Abstract
Background
Delirium is a common disorder among hospitalized older patients and results in increased morbidity and mortality. The prevention of delirium is still challenging in older patient care. The role of antipsychotics in delirium prevention has been limited. Therefore, we conducted a trial to investigate the efficacy of quetiapine use to prevent delirium in hospitalized older medical patients.
Methods
This study was a randomized double-blind controlled trial conducted at Ramathibodi Hospital, Bangkok, Thailand. Patients aged ≥65 years hospitalized in the internal medicine service were randomized to quetiapine 12.5 mg or placebo once daily at bedtime for a maximum 7-day duration. The primary end point was delirium incidence. Secondary end points were delirium duration, length of hospital stay, ICU admission, rehospitalization and mortality within 30 and 90 days.
Results
A total of 122 patients were enrolled in the study. Eight (6.6%) left the trial before receiving the first dose of the intervention, whereas 114 (93.4%) were included in an intention-to-treat analysis allocated to the quetiapine or placebo group (n = 57 each). The delirium incidence rates in the quetiapine and placebo groups were 14.0 and 8.8% (OR = 1.698, 95% CI 0.520–5.545, P = 0.381), respectively. Other endpoints in the quetiapine and placebo groups were the median length of hospital stay, 6 (4–8) days versus 5 (4–8) days (P = 0.133), respectively; delirium duration, 4 (2.3–6.5) versus 3 (1.5–4.0) days (P = 0.557), respectively; ICU admission, 3 (5.3%) patients from both groups (P = 1.000); and mortality in the quetiapine and placebo groups, 1 (1.8%) versus 2 (3.5%) at 30 days (P = 0.566) and 7 (12.3%) versus 9 (15.8%) days at 90 days (P = 0.591). There were no significant differences in other outcomes. None of the participants reported adverse events.
Conclusions
Quetiapine prophylaxis did not reduce delirium incidence in hospitalized older medical patients. The use of quetiapine to prevent delirium in this population group should not be recommended.
Trial registration
This trial was retrospectively registered with the Thai clinical trials registry (TCTR) at clinicaltrials.in.th (TCTR20190927001) on September 26, 2019.
Similar content being viewed by others
Background
Acute delirium is one of the most common clinical syndromes in hospitalized older patients. The features of delirium include acute onset and disturbances in attention and cognition [1]. A previous systematic review found the overall prevalence of delirium on admission to range between 10 and 31% and the overall rate to range between 11 and 42% during the hospital stay [2]. In geriatric wards, Inouye SK et al. found that the prevalence and incidence of delirium were 25% and 20–29%, respectively, which were much higher than those in general medical wards [3].
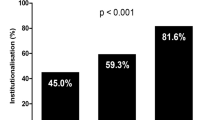
Older patients who developed delirium were associated with a 1.9x increased risk of mortality, a 1.3x increased risk of falls, and a 2.5x increased risk of institutionalization [3]. Furthermore, delirium was found to be related to an increased length of hospital stay. Some patients still had persistent symptoms of delirium at discharge and at 6 and 12 months. Mortality was also increased at 12 months after discharge [2].
The development of delirium is dependent on the interrelationship between a vulnerable patient with predisposing factors and exposure to precipitating factors. Some predisposing factors include age 65 years or older, cognitive impairment or dementia, history of delirium, functional impairment, visual or hearing impairment, comorbidity or severity of illness, depression, and history of stroke and alcohol abuse. Factors that can precipitate delirium include psychoactive or sedative drugs, use of physical restraints, urinary catheterization, infection and surgery [3, 4].
Delirium is preventable in 30–40% of cases [3, 5]. Recent meta-analyses have demonstrated that multicomponent nonpharmacological interventions were effective in reducing the incidence of delirium [6, 7]. The Hospital Elder Life Program (HELP) is an example of a successful intervention model [8, 9].
Pharmacological interventions have also shown some benefit. A study using ramelteon, a melatonin agonist, demonstrated the prevention of delirium in patients who were admitted due to serious medical problems [10]. Role of antipsychotics has also been studied. Although the recent meta-analyses have shown first-generation antipsychotics (e.g., haloperidol) could not prevent delirium, second-generation antipsychotics (e.g., olanzapine and risperidone) tended to reduce the incidence of delirium in postoperative patients. However, the routine use of antipsychotics to prevent delirium has not yet recommended because of insufficient evidence and potential adverse events [11, 12].
Quetiapine, which is one of second-generation and preferable antipsychotics in treating delirium in older patients due to reduced extrapyramidal side effects with equal efficacy [13,14,15,16,17], has limited data on delirium prevention. To our knowledge, there has been no study on quetiapine in hospitalized internal medicine patients.
Therefore, in our study, we aimed to evaluate the efficacy of quetiapine for the prevention of delirium in hospitalized older patients.
Method
Trial design
We conducted a single-center, double-blind, randomized, placebo-controlled study at Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. Participants were recruited between August 2018 and December 2018. The study was approved by the certified Medical Ethics Committee of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University. Generic quetiapine was supplied by the pharmaceutical department of Ramathibodi Hospital.
The hospital pharmacy prepackaged the study drug and placebo into identical capsules, carried out the randomization, and blinded the investigators and subjects. An independent data and safety monitoring committee evaluated all potentially serious adverse events. The study was conducted according to the Declaration of Helsinki and Good Clinical Practice guidelines. The trial was retrospectively registered with the Thai clinical trials registry (TCTR) at clinicaltrials.in.th (TCTR20190927001). The study adheres to CONSORT guidelines.
Participants
Eligible participants were patients aged ≥65 years and acutely hospitalized in a medical specialty. All patients were recruited from the emergency medical observation unit and general medical wards. Patients provided written informed consent before participation. Exclusion criteria included patient or family refusal or patients who were already diagnosed with delirium, dementia, or severe Parkinson’s disease, patients who were critically ill, unable to take medication, unable to communicate, expected to be discharged within 24 h, needed emergency surgery, had terminal illness, were currently taking antipsychotics, or patients who had active cardiac conditions, history of epilepsy, substance dependence or abuse, a blood potassium level ≤ 3.0 mEq/L or a corrected QTc ≥ 500 msec from EKG.
Randomization and interventions
Eligible and consenting patients were randomly assigned to quetiapine 12.5 mg tablets or placebo once daily at 9 pm for a maximum of seven consecutive days. The dosage of quetiapine was based on the recommended initial dose for delirium treatment in older patients [13]. Quetiapine was given once daily at bedtime due to sedating effects to aid sleep and cover the night time, when delirium usually developed [18,19,20,21]. The duration of the intervention was 7 days, which is the time during which most patients develop new-onset delirium [22]. Patients were randomized into the intervention or placebo group using fixed randomization schemes per site with a block size of 4 (1:1) according to a computer-generated randomization list.
Placebo and quetiapine were identical in appearance and packaged in identical medical envelopes containing 7 tablets with sequentially numbered labels, each with a unique study identification number. The medication was given by the nurse. Emergency unblinding was possible via 24-h contact with an on-call pharmacist, in case delirium developed or assigned intervention might affect patient care. Study staff, clinicians and participants were to remain blinded throughout the study.
Outcomes
The primary outcome was delirium incidence within seven consecutive days after the intervention was initiated. Secondary outcomes were delirium duration, hospital length of stay, ICU admission, rehospitalization, and 30- and 90-day mortalities.
Data collection
All patients were interviewed and assessed by trained clinicians and investigators. Baseline demographic and health-related characteristics were recorded. Delirium was assessed at baseline by experienced clinicians or investigators. Patients who were diagnosed with delirium at baseline or had medical records suspecting delirium during admission were excluded from the study. During the study intervention period, all patients were assessed daily by clinicians or investigators. Patients were also observed by nursing and medical staff. A session of delirium assessment training based on the confusion assessment method (CAM) [23] was provided for the nurses in every participating ward. A document consisting of a questionnaire based on CAM [24] was attached to the patient’s medical chart and filled in by the investigator or nurses to monitor and record the symptoms. Medical and nursing records were also reviewed for evidence of delirium symptoms. Delirium diagnosis was confirmed by a clinician or investigator according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V) criteria for delirium [25].
When delirium was diagnosed, the intervention was unblinded. The patient was further investigated for all potential causes and received standard delirium treatment. The patient remained under follow-up until discharge. Medical records from every patient were reviewed after discharge and at 3 months to collect data on primary diagnosis, comorbidities, complications, ICU admission, readmission and mortalities. Safety was monitored throughout the study by daily observation, examination by clinicians and investigators and by patient report. The study would be immediately terminated and unblinded in the case of suspected adverse events.
Sample size
Sample size was calculated based on the assumptions that the incidence of delirium in the placebo group would be 30% and that quetiapine prophylaxis would result in an absolute risk reduction of 20%. The estimate of the incidence of delirium in the placebo group was based on a previous study in a geriatric ward, which reported incidence rates ranging from 20 to 29% [3]. To detect a significant difference between groups, we sought to randomize 118 patients into 2 groups of 59 patients per treatment arm to give 80% statistical power at a two-sided 5% significance level (alpha).
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 23. Descriptive statistics [mean ± standard deviation (SD)], frequency and percentage, or median and interquartile range (IQR) were used to describe baseline patient characteristics. Intention-to-treat (ITT) analysis was performed. Patients who did not develop delirium during the 7-day intervention period or left the study in case of early termination or hospital discharge were regarded as negative on the primary outcome.
The incidence of delirium was based on the number of participants who developed at least one delirium episode within the first 7 days after study initiation. The incidence of delirium was compared between groups using the Chi-squared test. Odds ratios (ORs) with 95% confidence intervals (CIs) were reported as effect sizes using placebo as a reference group. Secondary outcomes were compared by using the chi-square test or Fisher’s exact test for dichotomous and nominal outcomes, the independent-samples t-test for normally distributed continuous outcomes, the Mann-Whitney U-test for ordinal outcomes and continuous outcomes that were not normally distributed and the Hodges-Lehmann estimator for confidence intervals for the difference between 2 medians. P-values < 0.05 were considered statistically significant. Survival analyses presented by Kaplan-Meier curves were used for graphical demonstration. Cox proportional hazard regression analyses were performed to estimate the hazard ratios (HRs) for 30- and 90-day survival for the quetiapine and placebo groups. Sensitivity analyses were performed with age and length of hospital stay groups. Age groups were stratified by age less than 75 years and 75 years and over according to the mean age (75.3 ± 7.1 years) from our study baseline characteristics. Length of hospital stay were stratified by less than or equal to 5 days and over 5 days groups according to median length of hospital (5 days) from our study outcomes. Interaction was tested by subgroup.
Results
Enrollment and baseline data
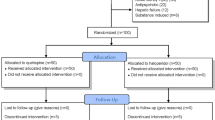
From August 2018 to December 2018, 1878 eligible patients aged over 65 years were admitted to a medical specialty. A total of 1756 patients were excluded, mostly due to active cardiac condition. A total of 122 participants were randomly assigned to quetiapine (n = 61) or placebo (n = 61). Eight participants (6.6%) were excluded (4 from each group) because of previous antipsychotic use, patient referral, patient or their relative’s denial and discharge before intervention initiation. A total of 114 participants (93.4%) (57 from each group) were included for ITT analysis of the primary outcome. However, 55 participants in the intervention group and 54 participants in the placebo group completed the trial. (Fig. 1) Three participants died during admission, and 4 participants died within the 3-month follow-up. The baseline characteristics of the quetiapine and placebo groups were not significantly different, as demonstrated in Table 1. Other baseline laboratory findings, previous comorbidities, and primary diagnoses of hospital admissions are described in the Supplementary Materials (Tables 1, 2 and 3 in Supplementary Materials), which were quite similar between both groups.
Primary outcome
The incidence of delirium in the quetiapine group was 14.0%, while that in the placebo group was 8.8% (OR = 1.698, 95% CI 0.520–5.545, P = 0.381). (Table 2).
Secondary outcome
The median durations of delirium in the quetiapine and placebo groups were 4 (2.3–6.5) days and 3 (1.5–4.0) days, respectively, difference = 0 day (95% CI 0–0, P = 0.557). The median lengths of hospital stay were 6 (4-8) days and 5 (4-8) days in the intervention and placebo groups, respectively, difference = 0 day (95% CI 0–0, P = 0.133). Three patients (5.3%) from each group were transferred to the intensive care unit, OR = 1.000 (95% CI 0.193–5.177, P = 1.000) The rates of rehospitalization within 90 days after discharge were not significantly different between the two groups, which involved 24 (42.1%) and 23 (40.4%) patients in the intervention and placebo groups, OR = 1.075 (95% CI 0.510–2.267, P = 0.849), respectively. Mortality within 30 days affected 1 (1.8%) and 2 (3.5%) patients in the quetiapine and placebo groups, OR = 0.491 (95% CI 0.043–5.573, P = 0.566), respectively, whereas mortality within 90 days affected 7 (12.3%) and 9 (15.8%) patients in the quetiapine and placebo groups, OR = 0.747 (95% CI 0.258–2.164, P = 0.591), respectively. Survival analyses showed no difference between the quetiapine and placebo groups, HR = 0.50 (95% CI 0.05–5.55) and HR = 0.74 (95% CI 0.28–2.00) for 30- and 90-day survival, respectively. (Fig. 2) There were no reports of any adverse events during the current study period.
Subgroup analysis
Sensitivity analyses were performed according to age group and length of hospital stay. No significant interaction between any of the subgroups and treatment was found. Delirium incidences and 30- and 90-day mortalities across both tested subgroups showed no significant differences between patients who received quetiapine and placebo. (Table 3).
Discussion
Antipsychotic prophylaxis for delirium prevention has been studied in a few trials. Most of the studies have focused on surgical and postoperative or critically ill patients. However, the results remain uncertain [11, 12, 14, 26,27,28]. The evidence for the role of antipsychotics in older medical patients has also been limited. A recent study using haloperidol versus placebo in acutely hospitalized older patients in general medicine or surgical specialties showed no differences in delirium incidence [29]. To our knowledge, this is the first study focusing on quetiapine use for delirium prevention in hospitalized older medical patients.
In our study, a randomized, double-blind, placebo-controlled trial, we found no positive outcome on delirium incidence in older medical patients admitted to the hospital. The secondary outcomes were nonsignificant between both groups. This result was similar to a previous study on haloperidol prophylaxis that included both medical and surgical patients [29].
Nonetheless, our study had some limitations. First, the delirium incidence rates in both groups were only 11.4%, which were much lower than the previous reference study, which had 20–29% incidence rates [3]. This might be because of our strict inclusion and exclusion criteria and hypoactive delirium underdetection. Those who were critically ill, had terminal illnesses, had active cardiac conditions, were unable to communicate or had dementia, which are high-risk groups for delirium, were not included in our study. Moreover, we did not find any hypoactive delirium incidence. It was possible that the event was underdetected because daily assessment and medical record review might not be sensitive enough to detect all occurrences. The majority of the participants were quite physically fit, and almost all patients could ambulate before admission, mostly without gait aids. In addition, due to certain unknown effects of antipsychotics (quetiapine in this study) on this particular population, we could not obtain accurate sample numbers. Therefore, we could not reach statistical power from our expected sample calculation.
Second, the dosage and administration of the intervention drug might influence the results. In this study, we administered only 12.5 mg of quetiapine once daily, which is the initial starting dosage for older patients. Those with strong significant precipitating factors such as sepsis or deoxygenation possibly needed a higher dosage of quetiapine to prevent delirium. Moreover, once daily administration at bedtime may not be an adequate treatment due to the short half-life of quetiapine, which is typically 6 h [30].
In addition, unlike surgical or critically ill patient groups who have significant precipitating factors for delirium, our population had various medical conditions with different disease severities, which could affect delirium incidences. We did not assess or collect data about the severity of diseases, although our report on primary diagnoses showed quite similar results between the two groups. Previous comorbidities were also collected and showed no difference at baseline. In subgroup analyses, patients with longer hospitalization might have worse medical conditions; however, the results remained nonsignificant.
Finally, we did not have data on cognition. We did not collect data on cognitive testing at baseline because of unreliable interpretation in acutely ill patients. Those with previously diagnosed dementia were excluded at the beginning. Nevertheless, cognition had a great impact on delirium outcome. Older patients with cognitive impairment or dementia had a higher rate of delirium during hospital admission [3], which could possibly affect our outcomes.
Although this study did not demonstrate a benefit for quetiapine prophylaxis in preventing delirium in older adults during hospital admission, the study provokes some further questions. Further trials focusing on different antipsychotics such as olanzapine, risperidone or other medications such as trazodone with various dosages and administration methods should be conducted. The study population might be narrowed down to one specified disease with similar comorbidities or stratified into disease categories and severities to see the potential effect of the medication within different patient groups. Moreover, delirium severity should also be collected as an additional outcome which could provide a sensitive continuous measurement of delirium between the groups.
Conclusion
Our study demonstrated that quetiapine prophylaxis did not reduce the incidence of delirium in hospitalized older medical patients. The length of hospital stay, delirium duration, ICU admission, mortality and rehospitalization and mortality rates within 90 days after discharge were not significantly different between the intervention and control groups. In conclusion, quetiapine may not have benefit for preventing delirium in this population group.
Availability of data and materials
All datasets generated and analyzed during the current study are available in the figshare.com repository, https://doi.org/10.6084/m9.figshare.13182947
Abbreviations
- BMI:
-
Body mass index
- CAM:
-
Confusion Assessment Method
- CI:
-
Confidence interval
- EKG:
-
Electrocardiography
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- ITT:
-
Intention-to-treat
- kg/m2:
-
Kilogram per square meter
- mEq/L:
-
Milliequivalents per liter
- msec:
-
Millisecond
- N:
-
Number
- OR:
-
Odds ratio
- P :
-
P value
- QIR:
-
Interquartile range
- QTc:
-
Q-T corrected (corrected Q-T interval)
- SD:
-
Standard deviation
References
European Delirium Association, American Delirium Society. The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med. 2014;12(1):141. https://doi.org/10.1186/s12916-014-0141-2.
Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350–64. https://doi.org/10.1093/ageing/afl005.
Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22. https://doi.org/10.1016/S0140-6736(13)60688-1.
Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157–65. https://doi.org/10.1056/NEJMra052321.
Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, Cooney LM Jr. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–76. https://doi.org/10.1056/NEJM199903043400901.
Hshieh TT, Yue J, Oh E, Puelle M, Dowal S, Travison T, Inouye SK. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512–20. https://doi.org/10.1001/jamainternmed.2014.7779.
Martinez F, Tobar C, Hill N. Preventing delirium: should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature. Age Ageing. 2015;44(2):196–204. https://doi.org/10.1093/ageing/afu173.
Inouye SK, Baker DI, Fugal P, Bradley EH, Project HD. Dissemination of the hospital elder life program: implementation, adaptation, and successes. J Am Geriatr Soc. 2006;54(10):1492–9. https://doi.org/10.1111/j.1532-5415.2006.00869.x.
Inouye SK, Bogardus ST Jr, Baker DI, Leo-Summers L, Cooney LM Jr. The hospital elder life program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital elder life program. J Am Geriatr Soc. 2000;48(12):1697–706. https://doi.org/10.1111/j.1532-5415.2000.tb03885.x.
Hatta K, Kishi Y, Wada K, Takeuchi T, Odawara T, Usui C, Nakamura H, Group D-J. Preventive effects of ramelteon on delirium: a randomized placebo-controlled trial. JAMA Psychiatry. 2014;71(4):397–403. https://doi.org/10.1001/jamapsychiatry.2013.3320.
Oh ES, Needham DM, Nikooie R, Wilson LM, Zhang A, Robinson KA, Neufeld KJ. Antipsychotics for preventing delirium in hospitalized adults: a systematic review. Ann Intern Med. 2019;171(7):474–84. https://doi.org/10.7326/M19-1859.
Neufeld KJ, Needham DM, Oh ES, Wilson LM, Nikooie R, Zhang A, Koneru M, Balagani A, Singu S, Aldabain L et al. In: Antipsychotics for the Prevention and Treatment of Delirium. Rockville (MD); 2019.
Marcantonio ER. Delirium in Hospitalized Older Adults. N Engl J Med. 2017;377(15):1456–66. https://doi.org/10.1056/NEJMcp1605501.
Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM. Antipsychotic medication for prevention and treatment of delirium in hospitalized adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2016;64(4):705–14. https://doi.org/10.1111/jgs.14076.
Devlin JW, Roberts RJ, Fong JJ, Skrobik Y, Riker RR, Hill NS, Robbins T, Garpestad E. Efficacy and safety of quetiapine in critically ill patients with delirium: a prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med. 2010;38(2):419–27. https://doi.org/10.1097/CCM.0b013e3181b9e302.
Kim KY, Bader GM, Kotlyar V, Gropper D. Treatment of delirium in older adults with quetiapine. J Geriatr Psychiatry Neurol. 2003;16(1):29–31. https://doi.org/10.1177/0891988702250533.
Yoon HJ, Park KM, Choi WJ, Choi SH, Park JY, Kim JJ, Seok JH. Efficacy and safety of haloperidol versus atypical antipsychotic medications in the treatment of delirium. BMC Psychiatry. 2013;13(1):240. https://doi.org/10.1186/1471-244X-13-240.
Anderson SL, Vande Griend JP. Quetiapine for insomnia: a review of the literature. Am J Health Syst Pharm. 2014;71(5):394–402. https://doi.org/10.2146/ajhp130221.
Coe HV, Hong IS. Safety of low doses of quetiapine when used for insomnia. Ann Pharmacother. 2012;46(5):718–22. https://doi.org/10.1345/aph.1Q697.
Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7–21. https://doi.org/10.1097/00019442-200401000-00002.
Martins S, Fernandes L. Delirium in elderly people: a review. Front Neurol. 2012;3:101.
Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852–7. https://doi.org/10.1001/jama.1996.03530350034031.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8. https://doi.org/10.7326/0003-4819-113-12-941.
Wongpakaran N, Wongpakaran T, Bookamana P, Pinyopornpanish M, Maneeton B, Lerttrakarnnon P, Uttawichai K, Jiraniramai S. Diagnosing delirium in elderly Thai patients: utilization of the CAM algorithm. BMC Fam Pract. 2011;12(1):65. https://doi.org/10.1186/1471-2296-12-65.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. https://doi.org/10.1176/appi.books.9780890425596.
Schrijver EJ, de Graaf K, de Vries OJ, Maier AB, Nanayakkara PW. Efficacy and safety of haloperidol for in-hospital delirium prevention and treatment: a systematic review of current evidence. Eur J Intern Med. 2016;27:14–23. https://doi.org/10.1016/j.ejim.2015.10.012.
Serafim RB, Bozza FA, Soares M, do Brasil PE, Tura BR, Ely EW, Salluh JI. Pharmacologic prevention and treatment of delirium in intensive care patients: a systematic review. J Crit Care. 2015;30(4):799–807. https://doi.org/10.1016/j.jcrc.2015.04.005.
Teslyar P, Stock VM, Wilk CM, Camsari U, Ehrenreich MJ, Himelhoch S. Prophylaxis with antipsychotic medication reduces the risk of post-operative delirium in elderly patients: a meta-analysis. Psychosomatics. 2013;54(2):124–31. https://doi.org/10.1016/j.psym.2012.12.004.
Schrijver EJM, de Vries OJ, van de Ven PM, Bet PM, Kamper AM, Diepeveen SHA, van Marum RJ, van Strien AM, Anten S, Lagaay AM, Boelaarts L, Bloemers FW, Kramer MHH, Nanayakkara PWB. Haloperidol versus placebo for delirium prevention in acutely hospitalised older at risk patients: a multi-Centre double-blind randomised controlled clinical trial. Age Ageing. 2018;47(1):48–55. https://doi.org/10.1093/ageing/afx124.
AstraZeneca Pharmaceuticals LP. Seroquel full prescribing information 2013. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/020639s061lbl.pdf.
Acknowledgments
We would like to thank Thongchai Sawatmongkonkun, MD, Prapakorn Aiewmsopon, MD and Wipawee Hantrakul, MD for patient recruitment, Vittavat Termglinchan, MD and Lily Chaisompong, MD for manuscript review, Nisakron Thongmung for statistical analysis advice, residents from the Department of Medicine, Faculty of Medicine, Ramathibodi Hospital for assistance, patient observation and notification, and all nurses and staff from the observation and general medicine ward and from the emergency department for their great support and help with patient recruitment, monitoring and notification when the patient’s clinical status changed.
Funding
The study was funded by the Geriatric Medicine Fund from the Ramathibodi Foundation, Ramathibodi Hospital. This funding source had no role in the design, execution, analyses, and interpretation of the data in this study.
Author information
Authors and Affiliations
Contributions
ST contributed to concepts, designed the study, included participants, collected data, analyzed and interpreted the data and was a major contributor in writing the manuscript. SR contributed to the concepts, designed the study, interpreted the data and substantially revised the manuscript. OS contributed to the concepts, interpreted the data and substantially revised the manuscript. SC designed the study, interpreted the data and substantially revised the manuscript. PI contributed to the concepts, designed the study, analyzed and interpreted the data, drafted the work and wrote the manuscript. TN contributed to the concepts, designed the study, included participants, and collected data. LS TN contributed to the concepts, designed the study, included participants, and collected data. PC included participants, collected data, interpreted data and drafted the work. KS was a major data analysis, data interpretation and drafted the work. TA PI contributed to the concepts, designed the study, analyzed and interpreted the data, drafted the work and wrote the manuscript. All authors read and approved the final manuscript.
Authors’ information
-
1.
Saran Thanapluetiwong, MD
A geriatrician and clinical educator at the Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
2.
Sirasa Ruangritchankul
A geriatrician and clinical educator at the Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
3.
Orapitchaya Sriwannopas, MD
A geriatrician and clinical educator at the Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
4.
Sirintorn Chansirikarnjana
A geriatrician and clinical educator at the Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
5.
Pichai Ittasakul, MD
A psychiatrist and clinical educator at the Department of Psychiatry, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
6.
Tipanetr Ngamkala
A geriatric nurse at the Department of Nursing, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
7.
Lalita Sukumalin
A nurse at Ramathibodi School of Nursing, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
8.
Piangporn Charernwat
A researcher at Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
9.
Krittika Saranburut
A researcher and statistician at Cardiovascular and Metabolic Center, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
-
10.
Taweevat Assavapokee
A geriatrician and clinical educator at the Division of Geriatric Medicine, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand based on the Declaration of Helsinki on May 3, 2018, on protocol number ID 02–61-54. Informed consent forms were signed by all participants or their legal representatives before attending the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1
. Baseline laboratory characteristics (Intention-to-treat). Table 2. Baseline comorbidities (intention-to-treat). Table 3. Primary diagnosis of participants (intention-to-treat). Table 4. Baseline characteristics of delirious participants.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thanapluetiwong, S., Ruangritchankul, S., Sriwannopas, O. et al. Efficacy of quetiapine for delirium prevention in hospitalized older medical patients: a randomized double-blind controlled trial. BMC Geriatr 21, 215 (2021). https://doi.org/10.1186/s12877-021-02160-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02160-7