Abstract
Background
There is wide variation in clinical practice for the early detection of prostate cancer, not least because of the ongoing debate about the benefits of prostate-specific antigen (PSA) testing. In this study, we aimed to assess the approaches, attitudes, and knowledge of general practitioners (GPs) regarding PSA testing in primary care in the Netherlands, particularly regarding recommendations for prostate cancer.
Methods
Questionnaire surveys were sent to 179 GPs in the north-east of the Netherlands, of which 65 (36%) were completed and returned. We also surveyed 23 GPs attending a postgraduate train-the-trainer day (100%). In addition to demographic data and practice characteristics, the 31-item questionnaire covered the attitudes, clinical practice, adherence to PSA screening recommendations, and knowledge concerning the recommendations for prostate cancer early detection. Statistical analysis was limited to the descriptive level.
Results
Most GPs (95%; n = 82) stated that they had at least read the Dutch GP guideline, but just half (50%; n = 43) also stated that they knew the content. Almost half (46%; n = 39) stated they would offer detailed counseling before ordering a PSA test to an asymptomatic man requesting a test. Overall, prostate cancer screening was reported to be of minor importance compared to other types of cancer screening.
Conclusions
Clinical PSA testing in primary care in this region of the Netherlands seems generally to be consistent with the relevant guideline for Dutch GPs that is restrictive to PSA testing. The next step will be to further evaluate the effects of the several PSA testing strategies.
Similar content being viewed by others
Background
Prostate cancer is the second most frequent cancer and the fifth leading cause of cancer death in men worldwide [1, 2]. This estimated that there would be about 1.3 million new prostate cancer cases and 359,000 related deaths worldwide in 2018 [1, 2]. However, although the incidence of prostate cancer rose rapidly in most countries due to an increase in screening for prostate cancer by prostate-specific antigen (PSA) testing in the 1990s, it has been decreasing in the Netherlands over recent years [3,4,5]. In contrast, the country-specific standardized PCa mortality showed a steady decrease from 35.1 per 100,000 in 1995 to 22.2 per 100,000 in 2016 [4].
Prostate cancer screening based on PSA testing has been a matter of debate for many years, mainly because large clinical trials examining its effects on mortality have shown inconsistent results [6,7,8,9,10,11,12,13]. Indeed, a recent systematic review concluded that, at best, prostate cancer screening leads to a small reduction in disease-specific mortality over 10 years, but that it has no effect on overall mortality [14]. This is compounded by the reality that PSA screening is not without adverse consequences, such as overdiagnosis and overtreatment, with the potential for avoidable physical harm, anxiety, and costs [14,15,16,17]. Therefore, the net benefit of prostate cancer screening remains unclear, resulting in ambiguity that is reflected by different PSA testing recommendations for physicians [18,19,20]. Coupled with the absence of a formal screening program, this leads to uncertainty about testing for men who may otherwise be eligible for screening. Men considering screening may then receive inconsistent advice from their physicians.
In health systems predicated on evidence-based care, the attitudes and daily practice of physicians are expected to follow clinical guidelines based on the most relevant clinical trial results. Physicians should then individualize decisions according to these, also considering patient values, settings, comorbidities, general health, and other relevant characteristics. In terms of PSA testing, it has been shown that the personal beliefs and the specialization of the physician may also be relevant to the usage of PSA testing [21,22,23]. Variability in practice for PSA testing is not unusual among general practitioners (GPs), including those in the Netherlands. This is despite the fact that the Dutch College of General Practitioners (Nederlands Huisartsen Genootschap [NHG]) produced a practice guideline for Lower Urinary Tract Symptoms in Men in 2013 (henceforth, the NHG guideline) that includes a PCa screening approach due to the fact that patients frequently (wrongly) connect these two [20]. In 2014, the PSA threshold in this guideline was lowered from 4 ng/mL to 3 ng/mL to be consistent with the national guideline on prostate cancer issued by the Dutch Urological Association (Nederlandse Vereniging voor Urologie) [19, 24]. The guideline recommends against active offering of PSA testing to men without clinical symptoms of PCa and is actually (in 2020) under revision. Apart from being free available on the internet, the guideline is, among others, published in a Dutch scientific journal for GPs, and is part of trainings and education for GPs.
In the present study, we aimed to survey GPs in the Netherlands to assess their approaches, attitudes, and knowledge regarding the use of PSA screening for early prostate cancer detection, focusing on the prostate cancer recommendations set out in the NHG guideline.
Methods
Study design, setting, and participants
This cross-sectional pilot survey was performed in April and May 2016 by asking GPs in the north-east of the Netherlands to complete paper-based questionnaire. We used conventional mail to contact all GPs affiliated to the University Medical Center Groningen. In addition, the questionnaire was distributed at a training day that took place at the University Medical Center Groningen during the study period and was attended by 23 GP trainers (educational supervisors of GPs in training).
Questionnaire development and data collection
As the questionnaire in this project was conducted in the context of a binational project, a German version of the questionnaire was translated into Dutch. Formal back and forwards translations were performed by native speakers of both German and Dutch [22]. After translation, the questionnaire was adapted to the Dutch prostate cancer guidelines and the Dutch health care system. Adaptations included for example the inclusion of digital rectal examination (DRE) results in case scenarios and questions on usage of DRE. We used the NHG guideline for reference because we expected that most GPs in the Netherlands would report using this guideline. Additional File 1 shows the Dutch questionnaire, Additional File 2 the English translation of this questionnaire.
The final iteration comprised 31 questions in five sections, addressing issues such as how and when to initiate PSA screening, the implications of results, awareness of the recommendations from national guidelines, and awareness of the results of relevant studies concerning PSA screening. Variations in daily practice of PSA testing were explored by presenting standardized case scenarios (unrelated to those listed in Section 2.3). In addition, some demographic and organizational data were collected about the participants and their practices.
Questions requiring graded responses were mostly answered on five-point Likert scales. To test the questionnaire on acceptance, comprehensibility, ease of use, feasibility and validity, pretests were conducted among urologists and GPs for both versions of the questionnaire. The Dutch version was regarded by a three Dutch GPs and a Dutch urologist. Based on this, the questionnaire was revised, according to the comments of the physicians. Questionnaires were completed once.
The NHG guideline
The 2013 NHG guideline on Lower Urinary Tract Symptoms in Men provides strategies for early prostate cancer detection without advocating general PSA screening for prostate cancer [20]. Instead, guidance for PSA testing is given in two scenarios, and even then, depends on clinical assessments: [1] when an asymptomatic patient makes a request; and [2] when there is clinical suspicion.
Patient request (scenario 1): an asymptomatic patient requests testing
When faced with a patient request, GPs are advised to provide balanced and detailed information on the risks and benefits of screening to help the patient make an informed decision. Physicians are required to provide the following details related to prostate cancer: the risk in older men (incidence), the rarity of symptoms, and the risk of death. If the patient decides to undergo early detection, a DRE should be performed first, and a suspicious outcome should trigger direct referral to a urologist. In this scenario, a PSA test should only be ordered if the DRE is normal.
Suspected prostate cancer (scenario 2): the presence of suggestive symptoms or signs
When cancer is suspected based on an abnormal DRE and when patients have a life expectancy of more than 10 years they should be referred directly to a urologist without performing a PSA test. However, for those with a life expectancy of less than 10 years, the policy varies based on the suspicion of metastases. For example, a DRE should be performed when metastases are suspected, with a suspicious result triggering referral to a urologist and a normal result triggering PSA testing. The PSA test results then dictate the direction of any subsequent referral: a patient is referred to a urologist if the PSA level is ≥4 ng/mL and is referred to an oncologist if the PSA is < 4 ng/mL.
Statistical analysis
Response proportions were calculated separately for the GPs and the GP trainers. Participant characteristics and survey responses were analyzed descriptively by absolute and relative frequencies for categorical variables. Because of the exploratory nature of the survey and the low numbers of participants within subgroups, formal statistical tests were not applied. Data analysis was done using IBM SPSS Version 25 (IBM Corp., Armonk, NY, USA).
Ethics and data security
The German part of the study was approved by the Medical Ethics Committee of the Carl von Ossietzky University Oldenburg (No. 041/2016), which was in line with local law. For the Dutch part, no ethical approval was required, as participants were healthy volunteers and no patients, it was a one-time questionnaire, and the questions were not intrusive. Before answering the questionnaire, the participants were informed that their privacy would be respected. Data were anonymized before data handling.
Results
Response proportion and responder characteristics
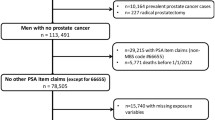
Of the 179 postal questionnaires 65 (36%) were completed and returned. By contrast, all 23 GPs at the training day completed the questionnaires (100%). Additional File 3 shows the participation flowchart.
The characteristics of the participants and their practices are shown in Table 1. The median age of all GPs was 54 years, 25 (29%) were female, 77 (89%) had more than 10 years’ experience as a GP, and 16 (18%) worked in a practice on their own. Although almost a third (32%; n = 28) reported having had at least some work experience in urology during or after medical school, this was less than 1 month for most (82%; n = 23). More than half of the GPs (59%; n = 51) had attended a postgraduate training course on the usage of PSA testing.
Familiarity with the NHG recommendations on prostate cancer in the LUTS guideline
Apart from 1 GP (1%), all 86 GPs had at least heard of the NHG guideline [20]. Only 3 GPs (4%) had never read or used the guideline, and of the remaining 82 (95%), half had read it and could recall the content (50%, n = 43). Those who reported having read the NHG guideline stated that they sought to use the recommendations in daily practice.
Approaches and attitudes of GPs to PSA screening
GPs reported that they usually addressed the impact of PSA screening (testing in asymptomatic men) by looking at the disease-specific mortality when discussing PSA screening (Table 2). It was reported that adverse effects, such as overdiagnosis or the potential for false-positive results, were also discussed often, but that the chance of detecting prostate cancer before metastasis was rarely mentioned.
In general, the surveyed GPs were critical of PSA screening (Table 3). Almost none would recommend testing to relatives and most of the male GPs (71%; n = 44) had not undergone PSA testing themselves and did not plan to do so in the future. More than 40% of the GPs (43%; n = 37) were not worried about missing a diagnosis of prostate cancer in patients, and in most cases, considered screening for other cancers to be more important.
Approaches of GPs in specific case scenarios
Table 4 shows the results of the approaches of GPs when presented with different scenarios. For symptomatic patients, GPs tended to order PSA tests rarely for lower urinary tract symptoms compared with sometimes for other unclear discomfort. Over three-quarters of the GPs (76%; n = 67) always or often perform a DRE before requesting a PSA test. The most common indication for PSA testing was a DRE suggestive of prostate cancer (67%; n = 59).
Almost all GPs (94%; n = 80) reported that there were circumstances in which they would not refer a patient with an increased PSA level to a urologist. Examples included advanced age, short life expectancy, or a plausible diagnosis of prostatitis. Some GPs used specific PSA thresholds to determine whether to refer asymptomatic patients, citing levels of 4, 5, 7, and 10 ng/mL. In patients with a normal PSA level, most GPs preferred not to retest (80%; n = 67).
In asymptomatic patients actively requesting PSA testing, 39 GPs (46%) said that they would agree to the request within the same session after providing information on the benefits and risks of the test. Less commonly, GPs reported they would first discuss the test but would require a separate appointment before deciding whether to perform the test (35%; n = 30).
Discussion
We have presented the results of a survey conducted in the north-east of the Netherlands to assess the approaches, attitudes, and knowledge of GPs concerning the application of PSA screening for the early detection of prostate cancer. Most GPs stated that they used the NHG recommendations in daily practice when applying PSA testing in primary care: Before performing a PSA test, most stated that they discussed relevant topics with their patients, covering the many advantages and disadvantages.
Other studies on approaches to PSA testing have shown varying results. Research in the Netherlands concerning the PSA testing policy among GPs and non-urological medical specialists has revealed comparable approaches to those in the present study when faced with a patient requesting a PSA test [25]. However, before ordering a PSA test, GPs in that study performed DRE less frequently than in ours, which is consistent with the results of a survey among 303 physicians in South Africa [26]. GPs in Northern Ireland have also been shown to have similar DRE practices to those found in our study, but GPs in that study were less reserved about PSA testing (e.g., in patients with urinary tract symptoms) [27]. This finding was notable because most GPs in our survey were male, and research has indicated that male GPs are more likely to order a PSA test than female GPs [28, 29].
Another study identified considerable differences in the approaches to PSA testing between GPs in Australia and the United Kingdom (UK). Decisions about screening and PSA testing made by GPs in Australia were mostly at the discretion of individual clinicians, resulting in significant variations in practice. However, the replies of GPs in the UK reflected a clear, consistent, organizationally embedded approach based on evidenced recommendations to discourage screening [30]. The approaches reported by GPs in our survey were comparable to those reported by GPs in the UK. We agree that this suggests that health care systems, organizational structures, and guidelines collectively affect how physician’s view and handle PSA testing for early cancer detection, which is also supported by others [30]. Differences between these factors can also play a role when comparing PSA and DRE practices between countries and must therefore also be considered.
Concerning guideline adherence, a study among 55 physicians in Switzerland found that physicians generally had favorable attitudes toward clinical guidelines, but that only one-third used them very often or often [31]. Although most GPs in our study reported using the NHG guideline in daily practice, only a few followed the advice to refer a patient to a urologist without performing a PSA test if the DRE raised suspicion. After the main outcomes of the European Randomized Study of Screening for Prostate Cancer were published, the level of follow-up testing among Dutch GPs decreased after an increased PSA result [32]. The reason for this remains unclear, as do the reports by some of our respondents that they adopt their own (unsuitable) criteria and PSA cut-off values for when not to refer a patient to a urologist. In Lower Saxony, Germany, evidence has also been published showing that GPs and urologists did not treat patients in accordance with established guidelines on prostate cancer [22]. A systematic review looking at the state of PSA testing policies worldwide revealed significant variation in follow-up policies after a normal or raised PSA level, and that this is often discordant with the available practice guidelines [33]. The conflicting advice in current guidelines on prostate cancer could lead to the variations seen in daily practice [34].
There are several limitations to our survey, primarily related to the small sample and the restricted catchment area of a single university hospital, which may not have been representative of the national population. This was aggravated by the low response proportion in general and the difference in response among GPs contacted by mail compared with those surveyed at the training day. Although other postal surveys among GPs show comparable or even lower response proportions, this could be improved by relying on on-site surveys [35, 36]. The pooling of the data for the two groups is an important limitation because the conditions among those groups were different; however, we considered that the number of GPs was too small to stratify the results further. That said, we acknowledge that being a GP trainer is likely to influence opinions and knowledge on PSA testing, and that 60% of the surveyed GPs had participated in a postgraduate course on PSA testing, skewing the results to overestimate the levels of guideline adherence and knowledge. Of course, this assumes that the surveyed GP trainers involved in education and/or research are more compliant and knowledgeable than non-responders. Another factor possibly leading to an overestimation of the results may be that all answers are self-reported. However, in the Netherlands most GPs are aware of the existence and content of the Dutch GP guidelines [37]. Finally, the questionnaire was developed in German and translated to Dutch. Although we took care to ensure comparability between the two versions, we cannot exclude the possibility that the questionnaire lacks validity and reliability in the Dutch health system.
Conclusion
Routine clinical practice regarding PSA testing in primary care seems generally to be consistent with the NHG guideline that is restrictive to PSA testing. We propose that future research should further evaluate the effects of the several PSA testing strategies.
Availability of data and materials
Data and materials supporting the conclusion were included in the main paper. Further data were available from the corresponding author on reasonable request.
Abbreviations
- DRE:
-
Digital rectal examination
- GP:
-
General practitioner
- NHG:
-
Dutch College of General Practitioners (Nederlands Huisartsen Genootschap)
- PSA:
-
Prostate-specific antigen
- UK:
-
United Kingdom
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108.
Hsing AW, Tsao L, Devesa SS. International trends and patterns of prostate cancer incidence and mortality. Int J Cancer. 2000;85(1):60–7.
Integraal Kankercentrum Nederland. Dutch cancer figures 2017 [Available from: https://www.cijfersoverkanker.nl/selecties/dataset_1/img5b9622d157dca.
Larrañaga N, Galceran J, Ardanaz E, Franch P, Navarro C, Sánchez MJ, et al. Prostate cancer incidence trends in Spain before and during the prostate-specific antigen era: impact on mortality. Ann Oncol. 2010;21(suppl 3):iii83–i9.
Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360(13):1320–8.
Eckersberger E, Finkelstein J, Sadri H, Margreiter M, Taneja SS, Lepor H, et al. Screening for prostate cancer: a review of the ERSPC and PLCO trials. Rev Urol. 2009;11(3):127.
Andriole GL, Crawford ED, Grubb RL III, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360(13):1310–9.
Andriole GL, Crawford ED, Grubb RL, Buys SS, Chia D, Church TR, et al. Prostate cancer screening in the randomized prostate, lung, colorectal, and ovarian Cancer screening trial: mortality results after 13 years of follow-up. J Natl Cancer Inst. 2012;104(2):125–32.
de Koning HJ, Gulati R, Moss SM, Hugosson J, Pinsky PF, Berg CD, et al. The efficacy of prostate-specific antigen screening: impact of key components in the ERSPC and PLCO trials. Cancer. 2018;124(6):1197–206.
Lakes J, CJDU A. PSA-Screening und molekulare Marker. Urologe A. 2019;58(5):486–93.
Bray F, Lortet-Tieulent J, Ferlay J, Forman D, Auvinen A. Prostate cancer incidence and mortality trends in 37 European countries: an overview. Eur J Cancer. 2010;46(17):3040–52.
Schroder FH, Hugosson J, Roobol MJ, Tammela TLJ, Ciatto S, Nelen V, et al. Prostate-Cancer mortality at 11 years of follow-up. N Engl J Med. 2012;366(11):981–90.
Ilic D, Djulbegovic M, Jung JH, Hwang EC, Zhou Q, Cleves A, et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ. 2018;362:k3519.
Ilic D, Neuberger MM, Djulbegovic M, Dahm P. Screening for prostate cancer. Cochrane Database Syst Rev. 2013;(1):Cd004720.
Thompson IM, Ankerst DP, Chi C, Lucia MS, Goodman PJ, Crowley JJ, et al. Operating characteristics of prostate-specific antigen in men with an initial PSA level of 3.0 ng/ml or lower. Jama. 2005;294(1):66–70.
Hjertholm P, Fenger-Grøn M, Vestergaard M, Christensen MB, Borre M, Møller H, et al. Variation in general practice prostate-specific antigen testing and prostate cancer outcomes: an ecological study. Int J Cancer. 2015;136(2):435–42.
Mottet N, Bellmunt J, Briers E, Bolla M, Bourke L, Cornford P, et al. EAU – ESTRO – ESUR – SIOG Guidelines on Prostate Cancer; 2018.
Prostaatcarcinoom. Landelijke richtlijn, Versie: 2.1.: Nederlandse Vereniging voor Urologie; 2016. Available from: https://richtlijnendatabase.nl/richtlijn/prostaatcarcinoom/algemeen.html.
Blanker MH, Klomp MAR, van den Donk M, van der Heide WK, Opstelten W, Burgers JS. Summary of the NHG practice guideline ‘Lower urinary tract symptoms in men’. Ned Tijdschr Geneeskd. 2013;157(18):A6178.
Drummond FJ, Carsin A-E, Sharp L, Comber H. Factors prompting PSA-testing of asymptomatic men in a country with no guidelines: a national survey of general practitioners. BMC Fam Pract. 2009;10(1):1–12.
Kappen S, Jurgens V, Freitag MH, Winter A. Early detection of prostate cancer using prostate-specific antigen testing: an empirical evaluation among general practitioners and urologists. Cancer Manag Res. 2019;11:3079–97.
Ross LE, Hall IJ, Howard DL, Rim SH, Richardson LC. Primary care physicians beliefs about prostate-specific antigen evidence uncertainty, screening efficacy, and test use. J Natl Med Assoc. 2018;110(5):491–500.
Blanker MH, de Reijke TM, van Moorselaar RJ, Opstelten W. Changes to Dutch College of General Practitioners guideline ‘Micturition problems in men’. Ned Tijdschr Geneeskd. 2014;158:A8070.
van der Meer S. Prostate-specific antigen testing policy. Non-urologists and guideline adherence. Groningen: University of Groningen; 2015.
Spencer K. A finger or not? Prostate examinations by non-urologists at a South African academic institution. South Afr Med J. 2017;107(7):631–5.
Little B, Ho KJ, Gormley G, Young M. PSA testing in general practice. Prostate Cancer Prostatic Dis. 2003;6(2):154–8.
Gormley GJ, Catney D, McCall JR, Reilly PM, Gavin AT. Prostate-specific antigen testing: uncovering primary care influences. BJU Int. 2006;98(5):996–1000.
Engler J, Dahlhaus A, Guthlin C. The readiness of German GPs to recommend and conduct cancer screening is associated with patient-physician gender concordance. Results of a survey. Eur J Gen Pract. 2017;23(1):11–9.
Pickles K, Carter SM, Rychetnik L, Entwistle VA. Doctors' perspectives on PSA testing illuminate established differences in prostate cancer screening rates between Australia and the UK: a qualitative study. BMJ Open. 2016;6(12):e011932.
Birrenbach T, Kraehenmann S, Perrig M, Berendonk C, Huwendiek S. Physicians’ attitudes toward, use of, and perceived barriers to clinical guidelines: a survey among Swiss physicians. Adv Med Educ Pract. 2016;7:673–80.
Van der Meer S, Kollen BJ, Hirdes WH, Steffens MG, Hoekstra-Weebers JE, Nijman RM, et al. Impact of the European randomized study of screening for prostate Cancer (ERSPC) on prostate-specific antigen (PSA) testing by Dutch general practitioners. BJU Int. 2013;112(1):26–31.
van der Meer S, Lowik SA, Hirdes WH, Nijman RM, van der Meer K, Hoekstra-Weebers JE, et al. Prostate specific antigen testing policy worldwide varies greatly and seems not to be in accordance with guidelines: a systematic review. BMC Fam Pract. 2012;13:100.
Ranasinghe WK, Kim SP, Papa NP, Sengupta S, Frydenberg M, Bolton D, et al. Prostate cancer screening in primary health care: the current state of affairs. SpringerPlus. 2015;4:78.
Martini F, Lazzati A, Fritsch S, Liagre A, Iannelli A, Paolino L. General practitioners and bariatric surgery in France: are they ready to face the challenge? Obes Surg. 2018;28(6):1754–9.
Giezendanner S, Monsch AU, Kressig RW, Mueller Y, Streit S, Essig S, et al. General practitioners’ attitudes towards early diagnosis of dementia: a cross-sectional survey. BMC Fam Pract. 2019;20(1):65.
Grol R. De verspreiding van NHG-standaarden onder huisartsen. Huisarts Wet. 1989;32(13):494–7.
Acknowledgments
We would like to thank all GPs taking the time to participate in this survey. Further, we would like to express our thanks to the Department of General Practice and Elderly Care Medicine of the University Medical Center Groningen for supporting the study. Finally, we thank Erika Timmer and Susanne Doerner for translating the questionnaire and Dr. Robert Sykes (www.doctored.org.uk) for providing editorial services.
Funding
The German part of this study was funded by the research pool of the Carl von Ossietzky University Oldenburg. For the Dutch part, no funding was available. The funding body had no influence on the study design, the collection, analysis, and interpretation of data, and in writing the manuscript. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
GHB, AT, and VJ were responsible for the study design. SK, LK, and VJ did the literature search. All authors helped developing the original German questionnaire and the questionnaire used in this study. LK, MHB, and GHB were responsible for conducting the questionnaire. SK, LK, and VJ performed the descriptive analysis and the data management. SK, LK, VJ, MHB, and GHB and interpreted the data. SK, VJ, and GHB drafted the manuscript, while all other authors revised it. All authors have read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The German part of the study was approved by the Medical Ethics Committee of the Carl von Ossietzky University Oldenburg (No. 041/2016), which was in line with local law. For the Dutch part, no ethical approval was required, as participants were healthy volunteers and no patients, it was a one-time questionnaire, and the questions were not intrusive. Before answering the questionnaire, the participants were informed that their privacy would be respected. Data were anonymized before data handling.
Consent for publication
Not applicable.
Competing interests
MHF receives personal fees from DAK Gesundheit, unrelated to the submitted work. The authors report no other conflicts of interest in this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Dutch questionnaire. This questionnaire was conducted among the participants of this Dutch part of the study.
Additional file 2.
English questionnaire. English translation of the questionnaire that was conducted among the participants of this Dutch part of the study.
Additional file 3.
Participation flowchart. GP = general practitioner. Flowchart of the invited, participated and analyzed participants of this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kappen, S., Koops, L., Jürgens, V. et al. General practitioners’ approaches to prostate-specific antigen testing in the north-east of the Netherlands. BMC Fam Pract 21, 270 (2020). https://doi.org/10.1186/s12875-020-01350-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-020-01350-3