Abstract
Background
Clinical practice guidelines (CPGs) synthesize high-quality information to support evidence-based clinical practice. In primary care, numerous CPGs must be integrated to address the needs of patients with multiple risks and conditions. The BETTER program aims to improve prevention and screening for cancer and chronic disease in primary care by synthesizing CPGs into integrated, actionable recommendations. We describe the process used to harmonize high-quality cancer and chronic disease prevention and screening (CCDPS) CPGs to update the BETTER program.
Methods
A review of CPG databases, repositories, and grey literature was conducted to identify international and Canadian (national and provincial) CPGs for CCDPS in adults 40–69 years of age across 19 topic areas: cancers, cardiovascular disease, chronic obstructive pulmonary disease, diabetes, hepatitis C, obesity, osteoporosis, depression, and associated risk factors (i.e., diet, physical activity, alcohol, cannabis, drug, tobacco, and vaping/e-cigarette use). CPGs published in English between 2016 and 2021, applicable to adults, and containing CCDPS recommendations were included. Guideline quality was assessed using the Appraisal of Guidelines for Research and Evaluation (AGREE) II tool and a three-step process involving patients, health policy, content experts, primary care providers, and researchers was used to identify and synthesize recommendations.
Results
We identified 51 international and Canadian CPGs and 22 guidelines developed by provincial organizations that provided relevant CCDPS recommendations. Clinical recommendations were extracted and reviewed for inclusion using the following criteria: 1) pertinence to primary prevention and screening, 2) relevance to adults ages 40–69, and 3) applicability to diverse primary care settings. Recommendations were synthesized and integrated into the BETTER toolkit alongside resources to support shared decision-making and care paths for the BETTER program.
Conclusions
Comprehensive care requires the ability to address a person’s overall health. An approach to identify high-quality clinical guidance to comprehensively address CCDPS is described. The process used to synthesize and harmonize implementable clinical recommendations may be useful to others wanting to integrate evidence across broad content areas to provide comprehensive care. The BETTER toolkit provides resources that clearly and succinctly present a breadth of clinical evidence that providers can use to assist with implementing CCDPS guidance in primary care.
Similar content being viewed by others
Background
Turning the tide on chronic disease is a major health system priority and integral to improving health outcomes, services, and costs. Seventy-three percent of Canadians 65 years of age and older have at least 1 of the 10 most common cancers and/or chronic diseases [1]. Many of these could be prevented through management of modifiable risk factors and early detection through screening [2].
Primary care provides the first contact for patients in the healthcare system and therefore is an ideal setting to implement cancer and chronic disease prevention and screening (CCDPS) in Canada. Unfortunately, a substantial gap exists between clinical recommendations for CCDPS and actual practice [2,3,4,5,6]. Due to a fragmented healthcare system and provider time constraints, implementation of guidelines tends to focus on recommendations for specific organ systems, medical conditions, or single risk factors [6, 7]. Initiatives such as the Canadian Cardiovascular Harmonized National Guidelines Endeavour (C-CHANGE) [8,9,10] and the Building on Existing Tools to Improve Chronic Disease Prevention and Screening in Primary Care (BETTER) program [6, 11] exemplify efforts to present compilations of high-quality, evidence-based recommendations across multiple conditions in a way that is accessible and actionable by primary care providers (PCPs).
The BETTER program [12], with over 15 years of in-depth study, has developed a novel, comprehensive approach to CCDPS in primary care based on the Chronic Care Model (CCM), which identifies essential elements needed to provide comprehensive, proactive care for patients with chronic conditions from health promotion to disease management [13,14,15]. This approach introduces an enhanced role, the Prevention Practitioner (PP), typically undertaken by a clinician not responsible for ongoing care decisions or routine care. The PP works directly with patients to determine which CCDPS actions they are eligible to receive, and through a process involving shared decision-making and S.M.A.R.T. (specific, measurable, attainable, realistic, time-bound) goal setting, develops a unique, personalized “prevention prescription” with each patient [16]. The evidence-based prevention prescription is rooted in harmonized, high-quality CCDPS guidelines and tailored to patients based on their medical history, risk factors, and family history. This cost-effective intervention has been demonstrated to improve uptake of CCDPS actions in urban primary care settings as compared to usual care [2] and similar improvements have been observed in rural and remote communities [17] and public health settings [18] across Canada.
In this paper, we describe the rigorous process undertaken to synthesize and harmonize high-quality CCDPS clinical practice guidelines (CPGs) to update the clinical recommendations used in the BETTER program. This work was part of the Building on Existing Tools to Improve Cancer and Chronic Disease Prevention and Screening in Primary Care for Wellness of Cancer Survivors and Patients (BETTER WISE) project, a multi-provincial cluster randomized controlled trial (cRCT) [19]. The results from the BETTER WISE trial, including patient-level outcomes to assess the effectiveness of the approach and qualitative findings describing the impacts of the global pandemic of coronavirus disease 2019 (COVID-19) on the trial and overall prevention and screening services in primary care, are reported elsewhere [20,21,22]. We also describe the updated BETTER toolkit, a unique set of resources and tools aimed at supporting prevention of multiple cancers and chronic conditions in the primary care setting. Refinement of the toolkit was undertaken due to changes to the clinical evidence since its last iteration and to include new content areas informed by emerging evidence and feedback received from end-users. The BETTER toolkit informs the PP role and provides PCPs with accessible evidence-based clinical practice tools to address CCDPS.
Methods
Overview of the evidence review and CPG harmonization process
The process used to search, identify, appraise, synthesize, and harmonize CPGs for the BETTER program builds on our previous work [6, 11], and involved the development of a compilation of robust CCDPS recommendations across the targeted conditions and risk factors while ensuring these were actionable and implementable in diverse settings across Canada. The clinical recommendations previously included were appliable to patients 40–65 years of age and encompassed the following areas: 1) cancers—breast, cervical, colorectal, lung and prostate; 2) chronic diseases – diabetes, cardiovascular disease, and obesity; 3) other conditions – depression; and 4) lifestyle risk factors – diet, physical activity, and alcohol and tobacco use. As described elsewhere [6, 11], implementation science theories, models, and frameworks were used to inform the BETTER program and the approach undertaken to update the clinical evidence for the program to ensure that these recommendations were relevant, practical, feasible, and implementable in primary care settings.
The BETTER evidence review and CPG synthesis/harmonization process involved 3 main phases: 1) evidence review and identification of high-quality CPGs; 2) guideline synthesis and harmonization to standardize recommendations; and 3) refinement of the BETTER toolkit. These 3 phases were conceptualized within the Canadian Institutes of Health Research (CIHR) knowledge-to-action process model, a conceptual framework that depicts the process of knowledge translation as a continuous cycle with knowledge creation at the core and the activities related to “action” or application/implementation of created knowledge at the periphery [6, 11, 19, 23]. This model has been identified as an implementation tool that can guide the process of translating evidence into practice [24]. This process culminated in the refinement and creation of knowledge resources and tools to support primary prevention and screening for relevant cancers and chronic diseases: the BETTER toolkit. Composed of clinical tools that succinctly and visually represent the clinical recommendations used in the program as well as a collection of accessible programs and resources available to providers and patients to support CCDPS efforts, the BETTER toolkit includes: a health survey, care paths for prevention and screening, a prevention prescription, a S.M.A.R.T. goals sheet, and bubble diagrams which provide CCDPS targets for patients at average risk.
Phase 1: evidence review and identification of high-quality CPGs
Review of the literature
An evidence review involving a targeted search strategy developed by the Centre for Effective Practice (CEP) [25] (a non-profit independent knowledge translation organization based in Toronto, Canada,) was conducted for 19 topics related to CCDPS in the following areas: 1) cancers—breast, cervical, colorectal, lung and prostate; 2) chronic diseases – chronic obstructive pulmonary disease (COPD), diabetes, cardiovascular disease, hepatitis C, obesity, and osteoporosis/bone health; 3) other conditions – depression; and 4) lifestyle risk factors – diet, physical activity, alcohol, cannabis, drug, tobacco, and vaping/e-cigarette use.
Search criteria and search strategy
The search updated the previous evidence review, which was conducted in 2016 [6, 11], and was limited to CPGs published in English between 2016 and 2021 focused on adults. Priority was given to Canadian guidelines (national and provincial – Alberta, Ontario, Newfoundland and Labrador, and Nova Scotia as these jurisdictions were engaged in the BETTER WISE project or actively implementing the BETTER program). Guidelines were excluded if they solely provided recommendations for diagnosis, treatment, or management of cancer, and not screening or prevention of cancer, or if they were not applicable to the primary care setting as the focus of the BETTER program is primary prevention and screening of cancer and chronic disease in primary care.
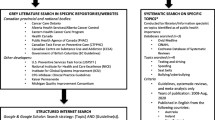
The 4-step search strategy used by the CEP to identify CPGs for each topic is described in Table 1. Specific details regarding the search strategies for each topic are provided in Appendix 1. Titles and abstracts of CPGs identified through this search were reviewed for relevance, and promising results were retrieved in full-text for further consideration.
CPG quality appraisal
Full-text guidelines underwent an initial quality appraisal using the Appraisal of Guidelines for Research and Evaluation (AGREE) II Instrument, the purpose of which is to evaluate the process of CPG development and quality of reporting [26]. To pass the initial quality check performed by trained reviewers at the CEP, a guideline had to include clear recommendations linked to levels of evidence and be based on a systematic review of the literature (items 7 and 12 in the “Rigour of Development” domain of AGREE II). CPGs that fulfilled these criteria were appraised independently by 2 reviewers using the full AGREE II, consisting of 23 items across 6 domains and an overall quality score, in preparation for Phase 2. These appraisals were subsequently reviewed by a lead expert reviewer and reconciled into a single score to provide an overall summary of the methodological quality of each guideline.
A review was also conducted to identify guidelines published by provincial organizations in the 4 jurisdictions of interest. Provincial guidance documents published between 2016 and 2021, regardless of whether or not they passed the “Rigour of Development” criteria described above, were included for review in Phase 2 because of their relevance to the local context, as the BETTER program was actively being implemented in these jurisdictions and we needed to ensure that the recommendations incorporated into the program would be actionable, accounting for regional differences. The recommendations from the included high-quality CPGs and key provincial guidelines were extracted into evidence tables for review in Phase 2, which also included each recommendation’s level of evidence and the strength of recommendation, where available.
Phase 2: guideline synthesis and harmonization to standardize recommendations
The BETTER Clinical Working Group (CWG) was convened for 5 months (January to May 2022) to review the international and Canadian CPGs identified through Phase 1 and to integrate recommendations and resources for inclusion in the BETTER program (see Fig. 1). Members of the CWG included patients, health policy experts (regional, provincial, federal; government and non-government), PCPs, content experts (e.g., cancer, obesity, diabetes, lifestyle risk factors), and primary care and primary healthcare researchers who shared their perspectives to synthesize and harmonize the identified CPGs into clear, actionable recommendations. In this phase, the CWG was divided into 3 topic-review teams based on their area(s) of expertise:
-
1.
Cancer team (5 members), focusing on breast, cervical, colorectal, lung, and prostate cancer;
-
2.
Chronic disease team (10 members), focusing on cardiovascular disease, COPD, depression, diabetes, hepatitis C, obesity, and osteoporosis; and
-
3.
Lifestyle risk factor team (4 members), focusing on alcohol, cannabis, drug, tobacco, and vaping/e-cigarette use, diet, and physical activity.
Topic-review teams worked independently to evaluate each recommendation within their ambit for clarity, actionability, and to determine if the recommendation could be operationalized in the primary care setting based on the following criteria: 1) focus on primary prevention and screening; 2) relevance to adults 40–69 years of age, the age group to which most CCDPS recommendations apply; and 3) applicability to primary care settings across different Canadian jurisdictions. Specifically, team members voted “yes” (i.e., include in BETTER), “no” (i.e., do not include in BETTER) with rationale for any “no” votes clearly documented, and “maybe” (i.e., further discussion required). The topic-review teams presented their assessments to the larger CWG at scheduled meetings. Any disagreements or ambiguities were resolved through discussion until consensus for inclusion or exclusion was reached. In cases where multiple individual recommendations for a topic were endorsed for inclusion, these were combined, harmonized, and simplified when appropriate, through group discussion. Recommendations emerging from provincial guidance documents that did not meet the initial quality appraisal criteria were reviewed and harmonized alongside those derived from the high-quality CPGs to ensure that recommendations were actionable in different contexts. Most of these provincial recommendations were consistent with those already incorporated, though there were some regional differences. For example, provincial guidance differed in regard to the criteria that should be used to determine the appropriate screening modality for an individual at elevated risk for colon cancer, all of which were reasonable based upon the high-quality guidance. Any jurisdictional nuances, such as differences in frequency of screening, were captured and indicated in the harmonized recommendations. Across all topics, individual and family risk factors (e.g., genetics, pre-existing medical conditions [personal or family], ethnic background) were incorporated to ensure that recommendations specific to high-risk and average-risk individuals were clear [11].
In Step 1, each topic-review team reviewed the international and national CPG recommendations identified through Phase 1 (see Fig. 1). As part of this first step, members were also asked to identify any high level international and national guidelines of which they were aware that were not included in their review. In Step 2, international and national clinical recommendations that reached consensus for inclusion were compared with provincial recommendations and policies to determine whether they were implementable in the 4 Canadian provinces of interest. For example, at the time of these discussions, the use of low-dose computed tomography (CT) scan for lung cancer screening, flexible sigmoidoscopy for average-risk colorectal cancer screening, and HPV testing for cervical cancer screening each varied among the different provinces. Any provincial clinical recommendations that differed from those already included and which were necessary to comply with a province’s approach to CCDPS were accepted for inclusion, noting the specific relevance to that province.
Finally, in Step 3, the topic-review teams reviewed the tools and resources previously included in the BETTER program [6, 11] alongside new tools/resources that were identified through our search strategy. Teams reflected on the tools’ clarity (i.e., use of unambiguous, understandable language), applicability (e.g., to diverse populations, patients 40–69 years of age), and clinical usefulness (e.g., for primary care settings and PPs). Validity was also considered for assessment tools (e.g., Patient Health Questionnaire 2-item (PHQ-2) [27] screen for depression, QRISK3 [28] cardiovascular disease risk calculator, and General Practice Physical Activity Questionnaire (GPPAQ) [29] screen for aerobic physical activity). Through this process, teams assembled updated, relevant, and useful clinician and/or patient-facing tools and resources to support the implementation of recommendations.
Phase 3: refinement of the BETTER toolkit
The final CPG recommendations selected for inclusion were synthesized and harmonized using succinct, clear, and actionable language while considering PCPs’ and PPs’ scope of practice, role in patient care, and linkages to community resources. These recommendations were then used to refine the existing BETTER toolkit to assist PCPs and PPs with the implementation of recommendations. The toolkit provides PCPs and patients with the tools and resources needed to: 1) evaluate the individual patient’s risks for cancer and chronic disease, 2) identify CCDPS action(s) relevant to the patient, and 3) educate and prevent cancer and chronic diseases through a process of shared decision-making, resulting in a personalized ‘prevention prescription’ and actionable goals for the patient [11].
Results
Search results and clinical recommendations
The titles and abstracts of 6,038 CPGs identified through the search strategy were reviewed for relevance to CCDPS and primary care settings. Of these, 243 guidelines were retrieved, considered in full-text, and underwent initial quality appraisal. CPGs that passed the initial quality appraisal and that were further assessed using the full AGREE II received an overall quality score between 0 and 7, where a higher score indicates higher overall quality, with 7 indicating a CPG of the highest quality [26]. Thirteen percent of the CPGs assessed using the full AGREE II received an overall quality score of 4, 28% received a score of 5, 55% received a score of 6, and 4% received a score of 7 (see Appendix 3 for full AGREE II scores, including scores for overall quality). After excluding those that did not meet the inclusion or quality criteria, Phase 1 yielded 51 CPGs which provided current, relevant CCDPS recommendations for the general population (see Fig. 2). A summary of the search results is provided in Appendix 2.
PRISMA diagram
*Guidelines reviewed in full text. Initial quality appraisal completed using two key items assessing ‘Rigour of Development’ in the AGREE II instrument (items 7 and 12). A score of 5 or more in these domains typically indicates that the criteria is satisfied, however, guidelines with domain scores of least a 3 were considered for further appraisal** Appraised using full, 23-item, AGREE II Instrument. An additional 22 provincial guidelines were identified and included for review in Phase 2
Supplementary searches identified an additional 22 guidelines by provincial organizations in Alberta, Ontario, Nova Scotia, and Newfoundland and Labrador, which were also reviewed by the BETTER CWG in Phase 2. Discussions within topic-review teams and the larger CWG determined that 3 of the new topics proposed (COPD, hepatitis C, and drug use) did not have sufficient evidence for inclusion (e.g., lack of prevention and screening CPGs for the topic, focus on diagnosis, treatment, and/or management) and thus were excluded from the final recommendations, resulting in 16 topics included in the program – 3 new: osteoporosis/bone health, cannabis use, and vaping/e-cigarette use. Notably, there were no CPGs published between 2016 and 2021 that met our criteria for inclusion on the topic of depression. The decision made by the CWG was to include a recommendation to screen for depression since this was already a part of the BETTER program. The final recommendations and resources/tools included in the BETTER program are presented in Tables 2 and 3, respectively.
Updates to the BETTER toolkit
The updated BETTER toolkit consists of clinical practice tools and resources that help assess patients, support patient education, shared decision-making, and self-management, including regional, provincial, and national resources that patients can access (via a provider or self-referral) to help them achieve their health goals. The BETTER toolkit includes:
-
1.
The BETTER Primary Prevention and Screening Maps (Figs. 3a and b, 4a, and b), depict the harmonized clinical recommendations included in the BETTER program for adults 40–69 years of age (summarized in Table 2). Represented as care paths for each CCDPS topic, the maps are intended to help PCPs determine a patient’s eligibility for CCDPS as well as appropriate next steps, including frequency of screening and recommended screening modality based on personal medical history, family history, and genetics.
-
2.
A patient survey, which captures a patient’s detailed prevention and screening history, including lifestyle risks and family history. The survey contains validated tools (e.g., PHQ-2, GPPAQ) and documents patients’ level of confidence and how prepared they are to make changes.
-
3.
The BETTER Bubble Diagrams (Figs. 5a and b), which are patient- and clinician- friendly representations of the BETTER prevention and screening maps with sex specific targets for patients at average risk. A blank version can be used as a patient-teaching tool to illustrate the patient’s current health status and their risk factors for each ‘bubble’ to help guide the conversation.
-
4.
A prevention prescription (Fig. 6), which provides a summary of the patient’s risk for cancer and chronic disease, their screening and prevention targets, and any follow-up actions that may be required.
-
5.
A goals sheet (Fig. 7) that summarizes the patient’s personalized, self-directed, actionable S.M.A.R.T. goals.
-
6.
A compilation of regional, provincial, and national resources and tools for patients and PCPs to support implementation of CCDPS recommendations, inform patients, and support patients’ health goals (Table 3).
Discussion
Improving CCDPS in primary care is crucial to reducing the burden of cancer and chronic disease and increasing the sustainability of the healthcare system. In this paper, we describe the development of a comprehensive suite of resources and harmonization of recommendations that support CCDPS in patients 40–69 years of age. These are tailored to the individual by taking their personal medical history, family history, and genetics into consideration and for implementation in 4 Canadian provinces by incorporating provincial guidance. Stakeholders and end-users representing diverse perspectives (patients, policy makers, clinicians, and researchers) were engaged throughout the process to ensure that the clinical recommendations integrated into the BETTER program would be relevant, usable, and implementable.
Our evidence review involved a structured search of CPG databases, guideline developers, and grey literature to compile evidence-based clinical recommendations for CCDPS applicable to adults in the primary care setting. The resulting clinical recommendations expanded the age group for the BETTER program from 40–65 to 40–69 and added 3 new primary prevention and screening topics to the comprehensive scope of the program. In addition, clinical recommendations for secondary prevention of diabetes were introduced – retinopathy screening and screening for chronic kidney disease (see Table 2).
Informed by 51 international and Canadian CPGs and 22 guidelines from provincial organizations across 16 topics, the refined BETTER toolkit includes updated CCDPS care maps with succinct, clear, actionable recommendations that translate clinical evidence to PCPs to inform patient care, a streamlined patient survey to capture a patient’s prevention and screening history, and agenda setting tools to help set expectations for discussions with patients. The BETTER tools can be used at point of care to identify outstanding CCDPS actions and provide opportunities to address prevention and screening comprehensively, across many cancers and chronic diseases, with individual patients while considering their health goals, values, and preferences.
Initiated by the 1995 Institute of Medicine report Setting Priorities for Clinical Practice Guidelines [30], several decades of investment have resulted in robust methods to create high-quality guidelines; however, to achieve intended outcomes, CPGs must be implementable in real-world practice. The BETTER program has demonstrated that nuanced clinical tools can be designed to facilitate decision-making between PCPs and patients across multiple chronic diseases and lifestyle factors [2, 17, 18]. In this evidence review, we extended our topic scope, included health policy makers and patients in the evidence synthesis process, and tailored the included clinical recommendations for implementation in 4 Canadian provinces. The BETTER program process, grounded in the intersection between clinical practice, health policy, and systematic evidence, addresses a needed step to ensure feasible implementation of CPGs.
We recognize that our approach has limitations. Our population of interest was limited to adults 40–69 years of age with a focus on CCDPS and related risk factors. However, we believe that our approach may be useful to extend the work to different age groups, secondary prevention, and chronic disease management. All guidelines included in our review were published between 2016 and 2021 and as a result, recommendations from recent research, including guidelines published following the COVID-19 pandemic, would have been missed. For example, while the BETTER toolkit was being refined, two Canadian CPGs relating to cardiovascular disease [9] and alcohol use [31] were published in 2022 and 2023, respectively. To ensure that the recommendations used in the BETTER program remained clinically relevant, a subset of the BETTER CWG reviewed the CPGs and decided to include their recommendations. This highlights the importance of periodically and consistently reviewing the existing evidence to ensure that clinical practice is informed by the best current guidance. Though the clinical guidance was tailored to 4 jurisdictions in Canada and may not be applicable to other global jurisdictions or Canadian regions, the national recommendations included are relevant to a broad Canadian audience, and the tailoring methods used may prove useful to others when incorporating guidance for use in their context.
We developed a structured approach to synthesizing and blending CPG recommendations for application into primary care settings as described in our previous work [6, 11]. The process involved members of the Clinical Working Group sharing their diverse perspectives during group discussions to reach consensus for inclusion, harmonization, and synthesis of clinical recommendations extracted from high-quality CPGs. Though this approach is novel and not as recognized as other methodological approaches, such as the Delphi Method, it may still be used to guide and inform others on how to incorporate current clinical guidance into practice. Lastly, members of the Clinical Working Group were not asked to declare possible conflicts of interest prior to their involvement in the evidence review process; however, they represented diverse groups (PCPs, other healthcare professionals, patients, health policy specialists, content experts, researchers) from 4 Canadian Provinces, many of whom are authors on this manuscript and who have declared any competing interests here.
Conclusions
The process used by the BETTER program to synthesize and harmonize international and Canadian CPG recommendations resulted in a suite of tools and resources to support CCDPS in primary care practice. This approach incorporates diverse perspectives of patients, PCPs, and health policy makers to ensure usability in real-world practice. Used together, the BETTER toolkit provides resources and tools that clearly and succinctly express the breath of high-quality clinical evidence that was synthesized into actionable recommendations to help inform patient care and enable primary care providers to address CCDPS comprehensively in their clinical settings. The methods used may be applicable to others contemplating integrating evidence across broad content areas in primary care to help facilitate comprehensive care. The updated BETTER toolkit is available to PCPs and interprofessional team members practicing in Canadian primary care settings through the BETTER program [12].
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed as part of the work described in this manuscript.
Abbreviations
- AGREE II:
-
Appraisal of Guidelines for Research & Evaluation II
- BETTER:
-
Building on Existing Tools to Improve Chronic Disease Prevention and Screening in Primary Care
- BETTER WISE:
-
Building on Existing Tools to Improve Cancer and Chronic Disease Prevention and Screening in Primary Care for Wellness of Cancer Survivors and Patients
- CCDPS:
-
Cancer and chronic disease prevention and screening
- CCM:
-
Chronic care model
- C-CHANGE:
-
Canadian Cardiovascular Harmonized National Guidelines Endeavour
- CEP:
-
Centre for Effective Practice
- CIHR:
-
Canadian Institutes of Health Research
- COPD:
-
Chronic obstructive pulmonary disease
- COVID-19:
-
Coronavirus disease of 2019
- CPG:
-
Clinical practice guideline
- cRCT:
-
Cluster randomized controlled trial
- CT:
-
Computed tomography
- CWG:
-
Clinical Working Group
- GPPAQ:
-
General Practice Physical Activity Questionnaire
- PCP:
-
Primary care provider
- PHQ-2:
-
Patient Health Questionnaire 2-item
- PP:
-
Prevention practitioner
- SMART:
-
Specific, measurable, attainable, realistic, time-bound
References
Public Health Agency of Canada. Prevalence of Chronic Diseases and Risk Factors among Canadians aged 65 years and older 2020 2020 [Available from: https://www.canada.ca/en/services/health/publications/diseases-conditions/prevalence-chronic-disease-risk-factors-canadians-aged-65-years-older.html.
Grunfeld E, Manca D, Moineddin R, Thorpe KE, Hoch JS, Campbell-Scherer D, et al. Improving chronic disease prevention and screening in primary care: results of the BETTER pragmatic cluster randomized controlled trial. BMC Fam Pract. 2013;14:175.
Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–41.
Porter J, Boyd C, Skandari MR, Laiteerapong N. Revisiting the time needed to provide adult primary care. J Gen Intern Med. 2023;38(1):147–55.
Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8 Suppl 2):II46-54.
Campbell-Scherer D, Rogers J, Manca D, Lang-Robertson K, Bell S, Salvalaggio G, et al. Guideline harmonization and implementation plan for the BETTER trial: building on existing tools to improve chronic disease prevention and screening in family practice. CMAJ Open. 2014;2(1):E1–10.
Manca DP, Greiver M, Carroll JC, Salvalaggio G, Cave A, Rogers J, et al. Finding a BETTER way: a qualitative study exploring the prevention practitioner intervention to improve chronic disease prevention and screening in family practice. BMC Fam Pract. 2014;15:66.
Tobe SW, Stone JA, Anderson T, Bacon S, Cheng AYY, Daskalopoulou SS, et al. Canadian Cardiovascular Harmonized National Guidelines Endeavour (C-CHANGE) guideline for the prevention and management of cardiovascular disease in primary care: 2018 update. CMAJ. 2018;190(40):E1192–206.
Jain R, Stone JA, Agarwal G, Andrade JG, Bacon SL, Bajaj HS, et al. Canadian Cardiovascular Harmonized National Guideline Endeavour (C-CHANGE) guideline for the prevention and management of cardiovascular disease in primary care: 2022 update. CMAJ. 2022;194(43):E1460–80.
Tobe SW, Stone JA, Brouwers M, Bhattacharyya O, Walker KM, Dawes M, et al. Harmonization of guidelines for the prevention and treatment of cardiovascular disease: the C-CHANGE Initiative. CMAJ. 2011;183(15):E1135–50.
Manca DP, Campbell-Scherer D, Aubrey-Bassler K, Kandola K, Aguilar C, Baxter J, et al. Developing clinical decision tools to implement chronic disease prevention and screening in primary care: the BETTER 2 program (building on existing tools to improve. Implement Sci. 2015;10:107.
The BETTER Program [Available from: www.better-program.ca.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9.
Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–44.
Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q. 2003;7(1):73–82.
Sopcak N, Fernandes C, O’Brien MA, Ofosu D, Wong M, Wong T, et al. What is a prevention visit? A qualitative study of a structured approach to prevention and screening - the BETTER WISE project. BMC Fam Pract. 2021;22(1):153.
Aubrey-Bassler K, Fernandes C, Penney C, Cullen R, Meaney C, Sopcak N, et al. The effectiveness of a proven chronic disease prevention and screening intervention in diverse and remote primary care settings: an implementation study on the BETTER 2 Program. BJGP Open. 2019;3(3). https://bjgpopen.org/content/3/3/bjgpopen19X101656.
Lofters AK, O’Brien MA, Sutradhar R, Pinto AD, Baxter NN, Donnelly P, et al. Building on existing tools to improve chronic disease prevention and screening in public health: a cluster randomized trial. BMC Public Health. 2021;21(1):1496.
Manca DP, Fernandes C, Grunfeld E, Aubrey-Bassler K, Shea-Budgell M, Lofters A, et al. The BETTER WISE protocol: building on existing tools to improve cancer and chronic disease prevention and screening in primary care for wellness of cancer survivors and patients - a cluster randomized controlled trial embedded in a mixed methods design. BMC Cancer. 2018;18(1):927.
Manca DP, Fernandes C, Lofters A, Aubrey-Bassler K, Shea-Budgell M, Campbell-Scherer D, et al. Results from the BETTER WISE trial: a pragmatic cluster two arm parallel randomized controlled trial for primary prevention and screening in primary care during the COVID-19 pandemic. BMC Prim Care. 2023;24(1):200.
Sopcak N, Fernandes C, Ofosu D, Wong M, Khalil I, Wong T, et al. Facilitators and Barriers to the Implementation of BETTER WISE, a Chronic Disease and Prevention Intervention in Canada: A Qualitative Study. Glob Implement Res Appl. 2023;3(2):162–72.
Sopcak N, Wong M, Fernandes C, Ofosu D, Khalil I, Manca D. Prevention and screening during the COVID-19 pandemic: qualitative findings from the BETTER WISE project. BMC Prim Care. 2023;24(1):27.
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13–24.
Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53.
Centre for Effective Practice [Available from: https://cep.health/.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839–42.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–92.
Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099.
National Health Service. The General Practice Physical Activity Questionnaire (GPPAQ): A screening tool to assess adut physical activity levels within primary care. 2009.
Institute of Medicine. Setting Priorities for Clinical Practice Guidelines. Field MJ, editor. Washington (DC): National Academy Press; 1995.
Paradis C, Butt P, Shield K, Poole N, Wells S, Naimi T, et al. Canada’s Guidance on Alcohol and Health: Final Report. Ottawa, ON; 2023.
British Columbia Centre on Substance Use. Provincial Guideline for the Clinical Management of High-Risk Drinking and Alcohol Use Disorder. British Columbia Centre on Substance Use (BCCSU); 2019.
Allen S, Forney-Gorman A, Homan M, Kearns A, Kramlinger A, Sauer M. Diagnosis and Treatment of Osteoporosis. Institute for Clinical Systems Improvement; 2017.
U. S. Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(18):1899–909.
The Management of Substance Use Disorders Work Group. VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders. In: Department of Veterans Affairs and Department of Defense, editor.: Department of Veterans Affairs and Department of Defense; 2021.
Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, et al. Hypertension Canada’s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2020;36(5):596–624.
ASaP+ Alcohol Use: Recommendation, Rationale and Supplemental References. Alberta Health Services, Alberta Cancer Prevention Legacy Fund; 2019.
Quality Standards: Problematic Alcohol Use and Alcohol Use Disorder. Care for People 15 Years of Age and Older. Ontario Health (Health Quality Ontario); 2020.
Nova Scotia Breast Screening of Average Risk Women. Nova Scotia Health Authority; 2019.
Hamashima C, Japanese Research Group for the Development of Breast Cancer Screening G, Hamashima CC, Hattori M, Honjo S, Kasahara Y, et al. The Japanese Guidelines for Breast Cancer Screening. Jpn J Clin Oncol. 2016;46(5):482–92.
Clinical Practice Guidelines – Breast Disease Site: Indications for Use of Breast Magnetic Resonance Imaging (MRI). Eastern Health; 2018.
Klarenbach S, Sims-Jones N, Lewin G, Singh H, Theriault G, Tonelli M, et al. Recommendations on screening for breast cancer in women aged 40–74 years who are not at increased risk for breast cancer. Can Med Assoc J. 2018;190(49):E1441–51.
Migowski A, Silva GAE, Dias MBK, Diz M, Sant’Ana DR, Nadanovsky P. Guidelines for early detection of breast cancer in Brazil. II - New national recommendations, main evidence, and controversies. Cad Saude Publica. 2018;34(6):e00074817.
Ontario Breast Screening Program (OBSP). Guidelines Summary. Ontario Health (Cancer Care Ontario ); 2015.
Breast Cancer Screening. Summary of the Clinical Practice Guideline Toward Optimized Practice. 2015.
Fischer B, Russell C, Sabioni P, van den Brink W, Le Foll B, Hall W, et al. Lower-Risk Cannabis Use Guidelines: A Comprehensive Update of Evidence and Recommendations. Am J Public Health. 2017;107(8):e1–12.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74(10):e177–232.
The Management of Dyslipidemia for Cardiovascular Risk Reduction Working Group. VA/DoD Clinical Practice Guideline for the Management of Dyslipidemia for Cardiovascular Risk Reduction. In: Department of Veterans Affairs and Department of Defense, editor.: Department of Veterans Affairs and Department of Defense. 2020.
Revised Screening Maneuvers Menu for Adults: Alberta Screening and Prevention Program (ASaP). Toward Optimized Practice. 2017.
Fontham ETH, Wolf AMD, Church TR, Etzioni R, Flowers CR, Herzig A, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70(5):321–46.
U. S. Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(7):674–86.
Cervical Cancer Screening Clinical Practice Guideline. Toward Optimized Practice; 2016.
Ontario Cervical Screening Program (OCSP) Screening Recommendations Summary. Ontario Health (Cancer Care Ontario); 2020.
Health Professional Guide: Cervical Screening Practice Guidelines. In: Program NSCC, editor.: Nova Scotia Health Authority; 2019.
Cervical Screening Guidelines for Newfoundland and Labrador. Cervical Screening Initiatives; 2016.
Canadian Task Force on Preventive Health C. Recommendations on screening for colorectal cancer in primary care. CMAJ. 2016;188(5):340–8.
U. S. Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(19):1965–77.
Helsingen LM, Vandvik PO, Jodal HC, Agoritsas T, Lytvyn L, Anderson JC, et al. Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: a clinical practice guideline. BMJ. 2019;367:l5515.
Leddin D, Lieberman DA, Tse F, Barkun AN, Abou-Setta AM, Marshall JK, et al. Clinical Practice Guideline on Screening for Colorectal Cancer in Individuals With a Family History of Nonhereditary Colorectal Cancer or Adenoma: The Canadian Association of Gastroenterology Banff Consensus. Gastroenterology. 2018;155(5):1325-47 e3.
Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68(4):250–81.
Colorectal Cancer Screening Clinical Practice Guideline. Toward Optimized Practice; 2020.
ColonCancerCheck (CCC) Guide to Average Risk Screening with the Fecal Immunochemical Test (FIT) in Ontario. Ontario Health (Cancer Care Ontario); 2020.
Clinical Practice Guidelines: Newfoundland & Labrador Colon Screening Program (NLCSP). Eastern Health; 2019.
Depression in adults: recognition and management. NICE Clinical guideline. National Institute for Health and Care Excellence; 2009.
Joffres M, Jaramillo A, Dickinson J, Lewin G, Pottie K, Shaw E, et al. Recommendations on screening for depression in adults. CMAJ. 2013;185(9):775–82.
Siu AL, Force USPST, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, et al. Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315(4):380–7.
Trangle M, Gursky J, Haight R, Hardwig J, Hinnenkamp T, Kessler D, et al. Adult Depression in Primary Care. Institute for Clinical Systems Improvement; Updated March 2016.
Canada D. Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes. 2018;2018(42):S1–325.
U. S. Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326(8):736–43.
The Management of Type 2 Diabetes Mellitus in Primary Care Work Group. VA/DoD Clinical Practice Guideline for the Managment of Type 2 Diabetes Mellitus in Primary Care. In: Department of Veterans Affairs and Department of Defense, editor.: Department of Veterans Affairs and Department of Defense. 2017.
Grunberger G, Sherr J, Allende M, Blevins T, Bode B, Handelsman Y, et al. American Association of Clinical Endocrinology Clinical Practice Guideline: The Use of Advanced Technology in the Management of Persons With Diabetes Mellitus. Endocr Pract. 2021;27(6):505–37.
Quality Standards: Prediabetes and Type 2 Diabetes. Care for People of All Ages. Ontario Health (Health Quality Ontario); 2021.
Rosella L, Bornstein S, Mackey S, Grignon M. Prevention and Screening for Type 2 Diabetes in Newfoundland and Labrador. St. John’s, NL: Newfoundland & Labrador Centre for Applied Health Research, Memorial University. 2016.
U. S. Preventive Services Task Force, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(10):962–70.
Mazzone PJ, Silvestri GA, Souter LH, Caverly TJ, Kanne JP, Katki HA, et al. Screening for Lung Cancer: CHEST Guideline and Expert Panel Report. Chest. 2021;160(5):e427–94.
Guidelines and Advice: Lung Cancer Screening Information for Healthcare Providers: Ontario Health (Cancer Care Ontario); n.d. [Available from: https://www.cancercareontario.ca/en/guidelines-advice/cancer-continuum/screening/lung-cancer-screening-information
Osteoporosis Prevention, Screening, and Diagnosis: ACOG Clinical Practice Guideline No. 1. Obstet Gynecol. 2021;138(3):494-506.
U. S. Preventive Services Task Force, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, et al. Behavioral Counseling Interventions to Promote a Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults With Cardiovascular Risk Factors: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;324(20):2069–75.
U. S. Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Behavioral Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(11):1163–71.
The Management of Adult Overweight and Obesity Work Group. VA/DoD Clinical Practice Guideline for the Management of Adult Overweight and Obesity. In: Department of Veterans Affairs and Department of Defense, editor.: Department of Veterans Affairs and Department of Defense. 2020.
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192(31):E875–91.
Nutrition Guideline: Adult Obesity Care. Alberta Health Services, Nutrition Services. 2020.
Scottish Intercollegiate Guidelines Network (SIGN). Management of osteoporosis and the prevention of fragility fractures. Edinburgh: Scottish Intercollegiate Guidelines Network (SIGN). 2021.
Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2019;104(5):1595–622.
U. S. Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Screening for Osteoporosis to Prevent Fractures: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(24):2521–31.
Qaseem A, Forciea MA, McLean RM, Denberg TD, Clinical Guidelines Committee of the American College of P, Barry MJ. Treatment of Low Bone Density or Osteoporosis to Prevent Fractures in Men and Women: A Clinical Practice Guideline Update From the American College of Physicians. Ann Intern Med. 2017;166(11):818–39.
Shoback D, Rosen CJ, Black DM, Cheung AM, Murad MH, Eastell R. Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Guideline Update. J Clin Endocrinol Metab. 2020;105(3):587–94.
Diagnosis and Managment of Osteoporosis. Clinical Practice Guideline.: Toward Optimized Practice; 2016.
WHO guidelines on physical activity and sedentary behaviour. Geneva; 2020.
Ross R, Chaput JP, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, et al. Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10 Suppl 2):S57–102.
U. S. Preventive Services Task Force, Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319(18):1901–13.
Carter HB, Albertsen PC, Barry MJ, Etzioni R, Freedland SJ, Greene KL, et al. Early detection of prostate cancer: AUA Guideline. J Urol. 2013;190(2):419–26.
Rendon RA, Mason RJ, Marzouk K, Finelli A, Saad F, So A, et al. Canadian Urological Association recommendations on prostate cancer screening and early diagnosis. Can Urol Assoc J. 2017;11(10):298–309.
Cancer Care Ontario Position Statement on Prostate Cancer Screening using the Prostate-Specific Antgen (PSA) Test. Ontario Health (Cancer Care Ontario); 2017.
Bell N, Connor Gorber S, Shane A, Joffres M, Singh H, Dickinson J, et al. Recommendations on screening for prostate cancer with the prostate-specific antigen test. CMAJ. 2014;186(16):1225–34.
U. S. Preventive Services Task Force, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, et al. Interventions for Tobacco Smoking Cessation in Adults, Including Pregnant Persons: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(3):265–79.
Registered Nurses’ Association of Ontario. Integrating Tobacco Interventions into Daily Practice. Toronto, ON; 2017.
Clinical Support Primer: Tobacco Harm Reduction - E-Cigarettes Alberta Health Services (Tobacco Reduction Program); 2019.
Vaping products including e-cigarettes. Ontario Health (Cancer Care Ontario); 2020.
Acknowledgements
The authors would like to acknowledge the contributions made to this work by Dr. J. Carroll who provided her family history and genetics expertise throughout the existence of the BETTER program, Department of Family Medicine Residents at the University of Alberta (H. Adl Golchin, H. Cai, J. Rogers) for participating as members of the chronic disease review team, members of the Centre for Effective Practice team who conducted assessments of identified clinical practice guidelines using the AGREE II tool (V. Burton, A. Du, V. Gnanapragasam, M. Gray), and M. Wong and F. Nagase for providing administrative support to the Clinical Working Group. The authors also acknowledge the contributions made by members of the 2017 BETTER Clinical Working Group whose work informed the BETTER WISE project intervention (K. Aubrey-Bassler, D. Campbell-Scherer, J. Carroll, R. Elford, E. Grunfeld, N. Hans, D. Klein, C. Korownyk, R. Lewanczuk, A. Lofters, D.P. Manca, M. Shea-Budgell, M. Wilson) and the graduate students who provided support for the group (I. Carneiro, M. Kebbe).
Funding
This work was made possible through funding received from Alberta Innovates via the Cancer Prevention Research Opportunity [2015 Collaborative Research and Innovation Opportunity (CRIO)] Grant #201500833. The opinions, results, and conclusions reported herein are those of the authors and do not necessarily represent the views of the funders. No endorsement by Alberta Innovates is intended nor should be inferred.
Author information
Authors and Affiliations
Contributions
AL, CF, DCS, DPM, EG, KAB, and MSB provided substantial contributions to the conception and design of the work. CD and KLR acquired, extracted, and appraised the clinical practice guidelines identified prior to review. AL, CF, DCS, DPM, EG, EH, HC, HY, KAB, KL, MW, RH, RL, SK, SW, TW, and WT contributed to the evidence review process, harmonization of recommendations, and knowledge product creation. CF, DCS, and DPM wrote the manuscript and all authors read and approved the final manuscript. We certify that all individuals listed as authors of this manuscript 1) have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) have been involved in drafting the manuscript or revising it critically for important intellectual content; 3) have given final approval of the version to be published; and 4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Author’s information
AL, DCS, DPM, EG, KAB, MW, RH, SW, and WT are family physicians and researchers with content expertise including expertise in qualitative and quantitative methodologies. CF is a senior research coordinator with expertise in implementation of the BETTER program and was the national research coordinator for BETTER WISE. HC is a respiratory therapist and a training and curriculum specialist with the BETTER program. KL is a dietitian and was a training and curriculum specialist with the BETTER program. RL is a physician, researcher, and policy maker with expertise in diabetes, health systems, and health policy. MSB is a research methodologist with expertise in oncology research and clinical guideline development. TW is an educator and researcher with expertise in advocacy. HY is a physician, researcher, and policy maker with expertise in screening programs, health systems, and health policy. EH is a researcher and policy maker with expertise in public health and cancer control. KLR and CD are librarians with expertise in literature reviews and quality assessment of clinical practice guidelines.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
CD and KLR report being employed by the Centre for Effective Practice through the BETTER WISE project to facilitate the guideline identification and harmonization process. AL, CF, DPM, and EG report serving as Directors of a Canadian not-for-profit organization, The BETTER Institute, which provides training and implementation support to practices, organizations, and communities interested in adopting or adapting the BETTER approach. All remaining authors do not have any competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Summary of Search Strategies.
Additional file 2: Appendix 2.
Summary of Search Results.
Additional file 3: Appendix 3.
Full AGREE II scores per clinical practice guideline (by topic area).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fernandes, C., Campbell-Scherer, D., Lofters, A. et al. Harmonization of clinical practice guidelines for primary prevention and screening: actionable recommendations and resources for primary care. BMC Prim. Care 25, 153 (2024). https://doi.org/10.1186/s12875-024-02388-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02388-3