Abstract
Background
The purpose of this study was to compare short-course radiotherapy (SC) or neoadjuvant long-course chemoradiotherapy (LC) treatment for locally advanced rectal cancer patients.
Methods
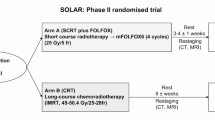
Patients with a diagnosis of locally advanced rectal cancer (LARC) who had undergone neoadjuvant radiotherapy before surgery between 2013 and 2018 at the medical center in China were included in this study. All patients’ MRI confirmed T2N+M0 or T3-4N0-3M0 clinical stages. Patients in the SC group received pelvic radiotherapy with a dose of 5 × 5 Gy (with or without chemotherapy at any time), followed by immediate or delayed surgery. Patients in the LC group received a dose of 50–50.4 Gy in 25–28 fractions, concomitantly with FOLFOX or capecitabine-based chemotherapy, followed by surgery 4–6 weeks later. All clinical data were retrospectively collected, and long-term follow-up was completed and recorded at the same time.
Results
A total of 170 were eligible to participate in this study, 32 patients in the SC group, and 138 in the LC group. The median follow-up time of living patients was 39 months. The disease-free survival (DFS) and overall survival (OS) rates in the SC group and LC group at 3 years, were, 84.9% versus 72.4% (P = 0.273) and 96.2% versus 87.2% (P = 0.510), respectively. The complete pathological response (pCR) rates in the SC group and LC group were, 25% versus 18.1% (the difference was not statistically significant, P = 0.375), respectively. However, the SC group had better node(N) downstaging compared to the LC group (P = 0.011).
Conclusions
There were no differences observed in DFS and OS between short-course radiotherapy and long-course chemoradiation, and both can be used as treatment options for patients with locally advanced rectal cancer.
Similar content being viewed by others
Background
Colorectal cancer is one of the most common malignant tumors, accounting for 1/10 of all cancer cases and deaths [1]. In China, the incidence rate of colorectal cancer is high, and it is ranked as one of the five main causes of cancer-related deaths [2]. Most of the patients are diagnosed at the locally advanced middle and late stages, which results in the poor prognosis of the patients.
Over the past few decades, as the management of rectal cancer has significantly evolved, and neoadjuvant therapy including radiotherapy and chemotherapy has become an indispensable part of the treatment. CAO/ARO/AIO-94 III phase trial [3] compared preoperative and postoperative radiotherapy and chemotherapy in patients with locally advanced rectal cancer. The recurrence rate and acute and chronic toxicity of the preoperative chemoradiotherapy group was found to have significantly decreased, and at 5 years, the cumulative local recurrence rate was reduced, establishing the status of preoperative radiotherapy and chemotherapy in locally advanced rectal cancer. Nowadays, preoperative radiotherapy followed by total mesorectal excision is the standard treatment for locally advanced rectal cancer. There are two standard preoperative therapy options, including short-course radiotherapy (5 × 5 Gy) with immediate or delayed surgery, and long course chemoradiotherapy (45–50 Gy) with concurrent chemotherapy and surgical treatment after 4–8 weeks. Short course radiotherapy is the most preferred option in Europe [4], while long course chemoradiotherapy is majorly supported in the United States [5]. Short-course has the advantages of reduced cost and improved patient convenience as treatment is completed within a shorter time, while long-term chemoradiotherapy is closely related to higher sphincter preservation and lower surgical morbidity. However, some prospective studies have demonstrated that there is no difference in long-term oncological outcomes [6, 7]. The current Chinese guidelines recommend long-term simultaneous radiotherapy and chemotherapy as grade I for preoperative treatment of middle and low rectal cancer in cT3/T4N + , while short-term radiotherapy is recommended as grade II, and needs to be discussed in many disciplines before implementation [8].
Although both short-course preoperative radiotherapy and long-course preoperative chemoradiotherapy have been practiced in parallel in the past few decades, it is not clear which is the best neoadjuvant therapy for locally advanced rectal cancer. In this retrospective study, we compared short-course radiotherapy with long-course chemoradiotherapy, to determine the most beneficial therapy for locally advanced rectal cancer. In this study, the results were reported after a minimum follow-up period of 3 years, and a comparison of disease-free survival, overall survival, complete pathological response rate, and tumor and lymph node descending stage was also included.
Methods
Patient selection
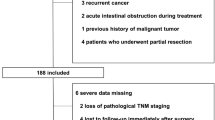
In this retrospective single-institution cohort study with long-term follow-up, patients with a diagnosis of locally advanced rectal cancer (LARC) who had undergone neoadjuvant radiotherapy before surgery between 2013 and 2018 at the medical center in China were included in this study. The eligibility criteria were as follows: histologically confirmed rectal carcinoma, lower border within 10 cm from the anal verge, magnetic resonance imaging (MRI) confirmed clinical T2/N+ or T3-4/any N. The exclusion criteria included evidence of distant metastases, recurrent rectal cancer, unknown clinical or pathological T and N category or missing follow-up data.
All relevant data, including patient’s demographic data, clinical stage, and characteristics, as well as neoadjuvant therapy and surgical methods, were retrieved from the hospital’s patient records and recorded in detail.
Treatment and follow-up
Eligible patients received either short-course radiotherapy (SC) or long-course chemoradiotherapy (LC) as neoadjuvant therapy. SC was defined as five fraction radiotherapy to a total dose of 25 Gy over five days, (with or without chemotherapy as part of their treatment course), followed by immediate surgery (within 4 weeks) or delayed surgery (more than 4 weeks).
LC comprised a total of 50–50.4 Gy in 25–28 fractions administered 5 days per week for the duration of radiation concomitantly with FOLFOX or capecitabine-based chemotherapy, followed by surgery 4–6 weeks later.
The radiation clinical target volume (CTV) included the primary rectal cancer, perirectal and internal iliac nodes, mesorectum, pelvic sidewalls, and presacral space with the upper border at the sacral promontory. Intensity-modulated radiotherapy (IMRT) using 6–18 MV photons was used, with daily image guidance.
Follow-up data were collected based on clinical examination or by telephone every 3 to 6 months after discharge, and dates of death were verified using data obtained from the census registry office.
TNM staging
Staging of rectal cancer was performed according to the Union for International Cancer Control/American Joint Committee of Cancer (UICC/AJCC) 8.0. The clinical stage of the neoplasm was assessed in preoperative examinations performed before radiotherapy: endorectal ultrasound, colonoscopy, abdominal ultrasound, chest x-ray, and pelvic MRI (Done by both observers with inter-observer agreement). Pathological TNM (ypTNM) was determined by a histologist after the assessment of the specimen. T and N downstaging was recorded when the pathological stage was lower than the clinical stage before neoadjuvant treatment. Complete pathological response (pCR) was defined as the absence of a residual tumor at the time of the histological examination of the resected specimen [9].
Statistical methods
The median and interquartile range (IQR) were used to express the continuous variables, and Kolmogorov–Smirnov test was used to detect the normal distribution, and t-test was used for those that conformed to the normal distribution, otherwise Mann–Whitney U test was used. The χ2 test or Fisher exact test was used to analyze the categorical variables. Survival data were analyzed using the Kaplan–Meier method and the log-rank test was used to detect differences between groups. All tests were two-sided and P < 0.05 was considered statistically significant. All statistical analyses were performed using the SPSS software (SPSS, version 24.0; SPSS Inc, Chicago, IL, USA).
Disease-free survival (DFS) was defined as the time from the date of operation to the time of confirmed local recurrence, distant metastases, or death due to disease or treatment. At the last follow-up, patients who were alive and disease-free (or died of non-rectal cancer causes, with no evidence of disease) were censored. Overall survival (OS) was defined as the time from the beginning of radiotherapy to death from any cause, with survivors being censored at the last follow-up time.
Results
Demographic data
Between 2013 and 2018, 170 patients were enrolled (SC, 32; LC, 138). Table 1. presents the patients’ characteristics between the two groups (age, sex, clinical staging, tumor localization, the level of CEA, mode, and type of operation). There were slightly more male patients (55.9% males), and most patients had a low tumor (63.5%, within 5 cm from the anal verge). The majority of the patients underwent laparoscopic surgery (53.5%) and Dixon surgery (62.9%), and 70.6% of the patients were confirmed to have stage T3, while 87.1% had lymph node-positive disease.
Disease-free survival rate and overall survival
On the last day of the final follow-up (August 19, 2020), 25 patients had died, and the median follow-up period for the surviving patients was 39 months. Figure 1 displays the Kaplan–Meier curve for overall survival of rectal cancer patients grouped by SC and LC. At 3 years, the DFS and OS rates in the SC and LC groups were, 84.9 vs. 72.4% (P = 0.273) and 96.2% versus 87.2% (P = 0.510), respectively. The median survival in patients receiving SC was 29.5 months, whereas the median survival in patients receiving LC was 41.5 months.
Pathological response to therapy
As shown in Table 2, nodal downstaging was found in 93.7% of the patients treated with SC, and 72.5% of the patients treated with LC (P = 0.011). pCR rates in the SC group and LC group were, 25% versus 18.1% (P = 0.375), respectively.
Discussion
In the current era of finding an accurate treatment for rectal cancer, insights into the effects of preoperative treatment, and determination of the best form of therapy is very important. This study showed no difference in DFS, OS, and pCR rates between the two different modes of preoperative treatments. In a randomized study by Bujko et al. [6], T3/4 stage patients receiving chemoradiation (50·4 Gy in 28 fractions of 1·8 Gy, bolus 5-fluorouracil, and leucovorin) were compared with patients who underwent radiation therapy (5 × 5 Gy), and the study reported no significant difference in the 4-year OS (66% vs. 67%, respectively) and DFS (58.4% vs. 55.6%, respectively). These findings were consistent with the results of this study.
Stockholm III trial [10] was the first to compare three different radiotherapy regimens (SC with immediate surgery, SC with delayed surgery, and LC with delayed surgery). However, the trial revealed that there was no significant difference in OS and DFS among the three groups. Besides, the pCR rate in the SC group with delayed surgery (10%) was superior to the other two groups [11]. In the present study, the pCR rate in the SC group (25%) was found to be better compared to the LC group (18.1%), and both were higher than 10%. This may be because the SC group received more preoperative chemotherapy. A previous meta-analysis found that LC presented a better pCR rate compared with the SC without chemotherapy, meaning that chemotherapy may enhance the efficacy of preoperative treatment [12]. Another randomized phase III study by Bujko et al. [13] compared patients receiving radiotherapy (5 × 5 Gy) and three cycles of FOLFOX4 with those receiving 50.4 Gy in 28 fractions combined with two 5-day cycles of bolus 5-Fu 325 mg/ m2/day and leucovorin 20 mg/m2/day during the first and fifth week of irradiation along with five infusions of oxaliplatin 50 mg/m2 once weekly. This study found that the pCR, DFS and OS in the two groups were, 16% versus 12% (P = 0.17), 53% versus 52% (P = 0.85), and 73% versus 65% (P = 0.046), respectively, thus confirming the importance of adequate chemotherapy. In the present study, we found better nodal downstaging in the SC group. However, this is not consistent with the results of the study by Brandon et al. [14], which found that the LC group were more likely to have nodal (25% vs 19%) downstaging, and pCR (15% vs 6%) compared with the SC group (all P < 0.05). SC itself has a similar biological effective dose as LC [15]. The large fractions used in SC can be more efficient in inducing both the innate and adaptive anti-tumor immunity, and eventually increase the biologic effects of concomitant and consolidation chemotherapy [16]. This results from the release of antigens due to the breakdown of tumoral cells, and the presentation of the antigens to T cells [17]. This difference may also be associated with the higher preoperative chemotherapy in the SC group in this study and SC with delayed surgery is also reported to have a satisfactory downstaging effect [18]. A matched pair analysis also observed that patients treated with SC and sequential FOLFOX Chemotherapy had improved rates of downstaging compared to the matched LC cohort [19]. This was precisely because early chemotherapy is likely to improve the overall therapeutic effect, hence complete neoadjuvant therapy has been proposed. There are two main proposed treatment modes: first chemoradiotherapy, and then consolidation chemotherapy, or the reverse order, induction chemotherapy first, and then chemoradiotherapy. In a multicentre, phase 2 trial by Julio et al. [20], 292 patients with stage II or III rectal cancer were divided into four groups and received zero, two, four, or six cycles of consolidation chemotherapy after preoperative chemoradiotherapy. After a median follow-up of 59 months, patients who received consolidation chemotherapy were found to have improved DFS (P < 0.05), and there were differences in survival between groups in patients who received at least one cycle of FOLFOX. In another phase III study [21] (STELLAR trial) in China, comparing short-course radiotherapy followed by chemotherapy with long-course chemoradiotherapy in LARC, the results showed that pCR rates in the experimental and control group were 18.6% vs. 5.4% (P = 0.029), respectively. These findings were consistent with the pCR rates reported in this study (18.1–25%).
The potential economic benefit cannot be ignored during the formulation of treatment. Using the micro-cost calculation method, Hanly et al. reported that SC is cheaper than LC [22]. Another study [23] analyzed the cost-effectiveness of immediate surgery after SC and LC with delayed surgery and showed that SC was the most cost-effective strategy. However, LC was also found to be a cost-effective approach for patients with distal tumors. Wang et al. [24] considered the economic benefits of both short-term and long-term radiotherapy after chemotherapy. Although the total cost of SC was much higher than that of LC ($78,937 and $38,140 respectively), the final result that was calculated through quality-adjusted life months (QALMs), found that SC was more cost-effective.
The National Comprehensive Cancer Network (NCCN) guidelines recommend SC as an acceptable alternative to LC except for patients with T4 stage rectal cancer [25]. Additionally, the American Society for Radiation Oncology (ASTRO) guidelines state that for patients with a high risk of circumferential resection margin positive or difficulty in R0 resection, LC should be used, otherwise both radiotherapy methods can be used [26]. Both SC and LC are recommended options for neoadjuvant treatment of LARC, however, the decision to choose one or the other is based on several considerations, including (1) LC is favored when a patient is at a higher risk of positive surgical margin or when tumors are distal and/or bulky and would benefit from downstaging, (2) SC followed by consolidation chemotherapy may be the most promising order for total neoadjuvant therapy (3) LC is the preferred approach when nonoperative management is being considered as it increases the chances of a complete clinical response compared with SC, (4) SC may be used in elderly and frail patients with comorbid conditions, such as heart failure since it is better tolerated than LC due to lower toxicity, and (5) SC may be used in countries with low health-care budgets or medical centers with long waiting lists because it is less expensive and more convenient.
There are still limitations to this study. Firstly, the imbalance in the number of patients receiving SC and LC may cause deviations in the results. More cases need to be included in future studies for more convincing results. Another limitation is the short follow-up time, thus evaluating long-term outcomes is uncertain. Therefore, follow-up time needs to be further extended. Then the limitations of preoperative staging should be taken into account. A meta-analysis on the diagnostic accuracy of MRI in rectal cancer patients showed that the specificities of MRI for the T category and lymph node involvement were only 75% and 71% [27]. In a future study, diffusion-weighted imaging (DWI) may be considered for improved preoperative staging, due to the high accuracy in evaluating colorectal diseases [28] and especially for poor risk patients, computed tomography (CT) [29] and virtual CT colonoscopy [30] would be a better choice because they are noninvasive and less expensive with better spatial resolution in diagnosis of colorectal lesions. Lastly, although we confirmed the importance of chemotherapy in the neoadjuvant therapy in locally advanced rectal cancer patients, due to the retrospective nature of this study, it was difficult to confirm which chemotherapy regimen or cycle number would be more beneficial. Further related research needs to be carried out in the future.
Conclusions
Short-term radiotherapy and long-term radiotherapy are both effective and safe treatment options in patients with locally advanced rectal cancer, based on pCR, DFS, and OS.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SC:
-
Short-course radiotherapy
- LC:
-
Long-course chemoradiotherapy
- LARC:
-
Locally advanced rectal cancer
- pCR:
-
Complete pathological response
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- MRI:
-
Magnetic resonance imaging
- CTV:
-
Clinical target volume
- IMRT:
-
Intensity-modulated radiotherapy
- IQR:
-
Interquartile range
- QALMs:
-
Quality-adjusted life months
- TAAs:
-
Tumor associated antigens
- CRM:
-
Circumferential resection margin
- DWI:
-
Diffusion-weighted imaging
- CT:
-
Computed tomography
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68:394–424.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. Cancer J Clin. 2016;66:115–32.
Kim JS, Jeong SY, Shin R, Oh HK, Park KJ, Park JG. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer. Eur J Surg Oncol. 2012;38:831.
Kye B, Cho H. Overview of radiation therapy for treating rectal cancer. Ann Coloproctol. 2014;30:165.
Mowery YM, Salama JK, Zafar SY, Moore HG, Willett CG, Czito BG, et al. Neoadjuvant long-course chemoradiation remains strongly favored over short-course radiotherapy by radiation oncologists in the United States. Cancer-Am Cancer Soc. 2017;123:1434–41.
Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski W, Bebenek M, Kryj M. Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br J Surg. 2006;93:1215–23.
Ngan SY, Burmeister B, Fisher RJ, Solomon M, Goldstein D, Joseph D, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group Trial 01.04. J Clin Oncol. 2012;30:3827–33.
CSOCOC DATG. Chinese Society of Clinical Oncology (CSCO) diagnosis and treatment guidelines for colorectal cancer 2018 (English version). Chinese J Cancer Res. 2019; 31:117–134
Pach R, Kulig J, Richter P, Gach T, Szura M, Kowalska T. Randomized clinical trial on preoperative radiotherapy 25 Gy in rectal cancer—treatment results at 5-year follow-up. Langenbecks Arch Surg. 2012;397:801–7.
Erlandsson J, Holm T, Pettersson D, Berglund Å, Cedermark B, Radu C, et al. Optimal fractionation of preoperative radiotherapy and timing to surgery for rectal cancer (Stockholm III): a multicentre, randomised, non-blinded, phase 3, non-inferiority trial. Lancet Oncol. 2017;18:336–46.
Erlandsson J, Lörinc E, Ahlberg M, Pettersson D, Holm T, Glimelius B, et al. Tumour regression after radiotherapy for rectal cancer—Results from the randomised Stockholm III trial. Radiother Oncol. 2019;135:178–86.
Yu Y, Li Y, Xu C, Zhang Z, Zhang X. Comparison of long course and short course preoperative radiotherapy in the treatment of locally advanced rectal cancer: a systematic review and meta-analysis. Rev Esp Enferm Dig. 2018;111:17–27.
Bujko K, Wyrwicz L, Rutkowski A, Malinowska M, Pietrzak L, Kryński J, et al. Long-course oxaliplatin-based preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for cT4 or fixed cT3 rectal cancer: results of a randomized phase III study. Ann Oncol. 2016;27:834–42.
Chapman BC, Goodman K, Hosokawa P, Gleisner A, Cowan ML, Birnbaum E, et al. Improved survival in rectal cancer patients who are treated with long-course versus short-course neoadjuvant radiotherapy: A propensity-matched analysis of the NCDB. J Surg Oncol. 2019;119:518–31.
Glimelius B, Gronberg H, Jarhult J, Wallgren A, Cavallin-Stahl E. A systematic overview of radiation therapy effects in rectal cancer. Acta Oncol. 2003;42:476–92.
Gandhi SJ, Minn AJ, Vonderheide RH, Wherry EJ, Hahn SM, Maity A. Awakening the immune system with radiation: optimal dose and fractionation. Cancer Lett. 2015;368:185–90.
Napolitano M, D Alterio C, Cardone E, Trotta AM, Pecori B, Rega D, et al. Peripheral myeloid-derived suppressor and T regulatory PD-1 positive cells predict response to neoadjuvant short-course radiotherapy in rectal cancer patients. Oncotarget. 2015;6:8261–70.
Pettersson D, Holm T, Iversen H, Blomqvist L, Glimelius B, Martling A. Preoperative short-course radiotherapy with delayed surgery in primary rectal cancer. Br J Surg. 2012;99:577–83.
Markovina SM, Youssef FM, Roy A, Aggarwal SB, Khwaja SM, DeWees TP, et al. Improved metastasis- and disease-free survival with preoperative sequential short course radiotherapy and FOLFOX chemotherapy for rectal cancer compared to neoadjuvant long course chemoradiotherapy; results of a matched pair analysis. Int J Radiat Oncol Biol Phys. 2017;99:417.
Garcia-Aguilar J, Chow OS, Smith DD, Marcet JE, Cataldo PA, Varma MG, et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol. 2015;16:957–66.
Jin J, Liu S, Zhu Y, Wang W, Wang X, Wang J, et al. The updated results for the Phase 3 study of 5×5 Gy followed by chemotherapy in locally advanced rectal cancer (STELLAR trial). Int J Radiat Oncol Biol Phys. 2017;99:E157.
Hanly P, Céilleachair AÓ, Skally M, Neill O, Sharp L, L. Direct costs of radiotherapy for rectal cancer: a microcosting study. Bmc Health Serv Res. 2015;15:184.
Raldow AC, Chen AB, Russell M, Lee PP, Hong TS, Ryan DP, et al. Cost-effectiveness of short-course radiation therapy vs. long-course chemoradiation for locally advanced rectal cancer. JAMA Netw Open. 2019;2:e192249.
Wang S, Wen F, Zhang P, Wang X, Li Q. Cost-effectiveness analysis of long-course oxaliplatin and bolus of fluorouracil based preoperative chemoradiotherapy vs 5×5Gy radiation plus FOLFOX4 for locally advanced resectable rectal cancer. Radiat Oncol. 2019;14:113.
Al B. Benson III APVM. Rectal cancer, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Ne. 2018; 16:874–901
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rödel C, Cervantes A, et al. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv22–40.
Al-Sukhni E, Milot L, Fruitman M, Beyene J, Victor JC, Schmocker S, et al. Diagnostic accuracy of MRI for assessment of T category, lymph node metastases, and circumferential resection margin involvement in patients with rectal cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2012;19:2212–23.
Abd-El Khalek Abd-ALRazek A, Fahmy DM. Diagnostic value of diffusion-weighted imaging and apparent diffusion coefficient in assessment of the activity of Crohn disease. J Comput Assist Tomo. 2018;42:688–96.
Rajendran H, Razek AAKA, Abubacker S. Multimodal imaging of fibrosing mesenteric tuberculosis. Radiol Case Rep. 2019;14:920–5.
Abdel Razek AA, Abu Zeid MM, Bilal M, Abdel Wahab NM. Virtual CT colonoscopy versus conventional colonoscopy: a prospective study. Hepatogastroenterology. 2005;52:1698–702.
Acknowledgements
Not applicable.
Funding
This work was supported by the Natural Science Foundation of Hunan province (Grant Number 2019JJ40490 and 2020JJ4903), Clinical Research Project of Xiangya Hospital (Grant Number 2016L06) and the 12th Five-Year Plan of Education Science in Hunan Province (XJKO11BGD032). The remuneration of those who made valuable recommendations on the design of the study, data analysis and interpretation, as well as those involved in data collection, was paid by the Natural Science Foundation of Hunan province (Grant Number 2019JJ40490 and 2020JJ4903). The cost of language refinement in the process of writing the manuscript was paid by the Clinical Research Project of Xiangya Hospital (Grant Number 2016L06) and the 12th Five-Year Plan of Education Science in Hunan Province (XJKO11BGD032).
Author information
Authors and Affiliations
Contributions
WJ analyzed and interpreted the patient data, and was a major contributor in writing the manuscript. LK and LYW collected and compiled data. ZH and PQ provided conception and designed the research body. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participates
The need for ethics approval was waived by the Ethic Committee of the Xiangya Hospital of Central South University. The consent was verbal and was approved by the ethics committee. All methods were carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, J., Long, Y., Liu, K. et al. Comparing neoadjuvant long-course chemoradiotherapy with short-course radiotherapy in rectal cancer. BMC Gastroenterol 21, 277 (2021). https://doi.org/10.1186/s12876-021-01851-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-021-01851-0