acquisition has been depreciate since 2016: technology is three-fold cheaper today.
The GERONTACCESS study improved the healthcare management of NH residents with limited access to care, even though the programme included primary care visits. Geriatric prevention via TLM is less costly than degeneration of a chronic condition. By detecting early geriatric syndrome or decompensation of chronical diseases, the GTLM programme may be limits disease progression, reveals early signs of deterioration. Therefore, it should be favoured by policymakers.
Limitations
The cost-utility of the GERONTACCESS study was not significant at 12 months, unlike many other studies [26]; this could be explained by missing data on more than 20% of the EuroQol- 5 Dimension (EQ5D) questionnaires (in turn explained by 20% of the residents being cognitively impaired). In this study we observed a high number of general practitioner consultation probably due to a contamination bias. Although TLM enhances cooperation among healthcare professionals [27], the NH nurses needed support throughout the study to use the TLM technology; TLM requires resident NH healthcare professionals, but French NHs are notoriously understaffed [28, 29]. Finally, a sociological analysis would have been useful to explore practice changes made within the NHs, as well as changes in the relationships between NHs and remote geriatricians, and in the perceptions of residents, NH’staff, geriatricians, and residents’ families. Given the novelty of this sociotechnical approach, such changes are inevitable [30, 31]. Nevertheless, we have taken the first steps towards implementation of TLM, which is critical given that populations with poor access to geriatric services are projected to grow.
Availability of data and materials
The datasets analysed during the current study and the study protocol are available from the corresponding author on reasonable request.
References
World Health Organization. Aging and health. 2021.
Brucksch A, Hoffmann F, Allers K. Age and sex differences in emergency department visits of nursing home residents: a systematic review. BMC Geriatr. 2018;18(1):151.
Ingber MJ, Feng Z, Khatutsky G, Wang JM, Bercaw LE, Zheng NT, et al. Initiative to reduce avoidable hospitalizations among nursing facility residents shows promising results. Health Aff. 2017;36(3):441–50.
Cohen AB, Knobf MT, Fried TR. Avoiding hospitalizations from nursing homes for potentially burdensome care: results of a qualitative study. JAMA Intern Med. 2017;177(1):137.
Guion V, De Souto BP, Rolland Y. Nursing home residents’ functional trajectories and mortality after a transfer to the emergency department. J Am Med Dir Assoc. 2021;22(2):393-398.e3.
Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing. 2014;43(6):759–66.
Unroe KT, Hickman SE, Carnahan JL, Hass Z, Sachs G, Arling G. Investigating the avoidability of hospitalizations of long stay nursing home residents: Opportunities for improvement. Innov Aging. 2018;2(2):igy017. Available https://academic.oup.com/innovateage/article/doi/10.1093/geroni/igy017/5049201. Viewed 7 March 2022.
Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, et al. Potentially avoidable hospitalizations of nursing home residents: Frequency, causes, and costs: [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp 760–761]. Am Geriatr Soc. 2010;58(4):627–35.
Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev. 2008;65(1):3–39.
du Toit M, Malau-Aduli B, Vangaveti V, Sabesan S, Ray RA. Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: a systematic review. J Telemed Telecare. 2019;25(1):3–16.
Bashshur RL, Shannon GW, Smith BR, Alverson DC, Antoniotti N, Barsan WG, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed E Health. 2014;20(9):769–800.
Rizvi SMH, Schopf T, Sangha A, Ulvin K, Gjersvik P. Teledermatology in Norway using a mobile phone app. Houwink EJF, (ed.). PloS One. 2020;15(4):e0232131.
Queyroux A, Saricassapian B, Herzog D, Müller K, Herafa I, Ducoux D, et al. Accuracy of teledentistry for diagnosing dental pathology using direct examination as a gold standard: results of the tel-e-dent study of older adults living in nursing homes. J Am Med Dir Assoc. 2017;18(6):528–32.
Low JA, Toh HJ, Tan LLC, Chia JWK, Soek ATS. The nuts and bolts of utilizing telemedicine in nursing homes – the GeriCare@North experience. J Am Med Dir Assoc. 2020;21(8):1073–8.
Piau A, Nourhashemi F, De Mauléon A, Tchalla A, Vautier C, Vellas B, et al. Telemedicine for the management of neuropsychiatric symptoms in long-term care facilities: the DETECT study, methods of a cluster randomised controlled trial to assess feasibility. BMJ Open. 2018;8(6):e020982.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital. In: The Cochrane Collaboration, editor. Cochrane Database of Systematic Reviews. Chichester: John Wiley & Sons, Ltd; 2006. P. CD006211. Available at: https://doi.wiley.com/10.1002/14651858.CD006211. Viewed 9 Mar. 2022.
Ellis G, Marshall T, Ritchie C. Comprehensive geriatric assessment in the emergency department. Clin Interv Aging. 2014;24(9):2033–43.
HAS. Choices in methods for economic evaluation. 2020. Available at: https://www.has-sante.fr/upload/docs/application/pdf/2020-11/methodological_guidance_2020_-choices_in_methods_for_economic_evaluation.pdf.
Kirsebom M, Hedström M, Wadensten B, Pöder U. The frequency of and reasons for acute hospital transfers of older nursing home residents. Arch Gerontol Geriatr. 2014;58(1):115–20.
Chadborn NH, Goodman C, Zubair M, Sousa L, Gladman JRF, Dening T, et al. Role of comprehensive geriatric assessment in healthcare of older people in UK care homes: realist review. BMJ Open. 2019;9(4):e026921.
Pilotto A, Cella A, Pilotto A, Daragjati J, Veronese N, Musacchio C, et al. Three decades of comprehensive geriatric assessment: evidence coming from different healthcare settings and specific clinical conditions. J Am Med Dir Assoc. 2017;18(2):192.e1-192.e11.
Tchalla AE, Lachal F, Cardinaud N, Saulnier I, Rialle V, Preux P-M, et al. Preventing and managing indoor falls with home-based technologies in mild and moderate Alzheimer’s Disease patients: Pilot Study in a community dwelling. Dement Geriatr Cogn Disord. 2013;36(3–4):251–61.
Katz PR, Resnick B, Ouslander JG. Requiring on-site evaluation in the nursing home before hospital transfer: Is this proposed CMS rule change feasible and safe? J Am Med Dir Assoc. 2015;16(10):801–3.
Feng Z, Ingber MJ, Segelman M, Zheng NT, Wang JM, Vadnais A, et al. Nursing facilities can reduce avoidable hospitalizations without increasing mortality risk for residents. Health Aff. 2018;37(10):1640–6.
Morphet J, Innes K, Griffiths DL, Crawford K, Williams A. Resident transfers from aged care facilities to emergency departments: can they be avoided? Emerg Med Australas. 2015;27(5):412–8.
Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Aff. 2014;33(2):244–50.
Gillespie SM, Moser AL, Gokula M, Edmondson T, Rees J, Nelson D, et al. Standards for the use of telemedicine for evaluation and management of resident change of condition in the nursing home. J Am Med Dir Assoc. 2019;20(2):115–22.
Martin C, Ramos-Gorand M. High turnover among nursing staff in private nursing homes for dependent elderly people in France: impact of the local environment and the wage. Ecostat. 2017;(493). Available at: https://www.insee.fr/en/statistiques/2890090. Viewed 26 Feb. 2022.
Bazin M, Muller M. Le personnel et les difficultés de recrutement dans les Ehpad. DRESS; 2018. Available at: https://drees.solidarites-sante.gouv.fr/sites/default/files/er_1067.pdf
Piau A, Vautier C, De Mauleon A, Tchalla A, Rumeau P, Nourhashemi F, et al. Health workers perception on telemedicine in management of neuropsychiatric symptoms in long-term care facilities: two years follow-up. Geriatr Nurs. 2020;41(6):1000–5.
Stephens CE, Halifax E, David D, Bui N, Lee SJ, Shim J, et al. “They don’t trust us”: the influence of perceptions of inadequate nursing home care on emergency department transfers and the potential role for telehealth. Clin Nurs Res. 2020;29(3):157–68.
Acknowledgements
The authors thank all GERONTACCESS participants for their time, and the staff of the nine NHs (i.e. the directors, nurses, co-ordinating physicians, healthcare assistants, referral physicians, geriatricians, and clinical research staff). The authors also thank Alexandre André and Didier Gendronneau (DSI CHU Limoges), Sandra Juge and Abdel Bentaleb (DRI CHU Limoges), Dr Thaï Binh Nguyen, Dr Marie-Agnès Picat, Dr Thomas Mergans, Dr Patrick-Joël Kajeu, Dr Vincent Douzon, Dr Thomas Rochette, Dr Hervé Merveille, Dr Alain Blond, Professor Christophe Bedane, Professor Thierry Dantoine, Muriel Malichier, Florent Lachal, and Eric Maynard from the GIP ESEA group, and Patrick Malléa and Pierre-Emmanuel Buyse from the ACETIAM (NEHS) Group.
Funding
This research was supported by ARS Limousin Nouvelle Aquitaine, CHU de Limoges and “La Chaire d’Excellence Académique E-santé, bien Vieillir et Sutonomie” of the Fondation Partenariale de l’Université de Limoges.
Author information
Authors and Affiliations
Contributions
CG and AT drafted the manuscript. CG, AT, KZ, MM, IT, MLL, and PMP read and revised the manuscript. KZ, MM, CG, and AT assisted with the statistical analysis. CG, CLM, NC, and AT collected data. CG, AT, IT, IDZ, SL, and PMP helped formulate the study methodology and draft the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial received ethical approval from the local institutional review board (Comité de Protection des Personnes du Sud-ouest et Outre-mer IV) on the 15th of July, 2015. The French « Agence Nationale de Sécurité du Médicament et des Produits de Santé» was notified on the 16th of September, 2015. The trial was registered with ClinicalTrials.gov on the 28th of June, 2016 (NCT02816177). Patients or their legal representatives gave written informed consent. We confirm that all experiments were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
No author has any competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gayot, C., Laubarie-Mouret, C., Zarca, K. et al. Effectiveness and cost-effectiveness of a telemedicine programme for preventing unplanned hospitalisations of older adults living in nursing homes: the GERONTACCESS cluster randomized clinical trial. BMC Geriatr 22, 991 (2022). https://doi.org/10.1186/s12877-022-03575-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03575-6