Abstract
Background
Visual impairment frequently occurs amongst older people. Therefore, the aim of this study was to investigate the predictive value of visual impairment on functioning, quality of life and mortality in people aged 85 years.
Methods
From the Leiden 85-plus Study, 548 people aged 85 years were eligible for this study. Visual acuity was measured at baseline by Early Treatment Diabetic Retinopathy Study charts (ETDRS). According to the visual acuity (VA) three groups were made, defined as no (VA > 0.7), moderate (0.5 ≤ VA ≤ 0.7) or severe visual impairment (VA < 0.5). Quality of life, physical, cognitive, psychological and social functioning were measured annually for 5 years. For mortality, participants were followed until the age of 95.
Results
At baseline, participants with visual impairment scored lower on physical, cognitive, psychological and social functioning and quality of life (p < 0.001). Compared to participants with no visual impairment, participants with moderate and severe visual impairment had an accelerated deterioration in basic activities of daily living (respectively 0.27-point (p = 0.017) and 0.35 point (p = 0.018)). In addition, compared to participants with no visual impairment, the mortality risk was 1.83 (95% CI 1.43, 2.35) for participants with severe visual impairment.
Discussion
In very older adults, visual impairment predicts accelerated deterioration in physical functioning. In addition, severely visually impaired adults had an increased mortality risk. A pro-active attitude, focussing on preventing and treating visual impairment could possibly contribute to the improvement of physical independence, wellbeing and successful aging in very old age.
Similar content being viewed by others
Introduction
Worldwide, a total of 2.2 billion have impaired vision [1]. Prevalence and incidence are increasing with age. Aging is one of the major risk factors for vision loss followed by smoking [2]. Age-related macular degeneration is the leading cause of blindness, followed by diabetic retinopathy, glaucoma and cataract. For these diseases, effective strategies exist to delay or prevent the visual impairment or blindness from occurring [3]. However, in older people visual problems are frequently underreported, overlooked or dismissed. Consequently, the burden associated with diminished vision is significant [3, 4].
Visual impairment can affect daily functioning, social participation and cognitive state, highlighting the importance of improving health services to promote healthy aging [5,6,7,8]. Impaired vision is associated with an increased fall risk [9], comprised mobility [10], poorer quality of life [11], isolation often resulting in depression [12], cognitive dysfunction [13] and higher mortality rates [14]. However, the association between visual impairment and the changes in level of functioning in very old adults is still unknown.
Therefore, in this research the predictive value of visual impairment on functioning, quality of life and mortality was studied, based on the data from the Leiden 85-plus Study. Three hypotheses were tested for older people with visual impairment: (i) they have a lower level of functioning and quality of life at baseline, (ii) they deteriorate faster in functioning and quality of life and (iii) visual impairment is associated with higher mortality risk.
Materials and methods
Population characteristics
The Leiden 85-plus Study, an observational population-based prospective cohort study, examined health, functioning and well-being in very old adults. Included were all people from Leiden, the Netherlands, who turned 85 between 1 September 1997 and 1 September 1999. Details are specified in a previous study [15]. Participants were visited annually by a research nurse, at their current place of residence, for interviews and performance tests. Furthermore, the participants’ medical history was acquired from the general practitioner, pharmacy records and/or the nursing home physician. Common chronic diseases were included such as arthritis, obstructive pulmonary disease, cerebrovascular accident, myocardial infarction, Parkinson’s disease, malignancy and diabetes mellitus. Subsequently, there was a 5-year follow-up for morbidity and level of functioning. For mortality, participants were followed until 95 years of age. All participants gave informed consent. In the case of severe cognitive impairment, this consent was obtained from a guardian. Furthermore, the study was approved by the Medical Ethics Committee of the Leiden University Medical Centre.
Determinant
At baseline, visual acuity (VA) was assessed with objective measurements, using the Early Treatment Diabetic Retinopathy Study charts (ETDRS), at a distance of three meters for the left eye, the right eye and both eyes simultaneously. Participants were asked to wear their corrective glasses during the assessment. Visual acuity was reported on decimal scale. Participants with missing data were excluded. Participants were stratified into three groups at baseline. No visual impairment was defined as a visual acuity of more than 0.7, moderate visual impairment as a visual acuity from 0.5 to 0.7 and severe visual impairment as a visual acuity of less than 0.5 [16].
Outcomes
Functional status
All participants were followed for 5 years or until their death and their functional status was measured annually. Functional status was divided in four subcategories: (i) physical, (ii) cognitive (iii) psychological and (iv) social functioning.
Physical functioning
was assessed with the Groningen Activity Restriction Scale (GARS), a non-disease specific instrument to measure disability in basic activities of daily living (BADL) and instrumental activities of daily living (IADL) [17]. The GARS contains nine questions regarding BADL and nine questions regarding IADL [18]. The minimal score for both BADL and IADL is 9 and the maximal score is 36. A score of 9 represents optimal function. For participants who had severe cognitive impairment (Mini-Mental State Examination below 19), information was obtained from a proxy.
Cognitive functioning
was measured with the Mini-Mental State Examination (MMSE) with scores varying from 0 to 30 (30 = optimal cognitive function) [19].
Psychological functioning
was assessed by measuring depressive symptoms with the 15-item Geriatric Depression Scale (GDS-15), with a score from 0 to 15, in which higher scores indicated more depressive symptoms [20]. The GDS-15 was administered only in participants with a MMSE score > 18 points.
Social functioning
was quantified with the De Jong Gierveld Loneliness Scale (DJG), an 11-item questionnaire combining emotional loneliness (six items) and social loneliness (five items) specifically developed for use in older populations, with an outcome from 0 to 11 (0 = not lonely) [21] and was solely administered in participants with a MMSE score > 18 points.
Quality of life
Quality of life was assessed with the Cantril’s Ladder, a visual analogue scale on perceived quality of life, varying from 0 to 10 (10 = extremely satisfied) [22].
Mortality
Mortality data was obtained from municipal registry recorded between the start of the study and Feb. 1, 2008.
Statistical analysis
Differences in baseline characteristics between the groups according to visual impairment were analysed with the Linear by Linear Association for categorical variables and the Jonckheere-Terpstra Test for continuous variables. Prospectively, differences between changes in functional status and quality of life in these groups were estimated using linear mixed models and presented as (predicted) means with standard errors. The mixed models included a term for time, vision status (severe, moderate or no visual impairment) and a term for interaction between time and vision status. In subjects with no visual impairment, the effect of time on the level of functioning reflects the annual changes in functioning. The interaction between the functioning levels and time, in an individual with impaired vision, represents the additional annual change in functioning. The time till death was estimated using Kaplan Meier curves and compared using a log-rank test. Mortality hazard ratios (HR) and corresponding 95% confidence intervals (CI) were calculated in a Cox proportional hazards model.
As a sensitivity analysis different cut-off values for visual impairment were used. Primarily, participants were ranked in three equal groups according to 33% tertiles (high, medium and low vision). Additionally, participants were categorized in three groups following the International Classification of Diseases and Related Health Problems (ICD-10) guidelines, with a visual acuity below 0.33 defined as low vision and 0.5 or higher as normal vision [23]. Lastly, the cross-sectional correlation between vision and functioning was examined as the effect of a decrease per 0.1 point in vision on the level of functioning. Statistical analysis was executed with IBM SPSS statistics version 24.0.
Results
Study population
A total of 705 inhabitants were eligible for the study. Before enrolment in the Leiden 85-plus Study, 14 persons died and 92 declined to participate because of several reasons, such as no interest, no time, too nervous or anxious, too tired or ill or being against surveys in general [15]. Of the 599 subjects, 51 participants had no or an incomplete visual assessment due to severe illness or unknown reasons. The demographics of these participants were similar compared with the group with complete visual assessment, however, a history of cerebrovascular accident and severely cognitive impairment were present more often. Individuals with missing data were excluded from this study. Therefore, baseline data were available of 548 participants.
Baseline characteristics
Table 1 presents the baseline characteristics. At baseline, 215 (39.2%) participants had no visual impairment, 215 (39.2%) moderate visual impairment and 118 (21.5%) severe visual impairment. Participants with severe visual impairment were less often men (27.1 versus 31.6% for moderate impairment and 39.1% for no impairment, p trend = 0.021), less often living independently (71.2 versus 84.2% for moderate impairment and 91.6% for no impairment, p trend < 0.001) and less often having a high income (39.7 versus 48.4% for moderate impairment and 57.3% for no impairment, p trend = 0.002). Moreover, the prevalence of diabetes and severe cognitive impairment was higher in participants with severe visual impairment (respectively p trend = 0.006 and < 0.001). Arthritis and osteoarthritis are less prevalent in this group (24.6 versus 31.3% in moderate group and 38.8% in no impairment group, p trend = 0.007). Between the groups, there was no difference in fall history, however, hip fractures occurred significantly more in the severe visually impaired group (p trend = 0.005). The level of physical, cognitive, psychological and social functioning at baseline was significantly lower for the groups with moderate and severe visual impairment (all p trend < 0.001). Furthermore, a difference was found for quality of life when comparing the three groups (p trend < 0.001).
Changes in functional status and quality of life over time
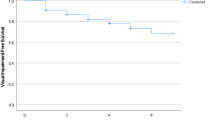
Table 2a describes the effect of visual impairment on the functional status and quality of life over time and results are visually represented in Fig. 1. Primarily, the basic annual change over time for the group with no visual impairment was determined in the linear mixed model analysis. A linear correlation was found between the level of functioning over time. For all variables this basic annual deterioration was statistically significant (at most p = 0.008). In participant with no visual impairment there was also an annual decrease in quality of life of 0.22 points on the Cantril’s Ladder (p < 0.001). Furthermore, compared to the participants with no visual impairment, the group with severe visual impairment had an additional annual deterioration in BADL of 0.35 points (p = 0.018, SE 0.146) and an additional annual change in quality of life of 0.12 points on the Cantril’s Ladder (p = 0.009,SE 0.048). In participants with moderate visual impairment an additional annual deterioration in BADL of 0.27 points was found (p = 0.017, SE 0.112) but not in quality of life. There was no significant additional annual change established for the other subcategories of functioning.
Effects of visual impairment on functional status and quality of life over time. Physical, cognitive and social functioning status were measured over time, during the 5 year follow-up period. Mean scores were compared for three groups according to the level of visual impairment. a Physical functioning: BADL. b Physical functioning: IADL. c Depression: GDS. d Cognition: MMSE. e Social functioning: DJG. f Quality of Life: Cantril
Table 2b and c illustrate the results of the in-depth analysis were participants were stratified according to their baseline level of functioning. Participants without physical impairment, were defined as a BADL score = 9 (n = 256), and participants with physical impairment, were defined as a BADL score > 9 (n = 291). Comparable to the overall analysis, a significant correlation was found between the level of functioning over time in both groups. In participants without physical impairment, an additional annual decline in quality of life of 0.14 points (p = 0.040, SE 0.068) was found for the people with severe visual impairment. For participants with physical impairment, a significant additional annual deterioration in BADL of 0.48 points (p = 0.007, SE 0.178) was found for the people with moderate visual impairment and of 0.41 points (p = 0.052, SE 0.209) for the people with severe visual impairment. This result was not observed in the group without physical impairment at baseline. In both groups, there were no other relevant significant additional annual change established for the other subcategories of functioning.
Sensitivity analysis
In our sensitivity analysis similar trends were found by using different cut-off values for visual impairment. Results are presented in Additional file 1.
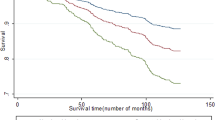
Mortality
The 10-year mortality risk increased from 1.21 (p = 0.089, 95% CI 0.97—1.50) in the group with moderate impaired vision to 1.83 (p < 0.001, 95% CI 1.43—2.35) in the group with severe impaired vision. The cumulative hazard ratios are depicted in Fig. 2.
Discussion
In this population-based study, the relation between visual impairment and physical, cognitive and social functioning, quality of life and mortality was investigated, using the data from the Leiden 85-plus Study. At baseline, in older persons aged 85 years, moderate and severe visual impairment was associated with lower levels of physical, cognitive, psychological and social functioning and a lower quality of life score. In the prospective analysis, overall the physical, cognitive and psychological functioning and the quality of life decreased over time. Visual impairment was related to an accelerated deterioration in BADL functioning over time. However, no correlation was found with IADL, cognitive, psychological or social functioning and quality of life. Moreover, the severe visual impaired group had an accelerated decline in BADL and a less decrease in quality of life over time. In addition, mortality risks were the highest in the group with severe visual impairment.
In accordance with previous research [24,25,26] an association was found between visual impairment and physical functioning in older people. Moreover, the effect of visual impairment on physical functioning was found to be independent of comorbidity and cognitive status [25]. In contrast to our research, studies reported that participants with visual impairment experienced more impairments with IADL activities compared to BADL activities, explained by the requirement to need better visual abilities for instrumental activities [24, 26]. In the present study, the accelerated deterioration solely found in BADL functioning, could be explained by the fact that the participants had already worse IADL functioning and could therefore not clearly change. In addition, another study [13] hypothesized the possible protective role of physical activity against visual impairment and they suggest that the level of physical functioning may be affected by visual impairment. This might explain the results from our in-depth analysis where we found an accelerated deterioration in BADL for the physically impaired group with visual impairment. Thus, visual impairment in combination with a physical impairment at baseline could be a possible predictor for accelerated deterioration in basic activities in daily living.
Moreover, in line with other research, visual impairment was associated with lower cognitive functioning and significantly higher levels of depression [27, 28]. An earlier study by Gussekloo et al. [16], with these data from the Leiden 85-plus Study, established that older people with visual impairment scored lower on visual cognitive tests, as a consequence of test problems due to their visual impairment. Additionally, in older people with lower cognitive function, the visual impairment could be overestimated because of less understanding of the instruction for the visual test. [16, 29].
Our results presented less decrease in quality of life in the severely visual impaired group. This result was also observed in our in-depth analysis for the people without physical impairment at baseline. Several studies showed that poor physical health, consequently visual impairment, among older people was hardly related to lower life satisfaction or social participation [5, 30, 31]. Visual impairment often results in anxiety and denial, which over the years decreases due to concepts as acceptance and adaption, influencing life satisfaction and thus quality of life [32]. It highlights the importance of the subjectively experienced well-being amongst older people. Increasing quality of life, obtained through adaptation, coping and acceptation, may be crucial to aging successfully [33]. A qualitative study by Haanes et al. [34] highlights the personal consequences caused by visual impairments in very old adults. Monitoring these people with visual impairment could be crucial to retain their independence and limit social isolation.
Consistent with other research [35], we have established a correlation between severe visual impairment and mortality. Visual impairment often goes hand in hand with more chronic diseases, a lower socio-economic status and an unhealthier lifestyle, all relating to a higher mortality [35].
The Cochrane review by Clarke et al. [3] indicated that visual screening did not improve vision in people aged 65 years or older, by referring them to suitable healthcare services. However, a systemic review by Nastasi [36] highlights the importance of future research to investigate the effects of interventions on visual status. Furthermore, research by van Nispen et al. [37] showed that basic ophthalmologic screening could help reduce the burden of visual impairment. Tan CS et al. [38] found that incentive-based intervention schemes increased compliance of attendance after community eye-screening. Thus, establishing the correlation between vision, functioning and mortality could be beneficial to increase the effectiveness of visual screening, by creating more awareness amongst the older people who are visually impaired [5].
The present study has several strengths. Primary, the population-based cohort had no exclusion criteria, an almost complete follow-up and a high response rate, enabling the generalisation of the conclusions to the overall elderly population. Secondly, multiple relevant endpoints, with repeated longitudinal measurements, were used for analysis, including functional status, quality of life and mortality. In addition, the growing aging population highlights the importance of clinical studies, specifically targeting the older population, to increase scientific evidence [36]. Moreover, a review study by Clarke et al. established that there is no difference between self-reported or identified vision problems by a vision test. Therefore, the standardised measurement of visual acuity was acknowledged as suitable screening tool [3]. A possible limitation of the present research is that only the results of the visual acuity were used for analysis, often resulting in an underestimation of visual impairment [36].
In conclusion, in very old adults, people with visual impairment are at risk for a lower level in physical, cognitive, psychological and social level of functioning. Moreover, visual impairment is associated with a reduced quality of life at baseline and the mortality risks are higher when severely visually impaired. In addition, visual impairment is a predictive factor for accelerated deterioration in physical functioning, mainly for activities in daily living. Highlighting this negative association could induce a pro-active attitude, focusing on preventing and treating visual impairment, possibly helping to improve physical independence, wellbeing and successful aging in very old age. However, more research is needed to establish this contribution.
Availability of data and materials
All authors had full access to the study data (including statistical reports and tables) and can take responsibility for the data integrity and the accuracy of the analysis. The datasets analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- VA:
-
Visual acuity
- ETDRS:
-
Early Treatment Diabetic Retinopathy Study charts
- GARS:
-
Groningen Activity Restriction Scale
- BADL:
-
Basic activities of daily living
- IADL:
-
Instrumental activities of daily living
- MMSE:
-
Mini-Mental State Examination
- DJG:
-
De Jong Gierveld Loneliness Scale
- QoL:
-
Quality of life, HR: hazard ratios
- CI:
-
Confidence intervals
- ICD-10:
-
International Classification of Diseases and Related Health Problems
References
World Health Organization. Blindness and vision impairment. 2021 http://www.who.int/mediacentre/factsheets/fs282/en/. Accessed 15 May 2021.
Wang WL, Chen N, Sheu MM, Wang JH, Hsu WL, Hu YJ. The prevalence and risk factors of visual impairment among elderly in Eastern Taiwan Koahsiung. J Med Sci. 2016;32(9):475–81.
Clarke EL, Evans JR, Smeeth L. Community screening for visual impairment in older people (Review). Cochrane Database Syst Rev. 2018;2:CD001054.
Van Houwelingen AH, Cameron ID, Gussekloo J, et al. Disability transitions in the oldest old in the general population. The Leiden 85-plus study. Age (Dordr). 2014;36(1):483–93.
Alma MA, Van der Mei SF, Groothoff JW, Suurmeijer TPBM. Determinants of social participation of visually impaired adults. Qual Life Res. 2012;21:87–97.
Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health. 2004;94(5):823–9.
Harrabi H, Kergoat MJ, Rousseau J, et al. Age-related eye disease and cognitive function. Invest Ophthalmol Vis Sci. 2015;56:1217–21.
Varin VK, Kergoat MJ, Belleville S, et al. Age-related eye disease and participation in cognitive activities. Sci Rep. 2017;7:17980.
Wood JM, Lacherez P, Black AA, Cole MH, Boon MY, Kerr GK. Risk of falls, injurious falls, and other injuries resulting from visual impairment among older adults with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52(8):5088–92.
Popescu ML, Boisjoly H, Schmaltz H, et al. Age-related eye disease and mobility limitations in older adults. Invest Ophthalmol Vis Sci. 2011;52(10):7168–74.
Chia EM, Wang JJ, Rochtchina E, Smith W, Cumming RR, Mitchell P. Impact of bilateral visual impairment on health-related quality of life: the Blue Mountains eye study. Invest Ophthalmol Vis Sci. 2004;45(1):71–6.
Heesterbeel TJ, van der Aa HPA, van Rens GHMB, Twisk JWR, van Nispen RMA. The incidence and predictors of depressive and anxiety symptoms in older adults with vision impairment: a longitudinal prospective cohort study. Ophthalmic Physiol Opt. 2017;37:385–98.
Ong SY, Cheung CY, Li X, et al. Visual impairment, age-related eye diseases, and cognitive function: the Singapore Malay Eye Study. Arch Ophthalmol. 2012;130(7):895–900.
Macedo AF, Ramos PL, Hernandez-Moreno L, et al. Visual and health outcomes, measured with the activity inventory and the EQ-5D, in visual impairment. Acta Ophthalmol. 2017;95:783–91.
Der Wiel AB, van Exel E, de Craen AJ, et al. A high response is not essential to prevent selection bias: results from the Leiden 85-plus study. J Clin Epidemiol. 2002;55(11):1119–25.
Gussekloo J, de Craen AJ, Oduber C, van Boxtel MP, Westendorp RG. Sensory impairment and cognitive functioning in oldest-old subjects: The Leiden 85+ Study. Am J Geriatr Psychiatry. 2005;13(9):781–6.
Kempen GI, Miedema I, Ormel J, Molenaar W. The assessment of disability with the Groningen Activity Restriction Scale. Conceptual framework and psychometric properties. Soc Sci Med. 1996;43(11):1601–10.
Bootsma-van der Wiel A, Gussekloo J, de Craen AJ, van Exel E, Knook DL, Lagaay AM, Westendorp RG. Disability in the oldest old: “can do” or “do do”? J Am Geriatr Soc. 2001;49(7):909–14.
Heeren TJ, Lagaay AM, von Beek WC, Rooymans HG, Hijmans W. Reference values for the Mini-Mental State Examination (MMSE) in octo- and nonagenarians. J Am Geriatr Soc. 1990;38(10):1093–6.
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17(1):37-49.
De Jong GJ, van Tilburg T. A shortened scale for overall, emotional and social loneliness. Tijdschr Gerontol Geriatr. 2008;39(1):4–15.
Cantril H. The Pattern of Human Concern. New Brunswick: NJ Rutgers University Press; 1965.
Dandona L, Dandona R. Revision of visual impairment definitions in the International Statistical Classification of Diseased. BMC Med. 2006;4:7.
Travis LA, Boerner K, Reinhardt JP, Horowitz A. Exploring functional disability in older adults with low vision. J Visual Impair Blin. 2004;98(9):534–45.
Keller BK, Morton JL, Thomas VS, Potter JF. The effect of visual and hearing impairments on functional status. J Am Geriatr Soc. 2005;47(11):1319–25.
Berger S, Porell F. The association between low vision and function. J Aging Health. 2008;20(5):504–25.
Aartolahti E, Häkkinen A, Lönnroos E, Kautiainen H, Sulkava R, Hartikainen S. Relationship between functional vision and balance and mobility performance in community-dwelling older adults. Aging Clin Exp Res. 2013;25(5):545–52.
Van Nispen RMA, Vreeken HL, Comijs HC, Deeg DJH, van Rens GHMB. Role of vision loss, functional limitations and the supporting network in depression in a general population. ACTA Ophthalmol. 2016;94:76–82.
Beyermann S, Trippe RH, Bähr AA, Püllen R. Mini-Mental State Examination in Geriatrics: an evaluation of diagnostic quality. Z Gerontol Geriatr. 2013;46(8):740–7.
Puvill T, Linderberg J, de Craen AJ, Slaets JP, Westendorp RG. Impact of physical and mental health on life satisfaction in old age: a population based observational study. BMC Geriatr. 2016;16:194.
Radicke F, Schwaneberg T, Neinke-Franze C, et al. Prevalence of impaired functional reading ability and its association with quality of life, daily activity, mobility and social participation among general older adults in Germany. BMC Geriatr. 2019;19:176.
Ejiakor I, Achigbu E, Onyia O, Edema O, Florence N. Impact of visual impairment and blindness on quality of life of patients in Owerri, Imo State. Nigeria Middle East Afr J Ophthalmol. 2019;26(3):127–32.
Von faber M, Bootsma-van der Wiel A, van Exel E, et al. Succesful aging in the oldest old: who can be characterizes as successfully aged? Arch Intern Med. 2001;161(22):2694–700.
Haanes GG, Hall EOC, Eilertsen G. Acceptance and adjustment: a qualitative study of experiences of hearing and vision impairments and daily life among oldest old recipients of home care. Int J Older People Nurs. 2019;14:e12236.
National Academics of Sciences, Engineering and Medicine. The impact of vision loss. In: Welp A, Woodbury RB, McCoy MA, Teutsch SM, editors. Making eye health a population health imperative: vision for tomorrow. Washington DC: The National Academies Press; 2016. doi: https://doi.org/10.17226/23471
Nastasi JA. Occupational therapy interventions supporting leisure and social participation for older adults with low vision: a systematic review. Am J Occup Ther. 2020;74(1):7401185020p1–9.
Van Nispen R, van der AA H, Timmermans F, et al. Reducing avoidable visual impairment in elderly home healthcare patients by basic ophthalmologic screening. Acta Ophthalmol. 2019;97:401–8.
Tan CS, Man R, Wong CW, Lee SY, Lamoureux EL, Ang M. Randomized controlled trial evaluating a novel community eye care programme for elderly individuals with visual impairment. Clin Exp Ophthalmol. 2018;46:593–9.
Acknowledgements
Not applicable
Funding
The Leiden 85-plus Study was partly funded by an unrestricted grant from the Dutch Ministry of Health, Welfare and Sports. The funder played no role in study design, collection, analysis and interpretation of data, writing of the report, and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
YMD and JG contributed to the study concept and design; ERJ performed the statistical analysis and wrote the initial draft; ERJ and YMD interpreted the data; all authors critically reviewed the manuscript for important intellectual content and approved the final version submitted for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. The Medical Ethical Committee of the Leiden University Medical Center approved the study in 1997 (reference number P97/04) and all participants provided fully informed consent with written documents prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Verbeek, E., Drewes, Y. & Gussekloo, J. Visual impairment as a predictor for deterioration in functioning: the Leiden 85-plus Study. BMC Geriatr 22, 397 (2022). https://doi.org/10.1186/s12877-022-03071-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03071-x