Abstract
Background
ColoDefense1.0 assay has demonstrated its excellent sensitivity and specificity for early detection of colorectal cancer (CRC) by detecting the methylation levels of SDC2 and SEPT9, while exhibited limitations on relatively large sample capacity required and limited detection throughput by applying triplicate PCR reactions for each sample. In this study, ColoDefense1.0 was simplified and optimized into ColoDefense2.0 in a single PCR reaction.
Methods
A total 529 stool specimens were collected, and 244 CRC patients, 34 patients with advanced adenomas (AA), 64 with small polyps (SP) and 187 control subjects were divided in training and validation cohorts. Methylation levels of SEPT9 and SDC2 were examined by qPCR reactions in triplicate or single.
Results
The stool DNA quantity stored in preservative buffer at 37 °C up to 7 days exhibited no significant decrease. In the training cohort, when the number of replicates reduced from 3 to 1, the overall performance of ColoDefense2.0 was identical to that of ColoDefense1.0, showing sensitivities of 71.4% for AA and 90.8% for all stage CRC with a specificity of 92.9%. In the validation cohort, sensitivities of SP, AA and CRC using ColoDefense2.0 were 25.0%, 55.0% and 88.2%, increased from 14.1% (20.3%), 40.0% (40.0%) and 79.4% (67.6%) using SDC2 (SEPT9) alone; along with an overall specificity of 90.2%, decreased from 94.1% (95.1%) using SDC2 (SEPT9) alone.
Conclusion
The simplified ColoDefense test maintained the overall performance while reduced the number of PCR reactions to 1/3, and provided an effective and convenient tool to detect early CRC and precancerous lesions and potentially improve the compliance of screening.
Similar content being viewed by others
Introduction
Globally, colorectal cancer (CRC) is the third most commonly diagnosed cancer and the second leading cause of cancer death, with over 1.9 million new cases and 0.9 million death estimated to occur in 2020, contributing to 10.0% of new cancer cases and 9.4% of cancer deaths [1]. Participation in CRC screening and removal of adenomatous polyps can significantly reduce the mortality and incidence of CRC. For example, colonoscopy prevalence in the U.S. adults of 50 years or older has increased from 20 to 61% from 2000 to 2018, contributing to the significantly decreased incidence rate from approximately 185 to 115 per 100,000 population in the U.S [2]. However, such high colonoscopy prevalence is difficult to reach in developing countries or in the COVID-19 pandemic, due to insufficient availability in medical resources, limited awareness, invasiveness and bothersome bowel preparation [3]. In this light, a number of noninvasive methods as preliminary screening strategies have been developed, such as high-risk factor questionnaire, fecal occult blood test (FOBT), fecal immunochemical test (FIT), plasma or stool DNA tests, with the objectives to improve the compliance of screening and to screen out high-risk population for diagnosis and treatment [4,5,6,7]. Our team previously has developed a cell-free DNA (cfDNA) test, ColoDefense1.0, that detected methylated SEPT9 and SDC2 simultaneously in a multiplex qPCR assay, exhibiting outstanding sensitivities of 92.3% for all stage CRC and 66.7% for AA with a specificity of 93.2% in stool samples, and sensitivities of 88.9% for CRC and 47.8% for AA with a specificity of 92.8% in plasma samples [8, 9]. These results demonstrated the potential of ColoDefense1.0 to become an effective and accurate tool for early detection of CRC.
Due to trace amount of cfDNA in the stool or plasma samples in detecting CRC, it is a common practice to apply multiple PCR reactions in a test to improve the detection accuracy. Oh et al. reported a blood-based qPCR assay detecting SDC2 methylation that was run in triplicate, and then a stool-based quantitative methylation-specific real time PCR (qMSP) method that implemented consecutive two rounds of PCR reactions to detect the methylation of SDC2 [10, 11]. Epi proColon, the first blood-based assay approved by FDA on methylation of SEPT9, were run in triplicate and exhibited a sensitivity of 22% for AA, 68% for all stages of CRC [12]. This assay was then applied in a prospective study using triplicate PCR reactions, resulting in a sensitivity of 48.2% for all stage CRC [13]. Our previous study applied and compared 2/3 and 3/3 rules in detecting methylated SFRP2 and SDC2 in stool to optimize the cut-off values, resulting in sensitivities of 61.5% for detecting AA and 88.5% for early stage CRC (stage 0-II) by 2/3 rule [14]. A triplicated PCR reaction was applied in ColoDefense1.0 as well. However, it is obvious that the detection throughput would be limited by multiple repetitions in PCR reactions. Therefore, this study aims to simplify and optimize ColoDefense1.0 assay in stool samples to a single PCR reaction.
Materials and methods
Sample collection
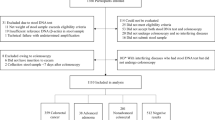
In this study, we enrolled 584 participants who underwent colonoscopy due to visited outpatient clinics or physical examination from two hospitals including two independent cohorts (Additional file 1: Fig. S1). The inclusion criteria consisted of the following: aged 18 or older, no history of CRC, nonpregnant, having colonoscopy results, and participants with abnormal colonoscopy results should have pathological diagnosis results. During stool sample collection, efforts were made to avoid transferring urine into the collection tube, and diarrhea samples were not collected. The exclusion criteria were as follows: other gastrointestinal malignancies, unable or unwilling to accept colonoscopy, missing or incomplete sample information, insufficient or excessive stool volume, repeated sampling, and insufficient DNA indicated by low ACTB levels (see Data Analysis). After excluding unqualified samples, training cohort collected at the Affiliated Hospital of Xuzhou Medical University included 142 CRC patients, 14 patients with advanced adenomas (AA, an adenoma with size ≥ 1.0 cm, significant villous features (> 25%) or high-grade dysplasia) and 85 control subjects who underwent colonoscopy for data analysis (Additional file 1: Fig. S1). The validation cohort included 102 CRC patients, 20 AA patients, 64 small polyp (SP, an adenoma < 10 mm in size without high-grade dysplasia and villous histologic features, or hyperplastic polyp < 10 mm in size) patients, and 102 control subjects collected at the Kunshan Hospital of Traditional Chinese Medicine (Additional file 1: Fig. S1). The control subjects enrolled in training and validation cohorts included diverticula, colitis and subjects with no evidence diseases. Training cohort was used for optimizing cut-off value, and the validation cohort was used for verifying the cut-off value, the colonoscopy and pathological results in validation cohort was blinded for laboratory staff. Stool samples (approximately 5 g) were collected before purgative bowel preparation or colonoscopy by using the single-use disposable buckets from Suzhou VersaBio Technologies Co., Ltd., and then each stool specimen was transferred into a 50 mL tube containing 25 mL of preservative buffer (Suzhou VersaBio Technologies Co., Ltd., Kunshan, China). All stool samples were stored at room temperature for no more than 7 days or at − 80 °C for longer-term storage before usage. This study was approved by the Institutional Review Board of the Affiliated Hospital of Xuzhou Medical University and Kunshan Hospital of Traditional Chinese Medicine, and the informed consent was obtained for all participating patients and control subjects.
Stool DNA stability study
The aim of this procedure was to investigate the efficiency of preservative buffer during stool sample collection and transportation. Two stool samples were collected from each of 10 healthy donors, one sample collected in a tube containing 25 mL preservative buffer (PS) and the other in 25 mL deionized water (DS). Each sample was transfer to the laboratory within 2 h from collection. The human genomic DNA for PS were extracted immediately, and then the remaining PS and DS were stored at 37 °C (approximately the highest average temperature in summer). The DS were processed for human genomic DNA extraction after 2 h and the remaining PS were processed for human genomic DNA extraction at 1, 3 and 7 days. Next, all stool DNAs were bisulfite-treated and detected by ACTB qPCR reaction.
The simplified assay
We named the simplified assay as “ColoDefense2.0”. Compared to the original assay (ColoDefense1.0), 3 PCR replicates were reduced to 1 PCR replicate in ColoDefense2.0, and the reaction volume was increased from 30 to 50 μL. The cut-off value for ColoDefense2.0 was set as follows: the stool sample was considered ‘invalid’ if the ACTB Ct value was greater than 43.0, the optimized cut-off values for methylated SEPT9 and SDC2 were Ct values less than 38.0 and 40.0, respectively (Additional file 2: Table S1), and a stool sample would be scored positive when any methylated marker was scored positive.
DNA extraction, bisulfite treatment and methylation detection
Stool samples were homogenized and centrifugated, and 150 μL supernatants were transferred for human genomic DNA extraction by using a Versa-Autopure Nucleic Acid Purification System (Suzhou VersaBio Technologies Co., Ltd., Kunshan, China). All samples underwent lysis and two washing steps and were finally eluted in 100 μL of elution buffer. Bisulfite treatment of purified DNA were performed with a fast bisulfite conversion kit (Suzhou VersaBio Technologies Co., Ltd.) according to previous study [8]. The purification of the converted products also using the Versa-Autopure Nucleic Acid Purification System by three washing steps and were finally eluted in 100 μL of elution buffer.
The methylation detection of ColoDefense1.0 according to the published procedure [8], and ColoDefense2.0 test include 25 µL template and 25 µL PCR master mix. Both ColoDefense1.0 and ColoDefense2.0 were analyzed on LC480-II thermal cycler (Roche Diagnostics, Basel, Switzerland) using the following cycling conditions: activation at 95 °C for 30 min, 50 cycles of 95 °C for 10 s, 56 °C for 30 s, and final cooling to 40 °C for 30 s.
Analytical performance of the simplified assay
To determine the limit of detection (LoD) for two methylated markers in ColoDefense2.0, fully methylated genomic DNA were diluted into unmethylated genomic DNA (1:100, w/w) to create mixtures. For SDC2, fully methylated genomic DNA with concentration gradient of 50 pg/reaction, 25 pg/ reaction and 12.5 pg/reaction tested, and each reaction was considered positive based on ColoDefense2.0 cut-off value. For SEPT9, fully methylated genomic DNA with concentration gradient of 200 pg/reaction, 100 pg/ reaction and 50 pg/reaction tested, and each reaction was considered positive based on ColoDefense2.0 cut-off value. Meanwhile, 20,000 pg/reaction fully unmethylated genomic DNA was used for analyzing the LOB (Limit of Blank) of the test. Each concentration sample was repeated for 20 times.
Data analysis
For ColoDefense1.0, Mean Ct values for each methylated marker were used for plotting receiver operating characteristic (ROC) curves, and the Ct values for ColoDefense2.0 were used for plotting ROC curves. The confidence interval (CI) of an area under the curve (AUC) was calculated. For those subjects without amplification signals in qPCR reaction, their Ct values were set to 50 (the maximal number of PCR cycles).
Results
A total of 529 participants were enrolled and their characteristics are shown in Table 1. Among all participants, 244 were CRC patients (including 8 of stage 0, 39 stage I, 72 stage II, 80 stage III, 23 stage IV and 22 of unknown stage), 98 patients having polyps (including 34 AA patients and 64 SPs), and 187 normal controls. Percentages of male patient, median and range of age at diagnosis for CRC patients was 56.3%, 63, 20–84 in the training cohort, comparable to those in the validation cohort (54.9%, 61, 27–89). However, the age distribution for control subjects was younger than that of the CRC patients in both training cohort and validation cohort (Additional file 2: Table S2).
Stool DNAs in samples collected without preservative buffer showed a drastic degradation after 2 h at 37 °C, and no amplification signal was detected in any samples, as shown in Fig. 1. From fresh (0 day) to 7 days, Ct values of ACTB from samples in preservative buffer exhibited no significant increase, which validated that no significant degradation of stool DNA and the stability of stool DNA was successfully preserved at 37 °C for at least a week.
To evaluate the limit of detection for methylated SDC2 and SEPT9 alone, methylated human genomic DNA with different concentrations were tested for 20 replicates. As shown in Table 2, ColoDefense2.0 was able to detected SDC2 and SEPT9 at a concentration of 25 and 100 pg/reaction at 100% positive rate, respectively. And neither methylated SDC2 or SEPT9 showed positive signals in fully unmethylated human genomic DNA.
The cut-off value for ColoDefense2.0 was optimized based on the Youden index by using the samples from the training cohort (Additional file 2: Table S1). In order to acquire the best accuracy, we set a minimum sensitivity and specificity of not less than 85%. And the results indicated that when setting the cut-off Ct value of SEPT9 as 38.0 and that of SDC2 as 40.0, the ColoDefense2.0 would achieve the best Youden index of 83.7% (Additional file 2: Table S1). Therefore, the subsequent data were analyzed with this cut-off value. In the training cohort, consistent performance of ColoDefense1.0 and ColoDefense2.0 was maintained when reducing the number of replicates from 3 to 1, as shown in Fig. 2 Using SDC2 alone (Fig. 2A), the sensitivities of AA increased from 57.1 to 64.3%, and that of CRC slightly decreased from 87.3 to 86.6%. Meanwhile, the sensitivities of AA dropped from 50.0 to 42.9%, and that of CRC slightly decreased from 82.4 to 79.6% by using SEPT9 alone (Fig. 2B). Specificities of both single methylated genes were 96.5% by either ColoDefense test kit, showing an excellent performance on avoiding false positive. As shown in Fig. 2C, the overall performance of ColoDefense1.0 and ColoDefense2.0 was identical in this cohort: the sensitivities for AA and CRC increased to 71.4% and 90.8%, and the specificity was slightly compensated to 92.9%, comparing to those from single methylated genes. Considering the unbalance of age distribution between CRC and control subjects, we excluded the control subjects younger than 40 years old and re-analyzed the specificity, resulting in a specificity of 90.9% (Additional file 2: Table S3).
For each stage of CRC, the performance of two version of ColoDefense kits were maintained as well (Fig. 3). The sensitivities by SDC2 in ColoDefense2.0 showed in significant increase of 9.1% for stage IV and minor fluctuations for other stages (Fig. 3A), and those by SEPT9 showed slight decrease for stage I to IV up to 9.1%, and an increase for unknown stage by 4.6% (Fig. 3B). The overall sensitivities of ColoDefense2.0 (increment from ColoDefense1.0) was 66.7% (0), 94.7% (0), 87.0% (0), 92.7% (− 2.4%), 100% (+ 9.1%), 90.0% (0) for stage 0 to IV and unknown, respectively. Since the number of patients was larger in stage III than that of stage IV, the fluctuation on sensitivities offset each other, leading to the same overall performance of two ColoDefense kits in this cohort.
Furthermore, AUC of ColoDefense1.0 and ColoDefense2.0 demonstrated no significant differences, as shown in Fig. 4. For ColoDefense1.0 (Fig. 4A), AUCs for SDC2 and SEPT9 were 0.948 (95% CI 0.910-0.973) and 0.934 (95% CI 0.893–0.962), respectively, and increased to 0.964 (95% CI 0.931–0.984) if combined. AUCs for ColoDefense2.0 showed no significant change (Fig. 4B), which were 0.945 (95% CI 0.907–0.971), 0.930 (95% CI 0.889–0.960), and 0.959 (95% CI 0.924–0.980) for SDC2, SEPT9 and combined, respectively.
In the validation cohort, the combination of SDC2 and SEPT9 exhibited a significant improvement of sensitivities, especially for precancerous lesions and early stage CRC. As shown in Fig. 5A, comparing to SDC2 (SEPT9) alone, the combined sensitivities of SP, AA and CRC of all stages were increased to 25.0%, 55.0%, 88.2% from 14.1% (20.3%), 40.0% (40.0%), 79.4% (67.6%), respectively. And the combined sensitivities for stage 0 to IV (Fig. 5B) were improved to 100.0%, 90.0%, 88.5%, 84.6% and 91.7% from 80.0% (80.0%), 65.0% (70.0%), 84.6% (76.9%), 84.6% (56.4%) and 75.0% (75.0%), respectively. Moreover, the sensitivity of SDC2 in detecting CRC were 11.8% higher than that of SEPT9 alone, and a 3.9% to 4.9% decrease in specificity was observed if two methylated genes were combined. Meanwhile, the specificity in the validation cohort would further decrease to 85.9% if excluding control subjects younger than 40 (Additional file 2: Table S3).
The ROC curves of SDC2, SEPT9 and combined in ColoDefense2.0 in the validation cohort was shown in Fig. 6, AUC values were 0.897 (95% CI 0.847–0.935), 0.898 (95% CI 0.848–0.936) for SDC2 and SEPT9, respectively, and increased to 0.944 (95% CI 0.903–0.971) if combined, all of which were comparable to those in the training cohort. The improvement clearly demonstrated the advantage of optimized multi-target detection.
Discussion
Screening and early diagnosis of CRC is essential to reduce the incidence and mortality in the long term. A study in 2015 estimated that about 63% of CRC deaths in the US may be attributed to non-screening [15]. Since the screening strategies such as the FOBT and colonoscopy were recommended in 1996–1997 and benefit covered in 2001 in the US, the incidence and mortality have been declining in recent decades [16]. Implementation of screening was considered to attribute to a 50% reduction in CRC incidence and death rate by modeling studies [17]. However, many countries and regions suffered from low participation and compliance rate despite significant benefits from screening, due to limited per capita medical infrastructure and staff, healthcare coverage, awareness and education for patients and providers. Therefore, strategies that provide satisfying accuracy and convenience for both participants and laboratories in relatively low cost and high throughput would be ideal for preliminary screening of CRC. In this study, we optimized a multiplex methylated DNA testing in a single PCR reaction, ColoDefense2.0, providing a potential tool for effective and higher throughput CRC screening.
Multiplex methylated DNA testing for CRC screening has its unique advantage over multiomics tests or single methylation tests. Multiomic tests for CRC screening was developed to achieve improved accuracy for CRC. Cologuard, a stool DNA test including methylated NDRG4 and BMP3, 7 KRAS mutations with a hemoglobin immunoassay, reported sensitivities of 42.4% for AA, 69.2% for HGD and 92.3% for all stage CRC, and a specificity of 89.8% from 9989 participants [18]. Such test gained its popularity among insured population in the U.S. due to its effectiveness and convenience. However, high complexity of processing associated with mulitiomics detections has led to a price as high as $649, which could be a major reason to hinder its popularity among uninsured people or in developing countries. Other than multiomic tests, several single-target methylation detection approaches have been launched in succession. However, limitations, such as limited sensitivity for all stages of CRC of SEPT9 in plasma (68% [12]), decreased sensitivity of stool SDC2 for late stage CRC (75.6% for stage IV [19]), were observed in these studies. Alternatively, multiplex methylated DNA testing for CRC detection have been developed to achieve improved sensitivity for CRC and for precancerous lesions, with a possible sacrifice of specificity. A recent study on a dual-target stool DNA test (methylated SDC2 and TFPI2) showed a sensitivity of 95.31% for CRC, exceeding the performance of either target alone. Meanwhile, its specificity was reduced from 100% by SDC2 alone to 96.67% in dual-target test [20]. Similar trends were observed in this study, the sensitivities of CRC increased from 79.4% by SDC2 and 67.6% by SEPT9 alone to 88.2% in combined. The sensitivities of SP and AA increased significantly from 14.1% (20.3%) and 40.0% (40.0%) for SDC2 (SEPT9) alone to 25.0% and 55.0% in combination, while the specificity reduced to 90.2% from 94.1% and 95.1% by SDC2 and SEPT9 alone. In addition, our multiplex PCR further reduced the cost and increased the detection throughput.
A triplicate PCR reaction was a common strategy to achieve an overall best performance, aiming to achieve a desirable balance between sensitivity and specificity in addition to the cut-off value optimized by Youden index. However, our study demonstrated that such replicates can be optimized and simplified to a single PCR reaction without loss of accuracy. Oh et al. reported that a blood-based test detecting SDC2 methylation in triplicate demonstrated a sensitivity of 87.0% for CRC from 131 patients with a specificity of 95.2% from 125 healthy participants [11]. The blood-based assay Epi proColon was designed to run in triplicate and exhibited a sensitivity of 22% for AA, 68% for all stages of CRC and 64% for stage I-III CRC, with a specificity of 80.0% from a screening population [12]. A triplicate PCR reaction was also applied in a prospective study of methylated SEPT9 in plasma from 7941 participants, yielding a sensitivity of 48.2% for all stage CRC, and 35.0%, 63.0%, 46.0% and 77.4% for stage I–IV, respectively, with a specificity 91.5% [13]. Our previous study applied and compared 2/3 and 3/3 rules in detecting methylated SFRP2 and SDC2 in stool to optimize the cut-off values, resulting in sensitivities of 89.1% and 88.5% with specificities of 93.5% and 89.5% in the training and validation cohorts, respectively [14]. In this study, we showed that the sensitivities of ColoDefense2.0 for detecting AA, early stage (0–II) CRC, late stage (III–IV) CRC and unknown stage CRC in the training cohort were 71.4% (10/14), 88.3% (60/68), 94.2% (49/52) and 90.9% (20/22), respectively, with a specificity of 92.9% (79/85), all of which happened to be the same as those of ColoDefense1.0 in triplicate. The sensitivities of ColoDefense2.0 for stage I–IV CRC were 1.7% higher than that from the training cohort in our previous study, and a minor reduction of 0.6% in specificity was also observed. These results implied that the impact of technical replicates in our tests was negligible, and a well-performed strategy was established. More importantly, the detection throughput has been increased by 2 times by reducing the technical triplicates.
Long-term stability of DNA during sampling and transport is the key factor affecting the performance of at-home cancer screening strategy [21]. Our results of stool DNA stability study indicated that the stool DNA collection and transport device used in this study could ensure nearly no DNA degradation in one week at 37 °C, thus we are able to develop a standard work-flow of ColoDefense2.0 and realize nationwide sampling for stool DNA test. Through simplification and/or optimization from the complex multiomics detection to a single multiplex approach, our goal is to reduce the screening cost and push the detection throughput to the limit while ensuring the overall accuracy, so as to encourage as many people as possible to participate in CRC screening. Although the number of participants in this study was limited and only retrospective studies were involved, this study confirmed the feasibility of optimizing the strategies. Further prospective studies of multi-center cohorts in the real-world application still need to be conducted. Meanwhile, there is another limitation of the study: the mean ages of the control subjects were younger than that of the cancer patients, although the adjust specificities in both training and validation cohort only slightly decreased compared with the whole control subjects (Additional file 2: Table S3). We will focus on this point in our future studies.
Conclusion
By simplifying the procedure of ColoDefense1.0 assay, the ColoDefense2.0 assay maintained its excellent performance on detecting CRC and adenomatous polyps, and increased the PCR reaction throughput in triple, which provided an affordable, accurate and convenient screening tool for CRC.
Availability of data and materials
The datasets used and/or analyzed for the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CRC:
-
Colorectal cancer
- AA:
-
Advanced adenomas
- SP:
-
Small polyps
- FOBT:
-
Fecal occult blood test
- FIT:
-
Fecal immunochemical test
- cfDNA:
-
Cell-free DNA
- PS:
-
Preservative buffer
- DS:
-
Deionized water
- LoD:
-
Limit of detection
- ROC:
-
Receiver operating characteristic
- CI:
-
Confidence interval
- AUC:
-
Area under the curve
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–64.
Patel S, Issaka RB, Chen E, Somsouk M. Colorectal cancer screening and COVID-19. Am J Gastroenterol. 2021;116(2):433–4.
Zhang J, Xu H, Zheng L, Yu J, Chen Q, Cao X, et al. Determinants of participation and detection rate of colorectal cancer from a population-based screening program in China. Front Oncol. 2020;10:1173.
Chen H, Li N, Ren J, Feng X, Lyu Z, Wei L, et al. Participation and yield of a population-based colorectal cancer screening programme in China. Gut. 2019;68(8):1450–7.
Yeoh K-G, Ho K-Y, Chiu H-M, Zhu F, Ching JYL, Wu D-C, et al. The Asia-Pacific Colorectal Screening score: a validated tool that stratifies risk for colorectal advanced neoplasia in asymptomatic Asian subjects. Gut. 2011;60(9):1236–41.
Navarro M, Nicolas A, Ferrandez A, Lanas A. Colorectal cancer population screening programs worldwide in 2016: an update. World J Gastroenterol. 2017;23(20):3632–42.
Zhao G, Liu X, Liu Y, Li H, Ma Y, Li S, et al. Aberrant DNA methylation of SEPT9 and SDC2 in stool specimens as an integrated biomarker for colorectal cancer early detection. Front Genet. 2020;11:643.
Zhao G, Li H, Yang Z, Wang Z, Xu M, Xiong S, et al. Multiplex methylated DNA testing in plasma with high sensitivity and specificity for colorectal cancer screening. Cancer Med. 2019;8(12):5619–28.
Oh TJ, Oh HI, Seo YY, Jeong D, Kim C, Kang HW, et al. Feasibility of quantifying SDC2 methylation in stool DNA for early detection of colorectal cancer. Clin Epigenetics. 2017;9:126.
Oh T, Kim N, Moon Y, Kim MS, Hoehn BD, Park CH, et al. Genome-wide identification and validation of a novel methylation biomarker, SDC2, for blood-based detection of colorectal cancer. J Mol Diagn. 2013;15(4):498–507.
Potter NT, Hurban P, White MN, Whitlock KD, Lofton-Day CE, Tetzner R, et al. Validation of a real-time PCR-based qualitative assay for the detection of methylated SEPT9 DNA in human plasma. Clin Chem. 2014;60(9):1183–91.
Church TR, Wandell M, Lofton-Day C, Mongin SJ, Burger M, Payne SR, et al. Prospective evaluation of methylated SEPT9 in plasma for detection of asymptomatic colorectal cancer. Gut. 2014;63(2):317–25.
Zhao G, Liu X, Liu Y, Ma Y, Yang J, Li H, et al. Methylated SFRP2 and SDC2 in stool specimens for Colorectal Cancer early detection: a cost-effective strategy for Chinese population. J Cancer. 2021;12(9):2665–72.
Meester RG, Doubeni CA, Lansdorp-Vogelaar I, Goede SL, Levin TR, Quinn VP, et al. Colorectal cancer deaths attributable to nonuse of screening in the United States. Ann Epidemiol. 2015;25(3):208-213 e1.
Kanth P, Inadomi JM. Screening and prevention of colorectal cancer. BMJ. 2021;374:n1855.
Zauber AG. The impact of screening on colorectal cancer mortality and incidence: has it really made a difference? Dig Dis Sci. 2015;60(3):681–91.
Imperiale TF, Ransohoff DF, Itzkowitz SH, Levin TR, Lavin P, Lidgard GP, et al. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014;370(14):1287–97.
Wang J, Liu S, Wang H, Zheng L, Zhou C, Li G, et al. Robust performance of a novel stool DNA test of methylated SDC2 for colorectal cancer detection: a multicenter clinical study. Clin Epigenetics. 2020;12(1):162.
Wang Z, Shang J, Zhang G, Kong L, Zhang F, Guo Y, et al. Evaluating the clinical performance of a dual-target stool DNA test for colorectal cancer detection. J Mol Diagn. 2022;24(2):131–43.
Qian CN. At-home cancer screening: a solution for China and other developing countries with a large population and limited number of healthcare practitioners. Chin J Cancer. 2017;36(1):68.
Acknowledgements
Not applicable.
Author statement
This manuscript has not been published or presented elsewhere in part or in entirety, and is not under consideration by another journal. All the authors have approved the manuscript and agree with submission to your esteemed journal.
Funding
The work was supported by the grants from Special Project of Diagnosis and Treatment Technology for Clinical Key Diseases in Suzhou (Grant No. LCZX201927), Key Technologies R & D Program for Social Development of Jiangsu Province (Grant No. BE2019688), Key Technologies R & D Program for Social Development of Xuzhou (Grant No. KC17184) and Suzhou Clinical Medicine Expert Team Project (No. SZYJTD201722).
Author information
Authors and Affiliations
Contributions
YD, GZ, JY and SX performed the statistical analyses and drafted the manuscript. JY, XZ, SX, XL, LG, JW, ZX and HX participated in sample collection and data analysis. YD, GZ, HX, SF and MZ conceived of the study and participated in the design and coordination of the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Affiliated Hospital of Xuzhou Medical University and Kunshan Hospital of Traditional Chinese Medicine, and the informed consent was obtained from all participating patients and healthy control subjects, and the study was performed according to the Declaration of Helsinki principles.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplemental Figure.
Additional file 2:
Supplemental Tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dai, Y., Zhao, G., Yang, J. et al. A simplified multiplex methylated DNA testing for early detection of colorectal cancer in stool DNA. BMC Gastroenterol 22, 428 (2022). https://doi.org/10.1186/s12876-022-02512-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02512-6