Abstract
Background
The complexity of health systems necessitates coordination between a multitude of stakeholders to enact meaningful change. Primary care physicians are a crucial partner to engage, as their investment and participation are critical to the success of any system-level initiative. The aim of this scoping review is to identify common barriers and effective strategies when engaging primary care physicians in designing and implementing health system change.
Methods
A scoping review was performed. A literature search was performed in March 2020 using five databases. 668 unique articles were identified and underwent a title and abstract review. 23 articles met criteria for full text review and 10 met final inclusion criteria. A backward citation analysis identified two articles. 12 articles underwent data extraction and thematic analysis.
Results
Several barriers to engagement were identified including a lack of trust between primary care physicians and decision-makers, strong professional physician identity, clinically irrelevant and complex proposals, and a lack of capacity and supports. Described strategies to overcome these barriers included building trust and relationships, contextual engagement strategies, working with physician leadership, enabling open and intentional communication channels, designing clinically relevant and straightforward initiatives, and considering financial incentives.
Conclusions
Barriers to primary care engagement should be addressed with contextually designed strategies and a focus on relationship building, collaborative efforts, and implementing relevant and feasible initiatives. Further research should explore how to best develop relationships with primary care, working with collective voices of primary care physicians, and to better understanding the impact of financial incentives on engagement.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Health systems are designed to provide comprehensive medical care for a defined population. These systems are constantly changing in pursuit of the Quadruple Aim, focused on achieving better outcomes, improved patient experience, lower healthcare costs, and improved clinical experience [1, 2]. Health systems are composed of numerous stakeholders including patients, healthcare providers, governments, hospitals, and private industry. Engaging these stakeholders is essential when implementing change.
Primary care is the backbone of well-functioning and comprehensive health systems focused on improving health outcomes and health equity [3, 4]. According to the World Health Organization, primary care has three core tenets: meeting people’s health needs through comprehensive care throughout the life course, systematically addressing the broader determinants of health, and empowering individuals, families, and communities to optimize their health [5]. Given the breadth of services provided, improving primary care can have significant impacts on individual and population health that include improved vaccination and cancer screening rates, lower total health costs, reductions in health equity disparities, and lower mortality rates [6,7,8].
In Canada, health system performance is measured among eight different categories: acceptability, accessibility, appropriateness, competence, continuity, effectiveness, efficiency, and safety [9]. Changes to the health system and primary care should aim to improve one or more of these factors. Despite efforts by governments and decision-makers around the world attempting to reform primary care, engaging primary care physicians to enable change aimed at improving these factors has proven difficult. As the service providers of primary care, physicians have significant influence in determining the success or failure of any reforms. Poor engagement can derail even the most well-intentioned and comprehensive plans for health system change.
Given the importance of primary care physicians, decision-makers need to be intentional in how they engage this group of stakeholders. However, engaging primary care physicians is poorly understood and inconsistently executed by governments and decision-makers. The purpose of this scoping review is to identify common barriers and effective strategies to consider when engaging primary care physicians in designing and implementing health system change.
Methods
Scoping reviews are “exploratory projects that systematically map the literature available on a topic, identifying key concepts, theories, sources of evidence and gaps in the research” and “are often preliminary to full syntheses, undertaken when feasibility is a concern - either because the potentially relevant literature is thought to be especially vast and diverse or there is a suspicion that not enough literature exists” [10]. The methodological framework of Arksey and O’Malley and Levac et al. was used to guide the facilitation of the scoping review [11, 12]. The framework consists of: identifying the research question; identifying relevant studies; study selection; charting data; collating, summarizing, and reporting results; and stakeholder consultations.[11, 12]. Stakeholder consultations were facilitated concurrently with this review and those results will be published in the future. A protocol for this review was not published.
Identifying the research question
The review’s objective was to identify common barriers and effective strategies when engaging primary care physicians in designing and implementing health system change.
Identifying relevant studies
An initial search was performed in March 2020 on the following databases: PubMed, Cochrane Library, CINAHL, SCOPUS, and EMBASE. No date restrictions were applied to the search. Search terms included keywords related to family medicine, health system change, and engagement. Indexed subject headings were used in database searches when available. A research librarian from Western University was consulted to assist with search strategy development and execution. Search queries for each database are listed in Appendix 1.
Study selection
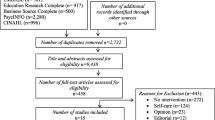
1081 results were identified in the databases search (Fig. 1). A manual review of duplicates was performed by one author (MST) and 413 duplicates were removed. The remaining 668 unique articles underwent a title and abstract review to identify articles for full text review. The inclusion criteria of the title and abstract review were: (1) specific mention of primary care or family medicine, (2)engagement in health system change, and (3) articles written in English. The exclusion criteria were: (1)focus on primary care provided by other generalist groups (e.g. internal medicine, pediatrics) and or non-physician professions (e.g. nurse practitioners), and (2) focus on patient engagement.
Two reviewers performed the title and abstract review (MST and JBB). Both reviewers independently assessed 25 of the 668 articles for inclusion and exclusion criteria that were randomly selected using an online number generator. Reviewers discussed determinations to ensure consistency in their individual assessments. Reviewers then assessed the remaining articles’ titles and abstracts. Following the independent assessments, the reviewers resolved disagreements through discussion. A third party was not required to resolve disagreements. Of the 668 articles, 23 met criteria for full text review.
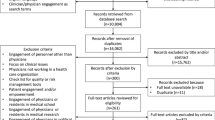
Full text review inclusion criteria were: (1) defines primary care as family medicine physicians or the equivalent in other countries, (2) focuses on at least one of three areas of primary care engagement in broad health system change (initiating engagement, maintaining engagement, or barriers and challenges in engaging primary care), and (3) articles written in English. The exclusion criteria were: (1) commentary articles, and (2) unavailable full text.
Two reviewers performed the full text review (MST and JBB). Both reviewers independently assessed 3 of the 23 articles for inclusion and exclusion criteria that were randomly selected using an online number generator. Reviewers discussed determinations to ensure consistency in their individual assessments. Reviewers then assessed the remaining articles’ titles and abstracts. Following the independent assessment, the reviewers resolved disagreements through discussion. A third party was not required to resolve disagreements. 10 articles met criteria for inclusion in the data extraction and analysis.
A backward citation analysis was then performed to identify articles from the reference sections of the 10 initially identified articles. Each reviewer (MST and JBB) assessed the titles of each reference. 321 titles were reviewed and 16 were identified by at least one reviewer for further evaluation of their abstracts. Five of the 16 articles met criteria for a full text review. Two articles met criteria for inclusion in the data extraction and analysis. The two articles underwent a repeated backward citation analysis. No relevant articles were identified from a total of 99 cited references.
Charting data
12 articles met criteria and underwent data extraction and categorization. Categories included: Authors, Title, Year of Publication, Journal, Country of Origin, Type of Study, Primary Care Definition, Barriers to Engagement, Engagement Initiation Strategies, Engagement Maintenance Strategies, and Overarching Lessons Learned. Five of the 12 articles were randomly selected, and data extraction was performed by two reviewers (MST and JBB). After completion by both reviewers, a meeting was held to ensure consistency in their individual assessments. Data extraction of the remaining 7 articles was then performed by MST. The charted data for those 7 articles was reviewed by JBB prior to continuing to thematic analysis.
Collating, summarizing and reporting the results
Qualitative thematic analysis was performed for the 12 included articles to group similar examples of barriers to engagement and strategies for effective engagement based on the information extracted in the Charting Data step. The two reviewers (MST and JBB) reviewed the charted data independently to establish common themes that addressed either barriers to engagement or strategies for effective engagement. The reviewers then met to discuss their independent analyses of the extracted data and discuss the overarching common barriers and strategies to effective engagement, which are described throughout the results section. A quantitative subgroup analysis of articles using quantitative or mixed methods was not performed.
Results
Study characteristics
Of the 12 articles included, six were conducted in Canada, three in the United States, two in the United Kingdom, and one in Australia (Table 1) [13,14,15,16,17,18,19,20,21,22,23,24]. Articles were published between 2014 and 2019. Nine of the 12 articles used a qualitative methodology, two used a quantitative methodology, and one used a mixed methods design.
Articles were assessed for findings that described barriers to engagement and strategies for the initiation and maintenance of engagement. Eleven of the twelve articles discussed barriers and ten of the twelve articles discussed initiation and maintenance strategies. Quotations extracted from the articles describing the barriers to engagement and strategies for effective engagement can be found in Tables 2 and 3, respectively.
Barriers to engagement
Four common barriers to engagement of primary care physicians by governments and decision-makers were identified among the articles: (1) lack of trust and poor relationships between primary care and decision-makers; (2) strong professional physician identity; (3) clinically irrelevant and complex proposals for change; and (4) lack of capacity and supports.
Lack of trust and poor relationships between primary care and decision-makers
Distrust in administration and governments often preceded change initiatives and was a significant hurdle to overcome when initiating the engagement process [13]. Exclusion of primary care in early discussions further exacerbated distrust and poor communication hindered collaborative efforts [14,15,16,17]. In some instances, physicians described differences in core values between physician and non-physician groups [17]. Others described a lack of primary care knowledge among decision-makers, leading to challenges in initiatives aimed at integrating care [18].
Strong professional physician identity
Professional autonomy and a strong physician identity were significant barriers. Primary care physicians desired control of clinical decision making and often viewed themselves as functioning independently of the larger health system [13, 14]. In some instances, change efforts created a spectrum of differing physician opinions [18]. Established physician groups that strengthened the physician voice could make change efforts quite difficult if the group were not in favour of the proposed change [19].
Clinically irrelevant and complex proposals for change
Primary care physicians were reluctant to engage if they felt interventions were unlikely to be clinically relevant or difficult to implement [20]. Unclear interventions and fears of increased administrative work without clinical improvement led to confusion and frustration that hampered efforts to further discussions [21].
Lack of capacity and supports
Lack of organizational and administrative supports for primary care physicians were deterrents to engagement [22]. Limited time and capacity further prevented engagement [15].
Strategies for effective engagement
Six strategies for effective engagement of primary care physicians by governments and decision-makers were identified among the articles: (1) building trust and collaborative relationships; (2) targeted engagement strategies as one size does not fit all; (3) physician leadership and collective voice; (4) open and intentional communication strategies; (5) clinically relevant initiatives and straightforward initiatives; and (6) financial incentives.
Building trust and collaborative relationships
Many studies highlighted trust as a key contributor to relationship building and cited both formal and informal efforts to develop these relationships with clinicians [13, 21]. For example, local administrators and primary care coordinators involved in a rural primary care setting were able act as translators between regional administrators and physicians because of predeveloped relationships, enabling dialogue that resulted in co-design of new programs and delivery of services [13].
Efforts to build trust were time-intensive and in some instances took years to develop [14]. Once relationships had been established, ongoing efforts were required to maintain them [13]. Fostering these relationships allowed for interdisciplinary partnerships to partake in shared strategic planning efforts [15].
Targeted engagement strategies as one size does not fit all
Many studies described generic engagement strategies like town-halls and newsletters. However, the most effective strategies were those created to engage a specific audience [24]. These specific strategies were effective, but also resource intensive [20].
Physician leadership and collective voice
Physician champions were a well-established role in engaging a larger primary care audience [23]. Beyond the leadership of individual physicians, an organized and credible collective physician voice sometimes provided a clear method for reaching a larger group to engage [13].
Open and intentional communication strategies
An open, non-judgemental communication channel was important in initiating engagement with physicians, especially for new or strained relationships [13]. Messaging mattered, as seen in instances where unclear language confused primary care physicians resulting in unproductive engagement efforts [17]. Intentional phrasing and communication strategies focused on developing a collaborative relationship with primary care physicians were helpful in cultivating ongoing engagement efforts [14].
Clinically relevant and straightforward initiatives
Administrators were able to improve engagement efforts by focusing initiatives on areas with clear efforts to improve patient care [13]. Physicians were more likely to buy in to initiatives if they were uncomplicated and tied to an observable measurement [21].
Financial incentives
Only one study had explicitly described providing funding to incentivize engagement. It was described as an effective strategy in engagement efforts [19]. However, few studies explored the role financial incentives had in promoting engagement. Some studies referenced articles that suggested financial incentives did not change quality of care [20, 23].
Discussion
Based on this review, there does not seem to be established best practices for engaging primary care, but common barriers are seen throughout the studies. Different combinations of strategies to overcome these barriers were implemented, though there was not one specific intervention that determined whether engagement efforts would succeed. Instead, targeted engagement efforts unique to the context and focused on mitigating commonly seen barriers seemed to provide the most benefit.
The engagement strategies described in the twelve studies, both successful and unsuccessful, provided the following lessons to consider when engaging primary care physicians.
Focus efforts on relationship building
A lack of trust between primary care and decision-makers, and the difficult relationships that resulted, was the most cited barrier to engaging primary care. Successful decision-makers prioritized establishing trust and repairing strained relationships as needed. Many differing tactics were used, but the most effective were those tailored to the specific group of local primary care physicians. Generic strategies like townhalls and newsletters improved communication and transparency, but true relationship building required significant time and intentional efforts. Targeted strategies, however, can be resource intensive and unfeasible in many circumstances, particularly with a provincial or national scope of change.
Clear communication was crucial in building strong, meaningful relationships. Intentional language that emphasized joint efforts and improving meaningful patient, provider, and health system outcomes is important when engaging primary care physicians.
Collaborate with primary care physician champions and primary care physician groups
Primary care physician champions were effective in building on pre-existing relationships to engage their local primary care community. They served local physicians as a direct line to decision-makers while simultaneously facilitating communication of initiative details to physicians for decision-makers.
Primary care physician groups composed of trusted local primary care leaders were able to speak as a collective and credible physician voice that engaged more physicians and had more impact in adjusting proposed initiatives. These groups were often able to unite local physicians, although opinions did not always align with those of administration. However, connecting with these groups was more streamlined for administrator engagement efforts.
Although physician champions and primary care physician groups cannot always engage with some dissenting physicians, both represent a credible, trusted physician voice and can be crucial partners to engage early when implementing health system change.
Ensure change Ideas are clinically relevant and feasible
Initiatives that were not clinically relevant quickly lost the support and engagement of primary care physicians. Low physician capacity and poor supports also hindered the uptake of change initiatives. Complicated initiatives also faced difficulty in achieving buy in compared to more straightforward solutions. Changemakers who focus on creating clinically relevant initiatives that improved primary care physician workload will be more successful in engaging physicians.
Consider use of financial incentives
Financial incentives have not been extensively studied in how they impact primary care engagement. A few studies extrapolated research that financial incentives do not improve quality of care and expressed financial incentives do not improve engagement. One study used financial incentives by paying physicians for time spent attending meetings and participation in program development [19]. The incentives were described to be effective at achieving engagement in a single study, but further investigation into the effectiveness and sustainability of this strategy is needed.
Limitations
Limitations in this scoping review include the timing of the review and the sources of research. The literature search was performed March 2020 and thus any subsequent publications discussing primary care engagement in system level change, specifically around primary care engagement in response to the COVID-19 pandemic, would not have been included in this scoping review. Grey literature reports were not included in the analyses and may not have identified themes exclusively described outside academic literature. Although a backward citation analysis was performed, a forward citation analysis was not and may have identified additional articles that met study criteria. Data extraction of 7 articles was performed by one reviewer and results were reviewed by the second rather independently assessed.
Conclusion
A scoping review was performed to identify common barriers and effective strategies to consider when engaging primary care physicians in designing and implementing health system change. Twelve articles were identified through a literature search and backward citation analysis. Commonly identified barriers included poor trust and relationships, strong professional physician identity, clinically irrelevant and complex initiatives, and a lack of capacity and supports. Some of these were addressed by commonly used strategies including efforts focused on relationship building, collaborating with primary care physician champions and primary care physician groups, and ensuring initiatives are clinically relevant and straightforward to implement. Although there are no published best practices available for engaging primary care, focused efforts that work to mitigate common barriers should see better engagement results.
Current work is underway by JBB exploring the role primary care leaders in health system change and how to define and measure the meaningful involvement of primary care [25]. Further research is required to better understand how to best build trust and develop relationships with primary care physicians and primary care groups. Additionally, the use of financial incentives was suggested as a strategy by one study, but further research is required to understand the impacts of providing financial incentives in initiating and maintaining engagement.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- MST:
-
Michael Sergio Taglione (author)
- JBB:
-
Judith Belle Brown (author)
References
Sikka R, Morath JM, Leape L. The quadruple aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24(10):608–10.
Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Family Med. 2014;12(6):573–6.
Shi L. The impact of primary care: a focused review. Scientifica. 2012;2012:432892.
Starfield B. Is primary care essential? The Lancet. 1994;344(8930):1129–33.
World Health Organization. Primary health care. 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/primary-health-care. Accessed 8 Dec 2020.
Hostetter J, Schwarz N, Klug M, Wynne J, Basson MD. Primary care visits increase utilization of evidence-based preventative health measures. BMC Fam Pract. 2020;21(1):1–0.
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502.
Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med. 2019;179(4):506–14.
Canadian Academy of Health Sciences. Making an Impact: A Preferred Framework and Indicators to Measure Returns on Investment in Health Research. 2009. Available from: https://cahs-acss.ca/wp-content/uploads/2011/09/ROI_FullReport.pdf. Accessed 7 Apr 2023.
Canadian Institutes of Health Research. A guide to knowledge synthesis. 2010. Available from: https://cihr-irsc.gc.ca/e/41382.html. Accessed December 1, 2020.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):1–9.
Snadden D, Reay T, Hanlon N, MacLeod M. Engaging primary care physicians in system change–an interpretive qualitative study in a remote and rural health region in Northern British Columbia, Canada. BMJ Open. 2019;9(5):e028395.
Hanlon N, Reay T, Snadden D, MacLeod M. Creating partnerships to achieve health care reform: moving beyond a politics of scale? Int J Health Serv. 2019;49(1):51–67.
Pratt R, Gyllstrom B, Gearin K, Lange C, Hahn D, Baldwin LM, VanRaemdonck L, Nease D, Zahner S. Identifying barriers to collaboration between primary care and public health: experiences at the local level. Public Health Rep. 2018;133(3):311–7.
Abou Elnour A, Dunbar J, Ford D, Dawda P. General practices’ perspectives on Medicare locals’ performance are critical lessons for the success of Primary Health Networks. Australasian Med J. 2015;8(10):320.
Kreindler SA, Struthers A, Metge CJ, Charette C, Harlos K, Beaudin P, Bapuji SB, Botting I, Francois J. Pushing for partnership: physician engagement and resistance in primary care renewal. J Health Organ Manag. 2019;33(2):126–40.
McDermott I, Checkland K, Moran V, Warwick-Giles L. Achieving integrated care through commissioning of primary care services in the English NHS: a qualitative analysis. BMJ Open. 2019;9(4): e027622.
Reay T, Goodrick E, Waldorff SB, Casebeer A. Getting leopards to change their spots: co-creating a new professional role identity. Acad Manag J. 2017;60(3):1043–70.
Pariser P, Pus L, Stanaitis I, Abrams H, Ivers N, Baker GR, Lockhart E, Hawker G. Improving system integration: the art and science of engaging small community practices in health system innovation. Int J Family Med. 2016;2016:5926303.
Kreindler SA, Metge C, Struthers A, Harlos K, Charette C, Bapuji S, Beaudin P, Botting I, Katz A, Zinnick S. Primary care reform in Manitoba, Canada, 2011–15: balancing accountability and acceptability. Health Policy. 2019;123(6):532–7.
Ashman I, Willcocks S. Engaging with clinical commissioning: the attitudes of general practitioners in East Lancashire. Qual Prim Care. 2014;22(2):91–9.
Skillman M, Cross-Barnet C, Singer RF, Ruiz S, Rotondo C, Ahn R, Snyder LP, Colligan EM, Giuriceo K, Moiduddin A. Physician engagement strategies in care coordination: findings from the centers for Medicare & Medicaid Services’ health care innovation awards program. Health Serv Res. 2017;52(1):291–312.
Kreindler SA, Larson BK, Wu FM, Gbemudu JN, Carluzzo KL, Struthers A, Van Citters AD, Shortell SM, Nelson EC, Fisher ES. The rules of engagement: physician engagement strategies in intergroup contexts. J Health Organ Manag. 2014;28(1):41–61.
Thorpe C, Brown JB, Terry A, Ryan B, Clark R, Hameed S. The Evolution of Family Physician Leadership in Health System Change. Conference presentation presented at: 50th North American Primary Care Research Group Annual Meeting. 2022 Nov 19.
Acknowledgements
Not applicable.
Funding
No specific funding sources were received for the completion of this research.
Author information
Authors and Affiliations
Contributions
MST and JBB developed the study design. MST created and performed the literature search. MST and JBB were involved in the scoping review as per the methodology section. MST performed the thematic analysis in consultation with JBB. MST and JBB wrote the manuscript and approved it for journal submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Literature search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Taglione, M.S., Brown, J.B. Primary care engagement in health system change: a scoping review of common barriers and effective strategies. BMC Prim. Care 24, 157 (2023). https://doi.org/10.1186/s12875-023-02117-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-023-02117-2