Abstract
Background
Risk stratification for patients with nonvariceal upper gastrointestinal (NVUGI) bleeding is crucial for successful prognosis and treatment. Recently, the AIMS65 score has been used to predict mortality risk and rebleeding. The purpose of this study was to compare the performance of the AIMS65 score with the Glasgow-Blatchford score (GBS), Rockall score, and pre-endoscopic Rockall score in Korea.
Methods
We retrospectively studied 512 patients with NVUGI bleeding who were treated at a university hospital between 2013 and 2016. The AIMS65, GBS, Rockall score, and pre-endoscopic Rockall score were used to stratify patients based on their bleeding risk. The primary outcome was in-hospital mortality. The secondary outcomes were composite clinical outcomes of mortality, rebleeding, and intensive care unit (ICU) admission. Each scoring system was compared using the receiver-operating curve (ROC).
Results
A total of 17 patients (3.3%) died and rebleeding developed in 65 patients (12.7%). Eighty-six patients (16.8%) required ICU admission. The AIMS65 (area under the curve (AUC) 0.84, 95% confidence interval, 0.81–0.88)) seemed to be superior to the GBS (AUC 0.72, 0.68–0.76), the Rockall score (AUC 0.75, 0.71–0.79), or the pre-endoscopic Rockall score (AUC 0.74, 0.70–0.78) in predicting in-hospital mortality, but there was not a statistically significant difference between the groups (P = 0.07). The AUC value of the AIMS65 was not significantly different from the other scoring systems in prediction of rebleeding, endoscopic intervention, or ICU admission.
Conclusions
The AIMS65 score in NVUGI bleeding patients was comparable to the GBS or Rockall scoring systems when predicting the mortality, rebleeding, or ICU admission. Because AIMS65 is a much easier, readily calculated scoring system compared to the others, we would recommend using the AIMS65 in daily practice.
Similar content being viewed by others
Background
Upper gastrointestinal (UGI) bleeding is a medical emergency with an incidence of mortality of 5–10% [1]. The guidelines recommend use of risk stratification tools in UGI bleeding to facilitate accurate triage and assist in clinical decisions such as endoscopic timing and level of care [2, 3]. It is important for physicians to identify UGI bleeding patients who are at high risk of mortality or rebleeding.
There are some scoring systems have been developed to predict bleeding outcomes for patients with UGI bleeding. The Rockall score (RS) and the Glasgow-Blatchford risk score (GBS) are the most widely-used scoring systems in clinical practice [4, 5]. These scoring systems have been reported to be useful in predicting mortality, rebleeding, need for transfusion, and hemostasis [6, 7]. However, there are limitations in these scoring systems. The GBS is difficult to calculate in routine clinical practice due to complex nature of score calculation, and the RS requires endoscopic findings.
Recently, much interest has been shown in pre-endoscopic risk scores for UGI bleeding. The pre-endoscopy Rockall score (PRS) excludes the endoscopic findings that are needed for the RS; because of this, using the PRS to make clinical predictions, has been controversial [8, 9]. The AIMS65 scoring system was developed to determine the prognosis of patients with UGI bleeding [10]. The AIMS65 score is based on albumin levels, prothrombin time (PT), international normalized ratio (INR), altered mental status, systolic blood pressure, and whether age is 65 years and older. One point is assigned to each variable that increases the risk of clinical outcomes. Compared to other scoring systems, the AIMS65 has the advantage of being simple to perform in an emergency situation [11,12,13]. But AIMS65 score has not been sufficiently validated in Korea. Few studies have compared AIMS65 score with other scoring systems [11, 14]. One study suggested that AIMS65 score was not suitable for predicting the need for endoscopic intervention [14].
The causes of UGI bleeding differ among countries. The prevalence of variceal bleeding is higher in Korea than in Western countries [14]. Limited data are available on validation of scoring systems in patients with non-variceal UGI (NVUGI) bleeding in Korea.
The aim of this study was to compare the predictive value of the AIMS65 with the GBS, PRS, and RS scores for a large scale of NVUGI bleeding patients in Korea.
Methods
Inclusion and exclusion criteria of patients
From January 2013 to June 2016, patients for the UGI bleeding who visited the emergency medical center of the Sanggye Paik Hospital, Seoul, South Korea were reviewed retrospectively in this study. UGI bleeding was confirmed by the hospital staff based on the presence of hematemesis or melena. All patients underwent emergency upper endoscopy within 24 h. Patients with esophageal or gastric variceal bleeding were excluded. Cases of iatrogenic post-procedural bleedings after endoscopic resection for gastric tumors were also excluded. The data of the patients were collected in the electronic medical record. Patients were excluded if the data required for calculation of relevant risk stratification scores were unavailable. The data were reviewed by two endoscopy specialists (M.S.K. and J.C.) for all cases.
Treatment of UGI bleeding
Patients received the same treatment according to emergency bleeding protocols. All patients received intravenous proton pump inhibitor infusion before upper endoscopy. Upper endoscopy was performed by endoscopy specialists within the first 24 h. Endoscopic therapies were applied as following conditions: (1) peptic ulcers with actively bleeding (type Ia), oozing hemorrhage (type Ib), or a nonbleeding visible vessel (type IIa); (2) Dieulafoy’s lesion (3) angiodyplasia (4) and any lesions with active bleeding. Adherent blood clot (type IIb), flat spot (type IIc), clean base ulcer (type III), or lesions with no active bleeding stigmata including acute gastric mucosal lesion or Mallory-Weiss tear were initially treated medication without endoscopic therapy.
Endoscopic therapies included injection of epinephrine, hemostatic forcep electrocoagulation, argon plasma coagulation, or application of endoscopic clips. In cases of failed endoscopic hemostasis, transarterial embolization was preferred over surgery. When rebleeding occurred after successful endoscopic therapy, endoscopic therapy was initially preferred. Surgery as salvage therapy was performed when embolization was unsuccessful.
Transfusion was required if hemoglobin was below 8 g/dL. ICU admission was considered in the following conditions: if the patients have any symptoms of confusion or altered mentality; presence of hemodynamic instability (systolic blood pressure < 90 mmHg, need for vasoactive drugs); or severe comorbid illness including heart failure, chronic renal failure, liver cirrhosis, or chronic lung disease. Decision of ICU admission was made finally by ICU unit attending physicians.
Study design
The following data were collected through electronic medical record review: age, sex, symptoms of visiting emergency centers (hematemesis, melena, shock, syncope, or altered mentality), vital sign (heart rate, systolic blood pressure), the Glasgow Coma Scale, mental status, medications that contribute to bleeding (aspirin, clopidogrel, warfarin, nonsteroidal anti-inflammatory drugs, other antithrombotic agents). Laboratory findings (hemoglobin, albumin level, blood urea nitrogen, PT, and INR), and endoscopic findings were also collected. The AIMS65 score, RS, PRS, and GBS were obtained based on the data. Components of the each scoring system were described in Table 1. Primary outcome was in-hospital mortality and secondary outcomes were composite clinical outcomes of in-hospital mortality, intensive care unit (ICU) admission; rebleeding; blood transfusion requirement; and endoscopic, radiologic, or surgical intervention.
Statistical analysis
The performance of each scoring system was evaluated with a receiver operating characteristic (ROC) curve, calculation of area under the curve (AUC) with 95% confidence intervals. In a ROC curve the true positive rate (sensitivity) is plotted in function of the false positive rate (100-specificity) for different cut-off points of a parameter. Each point on the ROC curve represents a sensitivity/specificity pair corresponding to a particular decision threshold. The cut-off value of each scoring system is determined by the ROC curve with the most specificity and sensitivity. The risk prediction scoring system was divided into two groups, high-risk group and low-risk group. For each scoring systems, a cutoff point was calculated that maximized the sum of sensitivity and specificity in predicting the primary and secondary outcomes. Fischer’s exact test was used for categorical variables. All confidence intervals are described as two-sided binomial 95% confidence intervals. The cut-off value 0.05 considered to be the threshold for statistical significance. In a Bonferroni correction to adjust for the multiple comparisons in the scoring systems (in which the P values were divided by 4 for the comparison with an alpha level of 0.05), the corrected P values were 0.0125 for the combination group versus. Data were analyzed using SPSS Statistics for Windows (version 23.0; IBM Corp., Armonk, NY, USA). AUCs were compared with the DeLong method by using MedCalc program (version 16.8.4; MedCalc Software, Mariakerke, Belgium).
Results
Baseline characteristics
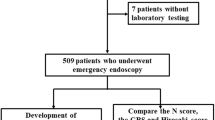
A total of 578 patients were enrolled, of which consecutive 512 patients were included in the final analysis. Of these, 66 patients were excluded from the study for the following reasons: 30 patients did not have sufficient data for the study; 16 had iatrogenic post-procedural bleedings (endoscopic submucosal dissection for gastric tumors (n = 11), endoscopic mucosal resection (n = 2), endoscopic sphincterotomy (n = 3)), and 20 patients were lost to follow-up (Fig. 1).
The median age was 64 (range, 48–80 years) years old, and 71.9% patients were men. Among patients, 397 (69.7%) patients had comorbidities and 327 (36%) were taking anti-platelet agents or anti-coagulant medications on admission. The most common symptom of visiting the emergency center was melena (27.5%). The common causes of bleeding were gastric ulcer (32.8%), duodenal ulcer (20.5%), Mallory-Weiss tear (13.1%), and acute gastric mucosal lesion (12.9%) (Table 2).
Primary clinical outcome: mortality
Seventeen of the 512 patients (3.3%) died. Their median age was 70.24 (range 43–93) years old. The causes of death were uncontrolled bleeding (n = 5), complications due to cirrhosis (n = 5), sepsis due to pneumonia (n = 4), renal failure (n = 2), and cerebral infarction (n = 1). In the cases of 5 deaths due to uncontrolled bleeding, two patients underwent angiographic embolization and two patients underwent angiography followed by surgery. One patient died of active duodenal ulcer bleeding and hypovolemic shock during endoscopic therapy.
All but one of the 17 patients who died had comorbidities. There was no difference between survivors and non-survivors in the use of anticoagulants. The mortality increased with increasing AIMS65 score, although death occurred in 1 patient who scored 0 on the AIMS65. Mortality was seen in 1/161 (0.6%) for AIMS65 0, 1/201 (0.5%) for AIMS65 1, 6/104 (5.8%) for AIMS65 2, 6/36 (16.7%) for AIMS65 3, 3/9 (33.3%) for AIMS65 4, 0/1 for AIMS65 5. The AUC values of each test were: AIMS65 = 0.84 (95% confidence interval (CI), 0.81–0.88), PRS = 0.74 (95% CI, 0.70–0.78), RS = 0.75 (95% CI, 0.71–0.79), and GBS = 0.72 (95% CI, 0.68–0.76). With regard to AUC value, there was a trend suggesting that the AIMS65 scoring system (0.84) seemed more accurate than the GBS system (0.72) for predicting mortality (P = 0.07) (Table 3) (Fig. 2).
Secondary clinical outcomes
Composite serious clinical outcomes
Of the 512 patients, 134 (26.2%) were diagnosed with serious clinical outcomes (in-hospital mortality, rebleeding, or ICU admission). For these composite serious clinical outcomes, the AUC values of AIMS65, PRS, RS, and GBS were 0.68 (95% CI, 0.64–0.72), 0.70 (95% CI, 0.65–0.74), 0.66 (95% CI, 0.62–0.70), and 0.65 (95% CI, 0.61–0.70), respectively. AUC values of each scoring system did not differ significantly in terms of composite serious clinical outcomes.
Rebleeding
Rebleeding occurred in 65 patients (12.7%). Rebleeding occurred in patients with elderly, or chronic kidney disease. The AUC values for predicted rebleeding were as follows: AIMS65 = 0.58 (95% CI, 0.54–0.62), PRS = 0.58 (95% CI, 0.54–0.62), RS = 0.63 (95% CI, 0.59–0.67), and GBS = 0.55 (95% CI, 0.51–0.59). In pairwise comparisons between the scores for rebleeding, the AUC value of RS was superior to that of PRS and GBS (pairwise comparison, P = 0.01 and P = 0.04), but not statistically different than that of AIMS65 (pairwise comparison, P = 0.11).
ICU admission
Eighty-six patients (16.8%) were admitted to the ICU. The AUC values for predicted admission were: AIMS65 = 0.73 (95% CI, 0.69–0.77), PRS = 0.70 (95% CI, 0.66–0.74), RS = 0.70 (95% CI, 0.66–0.74), and GBS = 0.71 (95% CI, 0.67–0.75). All four scoring systems similarly predicted the need for ICU admission.
Transfusion requirements
Transfusion was required in 264 patients (62.3%) and the median transfusion was 2 units (interquartile range, 0–4). The AUC values for the need of transfusion were: AIMS65 = 0.69 (95% CI, 0.65–0.73), PRS = 0.70 (95% CI, 0.65–0.73), RS = 0.74 (95% CI, 0.70–0.77), and GBS = 0.87 (95% CI, 0.66–0.74). GBS was superior to other scoring systems in predicting transfusion requirement.
Endoscopic intervention
Endoscopic intervention was required in 301 patients (58.8%). The AUC values for the prediction of the need of endoscopic intervention were: AIMS65 = 0.57 (95% CI, 0.53–0.62), PRS = 0.56 (95% CI, 0.52–0.61), RS = 0.56 (95% CI, 0.52–0.61), and GBS = 0.61 (95% CI, 0.57–0.66) (Table 3).
Cut-off value
The cut-off values for the endpoints of the risk stratification scores from the AIMS65, PRS, RS, and GBS were obtained when the cut-off value that maximized the sum of the sensitivity and the specificity was obtained. Sensitivity of AIMS65 was from 41.5% (CI 19.4–54.4, p < 0.001) to 88.2% (CI 63.6–98.5, p < 0.0001), which was similar to other scoring systems, ranging from 71.3 (CI 68.1–76.6, p < 0.001) to 78.6 (CI 74.1–82.6, p < 0.001), respectively. Cut-off as a value separating risk levels (high vs. low risk) for death was above 2 points on the AIMS65 and 8 points on the GBS, and 1 point on the AIMS65 and 11 points on the GBS for rebleeding. The cut-off values for ICU admission were 2 points on the AIMS65, 10 points on the GBS, 4 points on the PRS, and 5 points on the RS (Table 4).
Discussion
The AIMS65 scoring system was introduced to predict hospital mortality in patients with UGI bleeding based on clinical outcomes of bleeding has been validated for use in several studies [11, 15,16,17,18]. One study has found that the AIMS65 score is an independent predictor of mortality in patients with UGI bleeding [16]. One study showed that the accuracy of AIMS65 score is superior to that of GBS and PRS in predicting in-hospital mortality [16]. In contrast, one study showed that PRS is more useful for predicting mortality than the GBS and AIMS65 scores [18]. These results might be due to different patient characteristics and different mortality rate. The mortality rate was 3.3% in our study, compared to 4.2% in previous study [16], which suggests less severe patients were included in our study. It is important to compare the scoring systems within the same population and with a similar disease severity [12]. We conducted the present study in a large number of patients after excluding patients with variceal bleeding. The risk stratification score was calculated in all patients using the GBS, the PRS, and the RS. The AIMS65 showed similar performance to the GBS and the RS in predicting mortality, rebleeding, ICU admission, and endoscopic intervention.
The risk stratification scores were recommended for management of prognosis and serious outcomes for NVUGI bleeding [19]. In order to be an effective tool for risk stratification, a measure should be easy to use and accurately predict bleeding outcomes [16]. For example, the CHADS2 scoring systems, which is used to predict cerebral vascular risk in patients with atrial fibrillation, is widely used because of its accessibility and simplicity [20]. The GBS scoring system is limited by weighting, which makes calculation difficult. RS scoring system also has limitations. Weighting leads to complexity in calculation and it requires endoscopic data for calculation, impossible to apply at the time of presentation. Those systems are much more difficult to apply by the busy clinician in routine clinical practice due to their complexity [21]. AIMS65 has only 5 components (albumin, INR, mental status, systolic BP, age) and each component is the same value of 1 point. The recently-developed AIMS65 is much easier to apply in clinical practice.
In one study, GBS score 0 identified low-risk patients who can be managed safely as outpatients [22]. Another study showed lower-risk patients (GBS score < 12) who were taken urgently to endoscopy were related to the worse outcomes [23]. In our study, patients with AIMS65 score 0/1 had low risk of mortality of 0.5%. We believe that AIMS65 score 0/1 provides a rationale for delaying emergency endoscopic intervention until the next day when patients arrive in the evening or night time.
Several studies validated the performance of AIMS65 scoring system to predict the clinical outcomes in patients with UGI bleeding in Korea. One study showed that AIMS65 was not useful for predicting the need for endoscopic intervention and transfusion in Korea [14]. In this study, 22% (64/286) patients with variceal bleeding were included. AIMS65 score showed lower performance than GBS and RS regardless of variceal or non-variceal bleeding group. On the other hand, the other study involving 523 patients with NVUIB showed that AIMS65 score was useful for predicting the mortality, transfusion requirement, and endoscopic intervention in Korean patients with NVUIB [11]. This difference might be due to different patient characteristics and patient number.
There are limitations in this study. The study design was retrospective. However, the data were independently reviewed by two co-authors. We tried to minimize errors by collecting all medical records for NVUGI bleeding patients.
Despite the large number of patients included in this study, mortality occurred in only 17 patients (3.3%). Each scoring system to predict mortality was less accurate than previously reported, because death events were rare [7]. Another limitation of the study is single center study.
Conclusion
The AIMS65 score in NVUGI bleeding patients was comparable to the GBS or Rockall scoring systems when predicting mortality, rebleeding, ICU admission, and endoscopic intervention in Korean patients. The AIMS65 score, however, is much easier to calculate using variables routinely available in the emergency clinical situation, and has the advantage that it can be performed by the busy clinician before an endoscopy. Therefore, we recommend AIMS65 for prediction of severity of GI bleeding in daily practice. Before the AIMS65 becomes a standard of care for the risk stratification of UGI bleeding cases, further multicenter prospective studies will be required.
Availability of data and materials
Data for the analyses are available from the corresponding author on request.
Abbreviations
- AUC:
-
Area under the curve
- GBS:
-
Glasgow-Blatchford score
- ICU:
-
Intensive care unit
- NVUGI:
-
Non-variceal upper gastrointestinal
- PRS:
-
Pre-endoscopy Rockall score
- ROC:
-
Receiver-operating curve
- RS:
-
Rockall score
References
Laine L, Yang H, Chang SC, Datto C. Trends for incidence of hospitalization and death due to GI complications in the United States from 2001 to 2009. Am J Gastroenterol. 2012;107(8):1190–5 quiz 1196.
Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012;107(3):345–60 quiz 361.
Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair P, International Consensus Upper Gastrointestinal Bleeding Conference G. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152(2):101–13.
Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38(3):316–21.
Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000;356(9238):1318–21.
Bryant RV, Kuo P, Williamson K, Yam C, Schoeman MN, Holloway RH, Nguyen NQ. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc. 2013;78(4):576–83.
Stanley AJ, Laine L, Dalton HR, Ngu JH, Schultz M, Abazi R, Zakko L, Thornton S, Wilkinson K, Khor CJ, et al. Comparison of risk scoring systems for patients presenting with upper gastrointestinal bleeding: international multicentre prospective study. BMJ. 2017;356:i6432.
Chandra S, Hess EP, Agarwal D, Nestler DM, Montori VM, Song LM, Wells GA, Stiell IG. External validation of the Glasgow-Blatchford bleeding score and the Rockall score in the US setting. Am J Emerg Med. 2012;30(5):673–9.
Pang SH, Ching JY, Lau JY, Sung JJ, Graham DY, Chan FK. Comparing the Blatchford and pre-endoscopic Rockall score in predicting the need for endoscopic therapy in patients with upper GI hemorrhage. Gastrointest Endosc. 2010;71(7):1134–40.
Saltzman JR, Tabak YP, Hyett BH, Sun X, Travis AC, Johannes RS. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastrointest Endosc. 2011;74(6):1215–24.
Park SM, Yeum SC, Kim BW, Kim JS, Kim JH, Sim EH, Ji JS, Choi H. Comparison of AIMS65 score and other scoring Systems for Predicting Clinical Outcomes in Koreans with nonvariceal upper gastrointestinal bleeding. Gut Liver. 2016;10(4):526–31.
Simon TG, Travis AC, Saltzman JR. Initial assessment and resuscitation in nonvariceal upper gastrointestinal bleeding. Gastrointest Endosc Clin N Am. 2015;25(3):429–42.
Park SW, Song YW, Tak DH, Ahn BM, Kang SH, Moon HS, Sung JK, Jeong HY. The AIMS65 score is a useful predictor of mortality in patients with nonvariceal upper gastrointestinal bleeding: urgent endoscopy in patients with high AIMS65 scores. Clin Endosc. 2015;48(6):522–7.
Choe JW, Kim SY, Hyun JJ, Jung SW, Jung YK, Koo JS, Yim HJ, Lee SW. Is the AIMS 65 score useful in Prepdicting clinical outcomes in Korean patients with variceal and nonvariceal upper gastrointestinal bleeding? Gut Liver. 2017;11(6):813–20.
Zhong M, Chen WJ, Lu XY, Qian J, Zhu CQ. Comparison of three scoring systems in predicting clinical outcomes in patients with acute upper gastrointestinal bleeding: a prospective observational study. J Dig Dis. 2016;17(12):820–8.
Robertson M, Majumdar A, Boyapati R, Chung W, Worland T, Terbah R, Wei J, Lontos S, Angus P, Vaughan R. Risk stratification in acute upper GI bleeding: comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc. 2016;83(6):1151–60.
Ramaekers R, Mukarram M, Smith CA, Thiruganasambandamoorthy V. The predictive value of Preendoscopic risk scores to predict adverse outcomes in emergency department patients with upper gastrointestinal bleeding: a systematic review. Acad Emerg Med. 2016;23(11):1218–27.
Kalkan C, Soykan I, Karakaya F, Tuzun A, Gencturk ZB. Comparison of three scoring systems for risk stratification in elderly patients with acute upper gastrointestinal bleeding. Geriatr Gerontol Int. 2017;17(4):575–83.
Gralnek IM, Dumonceau J-M, Kuipers EJ, Lanas A, Sanders DS, Kurien M, Rotondano G, Hucl T, Dinis-Ribeiro M, Marmo R. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015;47(10):a1–a46.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS. Executive summary: heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):143–52.
Liang PS, Saltzman JR. A national survey on the initial management of upper gastrointestinal bleeding. J Clin Gastroenterol. 2014;48(10):e93–8.
Stanley AJ, Ashley D, Dalton HR, Mowat C, Gaya DR, Thompson E, Warshow U, Groome M, Cahill A, Benson G, et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. Lancet. 2009;373(9657):42–7.
Kumar NL, Cohen AJ, Nayor J, Claggett BL, Saltzman JR. Timing of upper endoscopy influences outcomes in patients with acute nonvariceal upper GI bleeding. Gastrointest Endosc. 2017;85(5):945–952 e941.
Acknowledgements
Not applicable.
Funding
This work was supported by the 2018 Inje University research grant. Funding bodies were not involved in the study design, collection, analysis and interpretation of the data or in writing of the manuscript.
Author information
Authors and Affiliations
Contributions
Study concept and design: MSK, JC. Acquisition of the data: MSK. Interpretation of the data: MSK, JC. Wrote the first draft of the manuscript: MSK. Writing, correction and addition of fundamental insights to the manuscript: MSK, JC, WCS. Contributed to the writing of the manuscript: MSK, JC, WCS. Agree with the manuscript’s results and conclusions: MSK, JC, WCS. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Sanggye Paik Hospital Clinical Trials Ethics Committee (SGPAIK 201612017). Informed consent was not acquired as this was a retrospective study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This similar abstract has been published at Journal of Gastroenterology and Hepatology, Volume 32, Issue S3 September 2017, Pages 70 for E-poster presentations at Asian pacific Digestive Week (APDW), Hong Kong, 23–26 September 2017.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kim, M.S., Choi, J. & Shin, W.C. AIMS65 scoring system is comparable to Glasgow-Blatchford score or Rockall score for prediction of clinical outcomes for non-variceal upper gastrointestinal bleeding. BMC Gastroenterol 19, 136 (2019). https://doi.org/10.1186/s12876-019-1051-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-019-1051-8