Abstract
Background
The role of obesity in mortality in the very old and old-oldest Hispanic population has not been studied. The objective of this study was to examine the effect of body mass index (BMI) on 12-year mortality among older Mexican Americans aged 75 years and older.
Methods
Twelve year prospective cohort study consisting of a population-based sample of 1415 non-institutionalized Mexican American men and women aged 75 and older from 5 southwestern states: Arizona, California, Colorado, New Mexico, and Texas. Data was from Wave 5 of the Hispanic Established Population for the Epidemiologic Study of the Elderly (2004/2005–2016). Socio-demographics, body mass index (BMI), self-reported medical conditions, disability, depressive symptoms, falls, Mini-Mental-State-Examination (MMSE), and Short Physical Performance Battery (SPPB) were assessed at baseline during 2004–2005. BMI (Kg/m2) was classified as underweight (< 18.5), normal weight (18.5 to < 25), overweight (25 to < 30), obesity category I (30 to < 35), and obesity category II/morbid obesity (≥ 35). For assessment of mortality, deaths were ascertained through the National Death Index and report from relatives. Cox proportional hazards regression analysis was performed to estimate the hazard ratio (HR) of 12-year mortality as a function of BMI categories at baseline.
Results
The mean BMI was 27.5 ± 1.7 with participants classified as 1.8% underweight, 30.8% normal weight, 39.2% overweight, 20.7% obesity category I, and 7.6% obesity category II/morbid obesity. Mexican Americans aged ≥75 years with overweight or obesity category I had a reduced HR of death (0.82, 95% CI = 0.70–0.96 and 0.75, 95% CI = 0.62–0.91, respectively) over 12-years of follow-up. The HR of death for underweight and obesity category II/morbid obesity participants was 1.59 (95% CI = 1.03–2.45) and 1.12 (95% CI = 0.85–1.46), respectively. Female participants and those with high scores in the MMSE and SPPB had decreased risk of death.
Conclusions
This study showed the protective effect of overweight and obesity on mortality in Mexican Americans above 75 years of age, which might have implications when treating older adults with overweight and obesity.
Similar content being viewed by others
Background
Obesity continues to rise in the United States. According to the Centers for Disease Control and Prevention (CDC), the prevalence of obesity in the U.S. has increased from 30.5 to 42.4% from 1999 to 2000 to 2017–2018 [1]. The Hispanic population is affected by the obesity epidemic, with 42.5% classified as obese compared with non-Hispanic white (34.5%), non-Hispanic black (48.1%), and non-Hispanic Asian adults (11.7%) [1]. Overall, the prevalence of obesity among women (38.3%) is higher than among men (34.3%) [1]. U.S. born Hispanics (47.1%) have a higher prevalence of obesity than foreign-born Hispanics (36.3%) [2].
A strong association has been found between obesity and mortality in several longitudinal studies in young and middle-aged adults [3]. However, an “obesity survival paradox” is seen in older persons above 65 years in which an increased risk in all-cause mortality from obesity is not seen, and the optimal body mass index (BMI) is increased to between 24 and 35 kg/m2, with most in the range of 27 to 30 kg/m2 [4]. Several studies have reported a decreased association of overweight (25 - < 30 kg/m2) [5,6,7,8,9,10,11,12,13] and obesity (> 30 kg/m2) [5,6,7,8,9, 11, 13, 14] with mortality compared to normal weight in older persons above 65 years and older.
The protective effect of obesity on mortality that has been reported in adults aged 65 years and older has also been reported in the very old and the oldest-old adults. For example, Kuznicka et al. using the PolSenior study found that a BMI of 25.0 to 34.9 kg/m2 was associated with the lowest mortality and underweight (BMI < 18.5 kg/m2) was associated with the highest mortality (p < 0.001) among those 65–79 years of age, while for those aged 80 year and older a BMI of 25.0–39.9 kgm2 was associated with lowest mortality while BMI ≤ 24.9 kg/m2 was associated with highest mortality (p < 0.001) over 3 years of follow-up [15]. In another study, Stenholm et al. found in a cohort of Finish older adults aged 50–91 years that those aged 70 years and older who were overweight and obese had 23 and 24%, respectively, decreased risk of mortality over 33 years of follow-up [16]. Dahl et al. found in a cohort of Swedish older adults aged 70 to 95 years that those in the overweight group had a 20% decreased risk for mortality compared to the normal group over 4 years of follow-up for those younger than 80 years and 2 years of follow-up for those over 80 years [17]. Wang et al. using the Chinese Longitudinal Healthy Longevity Survey (CLHLS) found that participants aged 80 years and older with overweight and obesity had a 11 and 9% decreased risk of mortality compared with the normal weight group over 3 years of follow-up [18].
Between now and 2050, those who are 65 years and older in the Hispanic population are expected to experience rapid aging [19]. By 2050, the percentage of Hispanics aged 65 and older is predicted to grow by 134% while the percentage of Non-Hispanic Whites is predicted to grow 58.4% [19, 20]. At birth in the United States, the life expectancy for Hispanics (78.83 years for males, 84.05 for females) is longer than for non-Hispanic whites (76.30 years for males, 81.06 for females) and non-Hispanic Blacks (71.41 for males, 77.62 for females) [21]. Male Mexican Americans live about 2.5 years and 7.4 years longer than their non-Hispanic white and non-Hispanic black counterparts, respectively [21]. Female Mexican Americans live about 3 years and 6.5 years longer than their non-Hispanic white and non-Hispanic black counterparts, respectively [21]. According to the National Vital Statistics report, the Hispanic population has a ‘survival advantage’ by age 65 compared to other populations in the U.S. and it increases with age [21]. Approximately, 87.7% of the Hispanic population survive to age 65 compared to 84.5% of the non-Hispanic white population and 76.5% of the non-Hispanic black population [21]. This report also found that 50.7% of the Hispanic population survive to age 65 compared with 41.5% in the Non-Hispanic White population and 32.1% in the non-Hispanic black population [21].
The role of obesity in mortality in the very old and old-oldest Hispanic population has not been studied. Therefore, we examined BMI as predictor of 12-year mortality among Mexican American older adults enrolled in the Hispanic Established Epidemiologic Study of the Elderly (HEPESE) aged 75 years and older. We hypothesize a protective effect of overweight and obesity on mortality in Mexican Americans above 75 years of age.
Methods
Sample
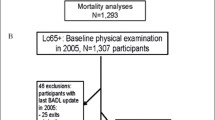
Data were from the HEPESE, a longitudinal cohort study of non-institutionalized Mexican Americans 65 years and older who reside in five southwestern states of the U.S. (Arizona, California, Colorado, New Mexico, and Texas). The original HEPESE cohort included 3050 Mexican Americans aged 65 years and older who were interviewed in-home face to face or via proxy in 1993/94. In 2004/05 a new cohort of 902 participants aged 75 years and older were added to the 1167 participants of the original cohort who were 75 years and older (N = 2069). Bilingual interviewers were trained to gather information on socio-demographic, health conditions, and psycho-social characteristics of respondents in their language of choice every 2 or 3 years. Nine waves of data have been collected. Information and data for the HEPESE are available at the National Archive of Computerized Data on Aging [22]. The present study used data collected from Wave 5 (hereafter referred as baseline) to Wave 9 (2004/05–2016), allowing for approximately 12 years of follow-up data. Out of 2069 eligible participants, we excluded 653 with incomplete information on body mass index and covariates. The final analytical sample included 1415 participants. Excluded participants were significantly more likely to be older, unmarried or US-born; to have a lower level of education, lower short physical performance (SPPB) and lower Mini-Mental State Examination (MMSE) scores; and to report more diabetes, high depressive symptoms, any or more falls, and limitations in activities of daily living (ADLs) than included participants. At the end of follow-up (2016), 376 participants were re-interviewed in person, 140 were lost to follow-up, and 899 were confirmed dead through the National Death Index and report from relatives.
Measurements
Predictor variable
Baseline measured body mass index (BMI) was calculated as weight in kilograms divided by height in squared meters. BMI was grouped according to the National Institutes of Health obesity standards (< 18.5 Kg/m2, underweight; 18.5 to < 25 Kg/m2, normal weight; 25 to < 30 Kg/m2, overweight; 30 to < 35 Kg/m2, obesity category I; and ≥ 35 Kg/m2, category II/morbid obesity).
Outcome
All cause mortality over 12 years of follow-up. Deaths were ascertained through the National Death Index and report from relatives.
Covariates
Sociodemographic variables (age, sex, marital status, years of formal education, and marital status), current smoking, and self-reported medical conditions (hypertension, diabetes, stroke, cancer, heart attack, or hip fracture). Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale. The scale consists of 20 items that ask how often specific symptoms were experienced in the past week and were scored on a 4-point scale (ranging from rarely/none of the time to most/all the time: 0, 1, 2, 3) and total scored range 0–60 [23]. A score of 16 or greater is used to determine a clinical range for those with depressive symptoms [24]. Cognitive function was assessed with the Mini Mental Status Examination (MMSE), with scores ranging from zero to 30. MMSE screens for difficulties in orientation, working memory, naming, language, image copying, and episodic memory [25]. Fall status was established by asking participants “During the last 12 months, how many times did you fall and land on the floor or ground?” and categorized as ≥1 falls in the last 12-months. Functional disability was assessed using seven items (walking across a small room, bathing, grooming, dressing, eating, transferring from a bed to a chair, and using the toilet) from a modified version of the Katz ADL scale [26]. Physical function was assessed using the SPPB, which includes three lower body extremity tests (walking speed, standing balance and repeated chair stands. Scores range from 0 to 12 with higher scores indicating higher physical functioning [27].
Statistical analysis
ANOVA, Chi square, and Fisher exact tests were performed to describe the baseline sample characteristics by BMI category. Cox proportional hazards regression analysis was performed to estimate the hazard ratio of 12-year mortality as a function of baseline BMI category controlling for all covariates. Those subjects who died or were unable to be located were censored at the date of last follow-up (last interview date for the 12-year follow-up). Three models were performed. Model 1 included BMI categories with all covariates. Model 2 was not adjusted for comorbidities. In Model 3, participants who died the first 2 years of follow-up and those were current smokers were excluded. The Cox proportional hazard regression assumption was confirmed. Statistical analysis was performed using the SAS, version 9.4 (SAS Institute, Inc., Cary NC).
Results
Table 1 presents the descriptive characteristics of the overall sample and by BMI categories. The overall mean age was 81.3 ± 4.5 years. The mean BMI was 27.5 ± 1.7 with participants classified as 1.8% underweight, 30.8% normal weight, 39.2% overweight, 20.7% obesity category I, and 7.6% category II/morbid obesity. Sixty percent of the participants were female, 45.3% were married, 58.0% were born in the United States, and the mean years of education was 5.5 ± 3.9. Mean MMSE and SPPB scores were 22.8 ± 5.4 and 6.4 ± 3.4, respectively. Sixty-two percent of participants reported hypertension, 8.0% heart attack, 6.9% cancer, 31.9% diabetes, 5.9% stroke, and 14.7% had high depressive symptoms at baseline. Thirty-two percent of participants had more than one fall in the past year and 24.6% had ADL disability at baseline. Sixty-four percent % of participants died over 12 years of follow-up. Female participants were significantly more likely to be in the obesity category I or obesity category II/morbid obesity. Overweight participants were significantly more likely to be married and to have higher level of education than those in other BMI categories. Underweight participants were significantly more likely to be current smokers and to have lower scores on the MMSE than those in the other BMI categories. Participants with category II/morbid obesity had the lowest mean years of education, scored lower in the SPPB, and were more likely to report hypertension, diabetes, and ADL disability compared to those in other BMI categories.
Table 2 presents the results of Cox proportional hazard analysis of 12-year mortality as a function of baseline BMI categories. In the Model 1, participants in the overweight or obesity category I had decreased hazard ratio (HR) of mortality (0.82, 95% CI = 0.70–0.96 and 0.75, 95% CI = 0.62–0.91, respectively) than those in the normal weight category after controlling for all covariates. Participants in the underweight category had increased HR of mortality (1.59, 95% CI = 1.03–2.45) than those in the normal weight category after controlling for all covariates. Obesity category II/morbid obesity was not associated with mortality (HR = 1.12, 95% CI = 0.85–1.46). Female participants and those with high SPPB and MMSE scores had decreased risk of mortality, while diabetes and heart attack had an increased risk of mortality. In Model 2, without adjusting for comorbidities, overweight and obesity category I were at less risk of mortality. When we excluded those who died during the first 2 years of follow-up and those who were current smokers (Model 3), those in the overweight or obesity category I had decreased hazards of mortality.
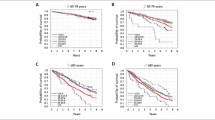
Figure 1 presents the survival curve of participants as a function of baseline BMI categories over 12 years of follow-up. Underweight participants had the sharpest decline in survival time over the period of follow-up.
Discussion
This study examined the effect of baseline BMI categories on 12-year mortality among Mexican American men and women aged 75 years and older. We found that compared to those in the normal weight category, overweight or obesity category I had an 18 and 25% decreased risk of mortality, respectively. Those in the underweight or obesity category II/morbid obesity had a 59 and 12% increased risk of mortality than those in the normal weight category. We found decreased risk of mortality among females and those who had higher scores on the MMSE and SPPB tests. This study showed the protective effect of overweight and obesity on mortality in Mexican Americans above 75 years of age, which might have implications when treating older adults with overweight and obesity.
Little has been written about BMI and mortality in the oldest old, especially among Mexican Americans. Our findings are similar to prior studies. For example, our findings are similar to those reported in the study of Finnish older adults above 70 years of age where overweight and obesity was associated with 23 and 24% decreased risk of mortality, respectively, over 33 years of follow-up [16]. Our results were also consistent with the limited number of studies that included participants over 80 years of age which showed overweight [15, 17, 18] and obesity [15, 18] to be associated with lower mortality and underweight [15, 18] with higher mortality. These studies included Polish, Swedish, or Chinese men and women. Dahl et al. found in a cohort of Swedish older adults aged 70 to 95 years that those in the overweight group had a 20% decreased risk for mortality compared to the normal group over 4 years of follow-up for those younger than 80 years and 2 years of follow-up for those over 80 years [17]. Wang et al. using the Chinese Longitudinal Healthy Longevity Survey (CLHLS) found that overweight and obese participants aged 80 years and older had a 11 and 9% decreased risk of mortality, respectively, compared with the normal weight group over 3 years of follow-up [18] Takata et al. found in a cohort of Japanese older adults aged 80 and older that the most-lean group (BMI < 19.5) had the highest all-cause mortality while the group with BMI 22.5 to < 23.8 had the lowest all-cause mortality [28]. Although our results are consistent with these studies, they include different ethnicities of participants which makes comparison difficult due to ethnic differences in body composition. Rolland et al. found in a cohort of French older women aged 75 years and older that mortality risk was higher in participants with BMI ≤ 24.6 at 12-years of follow-up [29]. Although we found similar results, this study used BMI as a continuous variable, had a different ethnic demographic, and included women only.
There are several possible mechanisms through which higher adiposity may confer lower mortality risk in the very old and oldest-old. First, adiposity in older adults may be protective from malnutrition by allowing an escape from a negative energy balance due to a greater metabolic reserve [30,31,32]. Second, obesity has been associated with increased bone density in older adults [31], which can offer protection from osteoporotic fractures through a fat cushioning effect for surrounding areas, like the hip, which are prone to fracture after a fall [4]. Third, overweight and obesity can modulate progression of heart failure [31, 32]. Studies have found overweight and obesity offer a better prognosis in chronic heart failure, possibly due to lower atrial naturetic peptide levels, lower sympathetic activation, and decreased reponse to activated renin-angiotensin-aldosterone system (RAAS) [33]. Fourth, adiposity in the older adults may provide better antioxidant defense [4]. Sarcopenia from weight loss results in loss of muscle mass in older adults [4]. According to Oreopoulos et al. sarcopenia reduces oxidative metabolism in the skeletal muscle which could increase oxidative stress and inflammation [4]. Lastly, reverse causality may also be playing a role in adiposity conferring a protective effect on mortality. Garcia et al. examined BMI and mortality in a U.S. cohort over 5 years of follow-up by excluding smokers and those with pre-existing conditions [34]. Exclusion of these individuals resulted in lower mortality risk in the underweight than it would have been included [34].
This study has some limitations. First, co-morbidities were assessed through self-reports. However, studies have shown agreement between self-report and comorbid conditions or diseases as well as medical events [35]. Second, participants excluded from the study were less healthy compared to those included, which might have resulted in underestimating the relationship between BMI and mortality. However, when we excluded those who died in the first 2 years of follow-up and those who were current smokers, the relationship between BMI and mortality did not change. Third, we did not analyze BMI categories change over time. However, previous studies have shown that increasing BMI was not associated with higher risk of mortality while decreasing BMI associated with higher risk of mortality [36,37,38]. Fourth, maybe the BMI value is overestimated due to height loss in older adults due to decrease vertebral bone mineral density [31]. We used BMI instead of other anthropometric measurements because it has been found that adjusting for height loss only has a slight effect on BMI when examining the association with mortality and healthcare cost estimates [39,40,41]. Fifth, our sample is not generalizable to the entire Hispanic population in the United States because it consisted only of Mexican Americans living in the Southwestern US. However, findings from the National Health Interview Survey that included only Hispanics showed that underweight was associated with increased mortality while those in the overweight or obesity category I were at increased mortality over 8-years of follow-up [42]. Similarly, findings from the National Health and Nutrition Examination Survey that analyzed only Mexican Americans showed BMI was not significantly associated with mortality [43]. Despite these limitations, our study has several strengths including the use of a large population-based sample of community dwelling of Mexican Americans aged 75 years and older, follow-up data over 12 years which is longer than the studies conducted in other race/ethnic groups, and the inclusion of both females and males.
Conclusions
The results of our study suggest the protective effect of overweight and obesity category I against mortality in Mexican Americans aged 75 years and older. At 12 years of follow-up, Mexican Americans aged 75 years and older with overweight or obesity category I had statistically decreased risk of mortality compared to normal weight. While participants with underweight had a statistically increased risk of mortality compared to normal weight. Our study has many implications for the care of older Mexican American adults in the group of very old and oldest-old. BMI should be carefully monitored by healthcare providers when caring for this population. Based on the height of the patient, an appropriate weight range can be calculated, suggested, and monitored. Appropriate prevention and intervention programs based on BMI maybe developed to maintain a healthy weight. With our study finding underweight having an increased risk of mortality, our public health recommendation for the very old and oldest old is to avoid drastic weight loss in order to not be in the underweight category. Instead, their weight should be maintained, particularly in the overweight or obesity type 1 categories. Providers should be cautious in recommending weight loss in the very old and oldest old [31]. More studies examining BMI and mortality must be done in this population to further support our conclusions.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available at https://www.icpsr.umich.edu/icpsrweb/NACDA/series/546.
Abbreviations
- BMI:
-
Body Mass Index
- MMSE:
-
Mini-Mental-State-Examination
- SPPB:
-
Short Physical Performance Battery
- ADL:
-
Activities of Daily Living
- HR:
-
Hazard Ratio
- HEPESE:
-
Hispanic Established Population for the Epidemiologic Study of the Elderly
- CDC:
-
Centers for Disease Control and Prevention
References
Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;(219):1–8.
Van Hook J, Baker E, Altman CE, Frisco ML. Canaries in a coalmine: immigration and overweight among Mexican-origin children in the US and Mexico. Soc Sci Med. 2012;74(2):125–34.
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338(1):1–7.
Oreopoulos A, Kalantar-Zadeh K, Sharma AM, Fonarow GC. The obesity paradox in the elderly: potential mechanisms and clinical implications. Clin Geriatr Med. 2009;25(4):643–59 viii.
Wu CY, Chou YC, Huang N, Chou YJ, Hu HY, Li CP. Association of body mass index with all-cause and cardiovascular disease mortality in the elderly. PLoS One. 2014;9(7):e102589.
Yi SW, Ohrr H, Shin SA, Yi JJ. Sex-age-specific association of body mass index with all-cause mortality among 12.8 million Korean adults: a prospective cohort study. Int J Epidemiol. 2015;44(5):1696–705.
Zaslavsky O, Rillamas-Sun E, LaCroix AZ, Woods NF, Tinker LF, Zisberg A, et al. Association between anthropometric measures and long-term survival in frail older women: observations from the Women’s Health Initiative Study. J Am Geriatr Soc. 2016;64(2):277–84.
Cheng FW, Gao X, Mitchell DC, Wood C, Still CD, Rolston D, et al. Body mass index and all-cause mortality among older adults. Obesity (Silver Spring). 2016;24(10):2232–9.
Hirani V, Naganathan V, Blyth F, Le Couteur DG, Gnjidic D, Stanaway FF, et al. Multiple, but not traditional risk factors predict mortality in older people: the Concord Health and Ageing in Men Project. Age (Dordr). 2014;36(6):9732.
Lee Y, Kim J, Han ES, Ryu M, Cho Y, Chae S. Frailty and body mass index as predictors of 3-year mortality in older adults living in the community. Gerontology. 2014;60(6):475–82.
Lee EY, Lee YH, Yi SW, Shin SA, Yi JJ. BMI and all-cause mortality in normoglycemia, impaired fasting glucose, newly diagnosed diabetes, and prevalent diabetes: a cohort study. Diabetes Care. 2017;40(8):1026–33.
Leigh L, Byles JE, Jagger C. BMI and healthy life expectancy in old and very old women. Br J Nutr. 2016;116(4):692–9.
Al Snih S, Ottenbacher KJ, Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007;167(8):774–80.
Dhana K, Berghout MA, Peeters A, Ikram MA, Tiemeier H, Hofman A, et al. Obesity in older adults and life expectancy with and without cardiovascular disease. Int J Obes. 2016;40(10):1535–40.
Puzianowska-Kuznicka M, Kuryłowicz A, Walkiewicz D, Borkowska J, Owczarz M, Olszanecka-Glinianowicz M, et al. Obesity paradox in Caucasian seniors: results of the PolSenior study. J Nutr Health Aging. 2019;23(9):796–804.
Stenholm S, Mehta NK, Elo IT, Heliövaara M, Koskinen S, Aromaa A. Obesity and muscle strength as long-term determinants of all-cause mortality--a 33-year follow-up of the Mini-Finland Health Examination Survey. Int J Obes. 2014;38(8):1126–32.
Dahl AK, Fauth EB, Ernsth-Bravell M, Hassing LB, Ram N, Gerstof D. Body mass index, change in body mass index, and survival in old and very old persons. J Am Geriatr Soc. 2013;61(4):512–8.
Wang J, Taylor AW, Zhang T, Appleton S, Shi Z. Association between body mass index and all-cause mortality among oldest old Chinese. J Nutr Health Aging. 2018;22(2):262–8.
US C-B. 2014 American community survey 1-year estimates, Hispanic or Latino origin by specific origin. Washington: U.S. Department of Commerce; 2014.
Ortman J, Velkoff V. An aging nation: the older population in the United States, Current Population Reports, P25-1140. Washington, DC: U.S. Census Bureau. 2014.
Arias E, Miniño A, Curtin S, Tejada-Vera B. U.S. decennial life tables for 2009-2011, United States life tables. Natl Vital Stat Rep. 2020;69(8):1–73.
Markides K, Chen N-W, Angel R, Palmer R, Graham J. Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE) Wave 7, 2010-2011 [Arizona, California, Colorado, New Mexico, and Texas]. Ann Arbor: Inter-university Consortium for Political and Social Research [distributor]; 2016. https://doi.org/10.3886/ICPSR36537.v2.
Radloff LS. The CES-D scale:a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample: understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982;39(10):1195–200.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Branch LG, Katz S, Kniepmann K, Papsidero JA. A prospective study of functional status among community elders. Am J Public Health. 1984;74(3):266–8.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–62.
Takata Y, Ansai T, Soh I, Awano S, Nakamichi I, Akifusa S, et al. Body mass index and disease-specific mortality in an 80-year-old population at the 12-year follow-up. Arch Gerontol Geriatr. 2013;57(1):46–53.
Rolland Y, Gallini A, Cristini C, Schott AM, Blain H, Beauchet O, et al. Body-composition predictors of mortality in women aged ≥ 75 y: data from a large population-based cohort study with a 17-y follow-up. Am J Clin Nutr. 2014;100(5):1352–60.
Pes GM, Licheri G, Soro S, Longo NP, Salis R, Tomassini G, et al. Overweight: a protective factor against comorbidity in the elderly. Int J Environ Res Public Health. 2019;16(19):1–10.
Javed AA, Aljied R, Allison DJ, Anderson LN, Ma J, Raina P. Body mass index and all-cause mortality in older adults: a scoping review of observational studies. Obes Rev. 2020;21(8):e13035.
Donini LM, Pinto A, Giusti AM, Lenzi A, Poggiogalle E. Obesity or BMI paradox? Beneath the tip of the iceberg. Front Nutr. 2020;7:53.
Wang S, Ren J. Obesity paradox in aging: from prevalence to pathophysiology. Prog Cardiovasc Dis. 2018;61(2):182–9.
Garcia GR 3rd, Coleman NC, Pond ZA, Pope CA 3rd. Shape of BMI-mortality risk associations: reverse causality and heterogeneity in a representative cohort of US adults. Obesity (Silver Spring). 2021;29(4):755–66.
Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145(8):762–9.
Ghaem Maralani H, Tai BC, Wong TY, Tai ES, Li J, Wang JJ, et al. The prognostic role of body mass index on mortality amongst the middle-aged and elderly: a competing risk analysis. Diabetes Res Clin Pract. 2014;103(1):42–50.
Graf CE, Herrmann FR, Spoerri A, Makhlouf AM, Sørensen TIA, Ho S, et al. Impact of body composition changes on risk of all-cause mortality in older adults. Clin Nutr. 2016;35(6):1499–505.
Holme I, Tonstad S. Survival in elderly men in relation to midlife and current BMI. Age Ageing. 2015;44(3):434–9.
Onwudiwe NC, Stuart B, Zuckerman IH, Sorkin JD. Obesity and medicare expenditure: accounting for age-related height loss. Obesity (Silver Spring). 2011;19(1):204–11.
Sorkin JD, Muller DC, Andres R. Longitudinal change in the heights of men and women: consequential effects on body mass index. Epidemiol Rev. 1999;21(2):247–60.
Li JB, Luo S, Wong MCS, Li C, Feng LF, Peng JH, et al. Longitudinal associations between BMI change and the risks of colorectal cancer incidence, cancer-relate and all-cause mortality among 81,388 older adults : BMI change and the risks of colorectal cancer incidence and mortality. BMC Cancer. 2019;19(1):1082.
Mehta T, McCubrey R, Pajewski NM, Keith SW, Allison DB, Crespo CJ, et al. Does obesity associate with mortality among Hispanic persons? Results from the National Health Interview Survey. Obesity (Silver Spring). 2013;21(7):1474–7.
Howell CR, Mehta T, Ejima K, Ness KK, Cherrington A, Fontaine KR. Body composition and mortality in Mexican American adults: results from the National Health and Nutrition Examination Survey. Obesity (Silver Spring). 2018;26(8):1372–80.
Acknowledgments
NA.
Funding
This work was supported by the National Institute on Aging, the National Institute on Minority Health and Health Disparities, and Texas Resource Center on Minority Aging Research (R01 AG10939, R01 AG017638, 1P30 AG059301-01, and R01 MD010355).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the completion of this study. RJ, KSM, and SAS developed the conception and design of the work. SAS completed data analyses. RJ wrote first draft of the manuscript. RJ, KSM contributed to the data interpretation and paper revision. All authors meet the authorship requirements as stated in the Uniform Requirement for Manuscripts Submitted to Biomedical Journals. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study and all research protocols were approved by the Institutional Review Board (IRB) of the University of Texas Medical Branch (IRB approval number: 92–85) in accordance with the Declaration of Helsinki. Informed verbal consent was approved by the Institutional Review Board of the University of Texas Medical Branch.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jadhav, R., Markides, K.S. & Al Snih, S. Body mass index and 12-year mortality among older Mexican Americans aged 75 years and older. BMC Geriatr 22, 236 (2022). https://doi.org/10.1186/s12877-022-02945-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-02945-4