Abstract
Background
Many patients following unicompartmental knee arthroplasty (UKA) also suffer from diabetes mellitus, which may lead to an increased likelihood of postoperative deep venous thrombosis (DVT). Therefore, we evaluated whether DVT incidence would increase 3 days following UKA in diabetic patients.
Methods
Patients who underwent UKA from August 2018 to September 2021 in our hospital were retrospectively included. Age, gender, body mass index, hypertension, mode of anesthesia, surgery time, intraoperative blood loss, tourniquet pressure and time, and glycosylated hemoglobin concentration were recorded as confounders. We compared the incidence and type of DVT between non-diabetic and diabetic patients and evaluated the effect of glycosylated hemoglobin levels on DVT.
Results
Of all the 224 patients, 96 had diabetes and 128 did not. Within 3 days after surgery, DVT occurred in 25 cases in the diabetic group and 17 cases in the non-diabetic group (p < 0.05), and the difference mainly exists in the lower limbs on the surgical side. Logistic regression analysis demonstrated that the risk of DVT in the diabetic group was 4.50 times higher compared with the non-diabetic group. For every 1 unit increase of glycosylated hemoglobin, the incidence of DVT increased 2.35 times. Differences in age, gender, body mass index, hypertension, mode of anesthesia, surgery time, intraoperative blood loss, tourniquet pressure, and time between the two groups were not significant.
Conclusions
The incidence of DVT in diabetic patients within 3 days after UKA was significantly higher than that in non-diabetic patients and was proportional to the concentration of glycosylated hemoglobin.
Similar content being viewed by others
Introduction
Orthopedic surgery, especially hip or knee arthroplasty, can remarkably increase the risk of hospital-acquired deep vein thrombosis (DVT) [1]. Even with prophylactic antithrombotic therapy, the incidence of DVT after total joint arthroplasty is close to 20% [2].
The occurrence of DVT is related to many aspects, such as gender, age, anesthetic mode, body mass index (BMI), heart disease, diabetes mellitus, active cancer, and so on [3]. The global population is entering an aging stage, followed by an increasing proportion of patients with diabetes in arthroplasties. Researchers have confirmed that when patients suffer from diabetes, their coagulation system [4], hemostatic system [5], and fibrinolysis [6] are abnormal, resulting in the procoagulant and thrombotic susceptibility, so diabetes may increase the risk of DVT [7, 8]. A retrospective study has shown that diabetic patients had a 2.71 times higher risk of postoperative DVT than that of non-diabetic patients following total knee arthroplasty (TKA) [9].
Unicompartmental knee arthroplasty (UKA) has become widely used in recent years. Compared with TKA, UKA is characterized by less trauma, short surgery time, and rapid postoperative recovery [10, 11]. These advantages may lead to a lower postoperative incidence of DVT in UKA than in TKA, making UKA the first choice of many doctors for end-stage unicompartmental knee osteoarthritis [12]. To our knowledge, the effect of diabetes on postoperative DVT has not been studied in UKA. Therefore, we performed a retrospective cohort study to compare the risk of DVT following UKA between diabetic and non-diabetic patients. The hypothesis is that diabetes increases the postoperative DVT risk in patients with UKA. And the risk is related to the glycosylated hemoglobin concentration.
Methods
Inclusion and exclusion criteria
This retrospective cohort study included the patients who underwent unilateral UKA with diagnosis of knee osteoarthritis from August 2018 to September 2021 in our hospital. We excluded patients who had infectious, gouty, or rheumatoid arthritis, DVT revealed by preoperative ultrasonography, previous history of DVT, or vascular surgery in lower extremities. Patients with coronary heart disease, arrhythmia, chronic heart failure, tumor history, long-term prophylactic use of anticoagulants such as aspirin, or severe postoperative complications were also excluded. The patients were assigned to the diabetes group and non-diabetes group, respectively.
Surgery technique
No prophylactic antithrombotic therapy was given before surgery. The anesthesiologist chose general or intraspinal anesthesia depending on the patient’s condition. A tourniquet was used from the beginning of the surgery until the prosthesis was fixed with bone cement, and the pressure of the tourniquet was generally set as systolic pressure plus 100 mmHg. The surgeries were performed with medial parapatellar approach incision, cemented Oxford phase III medial UKA prosthesis (two pegs; MP instrument; Biomet UK LTD, Waterton Industrial Estate, Bridgend CF31 3XS, UK), and cocktail injection (tranexamic acid 60 ml, parecoxib sodium 40 mg, epinephrine 0.15 ml, ropivacaine hydrochloride 20 ml:200 mg, oxycodone 10 ml:1 mg, injected into the joint capsule, synovium, subperiosteum, and subcutaneous tissues).
Postoperative management
No drainage was used after surgery. Ankle flexion and quadriceps muscle contraction exercises were required as early as possible. Full weight-bearing ambulation with crutches should be conducted four hours postoperatively. The lower extremity pneumatic circulation pump was used on the night of the surgery and was stopped the next morning. Diabetics controlled their fasting and postprandial blood glucose concentrations to 5-7 mmol/L and 8–10 mmol/L, respectively, by using long-acting insulin at bedtime and short-acting insulin before meals.
DVT diagnosis and treatment
To avoid the risk of early-stage bleeding, on the third day postoperatively, deep vein color Duplex sonography was performed and prophylactic or therapeutic dose of anticoagulant was used. Two experienced sonographers performed deep vein color Duplex sonography of lower extremities for all patients. If there was a solid echo in the lumen and after the probe was pressurized, the vascular lumen was not compressed, and no obvious blood flow signal was seen in Color Doppler flow imaging, it can be diagnosed as DVT. When the diagnosis results of the two sonographers were inconsistent, a unified final result will be given after consultation. Based on the ultrasound results, DVT was diagnosed and classified into distal (intermuscular vein thrombosis of the calf) and proximal (thrombosis in and above the popliteal vein) types, and then the therapeutic dose of low molecular weight heparin (LMWH; Enoxaparin Sodium Injection, 0.4 ml: 4,000 AxaIU) was given. Other patients without DVT underwent prophylactic anticoagulant therapy with LMWH (Enoxaparin Sodium Injection, 0.2 ml: 2,000 AxaIU) to prevent thrombosis. The patients received LMWH for 3–5 days in hospital and oral rivaroxaban for two weeks after discharge.
Statistical analysis
Demographics data included BMI, age, gender, surgery side, and concomitant disease. Recorded glycosylated hemoglobin value (normal value: 4%-6%), intraoperative tourniquet pressure and duration, and intraoperative blood loss.
t-test was used to compare continuous variables, and Pearson Chi-square test was used to compare counting variables. Logistic regression model was performed on the factors that may affect the incidence of DVT, and the odds ratio (OR) and its 95% confidence interval (CI) were calculated. To eliminate multicollinearity, diabetes and glycosylated hemoglobin were included in the regression model separately. Statistical packages R (The R Foundation; http://www.r-project.org; version 3.4.3) and Empower (R) (www.empowerstats.com, X&Y solutions, inc. Boston, Massachusetts) were used for analysis. If p-value < 0.05, the difference was considered significant.
Results
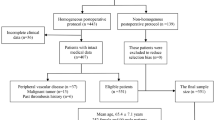
Two hundred eighty-eight patients underwent UKA from August 2018 to September 2021 in our hospital. Among them, 64 patients were excluded according to the exclusion criteria (2 patients of DVT showed by preoperative ultrasound, 1 patient of colon cancer history, 42 patients of coronary heart disease, 16 patients of long-term use of aspirin, and 3 patients of lower extremity surgery history). 25 of the 64 patients excluded had diabetes. A total of 224 patients were finally enrolled, 96 of whom had diabetes mellitus. No significant difference was observed between the two groups except for glycosylated hemoglobin (p < 0.001) and DVT (p < 0.05). Table 1 gives the characteristics of the study population.
On the third day after surgery, color Doppler ultrasound showed distal DVT in 42 patients. All DVTs were distal type and asymptomatic. The incidence of DVT in the diabetic group (26.0%) was higher than that in non-diabetic group (13.3%, p < 0.05). Among those with diabetes, 18 appeared in the ipsilateral leg, 4 in the contralateral leg, and 3 in the bilateral legs. Among those non-diabetic patients with DVT, 11 appeared in the ipsilateral leg, 5 in the contralateral leg, and 1 in bilateral legs. There was a significant difference in the incidence of DVT in the operative leg between the two groups (Fig. 1). After adjusting for BMI, age, hypertension, and some other confounding factors, multivariate logistic regression model showed that diabetes mellitus was a risk factor of DVT. Patients with diabetes had a 4.498 times greater risk of developing DVT than those without diabetes (Table 2). The distribution of glycosylated hemoglobin level of patients is shown in Table 3. Substituting the glycosylated hemoglobin value for diabetes and performing multiple regression analysis again, the results showed that the risk of developing DVT increased 2.351-fold (95% CI: 1.285–5.952, p< 0.05) for every unit of glycosylated hemoglobin increased.
Discussion
In this retrospective cohort study, we found that the incidence of DVT in early-stage after UKA was closely associated with diabetes, and was proportional to glycosylated hemoglobin levels.
DVT may cause pulmonary embolism (PE). The highest risk of symptomatic PE occurs within the first week postoperatively, with 81% occurring within three days after the surgery [13, 14]. Therefore, it is very important to prevent the occurrence of DVT and PE in the early stage after arthroplasty. DVT is caused by multiple factors, including BMI and increasing age, major surgery, congestive heart failure, arrhythmia, active cancer and, dyskinesia [15, 16]. Diabetes is also a potential risk factor for an increased incidence of DVT. Petrauskiene’s study found that after adjusting for age, the venous thromboembolism (VTE) risk in patients with diabetes was more than twice of that in non-diabetic people [7]. After further adjustment for race and gender, Tsai suggested that the risk of VTE at baseline in diabetic patients was 1.70 times higher compared with those who had normal fasting blood glucose (95% CI, 1.20–2.40) [17]. Retrospective analysis and prospective evaluation of renal transplants also showed that diabetes was remarkably related to VTE [8, 17, 18].
Our study found that patients with diabetes had a significantly higher incidence of DVT after UKA. UKA damages soft tissue and bone, leading to release of tissue factor that initiates the coagulation cascade [19]. Surgical trauma can also lead to vascular endothelial injury, promote thrombotic responses, and enhance blood coagulation [20]. Decreased mobility during postoperative recovery may cause venous stasis. When patients have diabetes mellitus, their hemodynamic abnormalities are aggravated. The platelet has higher adhesion levels and is more likely to aggregate [5]. Therefore, venous stasis, vascular endothelial dysfunction, and blood hypercoagulability under the combined effect of surgery attack and diabetes may exacerbate the development of DVT [21]. Intraoperative use of tourniquets hinders blood flow and aggravates blood stasis [22].This explains why the difference in the incidence of DVT mainly exists in the lower extremities on the surgical side. In addition, in our study, all DVTs were distal type. Some studies also found that the incidence of distal DVT after orthopedic surgery was significantly higher than that of the proximal [23, 24]. This may be related to the greater effect of tourniquet on venous blood stasis in distal limbs [25]. Asymptomatic distal DVT is generally considered to be self-limiting [26]. However, studies have found that when distal DVT is not treated effectively in time, the probability of distal DVT extending proximally is as high as 20% [27]. Proximal extension can lead to serious embolic complications, including PE. Therefore, asymptomatic distal DVT also requires attentive observation and effective prophylactics to prevent proximal extension of the thrombus. In our study, there was a small percentage of patients with contralateral or bilateral DVT after surgery in both diabetic group and non-diabetic group. Although the proportion is low, the surgeon should not ignore the possibility of postoperative DVT in the non-operative lower limbs.
A previous retrospective study of 358 knees showed that DVT incidence within 14 days after TKA in patients who had diabetes mellitus was 2.7 times higher compared with those without diabetes mellitus [9]. This is consistent with our results. Compared with TKA, both the surgery time of UKA and the interval between surgery and ambulation are much shorter. Thus, the duration of applying tourniquet, the amount of blood loss during surgery, and immobilization of the affected limb have less influence on the results, which resulted in the lower incidence of DVT in our study (18.8%) than that of TKA (55.3%) [9]. In addition, no patient had thrombosis-related symptoms such as lower extremity edema, severe pain, and dyspnea in our study. This is also the potential advantage of UKA.
Glycosylated hemoglobin reflects the average plasma glucose concentration over a period and is recommended for blood glucose control in those who had diabetes. Therefore, we further investigated quantitatively whether glycosylated hemoglobin levels in diabetic patients were associated with the incidence of DVT. The result showed that for every 1 unit increase in glycosylated hemoglobin, the risk of DVT increased by 2.351 times (95% CI: 1.285–5.952, p < 0.05). Therefore, when diabetic patients have poor glucose level control, the risk of DVT after surgery will increase sharply. However, the mechanism of glycosylated hemoglobin’s effect on macrovascular disease is not clear [28].
There are several limitations in our study. First, venography is the gold standard for diagnosing DVT, but its invasiveness and expensiveness limit its application. Color Doppler ultrasound is the most commonly-used preliminary screening method for DVT in clinical practice. A prospective clinical study comparing the accuracy of ultrasound versus venography for the diagnosis of DVT after TKA showed that the specificity and sensitivity of ultrasound were 63% and 87%, respectively, when venography results were used as a baseline reference. Therefore, as a non-invasive, safe, and convenient inspection method for DVT after arthroplasty, ultrasound is a reliable tool for preliminary screening of clinically suspected DVT [25]. Especially for proximal DVT, doppler ultrasonography provides good sensitivity (86%) and specificity (100%) [29]. The same patient was evaluated by two sonographers in our study, so the interference of ultrasound errors to the results can be ignored. Second, different types of diabetes may have different effects on DVT. However, since the admission records did not distinguish the type of diabetes, the influence of the type on DVT needs to be further studied. Third, different anesthetic methods exert different influences on hemodynamics, thus affecting the occurrence of postoperative DVT [30]. In our study, all patients received general or intraspinal anesthesia, and no significant difference was observed between them (p = 0.716). Additionally, the incidence of DVT was the highest in the first week following surgery [31]. However, patients who underwent UKA can be discharged from the hospital about five days after surgery due to the minimal trauma and rapid recovery, and VTE mainly occurs within three days after surgery [13, 14], so color Doppler ultrasound data were collected three days after surgery.
Conclusions
The risk of developing DVT in the early stage after UKA was significantly increased in the patients with diabetes mellitus. A higher level of glycosylated hemoglobin was related to a higher risk of DVT. It is hoped that a large-scale prospective population-based study in the future, including a detailed description of diabetes typing and glucose tolerance, will help to further clarify the relationship between diabetes and DVT.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DVT:
-
Deep vein thrombosis
- BMI:
-
Body mass index
- UKA:
-
Unicompartmental knee arthroplasty
- TKA:
-
Total knee arthroplasty
- PE:
-
Pulmonary embolism
- VTE:
-
Venous thromboembolism
References
Schindler OS, Dalziel R. Post-thrombotic syndrome after total hip or knee arthroplasty: incidence in patients with asymptomatic deep venous thrombosis. J Orthop Surg (Hong Kong). 2005;13:113–9.
Zhang H, Mao P, Wang C, Chen D, Xu Z, Shi D, Dai J, Yao Y, Jiang Q. Incidence and risk factors of deep vein thrombosis (DVT) after total hip or knee arthroplasty: a retrospective study with routinely applied venography. Blood Coagul Fibrinolysis. 2017;28:126–33.
Stubbs MJ, Mouyis M, Thomas M. Deep vein thrombosis. BMJ. 2018;360: k351.
Fuller JH, Keen H, Jarrett RJ, Omer T, Meade TW, Chakrabarti R, North WR, Stirling Y. Haemostatic variables associated with diabetes and its complications. Br Med J. 1979;2:964–6.
Mustard JF, Packham MA. Platelets and diabetes mellitus. N Engl J Med. 1977;297:1345–7.
Fearnley GR, Chakrabarti R, Avis PR. Blood fibrinolytic activity in diabetes mellitus and its bearing on ischaemic heart disease and obesity. Br Med J. 1963;1:921–3.
Petrauskiene V, Falk M, Waernbaum I, Norberg M, Eriksson JW. The risk of venous thromboembolism is markedly elevated in patients with diabetes. Diabetologia. 2005;48:1017–21.
Humar A, Johnson EM, Gillingham KJ, Sutherland DE, Payne WD, Dunn DL, Wrenshall LE, Najarian JS, Gruessner RW, Matas AJ. Venous thromboembolic complications after kidney and kidney-pancreas transplantation: a multivariate analysis. Transplantation. 1998;65:229–34.
Zhao Z, Wang S, Ma W, Kong G, Zhang S, Tang Y, Zhao Y. Diabetes mellitus increases the incidence of deep vein thrombosis after total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134:79–83.
Lombardi AJ, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res. 2009;467:1450–7.
Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della VC. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J ARTHROPLASTY. 2012;27:86–90.
Riddle DL, Jiranek WA, McGlynn FJ. Yearly incidence of unicompartmental knee arthroplasty in the United States. J ARTHROPLASTY. 2008;23:408–12.
Parvizi J, Huang R, Raphael IJ, Maltenfort MG, Arnold WV, Rothman RH. Timing of Symptomatic Pulmonary Embolism with Warfarin Following Arthroplasty. J ARTHROPLASTY. 2015;30:1050–3.
Granziera S, Cohen AT. VTE primary prevention, including hospitalised medical and orthopaedic surgical patients. Thromb Haemost. 2015;113:1216–23.
Heit JA, Spencer FA, White RH. The epidemiology of venous thromboembolism. J Thromb Thrombolysis. 2016;41:3–14.
Drouet L. Venous thromboembolic pathology. New acquired risk factors or new data on acquired risk factors. Arch Mal Coeur Vaiss. 2011;94:1318–26.
Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med. 2002;162:1182–9.
Bergqvist D, Bergentz SE, Bornmyr S, Husberg B, Konrad P, Ljungner H. Deep vein thrombosis after renal transplantation: a prospective analysis of frequency and risk factors. EUR SURG RES. 1985;17:69–74.
Deng W, Huo L, Yuan Q, Huang D, Li Q, Tian W. Risk factors for venous thromboembolism in patients with diabetes undergoing joint arthroplasty. BMC Musculoskelet Disord. 2021;22:608.
Badireddy M, Mudipalli VR. Deep Venous Thrombosis Prophylaxis. 2021 Aug 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 30521286.
Choi HK, Rho YH, Zhu Y, Cea-Soriano L, Avina-Zubieta JA, Zhang Y. The risk of pulmonary embolism and deep vein thrombosis in rheumatoid arthritis: a UK population-based outpatient cohort study. ANN RHEUM DIS. 2013;72:1182–7.
Mori N, Kimura S, Onodera T, Iwasaki N, Nakagawa I, Masuda T. Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: A prospective, randomized study. KNEE. 2016;23:887–9.
Harrison-Brown M, Scholes C, Douglas SL, Farah SB, Kerr D, Kohan L. Multimodal thromboprophylaxis in low-risk patients undergoing lower limb arthroplasty: A retrospective observational cohort analysis of 1400 patients with ultrasound screening. J Orthop Surg (Hong Kong). 2020;28:2309499020926790.
Kanchanabat B, Stapanavatr W, Meknavin S, Soorapanth C, Sumanasrethakul C, Kanchanasuttirak P. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg. 2011;98:1356–64.
Wang CJ, Huang CC, Yu PC, Chen HH. Diagnosis of deep venous thrombosis after total knee arthroplasty: a comparison of ultrasound and venography studies. Chang Gung Med J. 2004;27:16–21.
Li F, Wang X, Huang W, Ren W, Cheng J, Zhang M, Zhao Y. Risk factors associated with the occurrence of silent pulmonary embolism in patients with deep venous thrombosis of the lower limb. Phlebology. 2014;29:442–6.
Hughes MJ, Stein PD, Matta F. Silent pulmonary embolism in patients with distal deep venous thrombosis: systematic review. THROMB RES. 2014;134:1182–5.
Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, Golden SH. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. ANN INTERN MED. 2004;141:421–31.
Weinmann EE, Salzman EW. Deep-vein thrombosis. N Engl J Med. 1994;331:1630–41.
Zhou L.Y., Gu W., Liu Y, Ma Z.L. Effects of Inhalation Anesthesia vs. Total Intravenous Anesthesia (TIVA) vs. Spinal-Epidural Anesthesia on Deep Vein Thrombosis After Total Knee Arthroplasty. Med Sci Monit. 2018;24:67–75.
Saleh J, El-Othmani MM, Saleh KJ. Deep Vein Thrombosis and Pulmonary Embolism Considerations in Orthopedic Surgery. Orthop Clin North Am. 2017;48:127–35.
Acknowledgements
Not applicable
Funding
This work was supported by Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support, grant number: XMLX202139.
Author information
Authors and Affiliations
Contributions
XJ and ZL collated and analyzed all the data, and was major contributors in writing the manuscript. SA, JH and MF participated in the entire diagnosis, treatment and surgery of the cases, GC participated in the treatment of the cases and the article revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by ethics committee of Xuanwu Hospital Capital Medical University. All of the procedures were performed in accordance with the Declaration of Helsinki and relevant policies in China. Informed consent was obtained from all subjects whose data are used in this retrospective study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiao, X., Li, Z., An, S. et al. Does diabetes mellitus increase the incidence of early thrombosis in deep vein following unicompartmental knee arthroplasty: a retrospective cohort study. BMC Geriatr 22, 448 (2022). https://doi.org/10.1186/s12877-022-03153-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03153-w