Abstract
Background
The population of older trauma patients is increasing. Those patients have heterogeneous presentations and need senior-friendly triaging tools. Systolic blood pressure (SBP) is commonly used to assess injury severity, and some authors advocated adjusting SBP threshold for older patients. We aimed to describe and compare the relationship between mortality and SBP in older trauma patients and their younger counterparts.
Methods
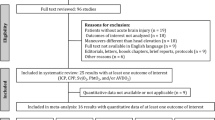
We included patients admitted to three level-I trauma centres and performed logistic regressions with age and SBP to obtain mortality curves. Multivariable Logistic regressions were performed to measure the association between age and mortality at different SBP ranges. Subgroup analyses were conducted for major trauma and severe traumatic brain injury admissions.
Results
A total of 47,661 patients were included, among which 12.9% were aged 65–74 years and 27.3% were ≥ 75 years. Overall mortality rates were 3.9%, 8.1%, and 11.7% in the groups aged 16–64, 65–74, and ≥ 75 years, respectively. The relationship between prehospital SBP and mortality was nonlinear (U-shape), mortality increased with each 10 mmHg SBP decrement from 130 to 50 mmHg and each 10-mmHg increment from 150 to 220 mmHg across all age groups. Older patients were at higher odd for mortality in all ranges of SBP. The highest OR in patients aged 65–74 years was 3.67 [95% CI: 2.08–6.45] in the 90–99 mmHg SBP range and 7.92 [95% CI: 5.13–12.23] for those aged ≥ 75 years in the 100–109 mmHg SBP range.
Conclusion
The relationship between SBP and mortality is nonlinear, regardless of trauma severity and age. Older age was associated with a higher odd of mortality at all SBP points. Future triage tools should therefore consider SBP as a continuous rather than a dichotomized predictor.
Similar content being viewed by others
Background
As life expectancy is increasing, trauma patients’ demographic is rapidly evolving. Since 2014, older adults aged 65 years and over represent the majority of admissions in Level-I trauma centres in the province of Québec (Canada) [1]. In the United Kingdom, a substantial increase (from 8.1% in 1990 to 26.9% in 2013) of the proportion of adults aged 75 years and over sustaining major trauma was reported [2]. In the USA, the proportion of older (≥ 65 years) trauma patients increased from 18 to 30% between 2005 and 2015 [3]. The aging trauma population represents a worldwide challenge for clinicians because of heterogeneous patient presentations due to frailty [4], pre-existing comorbidities [5], and the use of medications such as beta-blockers or anticoagulants [6] that alter physiological responses to trauma. Furthermore, advanced age has been associated with undertriage (inaccurate triage that results in a patient who requires higher-level care not being transported to a Level I or Level II trauma centre) [7], longer length of stay [8] and poor outcomes (higher mortality, morbidity and adverse events) compared to younger adults [9].
However, recent systematic reviews reported that current prehospital trauma triage tools may not accurately identify older patients with major trauma [10, 11]. It is therefore imperative to adapt trauma care with senior-friendly tools. For example, using a specific geriatric protocol to identify high-risk patients was found to reduce mortality [12]. Elsewhere, modified triage tools have been evaluated and have shown better sensitivity in identifying major trauma patients who need specialized trauma care [11, 13]. Although trauma patients’ initial systolic blood pressure (SBP) is commonly used as a severity and mortality indicator in triage protocols and as a trauma team activation criterion the standard SBP threshold (< 90 mmHg) may need to be adjusted for older patients [14, 15] or higher [16] could be a sign of hypotension and that this threshold could better identify seriously injured older patients [17]. However, the literature is heterogenous, and there is no consensus on whether it is accurate to use a unique threshold to define hypotension in the population of trauma patients.
Therefore, the main objective of this study was to describe and compare the relationship between mortality and systolic blood pressure (SBP) in older patients (65–74 years and ≥ 75 years) and their younger counterparts (16–64 years).
Methods
Study design and setting
We conducted a multicentre retrospective study based on the provincial Quebec Trauma Registry (RTQ), managed by the Quebec Ministry of Health and Social Services (Ministère de la Santé et des Services sociaux). The RTQ includes data from the 59 designated trauma centres of the province’s inclusive trauma system, which serves a population of 8.5 million in a geographic area of approximately 1.7 million km2 [18]. The system includes three Level-I adult trauma centres and two paediatric trauma centres providing highly specialized care in metropolitan areas (Montréal and Québec city). Trauma level designations are based on American College of Surgeons’ criteria and are periodically revised following on-site visits [19, 20].
Study population
We included patients aged ≥ 16 years with a primary diagnosis of trauma between March 2003 and December 2017 who were directly transported from the prehospital setting or transferred to one of the three level-I adult trauma centres. We excluded patients aged ≥ 65 years admitted for isolated hip fractures since this type of trauma is often related to chronic disease rather than a traumatic event [21]. Patients were stratified into three age groups: 16–64, 65–74, and ≥ 75 years.
Study data
Data from this provincial registry is prospectively collected and coded by trained medical archivists using patient electronic medical charts [22]. The RTQ is centralized and subject to systematic and periodic validation by ministry delegates to identify and rectify aberrant data values and verify date and time chronology. Inter-rater reliability is assessed randomly, thus ensuring a 98% accuracy.
Initial SBP was the first SBP measured by paramedics in the prehospital setting. We then used the first SBP measured upon ED admission if not available. We used the SBP measured in the initial ED if prehospital SBP was unavailable in transferred patients. The Injury Severity Score (ISS) was calculated after anatomic assessments were completed and was based on the 2008 version of the Abbreviated Injury Scale (AIS).
Outcome measures
The primary outcome of this study was in-hospital mortality (including ED deaths).
Data analysis
Categorical variables were described with frequencies and percentages, while medians with interquartile range (IQR), means, and standard deviation (SD) were computed for continuous variables. To obtain mortality curves by prehospital or ED SBP, we performed logistic regressions with age groups, and SBP was modelled using restricted cubic splines with 4 knots placed at the (5-35-65-95) percentiles. Knot locations were identified heuristically using Harrel’s Regression Modelling Strategies, and 95% CI were obtained using a clustered bootstrap [23]. The inflexion points of each curve were determined using the finite difference formula [24]. Three time periods (2003–2007, 2008–2012, and 2013–2017) were defined to assess whether there was a cohort effect. Odds ratios were computed to determine the association between age and mortality at different ranges of SBP, controlling for the following covariates: sex, mechanism, ISS, and comorbidities. We calculated sensitivity, specificity, and positive and negative predictive values for each SBP cutoff per 10 mmHg from 90 to 130 mmHg. We used multiple imputation with chained equation to handle missing Glasgow Coma Scale (GCS) score data [25]. We used Rubin’s rules to combine estimates across imputed datasets and to obtain 95% Confidence Intervals (95% CI) [26]. Patients with severe Traumatic Brain Injury (TBI, GCS score ≤ 8) and major trauma (ISS > 12) [27] present unique challenges and complexities compared to the broader population of trauma patients. This may be due to the distinct clinical characteristics, treatment needs, and potential variations in the relationship between SBP and mortality within these subgroups. We therefore performed further analyses within these two specific patient populations. Statistical analyses were conducted using SAS (Statistical Analysis System v9.4, SAS Institute Inc., Cary, NC, USA).
Ethics approval
The CHU de Québec-Université Laval Research Ethics Board approved this project (MP-20-2017-3180).
Results
Sociodemographic characteristics
Overall, 53,324 trauma admissions were recorded within the three level-I adult trauma centres. Of those, 47,661 met our inclusion criteria and were therefore considered for analyses. Patients aged 16–64 years represented 59.8% of our cohort, 12.9% were aged 65–74 years, and 27.3% were 75 years and over. The most common mechanism of trauma was fall in both groups of older patients (65–74 years: 73.1%, and ≥ 75 years: 86.6%), while motor vehicle collision was the most common among younger adults (38.5%). Mean ± SD SBP was higher in older patients (65–74 years: 141.8 mmHg ± 27.3, and ≥ 75 years:147.9 mmHg ± 27.6) compared to younger patients (131.3 mmHg ± 23.5). Mean ± SD ISS was 14 ± 11 in patients under the age of 65 and 14 ± 10 in patients aged 65–74 years, while it decreased to 12 ± 8.8 in those aged 75 years and over. In-hospital mortality was higher in older patients (3.9%, 8.1% and 11.7% for those aged 16–64 years, 65–74 years and ≥ 75 years, respectively, Table 1). The median [IQR] time between trauma and death was 5.3 [1.9–14.3] days.
The most common severe injuries (AIS ≥ 3) affected the head in all age groups (27.9%, 35.6% and 29.9%, Online resource 1).
Initial SBP and mortality
A nonlinear, U shape relationship between SBP and mortality was found in both older and younger patients. Mortality increased in all age groups across a wide range of SBP (from 130 to 90 mmHg), and this increase was higher for older patients (Fig. 1a). We observed distinct inflection points where mortality demonstrated an escalation in response to a decrease in SBP. Specifically, in the group of patients aged 16–64 years, the inflection point was identified at 129 mmHg while it was at 139 mmHg for individuals aged 65–74 years, and at 152 mmHg mmHg for patients aged ≥ 75 years (Fig. 1a). Similar results were observed with major trauma admissions (125, 131, and 146 mmHg respectively, Fig. 1b) and severe TBI (129, 130, and 135 mmHg respectively, Fig. 1c).
a Relationship between systolic blood pressure and in-hospital mortality in the global trauma population. b Relationship between systolic blood pressure and in-hospital mortality in patients with severe trauma (Injury Severity Score > 12). c Relationship between systolic blood pressure and in-hospital mortality in patients with severe traumatic brain injury (Glasgow Coma Scale score ≤ 8)
When assessing cohort effect in the three periods (2003–2007, 2008–2012 and 2013–2017), the results were similar in the global trauma population (Online resource 2a), as well as in the major trauma population (Online resource 2b) and the group of patients presenting with severe TBI (Online resource 2c).
Older age was associated with a higher odd for mortality at all ranges of SBP compared to younger adults (Fig. 2a). The highest OR for 65–74 years patients were 3.7 [95% CI: 2.1;6.5] in the 90–99 mmHg SBP range and 7.9 [95% CI: 5.1;12.2] for those aged ≥ 75 years in the 100–109 mmHg SBP range. Similar findings were found in the group of patients with major trauma (Fig. 2b) and in severe TBI patients with a SBP of 100–109, 120–129 and 130–139 mmHg (Fig. 2c).
a Adjusted odds ratio for mortality in older trauma patients compared to younger patients according to initial blood pressurea. b Adjusted odds ratio for mortality in older patients with severe trauma (ISS > 12) compared to younger patients according to initial blood pressurea. c Adjusted odds ratio for mortality in older patients with severe traumatic brain injury (GCS ≤ 8) compared to younger patients according to initial blood pressure
A higher odd for mortality was also found in older adults with hypertension (140 mmHg to ≥ 180 mmHg) compared to their younger counterparts (Fig. 2a).
Discussion
Our large Canadian trauma registry study found that the relationship between SBP and in-hospital mortality was non-linear (U-shape). Mortality was higher in older adults compared to their younger counterparts at all SBP points. It was also noted that hypotension was associated with a low sensitivity to predict mortality across all age groups when used alone.
Interpretation of findings and comparison to previous studies
The American College of Surgeons Committee on Trauma (ACS-COT) recommends treating patients with severe trauma in level-I or II trauma centres. This includes adults with SBP < 90 mmHg at any time [28]. Most current prehospital algorithms use a 90 mmHg cutoff to identify severe trauma patients, including those based on Vittel triage criteria [29]. This cutoff has been widely debated, and some authors previously suggested that a SBP threshold of < 110 mmHg could be a more clinically accurate definition of hypotension [30,31,32,33]. Some even suggested integrating thresholds higher than 110 mmHg in triage protocols. For instance, Oyetunji et al. reported that the highest area under the receiver operating characteristic curve (AUC) curve value for patients aged ≥ 65 years intersected at an SBP of 117 mmHg [16]. Elsewhere a 120 mmHg threshold was found to better predict mortality for patients aged between 50 and 69 years compared to 140 mmHg for those aged ≥ 70 years [34].
Brown et al. compared the impact of two SBP thresholds (90 mmHg vs 110 mmHg) on older adults (≥ 65 years) triage performance. They reported that using the higher threshold of 110 mmHg led to a 4.4% reduction of undertriage. The authors have also found that the optimal SBP threshold to predict mortality would be 118 mmHg, yielding a sensitivity of 29% and a specificity of 86% [14]. Increasing the SBP threshold to redefine hypotension in older adults may lead to lower undertriage rates, a critical issue in that population, which was found to be at higher odd of mortality compared to their younger counterparts with equal or less severe injuries. However, despite improved performance to predict poor outcomes a cutoff of < 110 mmHg remained associated with low sensitivity in previous studies as in the present one [31,32,33]. Thus, this suggests that hypotension should not be used alone to predict mortality in trauma patients.
Hypertension was also associated with increased mortality in trauma patients. This may be related to multiple underlying mechanisms. First, hypertension may exacerbate hemorrhages, leading to worsened outcomes, justifying the concept of permissive hypotension [35]. Second, hypertension may be a marker of underlying cardiovascular comorbidities that increase the risk of mortality in patients with severe trauma. Patients with hypertension may also be prone to cardiovascular events, such as myocardial infarction, which can increase mortality in patients with severe trauma. Third, hypertension can result in alterations to the microcirculation that decrease blood flow to injured tissues, hence increasing the risk of complications. Reynolds et al. hypothesized in a rat model of hemorrhagic shock that systemic and microvascular alterations accompanying chronic hypertension would increase the vulnerability to hemorrhage relative to normotensive controls [36]. Fourth, hypertension may be the consequence of severe brain injuries resulting in intracranial hypertension (Cushing reflex) [37].
Strengths and limitations
The present study is not without limitations. First, when prehospital SBP data was unavailable, we used initial SBP measured upon ED arrival, which may be slightly different. Nevertheless, paramedics were not trained to perform fluid resuscitation or to use vasopressors which could have led to a measurement variation between pre- and in-hospital SBP. Furthermore, in a similar prehospital system, Bruns et al. noted that the prehospital SBP was strongly correlated with the first SBP in the ED [30]. Another potential limitation is that only patients who met the RTQ inclusion criteria and were treated in level-I trauma centres were included in our analyses. Hence, our findings could be used to debate a new SBP threshold dedicated to identifying a major trauma or to activate a trauma team for older patients admitted to a level-I trauma centre. Finally, the odds ratio presented here likely overstate the true associations, given the elevated mortality risks observed among older patients [38].
The accuracy of the outcome (all causes of in-hospital mortality) could be debated. Indeed, some patients with non-trauma-related deaths may have been included in the analysis since the cause of death is not reported in the registry. Nevertheless, this potential bias is minor since half of the deaths occurred within the first five days after the trauma. It should also be acknowledged that some potential confounders that we were unable to consider and may impact the present findings.
Patient chronic conditions such as hypertension and anti-hypertensive medication usage may have affected SBP measures and should be considered in future investigations. In addition, some patients with TBI may experience high blood pressure due to intracranial hypertension (Cushing’s triad), which is associated with increased mortality risk. Therefore, the relationship between high blood pressure and mortality in TBI patients remains unclear, and further research is warranted to explore whether higher mortality rates are due to the severity of TBI-induced intracranial hypertension or HBP itself.
Clinical implications
Higher SBP cutoffs should be considered to define hypotension in current triage protocols or trauma team activation criteria for patients over the age of 65. The study also highlights the U-shaped relationship between SBP and mortality among injured patients admitted to the ED. Consequently, healthcare providers should be aware that patients presenting with hypertension may also be at higher risk for mortality. As such, widely used binary cutoffs to define hypotension and predicting mortality should be abandoned in favor of more tailored approaches. Future digital tools should consider integrating SBP as a continuous rather than a dichotomized predictor to account for the U-shaped relationship between SBP and mortality. Such approach may contribute to mitigate undertriage in this older adult population.
Finally, the study highlights the limitations of using hypotension alone to predict mortality, given its low sensitivity.
Research implications
This study was not designed to determine which SBP threshold would be optimal to predict mortality. This would require building or updating clinical decision rules with state-of-the-art methodology [39, 40]. Furthermore, as has been emphasized by other authors, continuous predictors (SBP in the present study) should not be dichotomized [41]. This may create problems rather than solving them, notably a considerable loss of information. Hence, further age-based risk prediction model studies are required to develop senior-friendly triage tools, in which other predictors should be integrated along with SBP to predict mortality. In addition, clinical decision tools should include SBP modelled using restricted cubic spines of fractional polynomials to capture the nonlinear association with in-hospital mortality.
Conclusion
The relationship between SBP and mortality is nonlinear, regardless of trauma severity and age. Older age was associated with a higher odd of mortality at all SBP points. Future triage tools should therefore consider SBP as a continuous rather than a dichotomized predictor.
Availability of data and materials
The authors used governmental datasets (the Registre des traumatismes du Québec) for this study. These datasets are available through a formal request at the Commission d’accès à l’information of the Gouvernement du Québec.
Abbreviations
- SBP:
-
Systolic blood pressure
- mmHg:
-
Millimetres of mercury
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- ED:
-
Emergency Department
- RTQ:
-
Quebec Trauma Registry
- IQR:
-
Interquartile range
- SD:
-
Standard Deviation
- ISS:
-
Injury Severity Score
- AIS:
-
Abbreviated Injury Scale
- GCS:
-
Glasgow Coma Scale
- TBI:
-
Traumatic Brain Injury
- SAS:
-
Statistical Analysis System
- ACS-COT:
-
American College of Surgeons Committee on Trauma
- AUC:
-
Area Under the receiver operating characteristic curve
References
Benhamed A, Batomen B, Boucher V, Yadav K, Mercier E, Isaac CJ, Berube M, Bernard F, Chauny JM, Moore L, et al. Epidemiology, injury pattern and outcome of older trauma patients: a 15-year study of level-I trauma centers. PLoS One. 2023;18(1):e0280345.
Kehoe A, Smith JE, Edwards A, Yates D, Lecky F. The changing face of major trauma in the UK. Emerg Med J. 2015;32(12):911–5.
Jiang L, Zheng Z, Zhang M. The incidence of geriatric trauma is increasing and comparison of different scoring tools for the prediction of in-hospital mortality in geriatric trauma patients. World J Emerg Surg. 2020;15(1):59.
Brousseau AA, Dent E, Hubbard R, Melady D, Émond M, Mercier É, Costa AP, for the Multinational Emergency Department Study, Gray LC, Hirdes JP, et al. Identification of older adults with frailty in the Emergency Department using a frailty index: results from a multinational study. Age Ageing. 2018;47(2):242–8.
Mubang RN, Stoltzfus JC, Cohen MS, Hoey BA, Stehly CD, Evans DC, Jones C, Papadimos TJ, Grell J, Hoff WS, et al. Comorbidity-polypharmacy score as predictor of outcomes in older trauma patients: a retrospective validation study. World J Surg. 2015;39(8):2068–75.
Williams TM, Sadjadi J, Harken AH, Victorino GP. The necessity to assess anticoagulation status in elderly injured patients. J Trauma. 2008;65(4):772–6 discussion 776-777.
Uribe-Leitz T, Jarman MP, Sturgeon DJ, Harlow AF, Lipsitz SR, Cooper Z, Salim A, Newgard CD, Haider AH. National study of triage and access to trauma centers for older adults. Ann Emerg Med. 2020;75(2):125–35.
Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–14.
Sammy I, Lecky F, Sutton A, Leaviss J, O’Cathain A. Factors affecting mortality in older trauma patients-A systematic review and meta-analysis. Injury. 2016;47(6):1170–83.
Fuller G, Pandor A, Essat M, Sabir L, Buckley-Woods H, Chatha H, Holt C, Keating S, Turner J. Diagnostic accuracy of prehospital triage tools for identifying major trauma in elderly injured patients: a systematic review. J Trauma Acute Care Surg. 2021;90(2):403–12.
Alshibani A, Alharbi M, Conroy S. Under-triage of older trauma patients in prehospital care: a systematic review. Eur Geriatr Med. 2021;2(5):903-19.
Bradburn E, Rogers FB, Krasne M, Rogers A, Horst MA, Belan MJ, Miller JA. High-risk geriatric protocol: Improving mortality in the elderly. J Trauma Acute Care Surg. 2012;73(2):435–40.
Ichwan B, Darbha S, Shah MN, Thompson L, Evans DC, Boulger CT, Caterino JM. Geriatric-specific triage criteria are more sensitive than standard adult criteria in identifying need for trauma center care in injured older adults. Ann Emerg Med. 2015;65(1):92–100 e103.
Brown JB, Gestring ML, Forsythe RM, Stassen NA, Billiar TR, Peitzman AB, Sperry JL. Systolic blood pressure criteria in the National Trauma Triage Protocol for geriatric trauma: 110 is the new 90. J Trauma Acute Care Surg. 2015;78(2):352–9.
Heffernan DS, Thakkar RK, Monaghan SF, Ravindran R, Adams CA, Kozloff MS, Gregg SC, Connolly MD, Machan JT, Cioffi WG. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69(4):813–20.
Oyetunji TA, Chang DC, Crompton JG, Greene WR, Efron DT, Haut ER, Cornwell EE 3rd, Haider AH. Redefining hypotension in the elderly: normotension is not reassuring. Arch Surg. 2011;146(7):865–9.
Newgard CD, Lin A, Eckstrom E, Caughey A, Malveau S, Griffiths D, Zive D, Bulger E. Comorbidities, anticoagulants, and geriatric-specific physiology for the field triage of injured older adults. J Trauma Acute Care Surg. 2019;86(5):829–37.
Institut national d'excellence en santé et services sociaux. In: Continuum de services en traumatologie. Québec: INESSS; 2015. https://www.inesss.qc.ca/thematiques/sante/traumatologie/continuum-de-services-en-traumatologie-cst.html.
American College of Surgeons, Committee on Trauma. Resources for optimal care of the injured patient. Chicago: American College of Surgeons, Committee on Trauma; 2014.
Bracewell N, Winchester DE. Accreditation in health care: does it make any difference to patient outcomes? BMJ Qual Saf. 2021;30(11):845-7.
Moore L, Stelfox HT, Turgeon AF, Nathens AB, Le Sage N, Emond M, Bourgeois G, Lapointe J, Gagne M. Rates, patterns, and determinants of unplanned readmission after traumatic injury: a multicenter cohort study. Ann Surg. 2014;259(2):374–80.
Moore L, Lavoie A, Sirois MJ, Amini R, Belcaid A, Sampalis JS. Evaluating trauma center process performance in an integrated trauma system with registry data. J Emerg Trauma Shock. 2013;6(2):95–105.
Huang FL. Using cluster bootstrapping to analyze nested data with a few clusters. Educ Psychol Meas. 2018;78(2):297–318.
Wicklin R. Find points where a regression curve has zero slope. 2020. https://blogs.sas.com/content/iml/2020/05/13/regression-curve-zero-slope.html.
Moore L, Hanley JA, Lavoie A, Turgeon A. Evaluating the validity of multiple imputation for missing physiological data in the national trauma data bank. J Emerg Trauma Shock. 2009;2(2):73–9.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99.
Van Ditshuizen JC, Sewalt CA, Palmer CS, Van Lieshout EMM, Verhofstad MHJ, Den Hartog D, Dutch Trauma Registry S. The definition of major trauma using different revisions of the abbreviated injury scale. Scand J Trauma Resusc Emerg Med. 2021;29(1):71.
Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1–20.
Group fT, Bouzat P, Ageron FX, Brun J, Levrat A, Berthet M, Rancurel E, Thouret JM, Thony F, Arvieux C, et al. A regional trauma system to optimize the pre-hospital triage of trauma patients. Crit Care. 2015;19(1):111.
Bruns B, Gentilello L, Elliott A, Shafi S. Prehospital hypotension redefined. J Trauma. 2008;65(6):1217–21.
Hasler RM, Nuesch E, Juni P, Bouamra O, Exadaktylos AK, Lecky F. Systolic blood pressure below 110 mm Hg is associated with increased mortality in blunt major trauma patients: multicentre cohort study. Resuscitation. 2011;82(9):1202–7.
Park SJ, Lee MJ, Kim C, Jung H, Kim SH, Nho W, Seo KS, Park J, Ryoo HW, Ahn JY, et al. The impact of age and receipt antihypertensives to systolic blood pressure and shock index at injury scene and in the emergency department to predict massive transfusion in trauma patients. Scand J Trauma Resusc Emerg Med. 2021;29(1):26.
Eastridge BJ, Salinas J, McManus JG, Blackburn L, Bugler EM, Cooke WH, Convertino VA, Wade CE, Holcomb JB. Hypotension begins at 110 mm Hg: redefining “hypotension” with data. J Trauma. 2007;63(2):291–7 discussion 297-299.
Edwards M, Ley E, Mirocha J, Hadjibashi AA, Margulies DR, Salim A. Defining hypotension in moderate to severely injured trauma patients: raising the bar for the elderly. Am Surg. 2010;76(10):1035–8.
Rossaint R, Afshari A, Bouillon B, Cerny V, Cimpoesu D, Curry N, Duranteau J, Filipescu D, Grottke O, Gronlykke L, et al. The European guideline on management of major bleeding and coagulopathy following trauma: sixth edition. Crit Care. 2023;27(1):80.
Reynolds PS, Song KS, Tamariz FJ, Wayne Barbee R. Hypertension and vulnerability to hemorrhagic shock in a rat model. Shock. 2015;43(2):148–56.
Fodstad H, Kelly PJ, Buchfelder M. History of the cushing reflex. Neurosurgery. 2006;59(5):1132–7 discussion 1137.
O’Connor AM. Interpretation of odds and risk ratios. J Vet Intern Med. 2013;27(3):600–3. https://doi.org/10.1111/jvim.12057.
Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925–31.
Moons KG, Kengne AP, Grobbee DE, Royston P, Vergouwe Y, Altman DG, Woodward M. Risk prediction models: II. External validation, model updating, and impact assessment. Heart. 2012;98(9):691–8.
Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25(1):127–41.
Acknowledgements
We would like to thank the Emergency physicians of the Hôpital de l’Enfant-Jésus (CHU de Quebec-Université Laval) for their support.
Funding
AB received a scholarship from the Fondation du CHU de Québec (no grant number). This project was funded by the Fonds de recherche du Québec – Santé under Grant number #33239. These funding agencies were in no way involved in the design, data collection and analyses of this study.
Author information
Authors and Affiliations
Contributions
AB, BB, ME contributed to conception and design. AB contributed to data analysis. EM, FB, JBL and ME contributed to data acquisition. AB, BB, VB, CJI, KT and ME drafted the manuscript. All authors critically revised the manuscript, contributed to interpretation, gave final approval, and agreed to be accountable for all aspects of the work ensuring integrity and accuracy. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project was approved by the CHU de Québec-Université Laval Research Ethics Board (MP-20–2017-3180). and the Commission d’Accès à l’information; therefore, patient consent was not required. Data were all anonymous before analysis.
Consent for publication
Not applicable.
Competing interests
None of the authors has competing interests regarding this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Benhamed, A., Batomen, B., Boucher, V. et al. Relationship between systolic blood pressure and mortality in older vs younger trauma patients – a retrospective multicentre observational study. BMC Emerg Med 23, 105 (2023). https://doi.org/10.1186/s12873-023-00863-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-023-00863-1