Abstract
Background
Although outcome goals for acute healthcare among older people living with frailty often include Health-Related Quality of Life (HRQoL) and other patient-reported outcome measures (PROMs), current quality metrics usually focus on waiting times and survival. Lay and patient review have identified the EuroQol EQ-5D as a candidate measure for this setting. This research appraised the EQ-5D for feasibility, psychometric performance, and respondents’ outcomes in the acute frailty setting.
Methods
People aged 65 + with Clinical Frailty Scale (CFS) 5–8 were recruited from eight UK hospitals’ emergency care and acute admissions settings. They completed the five-level EQ-5D and the EQ-VAS. Feasibility was assessed with completion times and completeness. For reliability, response distributions and internal consistency were analysed. Finally, EQ-Index values were compared with demographic characteristics and service outcomes for construct validity.
Results
The 232 participants were aged 65–102. 38% responded in emergency departments and 62% in admissions wards. Median completion time was 12 (IQR, 11) minutes. 98% responses were complete. EQ-5D had acceptable response distribution (SD 1.1–1.3) and internal consistency (Cronbach’s alpha 0.69). EQ-VAS demonstrated a midpoint response pattern. Median EQ-Index was 0.574 (IQR, 0.410) and was related positively with increasing age (p = 0.010) and negatively with CFS (p < 0.001). Participants with higher CFS had more frequent problems with mobility, self-care, and usual activities.
Conclusions
Administration of the EQ-5D was feasible in these emergency and acute frailty care settings. EQ-5D had acceptable properties, while EQ-VAS appeared problematic. Participants with more severe frailty had also poorer HRQoL.
Similar content being viewed by others
Introduction
Acute care encompasses emergency departments, urgent care, and acute admissions ward settings. Traditionally this operationalises ‘single-problem’ rapid-flowing pathways and is increasingly recognised to have limitations in serving older people living with frailty, who have multiple problems and require a more holistic approach [1]. Geriatric emergency medicine is emerging as a multidisciplinary subspecialty with its basis in person-centred care, wherein interventions are selected and tailored for individuals’ situations and perspectives [2,3,4]. Health-Related Quality of Life (HRQoL) is often the primary outcome goal of acute care episodes for older people living with frailty [5, 6]. This population group have poorer outcomes from acute care, but these have typically been qualified with system metrics including survival times, waiting times, and readmission rates rather than with HRQoL measures [7, 8].
Incorporating HRQoL measurement into healthcare metrics could facilitate more meaningful evaluation of outcomes for older people living with frailty. This could be achieved using Patient-Reported Outcome Measures [9]. Systematic reviews of PROMs have reported lower quality of life among people living with frailty in community settings [10, 11]. However, there is little knowledge regarding their HRQoL in the acute care setting, explained in part by the lack of any validated PROM for unwell older people living with frailty [9, 12]. A comprehensive PROM (or a combination) for this population would consider themes of autonomy and function [13]. In a systematic review and lay evaluation of potentially suitable PROMs for those themes of function, the EuroQol 5 Dimension (EQ-5D) presented an acceptable compromise between detail and brevity [14].
The EQ-5D has been administered in acute care research and audit programmes with specific groups of older people, notably those with trauma [15, 16]. Its feasibility has been demonstrated in community, outpatient, general medical, and focussed surgical settings [17]. However, it has yet to be evaluated for feasibility or psychometric properties during use by older people with frailty receiving acute healthcare – a setting uniquely epitomised by urgency and uncertainty.
EQ-5D invites respondents to rate the severity of problems experienced in the five dimensions mobility, self care, usual activities, pain / discomfort, and anxiety / depression [18]. People living with frailty are vulnerable to poor outcomes from health crises. Reduced independent function and heightened concern and discomfort would typically be expected among people receiving care following sudden change in situation due to acute illness or injury. These symptoms and their subsequent trajectory could be measured using the EQ-5D.
This evaluation of EQ-5D in emergency departments and acute admissions ward settings took place within a larger research programme aiming to improve understanding of the lived experience of older people receiving acute healthcare. This paper reports on objectives to (1) assess the feasibility of collecting EQ-5D from acutely unwell older people living with frailty, (2) assess the psychometric performance of the EQ-5D in this setting, and (3) describe HRQoL and its relationship with frailty in this population.
Methods
This was an analysis of PROM, demographic, and overview clinical service data. The study was nested within a programme developing a novel PROM for older people living with frailty receiving acute care (the PROM-OPAC), in which the EQ-5D was administered as a comparator instrument during two phases of administration.
Eligible participants were older people (aged 65 +) who were receiving care in hospital within seventy-two hours of unscheduled attendance. Precise locations included emergency departments, observation areas, and acute assessment wards. They were living with frailty, defined as having Clinical Frailty Scale (CFS) scores 5 (mild frailty) to 8 (very severe frailty) [19]. People with terminal illness who otherwise did not have severe frailty (CFS = 9) were not recruited. The recruiting sites routinely collected the CFS for people aged 65 + receiving acute care. Routine CFS measurements by nursing or medical staff were used by research practitioners to identify eligible individuals.
Participants were approached and recruited by research practitioners using convenience sampling. They provided written consent, given either themselves or by their consultee in the case of having capacity to complete the measure but not to consent to research. This included, for instance, people living with cognitive impairment who were able to express their perspectives and perceptions but who could not fully process or retain the research information or complete a consent form. The study protocol was reviewed and approved by an NHS Research Ethics Committee.
Data collection
Data were collected at eight UK hospitals. These were located in London and the South East (4), East Midlands (3), and the North West (1) of England. Participants’ age, CFS, gender, and ethnicity (using UK Office for National Statistics groups) were recorded. All participants completed PROMs using pen and paper, with or without the assistance of a scribe: the five-level EQ-5D-5L (which evaluates problems with mobility, self-care, usual activities, pain and discomfort, and anxiety and depression), and the EQ-VAS (a 1–100 scale of the user’s health that day). The administered instruments used English language. All responses were from participants and proxies were not used. Time to completion (from commencing instrument responses) was recorded.
The degree of assistance required by the first half of participants was rated by the research practitioner as none, minimal (demonstration only), moderate (reading aloud or scribing), or substantial (explaining options or prompting for responses). Meanwhile for the second half of participants, the single-item Self-Rated Health (SRH) was also collected, and clinical service data were recorded (presenting problem, location in hospital, time from attendance to participation, and destinational outcomes from the ED and after thirty days) [20].
Analyses
EQ-Index values (preference-weighted utilities for economic evaluation anchored at 1 (best health) and 0 (a state as bad as being dead)) were calculated from complete responses using a crosswalk value set [21]. Analyses were performed using R software with the packages eq5d, ggplot2, and psych [22].
Feasibility was first assessed. Times to completion were examined for normality, summarised, and compared with age and CFS using correlation and Kruskal–Wallis tests. Missing data were analysed for frequency and pattern.
Next, reliability was determined. EQ-5D data were analysed for response distributions (response level proportions and standard deviations) and internal consistency (question inter-relatedness using Cronbach’s alpha statistic) [23].
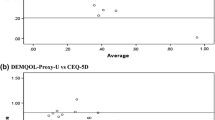
Finally, criterion and construct validity were examined. EQ-Index was assessed for convergence with EQ-VAS (all respondents) and SRH (second half of participants). EQ-Index was compared with age, CFS, gender, and ethnicity using correlation, Kruskal–Wallis, and chi-squared tests. The proportions of respondents with severe or extreme problems in each dimension were aggregated by CFS levels. EQ-Index and dimension-level proportions of severe problems for the second half of participants were tested for association with waiting time at participation, presenting problem (dichotomised as illness or injury), disposition destination from the ED, and clinical outcome after thirty days. Associations were hypothesised with lower ED EQ-Index and EQ-VAS for people with longer waits, injury presentations, subsequent hospital admissions, and subsequent reattendance or death within thirty days.
Results
Two hundred and thirty-two participants were recruited: 38% responded in emergency departments and 62% in acute admissions ward settings. Participants’ age ranged from 65 to 102 years, and they were living with mild to very severe frailty. More participants had mild to moderate (CFS 5, 31%, CFS 6, 50%)) than severe or very severe frailty (CFS 7, 18%; CFS 8, 1%). This approximated the expected distribution of CFS among older people receiving emergency care [24]. The sample recruited more females (62%), and nearly all participants reported white ethnicity (Table 1).
Feasibility
Median time for participants to complete the PROMs was 12 (IQR, 11) minutes. Completion time was weakly correlated positively with increasing age (Spearman rho = 0.15, p = 0.022) and was not associated with CFS (Kruskal–Wallis p = 0.358). There were minimal missing data, with 98% EQ-5D responses complete. The item ‘usual activities’ had the most frequent missing responses (1%). 102 of 128 (80%) first half participants used at least minimal assistance – 94 being supported with reading or scribing and 8 requiring explanations or prompts.
Psychometric properties
Ceiling effects were observed with the ‘self care’ and ‘anxiety / depression’ questions, respectively with 35% and 42% participants reporting no problems (Table 2). Response distribution remained satisfactory (standard deviation > 0.95) for all EQ-5D items. There was a midpoint response pattern with EQ-VAS, where 23% participants responded ‘50’. EQ-5D internal consistency was acceptable (α = 0.69).
EQ-Index converged with both the EQ-VAS (Spearman rho = 0.277, p < 0.001) and the SRH (Kruskal–Wallis p = 0.053).
Health-related quality of life
Relationships with participants’ characteristics
The median EQ-Index in this cohort was 0.574 (IQR, 0.410) and this was similar for participants recruited across the eight sites (chi-squared p = 0.170). 11 participants (5%) had EQ-Index lower than 0, corresponding to states worse than being dead. EQ-Index increased weakly with age (Spearman rho = 0.170, p = 0.010), and decreased with more severe frailty (Kruskal–Wallis p < 0.001). There was no association between EQ-Index and gender (chi-squared p = 0.244) and the recruited ethnicity distribution was insufficient for association testing.
With increasing CFS, participants more frequently reported severe or extreme problems with mobility (Kruskal–Wallis p = 0.010), self care (p < 0.001), and usual activities (p = 0.001). All participants living with very severe frailty (CFS 8) reported at least severe problems in these dimensions, although it should be noted that these were a very small proportion of the cohort. No association was apparent between frailty and having severe problems with pain and discomfort (p = 0.955) or anxiety and depression (p = 0.327) (Fig. 1).
Associations with clinical outcomes
Participants who participated at later points during the seventy-two hour acute care phase tended to have higher EQ-Index (Spearman rho = 0.229, p = 0.029). There was no significant difference in EQ-Index between respondents attending with illnesses or injuries (chi-squared p = 0.534). Similarly, responses did not significantly differ between groups admitted or discharged from the ED (chi-squared p = 0.334), or with different thirty-day clinical outcomes (chi-squared p = 0.240).
Discussion
This study adds to a limited evidence base considering HRQoL and its measurement in acutely unwell older people living with frailty. The objective was not to advocate for EQ-5D as a perfectly suited outcome measure for older people living with frailty; indeed, previous work has shown it to consider meaningful themes of function but not of autonomy [14]. However, collection of the EQ-5D from older people living with frailty receiving acute care appeared feasible. Measurements appeared reliable and the responses appeared valid against objective observation of frailty.
The high proportion of fully completed five-level EQ-5D responses observed here (98%) exceeded that (90%) reported in a recent systematic review of use by older people, where the three-level variant was most frequently administered [17]. All participants were accompanied by a research practitioner who offered assistance as a scribe. With 80% participants using this assistance, this intervention likely improved the rates of full completion and allowed people with common accessibility barriers to respond. Further work is required to evaluate completion rates among acute care respondents when support is not offered. The practical implications on representation and data quality of providing scribe support in routine PROMs programmes will also require consideration.
The adequate psychometric properties of response distribution and internal consistency for EQ-5D were consistent with previous reports in studies of older people living with frailty [25, 26]. However, the midpoint response pattern with EQ-VAS appears novel in this acute care application and is problematic. This may represent difficulty interpreting instructions or appreciating one’s health trajectory in the context of illness and uncertainty, or may indeed be an effect of feeling rushed by research practitioner presence.
Poorer mean (SD) EQ-Index values have been reported by people living with versus without frailty in the UK (0.71 (0.21) vs 0.92 (0.10)) and Vietnam (0.58 (0.20) vs 0.70 (0.18)) [27, 28]. The present sample of older people living with frailty and receiving acute care had still poorer EQ-Index (median 0.58), with 5% having negative values corresponding to situations worse than being dead. Having poorer HRQoL has been associated with increased mortality [29]. Similarly, the predictive performance for mortality of the Clinical Frailty Scale in ED has been widely reported [24, 30]. HRQoL and the CFS appear linked as objective and subjective manifestations of the frailty construct, wherein lived biographies are disrupted by functional deficits and uncertainty [31, 32]. While HRQoL has been observed to improve during geriatric ward admissions, further evaluation of person-reported outcomes from acute care is warranted [33, 34].
Limitations
This research recruited only those older people who were living with frailty. As such, the design did not allow direct HRQoL comparison with people who were younger or not living with frailty, and further evaluation is therefore required during and following acute illness. Furthermore, we did not study for the potential roles of educational attainment or socioeconomic deprivation. It is possible that these users of acute healthcare may have differed from the general population, with those having altered baseline physiology and function being more likely to experience crises. Baseline HRQoL may therefore also differ in people who subsequently require acute care, and this would require a large-scale cohort study to evaluate.
While people with impaired capacity were recruited with consultee consent, the study did not examine for the effect of cognitive impairment on response rate, completeness, or reported outcomes. This was a limitation of the study being conducted within a PROM development programme. While people living with cognitive impairment did participate, only individuals who could express their perspectives by responding or indicating responses to the items were recruited. The study design did not extend to scoring quantifying the severity of cognitive impairment, but we can assume that people with severe limitations were not represented here. Around one third of older people using the emergency department might be expected to have a dementia or delirium, and further work is required to determine accessibility and feasibility of PROMs participation with this cohort [35]. Other PROMs have used proxy completion to represent people living with dementia [36]. Acknowledging potential issues with precision, this approach may further widen the access to participation and is a topic for further study.
Calculation of EQ-Index used a value set produced from UK population-level data. These are not necessarily comparable to other populations. Furthermore, the precision of these values, which fall at the extreme-low end of the population range, should be considered cautiously in comparative studies. Validation and application of a value set focussed on an older population may be more meaningful.
All participants were recruited and accompanied by a research practitioner, which introduced potential selection and acquiescence biases. Research practitioners may have preferentially approached individuals who they thought would be better able to complete the instruments. People without fluent English, for instance, may have been excluded from participation and therefore further research using consecutive recruitment is indicated. While the administered PROMs did not directly invite participants to report on their healthcare experience, this design may still have prompted participants to report better outcomes in the presence of a professional.
Conclusions
Older people living with frailty were able to complete the EQ-5D and EQ-VAS while receiving acute care in emergency departments and admissions wards, with excellent data completeness. EQ-5D had adequate psychometric properties, while a midpoint response pattern was observed with EQ-VAS. This sample of older people living with frailty receiving acute healthcare had poor HRQoL, which was negatively associated with having increasingly severe frailty.
Availability of data and materials
The datasets generated and analysed during this study are not publicly available due to the ethics permissions received but are available from the corresponding author on reasonable request.
References
van Oppen J, Conroy S. Are Emergency Departments Responding to the Aging Demography? Ann Emerg Med. 2021;79(4):364–6.
Conroy S, Nickel CH, Jónsdóttir AB, Fernandez M, Banerjee J, Mooijaart S, et al. The development of a European curriculum in Geriatric Emergency Medicine. Eur Geriatr Med. 2016;7(4):315–21.
Ellis B, Carpenter C, Lowthian J, Mooijaart S, Nickel C, Melady D. Statement on Minimum Standards for the Care of Older People in Emergency Departments by the Geriatric Emergency Medicine Special Interest Group of the International Federation for Emergency Medicine. CJEM. 2018;20(3):368–9.
Mooijaart SP, Carpenter CR, Conroy SP. Geriatric emergency medicine—a model for frailty friendly healthcare. Age Ageing. 2022;51(3):afab280.
Phelps K, Regen E, van Oppen JD, Riley P, Lalseta J, Martin G, et al. What are the goals of care for older people living with frailty when they access urgent care? Are those goals attained? A qualitative view of patient and carer perspectives. Int Emerg Nurs. 2022;63: 101189.
Gettel C, Venkatesh A, Dowd H, Hwang U, Ferrigno R, Reid E, et al. A Qualitative Study of “What Matters” to Older Adults in the Emergency Department. West J Emerg Med. 2022;23(4):579–88.
Keeble E, Roberts HC, Williams CD, Van Oppen J, Conroy SP. Outcomes of hospital admissions among frail older people: a 2-year cohort study. Br J Gen Pract. 2019;69(685):e555–60.
Maynou L, Street A, Burton C, Mason SM, Stone T, Martin G, et al. Factors associated with longer wait times, admission and reattendances in older patients attending emergency departments: an analysis of linked healthcare data. Emerg Med J. 2023;40(4):248–56.
van Oppen JD, Valderas JM, Mackintosh NJ, Conroy SP. Patient-reported outcome and experience measures in geriatric emergency medicine. Zeitschrift für Gerontologie und Geriatrie. 2020;54(2):122–4.
Kojima G, Iliffe S, Jivraj S, Walters K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health. 2016;70(7):716.
Crocker TF, Brown L, Clegg A, Farley K, Franklin M, Simpkins S, et al. Quality of life is substantially worse for community-dwelling older people living with frailty: systematic review and meta-analysis. Qual Life Res. 2019;28(8):2041–56.
Melady D. Geriatric emergency medicine: Research priorities to respond to “The Silver Boom.” CJEM. 2018;20(3):327–8.
van Oppen JD, Coats TJ, Conroy SP, Lalseta J, Phelps K, Riley P, et al. What matters most in acute care: an interview study with older people living with frailty. BMC Geriatrics. 2022;22(1):156.
van Oppen JD, Alshibani A, Coats TJ, Graham B, Holch P, Lalseta J, et al. A systematic review and recommendations for prom instruments for older people with frailty in emergency care. J Patient Rep Outcomes. 2022;6(1):30.
Konda SR, Lott A, Saleh H, Gales J, Egol KA. Use of the STTGMA Tool to Risk Stratify 1-Year Functional Outcomes and Mortality in Geriatric Trauma Patients. J Orthop Trauma. 2018;32(9):461–6.
Barker A, Cameron P, Flicker L, Arendts G, Brand C, Etherton-Beer C, et al. Evaluation of RESPOND, a patient-centred program to prevent falls in older people presenting to the emergency department with a fall: A randomised controlled trial. PLoS Med. 2019;16(5): e1002807.
Marten O, Brand L, Greiner W. Feasibility of the EQ-5D in the elderly population: a systematic review of the literature. Qual Life Res. 2022;31(6):1621–37.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95.
Wuorela M, Lavonius S, Salminen M, Vahlberg T, Viitanen M, Viikari L. Self-rated health and objective health status as predictors of all-cause mortality among older people: a prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. 2020;20(1):1–7.
van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–15.
R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2022.
Mokkink L, Prinsen C, Patrick D, Alonso J, Bouter L, de Vet H, et al. COSMIN study design checklist for patient-reported outcome measurement instruments (version July 2019). COSMIN; 2019. Available from: https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf.
Elliott A, Taub N, Banerjee J, Aijaz F, Jones W, Teece L, et al. Does the Clinical Frailty Scale at Triage Predict Outcomes From Emergency Care for Older People? Ann Emerg Med. 2021;77(6):620–7.
Coast J, Peters TJ, Richards SH, Gunnell DJ. Use of the EuroQoL among elderly acute care patients. Qual Life Res. 1997;7(1):1–10.
Pérez-Ros P, Martínez-Arnau FM. EQ-5D-3L for Assessing Quality of Life in Older Nursing Home Residents with Cognitive Impairment. Life (Basel). 2020;10(7):100.
Nikolova S, Hulme C, West R, Pendleton N, Heaven A, Bower P, et al. Normative Estimates and Agreement Between 2 Measures of Health-Related Quality of Life in Older People With Frailty: Findings From the Community Ageing Research 75+ Cohort. Value Health. 2020;23(8):1056–62.
Nguyen AT, Nguyen LH, Nguyen TX, Nguyen HTT, Nguyen TN, Pham HQ, et al. Frailty Prevalence and Association with Health-Related Quality of Life Impairment among Rural Community-Dwelling Older Adults in Vietnam. Int J Environ Res Public Health. 2019;16(20):3869.
Rosenberg T, Montgomery P, Hay V, Lattimer R. Using frailty and quality of life measures in clinical care of the elderly in Canada to predict death, nursing home transfer and hospitalisation - the frailty and ageing cohort study. BMJ Open. 2019;9(11): e032712.
Kaeppeli T, Rueegg M, Dreher-Hummel T, Brabrand M, Kabell-Nissen S, Carpenter CR, et al. Validation of the Clinical Frailty Scale for Prediction of Thirty-Day Mortality in the Emergency Department. Ann Emerg Med. 2020;76(3):291–300.
Cluley V, Martin G, Radnor Z, Banerjee J. Frailty as biographical disruption. Sociol Health Illn. 2021;43(4):948–65.
Etkind SN, Li J, Louca J, Hopkins SA, Kuhn I, Spathis A, et al. Total uncertainty: a systematic review and thematic synthesis of experiences of uncertainty in older people with advanced multimorbidity, their informal carers and health professionals. Age Ageing. 2022;51(8):afac188.
Lin C-F, Huang Y-H, Ju L-Y, Weng S-C, Lee Y-S, Chou Y-Y, et al. Health-Related Quality of Life Measured by EQ-5D in Relation to Hospital Stay and Readmission in Elderly Patients Hospitalized for Acute Illness. Int J Environ Res Public Health. 2020;17(15):5333.
Franke AD. Feasibility of patient-reported outcome research in acute geriatric medicine: an approach to the ‘post-hospital syndrome’. Age Ageing. 2021;50(5):1834–9.
Lucke JA, de Gelder J, Heringhaus C, van der Mast RC, Fogteloo AJ, Anten S, et al. Impaired cognition is associated with adverse outcome in older patients in the Emergency Department; the Acutely Presenting Older Patients (APOP) study. Age Ageing. 2018;47(5):679–84.
Kelly C, Hulme C, Graham L, Ellwood A, Patel I, Cundill B, et al. Inter-rater reliability of care home staff’s proxy judgements with residents’ assessments of their own health-related quality of life: an analysis of the PATCH trial EQ-5D data. Age Ageing. 2021;50(4):1314–20.
Funding
Two authors received funding from the National Institute for Health and Care Research (NIHR): Doctoral Research Fellowship NIHR300901 (JvO) & Senior Investigator (TC).
Author information
Authors and Affiliations
Contributions
JvO conceptualised the study, conducted analyses, and drafted the manuscript under supervision of SC, TC, NM, and JMV. Data were collected by UK Clinical Research Network teams; the site principal investigators and recruiting research practitioners are gratefully acknowledged. JvO takes responsibility for the work overall.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the West Midlands—Coventry & Warwickshire NHS Research Ethics Committee (ref 21/WM/0049). Recruitment was with the informed consent of participants or their consultees. All methods were carried out in accordance with relevant guidelines and regulation.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
van Oppen, J.D., Conroy, S.P., Coats, T.J. et al. Measuring health-related quality of life of older people with frailty receiving acute care: feasibility and psychometric performance of the EuroQol EQ-5D. BMC Emerg Med 23, 137 (2023). https://doi.org/10.1186/s12873-023-00909-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-023-00909-4