Abstract
Background
Stroke is rapidly developing clinical signs of focal/ global disturbance of cerebral function, with symptoms lasting more than 24 h and leading to death. Data showed that stroke deaths in Ethiopia reached nearly seven percent of total deaths. Despite this report, there is a paucity of investigations about the problem.
Objective
To determine in-hospital mortality and its associated factors among hospitalized stroke patients in Hiwot Fana Comprehensive Specialized University Hospital and Jugal General Hospital, eastern Ethiopia from September 2016–August 2022 G.C.
Methods
A retrospective cohort study was conducted among hospitalized stroke patients. A sample size of 395 medical records was selected from a total of 564 stroke patients by a simple random sampling technique. The data was analyzed by SPSS version 26 using bivariable and multivariable cox-regression models. A p-value of 0.05 and less at a 95% confidence interval was used to establish a statistically significant association.
Results
Of the total, 109 (27.6%) died in the hospital while 57.2% and 15.2% of them were discharged with improvement and against medical advice, respectively. Age greater than 65 (AHR = 4.71, 95% CI = 1.11–19.96), creatinine level > 1.2 mg/dl (AHR = 1.54, 95% CI = 1.0-2.39), and co-morbidity with atrial fibrillation (AHR = 1.48, 95% CI = 1.0-2.21) were significantly associated with in-hospital mortality.
Conclusion
In-hospital mortality was found in more than a quarter of stroke patients. Mortality was more likely increased among the patients with age > 65, serum creatinine level > 1.2 mg/dl, and atrial fibrillation. Hence, these high-risk patients need to be monitored.
Similar content being viewed by others
Introduction
Stroke is defined as rapidly developing clinical signs of focal or global disturbance of cerebral function, with symptoms lasting more than 24 h, leading to death, with no apparent cause other than a pathological process of a blood vessel [1]. Stroke results in acute neurological dysfunction, which can manifest clinically as unilateral weakness of the face, arm, or leg, speech impediment, loss of vision, vertigo, or falling. It is caused by injury to the brain tissue and interruption of the blood supply, which leaves the body with insufficient amounts of oxygen and nutrients [2]. Hence, reducing ongoing neurologic injury, preventing complications due to immobility and neurologic dysfunction, and preventing stroke recurrence are the goals of treatment for acute stroke [3]. In order to achieve the desired outcome, stroke care should be delivered as quickly as possible. Moreover, the quality of stroke care, including a rapid diagnosis using cutting-edge imaging and adequate therapy consisting of thrombolysis or thrombectomy, as the most updated approved treatment, needs to be improved [4, 5].
According to the Global Burden of Disease (GBD) 2019 stroke report, there were 12.2 million incident cases, 101 million prevalent cases, 143 million disability-adjusted life years (DALYs) due to stroke, and 655 million stroke-related deaths globally. The majority of this—80% of all incidents, 77% of all survivors, 87% of all deaths from stroke, and 89% of all stroke-related DALYs—occurs in low- and middle-income countries (LMICs), including those in Africa [6]. Africa appears to be the global capital for strokes, with at least six Africans having a stroke every minute. The prevalence of strokes in Africa ranges from 15 per 100,000 in Ethiopia to 963 per 100,000 in Egypt and 1460 per 100,000 in Niger [7]. Epidemiological transitions and widespread vascular risk factors made stroke the most common health problem in Sub-Saharan Africa (SSA) at an early age; the estimated lifetime risk of developing stroke was 11.8% [8].
In Ethiopia, the burden and outcome of stroke vary over time and between regions. Between 2014 and 2019, stroke accounted for 7.5–19.3% and 11–42.8% of hospital admissions and deaths, respectively [9]. According to data from the WHO, stroke-related deaths increase over time, with 4.71% of total deaths in the 2014 report and 6.98% of total deaths in the 2020 report [10,11,12,13]. In addition, the mean age of stroke patients who present to hospitals is younger than stroke patients in western countries [14]; this could be an additional burden impacting productivity. The prognosis of stroke patients was extremely poor in Ethiopia. This is mostly due to a lack of important medications such as r-tPA, excessively prolonged pre-hospital delays, financial constraints, and a lack of CT scans [8, 15, 16]. Hence, identifying predictors of mortality following acute stroke is of paramount importance for clinicians so that specific therapies and management strategies can be applied to patients at high risk of dying with a consequent reduction in stroke mortality and disability [1].
Factors associated with stroke mortality and epidemiological studies considering patient clinical characteristics and socio-demographic features are limited in eastern, Ethiopia. Accordingly, this study aimed to determine in-hospital mortality of stroke and its associated factors in the selected public hospitals of eastern Ethiopia.
Methods and materials
Study design, setting, and period
A retrospective cohort study was conducted to determine in-hospital mortality at Hiwot Fana Comprehensive Specialized University Hospital (HFCSUH), and Jugal General Hospital (JGH), which are located in Harari Regional State, 526 km away from Addis Ababa, the capital city of Ethiopia, from September 11, 2016, to August 31, 2022, G.C. In the Harari region, HFCSUH and JGH are public hospitals that provide healthcare services to people around Harar and neighboring regions like Oromia Regional State, Dire Dawa City Administration, and Somali Regional State. They are delivering different health services to the community, like surgery, dental care, ophthalmologic, internal medicine, gynecology and obstetrics, pediatrics, maternal and child health (MCH), TB and HIV (TB/HIV), intensive medical care, neurology services, mental health care, dermatology, and venereal disease services, pharmacy, oncologic services, and laboratory services [17].
Study population
All stroke patients above 18 years of age with either a clinical diagnosis of stroke (without neuroimaging but treated as hemorrhagic or ischemic stroke) or a confirmed diagnosis of stroke with a CT scan during the study period from September 2016 to August 2022 G.C. All patient medical cards that fulfilled the inclusion criteria were included in the study. Medical record cards of stroke patients with incomplete information such as unknown outcomes (referred or disappeared), lost or missing data, or transient ischemic attack were excluded.
Sample size determination and sampling technique
A sample size was calculated considering the objectives of the study and previously published information [18]. Accordingly, the larger size was taken by adding 10% contingency, which was 395.
From September 11, 2016, to August 31, 2022, a total of 564 (403 from HFCSUH and 161 from JGH) adult stroke patients received care. Then, record numbers of those patients’ medical records were obtained from the medical registration book of the medical ward of hospitals. Finally, 395 patients’ medical records included in the study were selected using the proportionally allocated simple random sampling technique (Fig. 1).
Data collection methods
A data abstraction tool was developed by reviewing different literature [8, 19,20,21,22,23]. Identification cards of hospitalized patients with stroke were collected from a discharge summary of the patients who had been hospitalized during the period. A patient’s medical records were used to collect demographic characteristics, outcomes of treatment, comorbidity, medication for treatment, and clinical data such as vital signs and subtypes of stroke. Data was collected by two clinical pharmacists and one clinical nurse using data collection tools.
Variables
Dependent variables
-
In-hospital mortality.
Independent variables
-
Demographic factors (age, sex, marital status, education, occupational status).
-
Disease-related factors (hypertension, atrial fibrillation, DM, previous stroke, types of strokes, aspiration pneumonia, kidney injury, raised intracranial pressure).
-
Medication-related factors (prescribed medication) and other factors (lack of resources, length of hospital stays, median time from onset of symptom to hospitalization, economic status, or income).
Operational definitions
In-hospital mortality
A stroke patient died in the hospital after he/she was admitted to the hospital [24].
Stroke
was defined by WHO clinical criteria as rapidly developing clinical signs of (usually focal) disturbance of cerebral function lasting more than 24 h or leading to death [6].
Transient ischemic attack
which is defined as lasting less than 24 h, and patients with stroke symptoms caused by subdural hemorrhage, tumors, poisoning, or trauma [6].
Ischemic stroke
is defined as an episode of neurological dysfunction due to focal cerebral, spinal, or retinal infarction [6].
Hemorrhagic stroke
was defined as a stroke with a focal collection of blood in the brain not due to trauma [6].
Glasgow Coma Scale (GCS)
The measurement scale used to measure the level of consciousness of patients with stroke GCS is defined as good if the patient has a mild brain injury or is alert (GCS 13–15) or a moderate brain injury or is drowsy (GCS 9–12). GCS is defined as poor if the patients have severe brain injury or are unconscious (GCS (8)) [20].
Event
A stroke patient who died during treatment from any cause [9].
Time to death
Time from the first confirmed diagnosis date of stroke to death [9].
Survival status
The status of the patient’s survival to the outcome (death) or censored [9].
Data quality control
Before starting the data collection, the data collection format was cross-matched with available information on records, and then the study questions were rearranged as necessary. Incomplete charts were discarded. Cross-checking was done in both hospitals for 5% of hospitalized stroke patients’ medical records to ensure the reliability and variability of the data collection tools. After pretesting, all necessary adjustments were made to the data collection instruments before implementation in the main study. Data collectors were trained for half a day on data collection techniques. Supervision was provided by the principal investigators during the process, and any inconsistencies were amended on time.
Methods of data analysis
The collected data was checked, cleaned, and entered using Epidata Manager Version 4.6 and analyzed using SPSS version 26. Descriptive statistics, including frequency with percentage, and mean with standard deviations, were used to present the result. Categorical variables were compared by using the chi-square test or Fisher’s exact test, and continuous variables were compared by using the student’s t-test. Kaplan Meier survival analysis method was used to predict the probability of death over follow-up time. Cox regression was used to identify factors associated with hospital mortality. Variables with P ⩽ 0.25 were considered as cut-off points to select candidate variables in binary Cox regression. Multivariable Cox was used to identify factors associated with in-hospital mortality from stroke. Variables with a p-value of less than or equal to 0.05 were declared significantly associated with in-hospital mortality in multivariable Cox regression analysis. The adjusted hazards ratio (AHR) with a 95% confidence interval (CI) was used to express the association between the in-hospital mortality and the independent variables.
Results
Socio-demographic characteristics of stroke patients
From the total of 395 patients with stroke included in the study, nearly two-thirds (247, or 62.5%) of them were male. The mean age of the patients was 61.02 ± 14.37 years and nearly half of them (51.1%) were urban dwellers (Table 1).
Clinical and laboratory characteristics
Of the total of 395 patients with stroke, nearly two-thirds (64.6%) were diagnosed with ischemic stroke, while the rest of the patients had hemorrhagic stroke. The most common co-morbid disease condition identified among the patients was hypertension (49.1%) followed by diabetes (23.8%) (Table 2).
The mean (SD) systolic blood pressure and diastolic blood pressure at hospitalization were 148.73 ± 33.25 mmHg and 85.08 ± 18.64 mmHg, respectively. The mean random blood glucose at hospitalization was 167.11 ± 77.28, and 28.8% of the patients had elevated blood glucose (> 180 mg/dl). The mean time of presentation from symptom onset was 34.42 ± 26.33 h, with a median of 24 h. The mean (SD) Glasgow Coma Scale (GCS) at hospitalization was 11.04 ± 3.47, and the mean (SD) length of hospital stay was 8.34 ± 3.71 days (Table 3).
In-hospital mortality of stroke patients
Of the 395 patients, 109 (27.6%) died, and 286 (72.4%) were discharged alive. Of live patients, about 60 (15.2%) were left against medical advice on self and family requests, and 226 (57.2%) had improved outcomes. Of 109 patients who died during hospitalization, 56 (51.4%) had an ischemic stroke and 53 (48.6%) had a hemorrhagic stroke. Aspiration pneumonia 93(85.3%) and increased intracranial pressure 91 (83.4%) were the most frequently documented causes of death secondary to stroke. The most common complication during hospitalization was aspiration pneumonia (42.8%), and ICP/brain edema (34.2%) (Table 4).
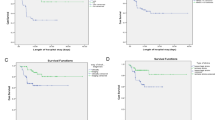
Overall survival rate of stroke patients
The study samples were followed for a minimum of 1 day and a maximum of 60 months with an estimated median survival time of 17 (95% CI: 13.8–20.1) months and an estimated mean survival time of 20.09 (95% CI: 17.3–22.8) months. The survival probability was highest in the first month of follow-up after a stroke was diagnosed, and then it relatively decreased as the follow-up time increased (Fig. 2).
Factors associated with in-hospital mortality
In the bivariable Cox regression analysis, eight variables were identified at a P-value of ≤ 0.25, and considered for multivariable analysis. In the multivariable Cox regression analysis, three variables; age greater than 65 years (AHR = 4.71, 95% CI = 1.11–19.96, p = 0.035), serum creatinine level > 1.2 mg/dl (AHR = 1.54, 95% CI = 1.00-2.39, P = 0.05), and co-morbidity with atrial fibrillation (AHR = 1.48, 95% CI = 1.00-2.21, P = 0.05) were associated with in-hospital mortality from stroke (Table 5).
Pharmacotherapy regimens of hospitalized stroke patients
Aspirin and atorvastatin, which were given to around 67.1% and 63.3% of the patients, respectively, were the most frequently utilized antiplatelet and lipid-lowering medications while the patients were hospitalized. Antihypertensive medications; enalapril and hydrochlorothiazide were used among 37.7% and 24.3% of stroke patients, respectively. In 49.1% of hospitalized stroke patients, antibiotics (ceftriaxone and metronidazole) were also given concurrently for the management of stroke consequences and comorbid diseases, primarily for the treatment of aspiration pneumonia and sepsis (Table 6).
Discussion
The finding of this study showed an overall in-hospital mortality rate of 27.6%. Age greater than 65 years, serum creatinine level greater than 1.2 mg/dl, and co-morbidity with atrial fibrillation were factors associated with in-hospital mortality from stroke.
The magnitude of in-hospital mortality was 27.6%. This was comparable with the study done in Namibia (26.4%) [25], Ethiopia (23.5%) [22], Nigeria (23.8%) [26], and Zimbabwe (24.9%) [27]. However, it was higher as compared to the study done in different regions of Ethiopia; Nekemte (6%) [23], Gondar (12%) [24], and Felege Hiwot Hospital (15.2%) [9]. However, lower than the study conducted in Gambia (57%) [28], Zambia (40.4%) [29], Ghana (43%) [30], Mozambique (33.3%) [31], Jimma, Ethiopia (37.57%) [18], St. Paul’s Teaching Hospital, Ethiopia (30.1%) [32], Nigerian teaching hospital (35%) [33], and Sierra Leoneans (34.8%) [34].
In general, the variability between these research outcomes (in-hospital mortality) might attributed to differences in study designs, geographical areas, and study population. This study was retrospective employing secondary data that account for accessing decreased sample size fulfilling inclusion criteria compared with prospective designs and primary data which enable more case finding and interventions [35]. Besides, geographical areas/ residency for the population, as well as the health care facility, also account for inconsistency. Studies showed evidence of an association between worse health outcomes the further a patient lived from the healthcare facilities they needed to attend [36]. In addition, the imbalanced distribution of health personnel can contribute to great disparities in health outcomes between rural and urban populations [37]. Urban areas are more attractive to healthcare professionals for their comparative social, cultural, and professional advantages [38]. Moreover, social and demographic variability are there across regions which could be independent predictors of nonuniform outcomes [39]. This is why pharmacoepidemiological and post-marketing surveillance are advocated to evaluate treatment outcomes in various populations [40].
In this study, stroke patients over the age of 65 years had almost five times the risk of dying than those under the age of 45 years old. The finding is in line with the previous studies in Pelopidas Silveira, United States [41], Kenya [42], Nigeria [33], Beirut [15], Jimma [20], and Felege Hiwot [9]. This might be related to aging, in which blood vessels become less flexible and more prone to damage [43]. This can lead to the buildup of fatty deposits in the arteries, which can cause blockages and increase the risk of stroke mortality. In addition, older people are more likely to have other comorbid conditions, in this study 40% (n = 158) were > 65 age with comorbidities, such as high blood pressure, diabetes, and heart disease which complicate clinical management and result in poor health outcomes. The unfavorable effects of medication, intoxication, and low progression of disease are more likely in older patients [44].
In the present study, another factor associated with in-hospital mortality from stroke is serum creatinine level. Accordingly, the risk of dying is higher among patients with serum creatinine levels greater than 1.2 mg/dl by about 54% when compared to patients with serum creatinine levels of less than 1.2 mg/dl. The result is consistent with other studies in Burkina Faso [45], Gondar [24], Bahir Dar [9], Sub-Saharan Africa [16] and Addis Ababa [46]. This may be due to an increased risk of cardiovascular disease mortality that increases the risk of cerebrovascular disease mortality. The interaction between different coagulation system components (coagulation cascade, platelets, and vessel wall) is markedly disturbed in patients with renal failure. Proteinuria in renal failure patients leads to the loss of endogenous anticoagulants like antithrombin, protein C, and protein S which leaves the coagulation pathway unchecked, resulting in thrombosis in deep veins and arteries throughout the body [47]. Patients with renal failure are prone to have other medical co-morbidities and in-hospital complications such as pneumonia, deep venous thrombosis, urinary tract infection, and sepsis that increase mortality risk [47].
The rate of in-hospital mortality was higher by 48% among stroke patients with co-morbidity of atrial fibrillation. The result agrees with those of other research conducted in Brazil [48], Beirut [15], and Burkina Faso [45]. Atrial fibrillation raises the risk of blood clot formation in the heart, which further increases the mortality rate from cardioembolic stroke [49]. This may be due to thromboembolism, a serious complication of atrial fibrillation that occludes cerebral arteries.
Strength and limitation of the study
This study has offered insight to understand the present state of in-hospital mortality and its contributing factors among hospitalized stroke patients with a generalizable sample size. However, due to the incompleteness of patient medical information, some important factors that might have a significant association with stroke mortality such as medication adherence, physical exercise, and educational status could not be found on the medical cards and were not assessed. As a hospital-based study, it may not reflect the true burden and outcome of stroke in our community as patients with critically acute stroke may die before hospitalization while relatively mild stroke patients may not be present in the hospital as well.
Conclusion and recommendation
In this study, more than a quarter of hospitalized stroke patients have died. This mortality was high and more likely increased among the patients with age greater than 65 years, serum creatinine level greater than 1.2 mg/dl, and co-morbidity of atrial fibrillation. Hence, these high-risk patients need to be identified, closely followed and aggressively treated to reduce mortality risks. Standard tools/scores (National Institute of Health Stroke Scale and Modified Rankin Scale ) that quantify stroke severity and disability have to be integrated into follow-up care. Further prospective research should be conducted to investigate the problem in-depth.
Data availability
All data supporting the findings of this study are available within the paper.
Abbreviations
- WHO:
-
World Health Organization
- UFH:
-
Unfractionated Heparin
- TIA:
-
Transient Ischemic Attack
- SS:
-
Sub-Saharan Africa
- R-TPA:
-
Recombinant Tissue Plasminogen Activator
- MRS:
-
Modified Rankin Scale
- MRI:
-
Magnetic Resonance Imaging
- LMIC:
-
Low Middle-Income Countries
- HS:
-
Hemorrhagic Stroke
- HRQoL:
-
Health-Related Quality Of Life
- HFCSUH:
-
Hiwot Fana Comprehensive Specialized University Hospital
- GCS:
-
Glasgow Coma Scale
- GBD:
-
The Global Burden Of Disease
- DM:
-
Diabetes Mellitus
- DALY:
-
Disability-Adjusted Life Years
- CT:
-
Computed Tomography
- ASA:
-
America Stroke Association
- AHA:
-
America Heart Association
- JGH:
-
Jugal General Hospital
References
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–418.
Daswani Bharti RM, Deepika N, Phate, Sagar D. Study of drug utilization and outcomes in stroke patient in a tertiary care hospital. 2021.
Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, Creager MA, Eckel RH, Elkind MSV, Fornage M. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(12):3754–832.
Deljavan R, Farhoudi M, Sadeghi-Bazargani H. Stroke in-hospital survival and its predictors: the first results from Tabriz Stroke Registry of Iran. Int J Gen Med. 2018;11:233.
Uwishema O, Berjaoui C, Correia IFS, Anis H, Karabulut E, Essayli D, Mhanna M, Oluyemisi A. Current management of acute ischemic stroke in Africa: a review of the literature. Eur J Neurol. 2022.
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, Abbasifard M, Abbasi-Kangevari M, Abd-Allah F, Abedi V. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820.
Akinyemi RO, Ovbiagele B, Adeniji OA, Sarfo FS, Abd-Allah F, Adoukonou T, Ogah OS, Naidoo P, Damasceno A, Walker RW. Stroke in Africa: profile, progress, prospects and priorities. Nat Reviews Neurol. 2021;17(10):634–56.
Gadisa DA, Busawa GB, Gebremariam ET, Tefera GM, Belete KT, Taye GM, Meskele LB, Gudeta BM, Gelaw BK. Clinical characteristics, treatment outcomes, and its predictors among hospitalized stroke patients in Ambo University Referral Hospital, West Ethiopia: a Retrospective Hospital-based study. Vasc Health Risk Manag. 2020;16:591.
Walelgn N, Abyu GY, Seyoum Y, Habtegiorgis SD, Birhanu MY. The Survival Status and predictors of Mortality among Stroke patients at North West Ethiopia. Risk Manage Healthc Policy. 2021;14:2983–94.
Alene M, Assemie MA, Yismaw L, Ketema DB. Magnitude of risk factors and in-hospital mortality of stroke in Ethiopia: a systematic review and meta-analysis. BMC Neurol. 2020;20:1–10.
Hagos Gufue Z, Gizaw NF, Ayele W, Yifru YM, Hailu NA, Welesemayat ET, Tsegay EW, Atsbaha AH, Gebru HT. Survival of stroke patients according to hypertension status in Northern Ethiopia: seven years retrospective cohort study. Vasc Health Risk Manag. 2020:389–401.
Abera SF. Epidemiology and social determinants of chronic diseases attributed adult mortality and its influence on maternal and young child nutrition in Tigray, 2009–2015: evidence from Kilte Awlaelo-Health and Demographic Surveillance Site. Dissertation, Hohenheim, Universität Hohenheim. 2024.
Mosisa W, Gezehagn Y, Kune G, Chego M, Yigezu HF, Getnet M. Survival status and predictors of mortality among adult stroke patients admitted to Jimma University Medical Center, South West Ethiopia: a retrospective cohort study. Vasc Health Risk Manag. 2023;19:527–41.
Baye M, Hintze A, Gordon-Murer C, Mariscal T, Belay GJ, Gebremariam AA, Hughes CML. Stroke characteristics and outcomes of adult patients in Northwest Ethiopia. Front Neurol. 2020;11:428. https://doi.org/10.3389/fneur.2020.00428
Abdo R, Abboud H, Salameh P, El Hajj T, Hosseini H. Mortality and predictors of death poststroke: data from a Multicenter prospective cohort of Lebanese stroke patients. J Stroke Cerebrovasc Diseases: Official J Natl Stroke Association. 2019;28(4):859–68.
Mohammed AS, Degu A, Woldekidan NA, Adem F, Edessa D. In-hospital mortality and its predictors among stroke patients in sub-saharan Africa: a systemic review and meta-analysis. SAGE open Med. 2021;9:20503121211036789.
JGH H. Annual report. In.: Hiwot Fana Comprehensive Specialized Hospital and Jugal General Hospital. 2020.
Beyene DT, Asefa H. A two year retrospective cross-sectional study on prevalence, associated factors and treatment outcome among patients admitted to medical ward (stroke unit) at Jimma University Medical Center, Jimma, South West, Ethiopia, 2018. Palliat Med Care. 2018;5(4):1–6.
Temesgen TG, Teshome B, Njogu P. Treatment outcomes and associated factors among hospitalized stroke patients at Shashemene Referral Hospital, Ethiopia. Stroke research and treatment. 2018;2018.
Zewudie AZ, Regasa T, Hambisa S, Nureye D, Mamo Y, Aferu T, Feyissa D, Yosef T. Treatment Outcome and Its Determinants among Patients Admitted to Stroke Unit of Jimma University Medical Center, Southwest Ethiopia. Stroke research and treatment. 2020;2020.
Abdella SG, Gebi NB, Gerffie ES, Tamirat KS. Clinical profile, in-hospital outcome and associated factors of stroke after the start of a standard organized stroke care unit at university of Gondar hospital, northwest Ethiopia. Research square. 2019.
Beyene N, Fanta K, Tatiparthi R. Pharmacotherapy Pattern and Treatment outcomes of Stroke patients admitted to Jimma University Medical Center, Ethiopia. Patient Relat Outcome Measures. 2021;12:267.
Fekadu G, Adola B, Mosisa G, Shibiru T, Chelkeba L. Clinical characteristics and treatment outcomes among stroke patients hospitalized to Nekemte referral hospital, western Ethiopia. J Clin Neurosci. 2020;71:170–6.
Gebreyohannes EA, Bhagavathula AS, Abebe TB, Seid MA, Haile KT. In-hospital mortality among ischemic stroke patients in Gondar University Hospital: a retrospective cohort study. Stroke research and treatment. 2019.
Neshuku SN, Kirchner-Frankle J, Nangolo M, Moses M, Einbeck CO, Kumire P, Zatjirua V, Banda J. The Burden and In-Hospital Mortality of Stroke Admissions at a Tertiary Level Hospital in Namibia: A Retrospective Cohort Study. Stroke research and treatment. 2023.
Desalu OO, Wahab KW, Fawale B, Olarenwaju TO, Busari OA, Adekoya AO, Afolayan JO. A review of stroke admissions at a tertiary hospital in rural Southwestern Nigeria. Ann Afr Med. 2011;10(2).
Kaseke F, Stewart A, Gwanzura L, Hakim J, Chikwasha V. Clinical characteristics and outcomes of patients with stroke admitted to three tertiary hospitals in Zimbabwe: a retrospective one-year study. Malawi Med J. 2017;29(2):177–82.
Walker RW, Rolfe M, Kelly PJ, George MO, James OFW. Mortality and recovery after stroke in the Gambia. Stroke. 2003;34(7):1604–9.
Nutakki A, Saylor D, Chishimba L, Chomba M, Mataa M, Zimba S. PREDICTORS OF STROKE MORTALITY AT UNIVERSITY TEACHING HOSPITAL IN LUSAKA, ZAMBIA. J Stroke Cerebrovasc Dis. 2022;31(4):106359.
Agyemang C, Attah-Adjepong G, Owusu-Dabo E, Aikins ADG, Addo J, Edusei AK, Nkum BC, Ogedegbe G. Stroke in Ashanti region of Ghana. Ghana Med J. 2012;46(2):12–7.
Damasceno A, Gomes J, Azevedo A, Carrilho C, Lobo V, Lopes H, Madede T, Pravinrai P, Silva-Matos C, Jalla S. An epidemiological study of stroke hospitalizations in Maputo, Mozambique: a high burden of disease in a resource-poor country. Stroke. 2010;41(11):2463–9.
Gedefa B, Menna T, Berhe T, Abera H. Assessment of risk factors and treatment outcome of stroke admissions at St. Paul’s teaching hospital, addis ababa, Ethiopia. J Neurol Neurophysiol. 2017;8(3):1–6.
Ekeh B, Ogunniyi A, Isamade E, Ekrikpo U. Stroke mortality and its predictors in a Nigerian teaching hospital. Afr Health Sci. 2015;15(1):74–81.
Russell JBW, Charles E, Conteh V, Lisk DR. Risk factors, clinical outcomes and predictors of stroke mortality in Sierra leoneans: a retrospective hospital cohort study. Annals Med Surg. 2020;60:293–300.
Nagurney JT, Brown DFM, Sane S, Weiner JB, Wang AC, Chang Y. The accuracy and completeness of data collected by prospective and retrospective methods. Acad Emerg Med. 2005;12(9):884–95.
Kelly C, Hulme C, Farragher T, Clarke G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open. 2016;6(11):e013059.
Dussault G, Franceschini MC. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4(1):12.
Van Lerberghe W, Conceicaõ C, Van Damme W, Ferrinho P. When staff is underpaid: dealing with the individual coping strategies of health personnel. Bull World Health Organ. 2002;80:581–4.
Reistetter TA, Karmarkar AM, Graham JE, Eschbach K, Kuo Y-F, Granger CV, Freeman J, Ottenbacher KJ. Regional Variation in Stroke Rehabilitation outcomes. Arch Phys Med Rehabil. 2014;95(1):29–38.
Langagergaard V, Palnum KH, Mehnert F, Ingeman A, Krogh BR, Bartels P, Johnsen SP. Socioeconomic Differences in Quality of Care and Clinical Outcome after Stroke. Stroke. 2011;42(10):2896–902.
de Oliveira ADP, de Andrade-Valença LPA, Valença MM. Factors associated with in-hospital mortality in very elderly patients with ischemic stroke: a cohort study. J Stroke Cerebrovasc Dis. 2019;28(10):104281.
Kaduka L, Muniu E, Oduor C, Mbui J, Gakunga R, Kwasa J, Wabwire S, Okerosi N, Korir A, Remick S. Stroke mortality in Kenya’s public tertiary hospitals: a prospective facility-based study. Cerebrovasc Dis Extra. 2018;8(2):70–9.
Nicholson M, Chan N, Bhagirath V, Ginsberg J. Prevention of venous thromboembolism in 2020 and Beyond. J Clin Med. 2020;9(8).
Anderson FA Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):19–16.
Labodi LD, Kadri C, Valentin YN, Christian N, Jean KB. Intra-hospital mortality of stroke and its predictive factors in a reference hospital in Ouagadougou, Burkina Faso. Brain. 2017;1(3):1–6.
Seifu L, Gashaye Y, Taye M. Renal dysfunction among stroke patients, Hospital Based Cross Sectional Study, Addis Ababa, Ethiopia, 2021. Ethiop J Health Dev. 2023;37(1).
Khatri R, Afzal MR, Qureshi MA, Maud A, Huanyu D, Rodriguez GJ. Pre-existing renal failure increases in-hospital mortality in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2019;28(2):237–42.
Moraes MA, Jesus PAPd, Muniz LS, Costa GA, Pereira LV, Nascimento LM, Teles CAS, Baccin CA, Mussi FC. Ischemic stroke mortality and time for hospital arrival: analysis of the first 90 days. Revista Da Escola De Enfermagem Da USP. 2023;57:e20220309.
Alberts M, Chen Y-W, Lin JH, Kogan E, Twyman K, Milentijevic D. Risks of stroke and mortality in Atrial Fibrillation patients treated with Rivaroxaban and Warfarin. Stroke. 2020;51(2):549–55.
Acknowledgements
We would like to thank the management and card room staff at HFCSUH and JGH for their cooperation during data collection.
Funding
The authors disclosed receiving financial support from Haramaya University for conducting this research work (for data collection).
Author information
Authors and Affiliations
Contributions
ZA, TG, AJ and DE contributed to the conception, design, and statistical analysis. ZA and AJ contributed to data collection and manuscript drafting. TG and DE supervised the study. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Ethical clearance was obtained from Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee with the reference number of IHRERC/177/2022. A written information sheet that explained the study was provided to the Medical Director of HFCSUH, JGH, and informed, voluntary, written, and signed consent was obtained. Then officials at different levels in the hospital communicated through formal letters. The information collected in this study was kept confidential. The patient names were not indicated. Only medical record numbers were used for identification. Data collectors were informed and trained to preserve information confidentiality; they reported the data only to the investigator, and the collected data was used only for the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Abas, Z., Gashaw, T., Jambo, A. et al. In-hospital mortality and its associated factors among hospitalized stroke patients at public hospitals of Eastern Ethiopia. BMC Cardiovasc Disord 24, 456 (2024). https://doi.org/10.1186/s12872-024-04106-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-04106-4