Abstract
Background and purpose
Chronic gastritis, especially that caused by helicobacter pylori (HP) infection, has been associated with increased risk of ischemic stroke. But the relationship between chronic gastritis and cerebral small vessel disease (CSVD) remains largely undetermined. This study aimed to determine the potential predictors for CSVD, with chronic gastritis and its proxies as alternatives.
Method
Patients aged 18 years or older with indications for electronic gastroscopy were enrolled. Presence of CSVD was evaluated with brain magnetic resonance imaging (MRI) results. Degree of CSVD was scored according to established criteria. Logistic regression analysis was used for identifying possible risk factors for CSVD.
Results
Of the 1191 enrolled patients, 757 (63.6%) were identified as with, and 434 (36.4%) as without CSVD. Multivariate analysis indicated that patients with chronic atrophic gastritis had an increased risk for CSVD than those without (adjusted odds ratio = 1.58; 95% CI, 1.08–2.32; P < 0.05).
Conclusions
Chronic atrophic gastritis is associated with the presence of CSVD. We should routinely screen the presence of CSVD for patients with chronic atrophic gastritis.
Similar content being viewed by others
Introduction
The neuroimaging markers of cerebral small vessel disease (CSVD) include white matter hyperintensities (WMH), lacunes, enlarged perivascular spaces (EPVS) and cerebral microbleeds (CMBs) [1]. As a subtype of ischemic stroke, CSVD is responsible for about a fifth of stroke incidence. Coexistence of CSVD usually deteriorate stroke outcomes of other subtypes [2, 3]. CSVD is a major cause of cognitive decline and dementia in elderly, second only to Alzheimer disease [4]. But the etiology of CSVD has been far from being determined to date.
CSVD has been associated with markers of inflammation. Previous studies associated WMH and EPVS with vascular inflammation and endothelial dysfunction in stroke patients [5,6,7]. A cross-sectional study showed that infectious burden consisting of multiple common pathogens was associated with CMBs [8]. On the other hand, some studies failed to associate lacunes or their markers with systemic inflammation [9, 10]. Recent studies indicated that chronic gastritis, especially that caused by HP infection, were related to ischemic stroke [11,12,13]. HP can lead to gastric mucosal injury and other gastric diseases, both of which may enhance systemic inflammatory reaction, and, therefore, increase the risk of stroke [13]. On the other hand, HP infection may likely influence gastric physiology and absorption of micronutrients such as folate and vitamin B12. Deficiency of folate and vitamin B12 may increase serum homocysteine level and causes vascular damage [14].
Although chronic gastritis has been proved to affect the risk of stroke occurrence and recurrence, whether chronic gastritis increases the risk of CSVD is largely undetermined. This study aimed to explore the relationship between chronic gastritis and the risk of CSVD.
Methods
Data source
Patients were screened from Affiliated Jiangning Hospital with Nanjing Medical University. The present study is part of a longitudinal study on the long-term mortality of middle-aged and elderly from Jinling Hospital, Nanjing Medical University. Patients hospitalized for physical examination aged 18 years or older with indications (including gastralgia, gastric distention, nausea, vomiting, acid reflux, nausea, constipation, and diarrhea or voluntary gastroscopy) for electronic gastroscopy were enrolled from January 1, 2011 to May 18, 2020, and patients who agreed to underwent brain magnetic resonance imaging (MRI) examination within 48 h after admission were finally included in the study. Patients with acute gastrointestinal bleeding, acute cardiovascular diseases, pulmonary insufficiency, coagulation disorders and cancer were excluded (Fig. 1).
Risk factor definitions
Risk factors were defined as the following. In this study, hypertension was defined as a blood pressure that exceeds 140/90 mm of mercury. The definition of diabetes was either being diagnosed with diabetes, or having fasting glucose levels exceeding 7.0 mmol/L. Hyperlipidemia was defined as a documented diagnosis of hyperlipidemia or on lipid-lowering medications. The presence of a previous episode of coronary heart disease or an attack of coronary heart disease at the time was considered a history of coronary heart disease. History of stroke was defined as the experience of ischemic stroke. The diagnosis of atrial fibrillation was made based on electrocardiographic evidence or self-reported physician diagnosis.
Clinical laboratory tests
Demographic and clinical data were collected. Red blood cell counting and biochemical examinations were performed before gastroscopy examination. Presence of gastric diseases was determined according to clinical characteristics, pathological changes and gastroscopy results. Endoscopy combined with histopathological examination was used to diagnose two types of gastritis: chronic non-atrophic gastritis and chronic atrophic gastritis [15]. HP infection were determined with carbon 14 urea breath test.
Neuroimaging evaluation
Enrolled patients underwent brain MRI examination with a 3.0 T scanner (Philips Medical Systems, Netherlands) with an 8-channel receiver array head coil. Head motion and scanner noise were reduced using foam padding and earplugs. Standardized parameters of the MRI sequences, including T1-weighted, T2-weighted and fluid-attenuated inversion recovery images were obtained. Burden of CSVD was graded as 0–4 based on imaging markers (WMH, lacunes, EPVS and CMBs) on MRI according to established criteria [16,17,18]. Briefly, one point represents each of the following phenomenon: more than 10 EPVS in basal ganglia, presence of lacuna, periventricular WMH with a Fazekas score of 3 or deep WMH with a Fazekas score of 2 or 3, presence of deep CMBs. Patients were then grouped as with (1–4 points) and without CSVD (0 points).
Gastroscopy examination
Gastroscopy examination was performed with an endoscope (GIF-HQ290, GIF-H290Z; Olympus Medical Systems, Tokyo, Japan) with video processors (EVIS LUCERA ELITE CV290/CLV290SL, Olympus Medical Systems). Five gastric mucosa tissue specimens, two from gastric antrum, two from gastric body and one from gastric corner were clamped during gastroscopy examination for biopsy. Chronic inflammation, atrophy and intestinal metaplasia were diagnosed according to the Sydney system [19].
Statistics
Continuous data were summarized as mean values with SDs for normal distribution or median value with interquartile range for skew distribution. Categorical data were presented as frequencies with proportions. Two-sample t test was used to compare continuous data. Categorical data were analyzed by the chi-square test. Logistic univariate and multivariate analyses were used for comparing group differences and identifying the risk factors of CSVD. All statistical analyses were performed using SPSS 25.0 (IBM, Armonk, NY).
Results
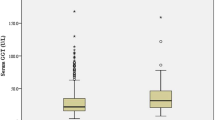
Of the 1191 enrolled patients, 757 (63.6%) were identified as with, and 434 (36.4%) as without CSVD. Patients with CSVD were older than those without (58.6 ± 9.9 vs 50.2 ± 9.4; P < 0.001). Patients with CSVD presented lower hemoglobin concentration than those without (137.3 ± 23.8 vs 140.3 ± 16.8 g/L; P < 0.05). Patients with CSVD had a higher prevalence of hypertension (48.0% vs 29.5%; P < 0.001), diabetic mellitus (19.4% vs 11.5%; P < 0.001), coronary artery disease (9.8% vs 3.9%; P < 0.001) and chronic atrophic gastritis (21.1% vs 12.0%; P < 0.001) than control subjects. Conversely, patients with CSVD had a lower prevalence of hyperlipidemia (7.7% vs 22.8%; P < 0.001) than patients without CSVD. CSVD patients had a higher ratio of history of ischemic stroke (25.4% vs 3.0%; P < 0.001) than patients without (Table 1).
After adjusting for covariates, logistic regression analysis identified chronic atrophic gastritis was related to CSVD (adjusted odds ratio = 1.58; 95% CI: 1.08–2.32; P < 0.05). Age (adjusted odds ratio = 1.07; 95% CI: 1.06–1.09; P < 0.001) and previous ischemic stroke (adjusted odds ratio = 7.45; 95% CI: 3.98–13.93; P < 0.001) were also associated with CSVD (Fig. 2).
Association of chronic atrophic gastritis and CSVD presence. OR, odds ratio; CI, confidence interval. Risk of CSVD was analyzed with logistic regression models, and OR was generated. We adjusted for Age, Hypertension, Diabetes, Hyperlipidemia, Coronary artery disease, Previous ischemic stroke, Atrial fibrillation and Hemoglobin concentration in regression model 1
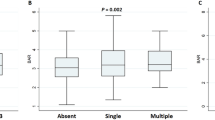
When patients were stratified, the results showed that patients with chronic atrophic gastritis presented significantly higher total CSVD scores than those without (1.8 ± 0.8 vs 1.5 ± 0.9, P < 0.01).The ratios of EPVS (37.9% vs 23.1%; P < 0.01) and lacunes (70.6% vs 56.5%, P < 0.01) in patients with chronic atrophic gastritis were significantly higher than patients without chronic atrophic gastritis. This result suggests that the difference in the total CSVD burden is mainly derived from EPVS and lacunes (Fig. 3).
Discussion
This study found that chronic atrophic gastritis was related to CSVD and the difference in the total CSVD burden is mainly derived from EPVS and lacunes.
Compared with patients with CSVD, the proportion of hyperlipidemia in non-CSVD patients is higher, this is contrary to previous studies [20, 21]. Hyperlipidemia has been identified as a risk factor for atherosclerosis and one potential candidate risk factor for CSVD, this may be related to the intake of lipid-lowering drugs and influence of different daily life habits and activities. The traditional risk factors are only able to partially explain the presence of CSVD [22], and the incomplete understanding of the pathogenesis of CSVD limits prevention and treatment efforts. Therefore, obtaining more predictors of progression is a rational target for therapeutic treatments. In recent years, some potential new risk factors of CSVD, including chronic infection and substance abuse, have attracted the attention of scholars [23], the discovery of these new risk factors provides new thinking for the prevention and treatment of CSVD patients.
Our study revealed the higher prevalence of CSVD in patients with chronic atrophic gastritis than those without even after adjustments for multiple confounding factors. This may be related to the following factors. Firstly, chronic atrophic gastritis is an organ-specific autoimmune disease, which affects the corpus-fundus gastric mucosa [24]. The decrease or disappearance of parietal cells results in reduced or absent acid production and loss of intrinsic factor, and it further interferes with the absorption of folate and vitamin B12 [25], and further lead to anemia and hyperhomocysteinemia. Deficiency of folate can result in hyperhomocysteinemia, which is a possible risk factor for cardiovascular diseases [26]. One meta-analysis indicated a 10% lower risk of stroke and a 4% lower risk of overall CSVD with folate supplementation [27]. The results of the China Stroke Primary Prevention Trial (CSPPT) randomized clinical trial among adults with hypertension in China showed that folate supplementation could significantly reduce the risk of first stroke [28]. Moreover, hyperhomocysteinemia has been recognized as an important risk factor for cardiovascular diseases. It may also involve in the development of dementia, diabetes mellitus, and renal disease [29]. A controlled study showed that hyperhomocysteinemia may increase the risk of lacunar infarction and severe white matter lesion [30].
There are several limitations in the current study. First, this is an observational study without further follow-up and dynamic observation of the progress of CSVD. Second, this study is based on clinical observation. Further studies are needed to explore the possible mechanisms. Third, this study is a single-center study involving individuals in the Han population in a single center. Therefore, further multicenter studies are needed to overcome these limitations.
Conclusions
The results of this study suggested that patients with chronic atrophic gastritis may have increased risk of CSVD. We should routinely screen the presence of CSVD for patients with chronic atrophic gastritis.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author, upon reasonable request.
Abbreviations
- CSVD:
-
Cerebral small vessel disease
- HP:
-
Helicobacter pylori
- WMH:
-
White matter hyperintensities
- EPVS:
-
Enlarged perivascular spaces
- CMBs:
-
Cerebral microbleeds
- CSPPT:
-
China Stroke Primary Prevention Trial
References
Wiegertjes K, Ter Telgte A, Oliveira PB, et al. The role of small diffusion-weighted imaging lesions in cerebral small vessel disease. Neurology. 2019;93:e1627–34.
Wardlaw JM, Smith C, Dichgans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. The Lancet Neurology. 2013;12:483–97.
Georgakis MK, Duering M, Wardlaw JM, Dichgans M. WMH and long-term outcomes in ischemic stroke: a systematic review and meta-analysis. Neurology. 2019;92:e1298–308.
Gorelick PB, Scuteri A, Black SE, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:2672–713.
Low A, Mak E, Rowe JB, Markus HS, O’Brien JT. Inflammation and cerebral small vessel disease: a systematic review. Ageing Res Rev. 2019;53: 100916.
Rouhl RPW, Damoiseaux JGMC, Lodder J, et al. Vascular inflammation in cerebral small vessel disease. Neurobiol Aging. 2012;33:1800–6.
Aribisala BS, Wiseman S, Morris Z, et al. Circulating inflammatory markers are associated with magnetic resonance imaging-visible perivascular spaces but not directly with white matter hyperintensities. Stroke. 2014;45:605–7.
Fan F, Yang C, Zhu X, et al. Association between infectious burden and cerebral microbleeds: a pilot cross-sectional study. Ann Clin Transl Neurol. 2021;8:395–405.
Staszewski J, Piusińska-Macoch R, Brodacki B, Skrobowska E, Stępień A. IL-6, PF-4, sCD40 L, and homocysteine are associated with the radiological progression of cerebral small-vessel disease: a 2-year follow-up study. Clin Interv Aging. 2018;13:1135–41.
Walker KA, Power MC, Hoogeveen RC, et al. Midlife systemic inflammation, late-life white matter integrity, and cerebral small vessel disease: the atherosclerosis risk in communities study. Stroke. 2017;48:3196–202.
Doheim MF, Altaweel AA, Elgendy MG, et al. Association between Helicobacter Pylori infection and stroke: a meta-analysis of 273,135 patients. J Neurol. 2021;268:3238–48.
Jiang J, Chen Y, Shi J, Song C, Zhang J, Wang K. Population attributable burden of Helicobacter pylori-related gastric cancer, coronary heart disease, and ischemic stroke in China. Eur J Clin Microbiol Infect Dis. 2017;36:199–212.
Shindler-Itskovitch T, Chodick G, Shalev V, Muhsen K. Helicobacter pylori infection and prevalence of stroke. Helicobacter. 2019;24: e12553.
Ren JR, Ren SH, Ning B, et al. Hyperhomocysteinemia as a risk factor for saccular intracranial aneurysm: a cohort study in a Chinese Han population. J Stroke Cerebrovasc Dis. 2017;26:2720–6.
Tang D, Wang L, Ling T, et al. Development and validation of a real-time artificial intelligence-assisted system for detecting early gastric cancer: a multicentre retrospective diagnostic study. EBioMedicine. 2020;62:103146–103146.
Lau KK, Li L, Schulz U, et al. Total small vessel disease score and risk of recurrent stroke: validation in 2 large cohorts. Neurology. 2017;88:2260–7.
Du H, Wilson D, Ambler G, et al. Small vessel disease and ischemic stroke risk during anticoagulation for atrial fibrillation after cerebral ischemia. Stroke. 2021;52:91–9.
Xiao L, Lan W, Sun W, et al. Chronic kidney disease in patients with lacunar stroke: association with enlarged perivascular spaces and total magnetic resonance imaging burden of cerebral small vessel disease. Stroke. 2015;46:2081–6.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. the updated Sydney system. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–81.
Warsch JR, Wright CB. Stroke: hyperlipidemia and cerebral small-vessel disease. Nat Rev Neurol. 2010;6:307–8.
Kraft P, Schuhmann MK, Garz C, et al. Hypercholesterolemia induced cerebral small vessel disease. PLoS ONE. 2017;12: e0182822.
Wardlaw JM, Allerhand M, Doubal FN, et al. Vascular risk factors, large-artery atheroma, and brain white matter hyperintensities. Neurology. 2014;82:1331–8.
Zhou LW, Panenka WJ, Al-Momen G, et al. Cerebral small vessel disease, risk factors, and cognition in tenants of precarious housing. Stroke. 2020;51:3271–8.
Massironi S, Zilli A, Elvevi A, Invernizzi P. The changing face of chronic autoimmune atrophic gastritis: an updated comprehensive perspective. Autoimmun Rev. 2019;18:215–22.
Neumann WL, Coss E, Rugge M, Genta RM. Autoimmune atrophic gastritis–pathogenesis, pathology and management. Nat Rev Gastroenterol Hepatol. 2013;10:529–41.
Mangoni AA, Jackson SH. Homocysteine and cardiovascular disease: current evidence and future prospects. Am J Med. 2002;112:556–65.
Li Y, Huang T, Zheng Y, Muka T, Troup J, Hu FB. Folic acid supplementation and the risk of cardiovascular diseases: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2016;5(8):e003768.
Huo Y, Li J, Qin X, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. 2015;313:1325–35.
Rodriguez-Castro KI, Franceschi M, Noto A, et al. Clinical manifestations of chronic atrophic gastritis. Acta Biomed. 2018;89:88–92.
Cao L, Guo Y, Zhu Z. Effects of hyperhomocysteinemia on ischemic cerebral small vessel disease and analysis of inflammatory mechanisms. Int J Neurosci. 2021;131:362–9.
Acknowledgements
Not applicable.
Funding
This research was supported by the Fund of Nanjing Medical Science and technique Development Foundation (YKK22216); Jiangning District Science and Technology Huimin Project (2022092S).
Author information
Authors and Affiliations
Contributions
GLX, JRL and ZLX contributed to the study design. Data collection was performed by CSW, CT, XMZ and XS. XMZ, CSW and CT were responsible for data analysis and imaging evaluation. The manuscript was written by CSW and GLX. All authors approved the final manuscript for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of Jinling Hospital (approval number 2010NLY-018) and all methods were performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all study participants.
Consent for publication
All patients gave informed consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, C., Tan, C., Zhang, X. et al. Chronic gastritis may predict risk of cerebral small vessel disease. BMC Gastroenterol 23, 429 (2023). https://doi.org/10.1186/s12876-023-03009-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-03009-6