Abstract
Background
Obesity and hypertension are major risk factors for cardiovascular diseases that affect millions of people worldwide. Both conditions are associated with chronic low-grade inflammation, which is mediated by adipokines such as adiponectin. Adiponectin is the most abundant adipokine that has a beneficial impact on metabolic and vascular biology, while high serum concentrations are associated with some syndromes. This “adiponectin paradox” still needs to be clarified in obesity-associated hypertension. The aim of this study was to investigate how adiponectin affects blood pressure, inflammation, and metabolic function in obesity hypertension using a Chinese adult case-control study.
Methods
A case-control study that had finished recruiting 153 subjects divided as four characteristic groups. Adiponectin serum levels were tested by ELISA in these subjects among these four characteristic Chinese adult physical examination groups. Waist circumference (WC), body mass index (BMI), systolic blood pressure (SB), diastolic blood pressure (DB), and other clinical laboratory data were collected. Analyzation of correlations between the research index and differences between groups was done by SPSS.
Results
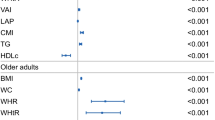
Serum adiponectin levels in the| normal healthy group (NH group) were significantly higher than those in the newly diagnosed untreated just-obesity group (JO group), and negatively correlated with the visceral adiposity index. With multiple linear egression analysis, it was found that, for serum adiponectin, gender, serum albumin (ALB), alanine aminotransferase (ALT) and high-density lipoprotein cholesterol (HDLC) were the significant independent correlates, and for SB, age and HDLC were the significant independent correlates, and for DB, alkaline phosphatase (ALP) was the significant independent correlate. The other variables did not reach significance in the model.
Conclusions
Our study reveals that adiponectin’s role in obesity-hypertension is multifaceted and is influenced by the systemic metabolic homeostasis signaling axis. In obesity-related hypertension, compensatory effects, adiponectin resistance, and reduced adiponectin clearance from impaired kidneys and liver all contribute to the “adiponectin paradox”.
Similar content being viewed by others
Introduction
Obesity, having an inexorable rise with over 650 million obese worldwide [1], is globally a significant public health challenge and accounts for 65–78% of cases of primary hypertension [2]. The pathways through which obesity causes hypertension are complicated, including sympathetic nervous system overactivation, stimulation of the renin-angiotensin-aldosterone system, alterations in adipose-derived cytokines, insulin resistance, and structural and functional renal changes [2]. Adipose tissue is one of the largest endocrine organs in the body playing multiple intricate roles including secretion of a number of biologically adipokines, of which the most abundant is adiponectin [1].
Adiponectin, a 28-kDa protein adipocytokine, mainly produced and secreted into the circulation by lean adipocytes [3, 4], has been very widely studied, over the past 25 years, since mid-1990s [5]. The primary function of adiponectin is the regulation of carbohydrate and lipid metabolism [6]. However, the full extent of its biological action remains to be elucidated, with a variety of effects on different cell and tissue types [3, 7]. Adiponectin is initially considered a guardian angel adipocytokine owing to its protective functions against various disease states associated with obesity, such as immune modulatory, insulinsensitizing, antidiabetic, antiobesogenic, antiinflammatory, antiatherogenic, anti-fibrotic, cardio and neuroprotective properties [3, 4, 7]. Adeno-viral over-expression of adiponectin in obese KKAy/a mice resulted in reduced blood pressure and reversed salt-induced hypertension [8]. Contrariwise to its protective effects against various pathological events in different cell types, adiponectin may have links to several systemic diseases and malignancies [1]. Accumulating reports of results of several meta-analyses demonstrated that elevated serum levels of both total and High Molecular Weight (HMW) adiponectin have been positively associated with both cardiovascular and, what is quite surprising and confusing, even with the all-cause mortality rate in the population above 65 years of age [9]. The biology underlying this paradox is still being studied [9].
This “adiponectin paradox” is remained, when coming to the role of adiponectin in hypertension. On one hand, compared to the patients with essential hypertension, adiponectin plasma levels were found to be significantly higher in the normotensive subjects [1, 10]. And lower adiponectin levels were associated higher blood pressure or with incident hypertension [11,12,13,14]. These phenomena may be due to their protecting role on vascular functions through improving the functions of macrophages and endothelial cells. These mechanisms may include attenuating the phenotype of macrophages M1 and to promote the phenotype of macrophages M2 and preventing endothelial dysfunction through enhancing endothelial nitric oxide synthase (eNOS) activity and nitric oxide (NO·) production via adiponectin receptors AdipoR1/R2-AMPK (Adenosine 5′-monophosphate (AMP)-activated protein kinase)-endothelial signaling and cyclooxygenase-2 (COX-2) expression and prostaglandin I2 (PGI2) production by means of calreticulin/CD91-dependent Akt (protein kinase B) signaling [15]. And adiponectin also can lower blood pressure by decreasing renal sympathetic nervous system activity through its short-lived action on brain in adiponectin knock-out mice [15,16,17,18,19,20,21].
On the other hand, chronic intracerebroventricular infusion of adiponectin did not alter blood pressure in normotensive or hypertensive rats [10, 22]. And Sprague-Dawley rats fed a high salt diet exhibited hypertension associated with elevated levels of adiponectin, suggesting that adiponectin does not play a protective role against salt-induced hypertension [20, 23]. Adiponectin KO mice developed hypertension without insulin resistance when maintained on a high-salt diet, indicating that hypoadiponectinemia, per se, is not sufficient for the development of hypertension but contributes to its development under insulin resistance and/or salt overload [8]. In normotensives and untreated hypertensives with normal kidney function, adiponectin is not associated with blood pressure even after adjustment for many risk factors [24]. Several longitudinal studies offer mixed insights into adiponectin’s influence on metabolic diseases like hypertension, with some linking high levels to reduced metabolic syndrome risk and others to increased mortality and no protection against hypertension [11, 13, 25,26,27,28,29]. These studies highlight the complexity of adiponectin’s role in metabolic health and the need for further research to clarify its impact. This study aimed to provide more clues for distinguishing the antinomy of adiponectin in obesity hypertension.
Data and methods
Study design and participants
This was a case-control study involving 153 Chinese adults (aged 40.78 ± 11.77 years; 119 men, 34 women) who underwent annual physical examinations in a hospital from September 2012 to July 2014 [30]. The participants were divided into four groups based on their body mass index (BMI) and blood pressure: the normal healthy (NH) group, the newly diagnosed untreated just-obesity (JO) group, the newly diagnosed untreated just-hypertension (JH) group, and the newly diagnosed untreated obesity-hypertension (OH) group. The inclusion and exclusion criteria for each group were set as previously reported [30,31,32,33,34] and are shown in Table 1. The number of subjects included in each group is also shown in this table. BMI was obtained by dividing the body weight by the square of the respective subject’s height (weight/height2 (kg/m2)) .
This study followed the Declaration of Helsinki and received approval from the Hangzhou Center for Disease Control and Prevention’s ethical committee. All participants agreed to join this study and signed a free and informed consent form [30,31,32,33,34].
Measurement protocol
The participants’ weight, height, waist circumference (WC) were measured according to standard protocols as previously described [30,31,32,33,34]. Before the measurement, the participants removed their shoes, heavy clothing, belts, and any other items that could interfere with the waist circumference (WC) measurement [35]. The WC was measured at the midpoint between the lower rib margin and the iliac crest while the participants gently exhaled [36].
General Obesity was defined as BMI ≥ 28 kg/m2 and central obesity was defined as WC ≥ 85 cm for males and ≥ 80 cm for females according to the definition created by the Chinese Obesity Working Group [30,31,32,33,34]. In the present study, BMI was used to identify obesity, i.e., the general obesity was used to define the subject groups [37, 38]. The visceral adiposity index (VAI) was calculated using a formula that incorporates WC, BMI, triglyceride (TG), and high-density lipoprotein cholesterol (HDLC) levels, i.e.,VAImen = [WC/(39.68 + 1.88 × BMI)] × (TG/1.03) × (1.31/HDLC); VAIwomen = [WC/(36.58 + 1.89 × BMI)] × (TG/0.81) × (1.52/HDLC) [39, 40].
The blood pressure is considered a good indicator of the status of the cardiovascular system. The blood pressure can be measured by direct intraarterial and indirect sphygmomanometer methods [41]. In this study, all participants had blood pressure measured using indirect method with electronic sphygmomanometer (HEM-4021, Omron, Kyoto, Japan) [42, 43]. Blood pressure was measured after at least 10 minutes of rest in a seated position using a standard protocol [44]. And the subject should avoid smoking, drinking caffeine, or exercising within 30 minutes of the test [45]. The inflatable cuff of the sphygmomanometer wrapped around the right upper arm at the same level as the heart and the arm was supported on a flat surface [46, 47]. Three measurements were taken with 5 to 15 minutes intervals and the average of three such systolic and diastolic blood pressure readings was taken as the examination blood pressure for the further analysis [44].
Hypertension was defined according to the recommendation of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure and the World Health Organization–International Society of Hypertension as a systolic blood pressure of 140 mmHg or higher and/or a diastolic blood pressure of 90 mmHg or higher at each of the three appointments [44, 48, 49].
Serum adiponectin level and other metabolic parameters
The routine clinical laboratory tests were carried out on the subjects’ blood and urine samples. Blood samples were collected after an overnight fast and frozen for later analysis. Serum adiponectin level was quantified using a commercially available ELISA kit that measures the total adiponectin concentration (including all isoforms) [31, 50]. According to the anamnesis and other clinical records, general demographic data, such as age and gender, as well as some biochemical parameters (see Table 2), were obtained [30,31,32,33,34].
Statistical analysis
R software (https://www.r-project.org) and SPSS for Windows V22.0 (IBM Corp., Armonk, NY) were used to perform the statistical analyses. The median and the interquartile range (P25, P75) were reported as descriptive statistics. Pearson’s test were applied to assess the associations between groups when the data (or transformed data) met the normality and equal variance assumptions; otherwise, the Mann–Whitney rank sum test and Spearman’s correlation test were used. The tested index among the four subgroups were compared using the rank-sum or T-test. Logistic regression, partial correlation or Fisher exact test were also employed when appropriate. The significance level at 0.05 was set for two-sided tests. Multiple regression models were fitted to study the independent association of the study variables with serum adiponectin, and SB (or DB).
Results
Characteristics
The table 2 shows the baseline characteristics of the subjects in the four groups, including their general and anthropometric data and biochemical parameters. The table presents the median, the quartiles (P25, P75), and the number of the following variables: GGT, ALB, ALT, LDLC, TG, HDLC, FA, SCR, IB, ALP, CB, GLU, TC, TB, TP, Ua, UREA, age, gender, and WC, BMI, SB, and DB. The full names of these indicators can be found in the notes below the Table 2.
The relationship between VAI and serum concentrations of adiponectin
The median (P25, P75) of VAI and serum adiponectin levels of the four groups are shown in Table 2.
After adjustment for gender and age, analysis of covariance (ANCOVA) revealed that the serum adiponectin level in the NH group was significantly higher than in the JO groups (P = 0.036). No significant differences of the serum adiponectin between other two groups. The order of serum adiponectin levels among the groups was NH > OH > JH > JO.
The difference of VAI between NH group and JO group (or the OH group) is statistically significant (P < 0.05) after adjusting for gender and age. The VAI of NH group is the smallest among the four subgroups. The difference of VAI between NH group and JO group is nearly statistically significant (P = 0.071). The P-value for the comparison of VAI between JO and OH groups was 0.376, which means that the difference was not statistically significant after adjustment for gender and age.
And, after adjustment for gender and age, partial correlation analysis revealed that serum adiponectin had a negative association with VAI that was trending towards significance (P = 0.055, r = − 0.157). All the data were log-transformed to follow a normal distribution before analysis.
Multiple regression models for the independent association of the study variables with serum adiponectin
A linear regression model towards serum adiponectin is shown in Table 3 (R2 = 0.314). Gender, ALB, ALT and HDLC were found to be independent determinants. The other variables did not reach significance in the model (P > 0.1). This model was responsible for 31.4% of the original variation of the serum adiponectin.
The difference of serum adiponectin levels between genders in the four group
Table 4 shows the comparisons of the serum adiponectin levels between genders in the four groups of subjects: JO, OH, JH, and NH. The table presents the median and the interquartile range of the serum adiponectin levels for each group and gender. The table also reports the P-values of the differences between males and females within each group. The results indicate that after the age was controlled, the serum adiponectin levels were significantly higher in females than in males in the OH and NH groups, but not in the JO and JH groups. This suggests that there is a sexual difference in the serum adiponectin levels, which may be influenced by the presence or absence of obesity and hypertension.
Multiple regression models for the independent association of the study variables with SB and DB
The linear regression models towards SB and DB are shown in Table 5 (R2 = 0.333) and Table 6(R2 = 0.230), respectively. For SB, age and HDLC were found to be independent determinants, and ALB was borderline significant. ALP barely escaped statistical significance The other variables did not reach significance in the model (P > 0.08). This model was responsible for 33.3% of the original variation of the SB serum adiponectin. For DB, ALP was found to be the independent determinant, and age had a considerable trend toward significance.
Discussion
Adiponectin is primarily produced and released by energy-storing cells in adipose tissue (body fat) called adipocytes [51,52,53,54,55]. Yet, other tissues and other types of cells can produce adiponectin, including osteoblasts, myocytes, heart muscle cells, liver parenchyma cells,endothelial cells and placental tissue [51,52,53,54,55,56,57,58,59,60,61]. Adiponectin is known as the most abundant adipokine and its paradoxical elevation in some disorders is receiving more attention [62,63,64]. Adeno-viral over-expression of adiponectin in genetically obese KKAy/a mice with obesity-related hypertension resulted in reduced blood pressure [8]. However, normal wild-type mice and mice with specific genetic backgrounds may exhibit different mechanisms for obesity-related hypertension and may also show varying roles of adiponectin in the context of this condition [65, 66].
This study investigated the role of adiponectin in obesity-hypertension by measuring its serum levels and correlations with various parameters in four groups of Chinese adults: NH, JO, JH, and OH.
Though adiponectin is mainly secreted by adipose tissue (AT), its circulating concentration is decreased in obesity [51,52,53,54,55]. The results in this study also demonstrated that the serum adiponectin level in the NH group is significantly higher than in the JO group. AT can broadly be divided into two types with distinct roles: white AT (WAT) and brown AT (BAT) [56, 67]. BAT has smaller lipid droplets and more blood vessels than WAT, resulting in a darker, brown macroscopic look [68, 69]. And beige adipose tissue, a type of inducible BAT, intermingles with WAT depots and occurs in response to cold exposure and pharmacological modulation of WAT [70,71,72]. This phenomenon of decreased serum adiponectin level in obese people might be attributed to fat cell dysfunction and/or hypermethylation of the adiponectin gene in morbid obesity [73, 74]. Some previous literature also shows that the adiponectin paradox, which refers to the paradoxical elevation of adiponectin in some disorders, is more evident in non-obese than in obese patients with diabetic microvascular complications [75]. The authors suggested that the paradoxical elevation of adiponectin in vascular damage might be a compensatory response, and that the responsive upregulation might be insufficient in obese patients [75]. Previous studies revealed that the quality of adipose tissue is largely compromised in patients with severe cardiovascular disorders [76, 77]. Additionally, during caloric restriction (CR), increased circulating adiponectin is observed to come from bone marrow adipose tissue (MAT) [78, 79].
And, it was found in this study that serum adiponectin levels negatively correlated with VAI. VAI is a mathematical formula that estimates the amount and function of visceral adipose tissue (VAT), which is the fat that surrounds the internal organs in the abdomen [80,81,82,83]. WAT can be divided into two major depots: VAT and subcutaneous adipose tissue (SAT). SAT is located under the skin. The distribution of WAT affects the production and function of adiponectin [84, 85]. Generally, VAT is associated with lower adiponectin levels and higher risk of metabolic and cardiovascular complications, such as diabetes, hypertension, and atherosclerosis [86,87,88]. This is because VAT is more prone to inflammation, insulin resistance, and lipolysis, which can impair adiponectin secretion and action [86,87,88]. On the other hand, SAT is mainly considered to be associated with higher adiponectin levels and lower risk of metabolic diseases [89, 90], though with the oppsite results exsiting [91]. This is because SAT is more responsive to insulin, has anti-inflammatory properties, and can store excess lipids away from harmful sites [92, 93]. However, not all SAT depots are equal. Fat on the lower extremities, such as the legs, is more beneficial than fat on the upper body, such as the abdomen [93, 94]. This is because lower-body fat has higher adiponectin expression and secretion, and can protect against the adverse effects of VAT [84, 94, 95]. Therefore, the role of WAT distribution in adiponectin levels and metabolic health is complex and depends on the location, amount, and function of different fat depots [91, 93, 96, 97]. A better understanding of the molecular mechanisms that regulate adipocyte differentiation and adiponectin secretion in different WAT subtypes may lead to new therapeutic strategies for obesity and its related complications [91, 93, 96, 97]. VAI takes into account waist circumference, body mass index, triglycerides, and HDLC levels, and it is different for men and women [80,81,82]. VAI has been shown to be a reliable indicator of visceral fat dysfunction and cardiometabolic risk [98]. VAI seems to represent a better predictive tool than common clinical parameters for metabolic disorders in Chinese and Caucasian samples [82, 99, 100].
And, in this study, we found that the NH group had a much lower VAI than almost all other groups (JO, JH, OH). The JH group also had a lower VAI than the OH group. Previous study reported weekend warrior activity patterns (WWs) and regular activity patterns offer the same benefits for reducing the VAI [101]. This suggests that the NH group and JH group might have higher level of physical activity and a larger proportion of muscle mass in their body weight than the other two groups. Aditionally, the serum adiponectin levels negatively correlated with VAI in this study. These results reflect that serum adiponectin levels positively correlated with physical activity and muscle mass proportion of the body. It has been shown that physical exercise can reduce fat mass [76], especially the accumulation of VAT [102,103,104], and lead to hypersecretion of adiponectin [102,103,104], which results in increased adiponectin production in adipose tissue and enhanced concentration of adiponectin in the blood [105,106,107,108]. Our study result accords with the phenomena discovered in those previous literature.
In this study, the comparison of VAI between JO and OH groups revealed no significant difference. This indicates that the VAI, a marker of visceral adiposity and cardiometabolic risk, was similar between the two groups. However, the increase of the serum adiponectin level in OH compared to JO may seem paradoxical, as adiponectin is generally considered to have anti-obesity and anti-hypertensive effects [9, 109]. Nevertheless, the result was in line with the phenomenon called “adiponectin paradox” in which adiponectin levels are elevated in some pathological conditions, such as cardiovascular disease, diabetes, and chronic kidney disease [76]. This may reflect a compensatory response of the body to maintain metabolic homeostasis and protect against further damage [9, 110]. Moreover, adiponectin levels may be influenced by other factors, such as gender, albumin, alanine aminotransferase, and high-density lipoprotein cholesterol, as we showed in the multiple regression analysis. And the interaction between adiponectin and other adipokines, such as leptin, resistin, and visfatin, should be taken into account [111, 112]. In addition to white adipokines (adipokines produced by WAT), the brown adipokines, adipokines present in brown adipose tissue, such as fibroblast growth factor 21 (FGF21), interleukin-6 (IL-6), neuregulin-4 (NRG4), insulin-like growth factor-1 (IGF-1), and tumor necrosis factor-alpha (TNF-α), may also play a role in the process known as the ‘adiponectin paradox [112, 113]. And these adipokines also have tortuous relationship with hypertension. As shown in previous studies, leptin’s effect on Trpm7 (TRP [transient receptor potential] melastatin 7) expression, via epigenetic changes and the pSTAT3(phosphorylated signal transducer and activator of transcription 3)-JAK2(Janus kinase 2) pathway, contributes to obesity-associated hypertension, but leptin’s role is additive, not essential, in the complex regulatory network leading to hypertension in obesity [33, 114,115,116]. Depending on the context, resistin appears to have both protective and detrimental effects to obesity-related hypertension, highlighting the complexity of resistin’s role in obesity and hypertension [30]. And, IL-6 may have diverse effects in the pathogenesis of obesity and hypertension, depending on the presence or absence of these conditions [34]. Therefore, the role of adiponectin in obesity-hypertension should be considered in the context of the systemic signaling axis and not in isolation [117].
Next, with the multiple regression model, it was found serum adiponectin level was significantly higer in females than in males (with std.β = 0.323). This result is in line with many previously studies, which demonstrate that adiponectin levels are generally higher in females than in males, especially in adulthood [118, 119]. This may be partly explained by the effects of sex hormones, such as testosterone and estrogen, on adiponectin production and secretion [119, 120]. Testosterone has been shown to suppress adiponectin expression in fat cells, whereas estrogen has been shown to stimulate it [120]. Therefore, during puberty, when sex hormones increase, adiponectin levels tend to decline in males and rise in females [119, 121]. However, the sex differences in adiponectin levels are not consistent across different ethnic groups and obesity levels. For example, some studies have found that Hispanic females have lower adiponectin levels than non-Hispanic white females, and that this difference is more pronounced in obese individuals [122,123,124]. And dietary patterns may also affect adiponectin levels and the sex differences in this hormone [125,126,127,128]. Healthy dietary patterns rich in fruits, vegetables, whole grains, fish, nuts, and unsaturated fats are linked to higher adiponectin levels, likely due to their bioactive compounds that promote adipose tissue function and insulin sensitivity [128,129,130,131]. Conversely, unhealthy diets high in red and processed meats, refined grains, sweets, fast foods, and saturated/trans fats correlate with lower adiponectin levels, potentially due to inflammation, oxidative stress, and insulin resistance that hinder adiponectin secretion and activity [128,129,130,131]. And a negative association between the Dietary Approaches to Stop Hypertension (DASH) diet index and VAI was reported among older Americans [132].
And the interaction between diet and genetics may modulate adiponectin levels and metabolic outcomes [133]. For eample, ADIPOQ variants conferred more metabolic risks in healthy dietary patterns than in adverse dietary patterns [133, 134]. And some literature indicated that moderate amounts of ethanol-containing beverages increased adiponectin concentrations, and sex-specific effects might depend on type of beverage consumed [135]. This may suggest that other factors, such as genetic, environmental, or lifestyle factors, may also influence adiponectin levels and modify the sex differences [118, 136,137,138]. In this study, blood samples were obtained after a 12-hour of fasting, which can avoid the short-term effects of the diet. And, after the age was controlled, the serum adiponectin levels were significantly higher in females than in males in the OH and NH groups, but not in the JO and JH groups. This suggests that there is a sexual difference in the serum adiponectin levels, which may be influenced by the presence or absence of obesity and hypertension [139].
According to vast majority of reports, adiponectin has been exhibited to have protective effect on vascular functions and thus has negative relationship with blood pressure, against incidence of obesity-hypertension [21, 140, 141]. But the contrary opinion holds that, in different subject groups, the relationships between the adiponectin and blood pressure are various, with positive and non-correlation existing [24, 142,143,144]. The preclinical expriments, longitudinal studies and clinical trials have reported inconsistent outcomes regarding the antihypertensive effects of adiponectin [11, 13, 25,26,27,28,29, 145]. In this study, using the multiple regression model, it was found that adiponectin was not associated with blood pressure (SB and DB) after adjustment for other risk factors (the anthropometric and biochemical characteristics mentioned in Table 2 ) used in multiple linear regression models. Age and HDLC were found to be independently positively correlate with SB, and ALB was at the edge of significance. ALP were found to be independently positively correlate with DB, and age has a considerable trend toward significance.
This study results revealed that ALB independently negatively and ALT, HDLC, and gender positively associate with serum level of adiponectin. These results were in line with many previous research outcomes. Serum adiponectin levels have been recorded to display a sexual difference, being higher in females than in males [118, 146,147,148], and were observed having inverse correlation with circulating albumin [120, 149, 150]. And recently, higher plasma adiponectin abundance was discovered in albumin knockout (KO) mice [151].
The associations between adiponectin and ALT have been shown to be different. Many research detailed the opposite connections [152,153,154,155], however positive and non-connections are likewise existing [156, 157]. And adiponectin knockout could ablate the significant rise in serum ALT elicited by high-fat diet feeding in mice [158].
Consistent with our study results, the serum HDLC has been reported to be independently positively associated with serum adiponectin in almost all the previous studies [159,160,161,162,163,164,165]. Adiponectin could upregulate ATP-binding cassette transporter A1 and G1 expression and hepatic apo-AI (Apolipoprotein A-I), reduce lipid accumulation, and efficiently promote nascent HDLC formation [166,167,168,169,170,171]. Lower adiponectin (ADIPOQ) gene expression are associated with diabetic dyslipidemia [172, 173].
Accounting for the mentioned above, in this mixed subjects of four Chinese subgroups, adiponectin did not have the dose-response conjunction with the blood pressure after adjustment for potential confounding factors, which was little illustrated in earlier investigations [11]. These conflicting results in different studies may be mostly due to the diversity of subjects included [24]. The direct relationship between adiponectin and hypertension (or blood pressure) may be influenced by many factors, among which the liver and kidney dysfunctions are often mentioned. Disorders of kidney or liver can lead to the elevation of the blood pressure and incident of hypertension [174, 175]. Meanwhile, the impaired liver function can affect adiponectin’s degradation in the liver, and the kidney dysfunctions can reduce renal clearance of adiponectin [174,175,176]. High serum ALT is known to reflect the situation of severe liver disease. In addition, in this study, ALP was found to independently positively correlate with DB and nearly with SB. High levels of ALP in the blood may indicate liver disease or certain bone disorders. Furthermore, in this study, ALB was found to have a negative association with SB that was trending towards significance. Low albumin levels in the blood are known to indicate serious liver and kidney problems.
Another explanation for the increase of adiponectin in individuals with risk towards mortality is that is a failing attempt of the body to do the protection [177], as pathological adiponectin resistance develops with its receptors down regulation in metabolically active organs including the adipose tissue, the heart, the liver and the vasculature [172, 173, 178]. Adiponectin exerts its both beneficial and detrimental effects via normal or impaired signaling through its receptors: Adiponectin receptor 1 and 2 (AdipoR1 and AdipoR2), T-cadherin and calreticulin [1]. Adiponectin exists in various isoforms in the circulation, including trimer (~ 67 kDa; low molecular weight, LMW), hexamer (136 kDa; middle molecular weight, MMW), 12-32mer (> 300 kDa, high molecular weight, HMW), and globular forms [76, 179, 180]. Different adiponectin isoforms bind to different receptors, resulting in various functions. Globular adiponectin preferentially binds to AdipoR1, influencing muscle cells [56]. T-cadherin, a non-transmembrane binding protein, is a key partner for HMW adiponectin, potentially accumulating it in heart, vascular endothelium, and muscle, with its downstream effects being studied [181,182,183]. Αdiponectin may bind to calreticulin on macrophage surfaces and other cells [184, 185]. AdipoR2 binds full-length adiponectin and is predominantly expressed in the liver [186]. However, the relative contributions of different adiponectin isoforms to obesity and hypertension are not fully understood and may vary depending on the population and the disease stage [180].
In general, our research investigated the role of adiponectin in obesity-hypertension using a case-control study with four groups of Chinese adults: normal healthy, just-obesity, just-hypertension, and obesity-hypertension. This design allows for a comprehensive comparison of the serum adiponectin levels and their associations with various anthropometric and biochemical parameters among different subgroups of obesity and hypertension. Thus, this research provided more clues for distinguishing the antinomy of adiponectin in obesity-hypertension by analyzing the correlations between adiponectin and visceral adiposity index, gender, serum albumin (ALB),alanine aminotransferase (ALT) and high-density lipoprotein cholesterol (HDLC), blood pressure, and other indicators. This research also indicated some factors that influence the sex differences in adiponectin. Next, the results of this research suggested that adiponectin may not always have a direct relationship with blood pressure. The importance of adiponectin must be viewed within the framework of the body’s key signaling pathways that regulate metabolic equilibrium in the face of obesity and cardiovascular disorders [187], such as the modulation by other adipokines (leptin, resistin, and visfatin, as well as brown adipokines, such as FGF21, IL-6, NRG4, IGF-1, and TNF-α). This research also indicated the potential mechanisms of adiponectin in regulating carbohydrate and lipid metabolism, inflammation, and vascular function. Furthermore, Different explanations for the adiponectin paradox have been discussed including adiponectin resistance, compensatory effects of adiponectin to subclinical pathologies, impaired renal function and decreased hepatic clearance of adiponectin [188,189,190]. And this research revealed that adiponectin’s role in obesity-hypertension is complex and depends on the systemic metabolic homeostasis signaling axis. And in the end, the results of this research indicated that in the context of obesity-related hypertension, compensatory effects, adiponectin resistance, and decreased adiponectin clearance due to impaired renal and hepatic function occur simultaneously, contributing to the “adiponectin paradox”.
Some limitations and strengths of our study should be addressed. At first, our results need to be interpreted in the context of a few limitations. One limitation is that the cross-sectional design and small sample size of our study and the subjects restricted to Chinese adults may limit the generalizability and causal inference of our findings. Therefore, Our results should be interpreted with caution and should be confirmed by larger, longitudinal studies across various genetic populations in the future. Another limitation is that we did not measure the adiponectin isoforms, which could have provided more nuanced insights into the role of adiponectin in obesity-hypertension. Previous studies have reported conflicting results on the associations of adiponectin isoforms and other adipokines (WAT or BAT adipokines) with blood pressure and metabolic parameters in different populations [56, 112, 179, 180]. Therefore, further studies are needed to investigate the differential effects of adiponectin isoforms on obesity-hypertension and to explore the potential mechanisms underlying the adiponectin paradox. Third limitation is that while the present study attempts to control for various confounders, there are still potential variables that might influence the results, such as dietary patterns, genetic predispositions, and environmental factors. We did not have comprehensive dietary data and we did not delve into the relationship between adiponectin and other adipokines (other BAT adipokines or other WAT adipokines). Finally, the VAI is not a direct and accurate measure of physical activity and that it may not capture the intensity, duration, and type of physical activity that the participants engaged in.
Notwithstanding these limitations, the multiple strengths of our study should be kept in mind. Firstly, the chosen population in the present study allowed us to investigate the role of adiponectin in obesity-hypertension axis in a relatively homogeneous and early-stage group, without the confounding effects of medication or other comorbidities. Secondly, to minimize the effects of diet, blood samples were obtained after a 12-hour fast in the present study to avoid the short-term effects of recent dietary intake. Thirdly, we have controlled for potential confounding factors, such as age, gender, and other biochemical indicators. And the use of multiple regression models adds rigor to the findings, offering insights into the independent determinants of serum adiponectin levels. Fourthly, the Visceral Adiposity Index (VAI), utilized in this study, serves as a comprehensive indicator of physical activity levels [98, 101]. It inversely correlates with physical activity and positively correlates with visceral fat dysfunction and cardiometabolic risk, making it a superior predictive tool for metabolic disorders in both Chinese and Caucasian populations [82, 99, 100]. Fifthly,we believe that our findings may have some relevance and applicability to other populations and settings because of the consistent with some previous studies that have reported no directly associations between adiponectin and blood pressure in different ethnic groups and regions, such as African Americans, Europeans, and Japanese [27, 191, 192]. These studies suggest that the “adiponectin paradox” may be a common phenomenon in obesity-hypertension, regardless of the population characteristics.
In summary, our study findings provide new insights into the “adiponectin paradox”. Adiponectin’s role in obesity-hypertension is multifaceted and is influenced by the systemic metabolic homeostasis signaling axis. In obesity-related hypertension, compensatory effects, adiponectin resistance, and reduced adiponectin clearance from impaired kidneys and liver all contribute to the “adiponectin paradox”.
And to further elucidate the role of adiponectin in obesity-hypertension, more studies are needed to investigate the adiponectin isoforms, the adiponectin receptors, and the signaling pathways involved in different tissues and organs. Moreover, the interactions between adiponectin and other adipokines, hormones, and inflammatory mediators should be explored in the context of obesity-hypertension. Additionally, the genetic, environmental, and lifestyle factors (such as dietary assessments including alcohol intake and direct measurement of physical activity) that influence adiponectin levels and function should be considered [173]. Finally, the therapeutic potential of adiponectin or its analogues for obesity-hypertension should be evaluated in clinical trials.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- WC:
-
Waist circumference
- BMI:
-
Body mass index
- SB:
-
Systolic blood pressure
- DB:
-
Diastolic blood pressure
- HMW:
-
High molecular weight
- eNOS:
-
Endothelial nitric oxide synthase
- NO:
-
Nitric oxide
- AMPK:
-
Adenosine 5’-monophosphate (AMP)-activated protein kinase
- COX-2:
-
cyclooxygenase-2
- PGI2:
-
Prostaglandin I2
- Akt:
-
Protein kinase B
- GGT:
-
Gamma-glutamyltransferase
- ALB:
-
Albumin
- ALT:
-
Alanine aminotransferase
- LDLC:
-
Low density lipoprotein cholesterol
- TG:
-
Triglyceride
- HDLC:
-
High density lipoprotein cholesterol
- FA:
-
Fructosamine
- SCR:
-
Serum creatinine
- IB:
-
Indirect bilirubin
- ALP:
-
Alkaline phosphatase
- CB:
-
Conjugated bilirubin
- UREA:
-
Urea
- Ua:
-
uric acid
- FBG:
-
Fasting blood glucose
- TC:
-
Total cholesterol
- TB:
-
Total bilirubin
- TP:
-
Total protein
- VAI:
-
Visceral adiposity index
- AT:
-
Adipose tissue
- WAT:
-
White adipose tissue
- BAT:
-
Brown adipose tissue
- MAT:
-
Bone marrow adipose tissue
- CR:
-
Caloric restriction
- VAT:
-
Visceral adipose tissue
- SAT:
-
Subcutaneous adipose tissue
- FGF21:
-
Fibroblast growth factor 21
- IL-6:
-
Interleukin-6
- NRG4:
-
Neuregulin-4
- IGF-1:
-
Insulin-like growth factor-1
- TNF-α:
-
Tumor necrosis factor-alpha
- Trpm7:
-
TRP [transient receptor potential] melastatin 7
- JAK2:
-
Janus kinase 2
- pSTAT3:
-
Phosphorylated signal transducer and activator of transcription 3
- apo-AI:
-
Apolipoprotein A-I
- LMW:
-
Low molecular weight
- MMW:
-
Middle molecular weight
- AdipoR1:
-
Adiponectin receptor 1
- AdipoR2:
-
Adiponectin receptor 2
- DASH:
-
Dietary approaches to stop hypertension
- WWs:
-
Weekend warrior activity patterns
- ANCOVA:
-
Analysis of covariance
- ABCA1:
-
ATP-binding cassette transporter A1
- ABCG1:
-
ATP-binding cassette transporter G1
- KO:
-
Knockout
References
Shklyaev SS, Melnichenko GA, Volevodz NN, et al. Adiponectin: A pleiotropic hormone with multifaceted roles. Probl Endokrinol (Mosk). 2021;67(6):98–112.
Shariq OA, TJ MK. Obesity-related hypertension: A review of pathophysiology, management, and the role of metabolic surgery. Gland Surg. 2020;9(1):80–93.
Mohamed MS, Youssef TM, Abdullah EE, et al. Correlation between adiponectin level and the degree of fibrosis in patients with non-alcoholic fatty liver disease. Egypt Liver J. 2021;11(1).
Parida S, Siddharth S, Sharma D. Adiponectin, obesity, and cancer: Clash of the bigwigs in health and disease. Int J Mol Sci. 2019;20(10).
Turer AT, Scherer PE. Adiponectin: Mechanistic insights and clinical implications. Diabetologia. 2012;55(9):2319–26.
Karbowska J, Kochan Z. Role of adiponectin in the regulation of carbohydrate and lipid metabolism. J Physiol Pharmacol. 2006;57(Suppl 6):103–13.
Udomsinprasert W, Honsawek S, Poovorawan Y. Adiponectin as a novel biomarker for liver fibrosis. World J Hepatol. 2018;10(10):708–18.
Ohashi K, Kihara S, Ouchi N, et al. Adiponectin replenishment ameliorates obesity-related hypertension. Hypertension. 2006;47(6):1108–16.
Menzaghi C, Trischitta V. The adiponectin paradox for all-cause and cardiovascular mortality. Diabetes. 2018;67(1):12–22.
Adamczak M, Wiecek A, Funahashi T, et al. Decreased plasma adiponectin concentration in patients with essential hypertension. Am J Hypertens. 2003;16(1):72–5.
Imatoh T, Miyazaki M, Momose Y, et al. Adiponectin levels associated with the development of hypertension: A prospective study. Hypertens Res. 2008;31(2):229–33.
Wildman RP, Mancuso P, Wang C, et al. Adipocytokine and ghrelin levels in relation to cardiovascular disease risk factors in women at midlife: Longitudinal associations. Int J Obes (Lond). 2008;32(5):740–8.
Chow WS, Cheung BM, Tso AW, et al. Hypoadiponectinemia as a predictor for the development of hypertension: A 5-year prospective study. Hypertension. 2007;49(6):1455–61.
Wang L, Manson JE, Gaziano JM, et al. Plasma adiponectin and the risk of hypertension in white and black postmenopausal women. Clin Chem. 2012;58(10):1438–45.
Ohashi K, Ouchi N, Matsuzawa Y. Adiponectin and hypertension. Am J Hypertens. 2011;24(3):263–9.
Tanida M, Shen J, Horii Y, et al. Effects of adiponectin on the renal sympathetic nerve activity and blood pressure in rats. Exp Biol Med (Maywood). 2007;232(3):390–7.
Rahmouni K, Correia ML, Haynes WG, et al. Obesity-associated hypertension: New insights into mechanisms. Hypertension. 2005;45(1):9–14.
Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;41(3 Pt 2):625–33.
Wang ZV, Scherer PE. Adiponectin, cardiovascular function, and hypertension. Hypertension. 2008;51(1):8–14.
Yiannikouris F, Gupte M, Putnam K, et al. Adipokines and blood pressure control. Curr Opin Nephrol Hypertens. 2010;19(2):195–200.
Kim DH, Kim C, Ding EL, et al. Adiponectin levels and the risk of hypertension: A systematic review and meta-analysis. Hypertension. 2013;62(1):27–32.
Bassi M, do Carmo JM, Hall JE, et al. Chronic effects of centrally administered adiponectin on appetite, metabolism and blood pressure regulation in normotensive and hypertensive rats. Peptides. 2012;37(1):1–5.
Kamari Y, Shimoni N, Koren F, et al. High-salt diet increases plasma adiponectin levels independent of blood pressure in hypertensive rats: The role of the renin-angiotensin-aldosterone system. J Hypertens. 2010;28(1):95–101.
Ivkovic V, Jelakovic M, Laganovic M, et al. Adiponectin is not associated with blood pressure in normotensives and untreated hypertensives with normal kidney function. Medicine (Baltimore). 2014;93(28):e250.
Onat A, Aydin M, Can G, et al. High adiponectin levels fail to protect against the risk of hypertension and, in women, against coronary disease: Involvement in autoimmunity? World J Diabetes. 2013;4(5):219–25.
Juonala M, Saarikoski LA, Viikari JS, et al. A longitudinal analysis on associations of adiponectin levels with metabolic syndrome and carotid artery intima-media thickness. The cardiovascular risk in young finns study. Atherosclerosis. 2011;217(1):234–9.
Kaze AD, Musani SK, Bidulescu A, et al. Plasma adiponectin and blood pressure progression in african americans: The jackson heart study. Am J Hypertens. 2021;34(11):1163–70.
Kim JY, Ahn SV, Yoon JH, et al. Prospective study of serum adiponectin and incident metabolic syndrome: The arirang study. Diabetes Care. 2013;36(6):1547–53.
Choi SH, Ku EJ, Hong ES, et al. High serum adiponectin concentration and low body mass index are significantly associated with increased all-cause and cardiovascular mortality in an elderly cohort, “adiponectin paradox”: The korean longitudinal study on health and aging (klosha). Int J Cardiol. 2015;183:91–7.
Wu O, Leng JH, Yang FF, et al. The paradox of the role of resistin in early-onset obesity hypertension: A comparative study among four chinese adult subgroups. Clin Exp Hypertens. 2021;43(5):385–91.
Wu O, Hang Leng J, Zhang XY, et al. The value of adiponectin-resistin (ar) index in newly diagnosed obesity hypertension: A case control study among chinese adult. Clin Exp Hypertens. 2022;44(1):40–5.
Wu O, Leng JH, Yang FF, et al. A comparative research on obesity hypertension by the comparisons and associations between waist circumference, body mass index with systolic and diastolic blood pressure, and the clinical laboratory data between four special chinese adult groups. Clin Exp Hypertens. 2018;40(1):16–21.
Wu O, Leng JH, Zhang X, et al. Controversial culprit of leptin in obesity hypertension: Clues from a case-control study with chinese newly diagnosed adult early-onset obesity hypertensives. Clin Exp Hypertens. 2022:1–7.
Wu O, Yuan C, Leng J, et al. Colorable role of interleukin (il)-6 in obesity hypertension: A hint from a chinese adult case-control study. Cytokine. 2023;168:156226.
Wang SK, Ma W, Wang S, et al. Obesity and its relationship with hypertension among adults 50 years and older in jinan, china. PLoS One. 2014;9(12):e114424.
Arimura ST, Moura BM, Pimentel GD, et al. Waist circumference is better associated with high density lipoprotein (hdl-c) than with body mass index (bmi) in adults with metabolic syndrome. Nutr Hosp. 2011;26(6):1328–32.
Apovian CM. Obesity: Definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22(7 Suppl):s176–85.
Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in europe. N Engl J Med. 2008;359(20):2105–20.
Amato MC, Pizzolanti G, Torregrossa V, et al. Visceral adiposity index (vai) is predictive of an altered adipokine profile in patients with type 2 diabetes. PLoS One. 2014;9(3):e91969.
Blus E, Wojciechowska-Kulik A, Majewska E, et al. Usefulness of new indicators of obesity (bai and vai) in estimation of weight reduction. J Am Coll Nutr. 2020;39(2):171–7.
Brown MA, Reiter L, Smith B, et al. Measuring blood pressure in pregnant women: A comparison of direct and indirect methods. Am J Obstet Gynecol. 1994;171(3):661–7.
Kubozono T, Akasaki Y, Kawasoe S, et al. Relationship between defecation status and blood pressure level or blood pressure variability. Hypertens Res. 2024;47(1):128–36.
Wang JG, Sun NL, Ke YN, et al. Long-term efficacy of olmesartan medoxomil in chinese hypertensive patients as assessed by clinic, ambulatory and home blood pressure measurements. Clin Drug Investig. 2012;32(11):729–34.
Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA. 2003;289(19):2560–72.
Muntner P, Einhorn PT, Cushman WC, et al. Blood pressure assessment in adults in clinical practice and clinic-based research: Jacc scientific expert panel. J Am Coll Cardiol. 2019;73(3):317–35.
Beevers G, Lip GY, O’Brien E, Abc of hypertension. Blood pressure measurement. Part i-sphygmomanometry: Factors common to all techniques. BMJ. 2001;322(7292):981–5.
Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88(5 Pt 1):2460–70.
Teng L, Zheng J, Leng J, et al. Clinical and molecular characterization of a han chinese family with high penetrance of essential hypertension. Mitochondrial DNA. 2012;23(6):461–5.
Banegas JR, Segura J, Ruilope LM, et al. Blood pressure control and physician management of hypertension in hospital hypertension units in spain. Hypertension. 2004;43(6):1338–44.
Czerwienska B, Lelek M, Gojowy D, et al. Effect of renal denervation on the plasma adiponectin concentration in patients with resistant hypertension. J Clin Med. 2023;12(6).
Mantula PS, Outinen TK, Jaatinen P, et al. High plasma resistin associates with severe acute kidney injury in puumala hantavirus infection. PLoS One. 2018;13(12):e0208017.
Li Z, Li Y, Overstreet JM, et al. Inhibition of epidermal growth factor receptor activation is associated with improved diabetic nephropathy and insulin resistance in type 2 diabetes. Diabetes. 2018;67(9):1847–57.
Swarbrick MM, Havel PJ. Physiological, pharmacological, and nutritional regulation of circulating adiponectin concentrations in humans. Metab Syndr Relat Disord. 2008;6(2):87–102.
Arita Y, Kihara S, Ouchi N, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999;257(1):79–83.
You H, Zhang T, Feng W, et al. Association of tcm body constitution with insulin resistance and risk of diabetes in impaired glucose regulation patients. BMC Complement Altern Med. 2017;17(1):459.
Achari AE, Jain SK. Adiponectin, a therapeutic target for obesity, diabetes, and endothelial dysfunction. Int J Mol Sci. 2017;18(6).
Berner HS, Lyngstadaas SP, Spahr A, et al. Adiponectin and its receptors are expressed in bone-forming cells. Bone. 2004;35(4):842–9.
Yoda-Murakami M, Taniguchi M, Takahashi K, et al. Change in expression of gbp28/adiponectin in carbon tetrachloride-administrated mouse liver. Biochem Biophys Res Commun. 2001;285(2):372–7.
Delaigle AM, Jonas JC, Bauche IB, et al. Induction of adiponectin in skeletal muscle by inflammatory cytokines: In vivo and in vitro studies. Endocrinology. 2004;145(12):5589–97.
Patel JV, Abraheem A, Dotsenko O, et al. Circulating serum adiponectin levels in patients with coronary artery disease: Relationship to atherosclerotic burden and cardiac function. J Intern Med. 2008;264(6):593–8.
Caminos JE, Nogueiras R, Gallego R, et al. Expression and regulation of adiponectin and receptor in human and rat placenta. J Clin Endocrinol Metab. 2005;90(7):4276–86.
Cohen KE, Katunaric B, SenthilKumar G, et al. Vascular endothelial adiponectin signaling across the life span. Am J Physiol Heart Circ Physiol. 2022;322(1):H57–65.
Aljafary MA, Al-Suhaimi EA. Adiponectin system (rescue hormone): The missing link between metabolic and cardiovascular diseases. Pharmaceutics. 2022;14(7).
Jang AY, Scherer PE, Kim JY, et al. Adiponectin and cardiometabolic trait and mortality: Where do we go? Cardiovasc Res. 2022;118(9):2074–84.
Han Y, Sun Q, Chen W, et al. New advances of adiponectin in regulating obesity and related metabolic syndromes. J Pharm Anal. https://doi.org/10.1016/j.jpha.2023.12.003. Epub ahead of print.
Kennedy AJ, Ellacott KL, King VL, et al. Mouse models of the metabolic syndrome. Dis Model Mech. 2010;3(3–4):156–66.
Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: An endocrine organ. Arch Med Sci. 2013;9(2):191–200.
Woodward L, Akoumianakis I, Antoniades C. Unravelling the adiponectin paradox: Novel roles of adiponectin in the regulation of cardiovascular disease. Br J Pharmacol. 2017;174(22):4007–20.
Kiess W, Petzold S, Topfer M, et al. Adipocytes and adipose tissue. Best Pract Res Clin Endocrinol Metab. 2008;22(1):135–53.
Oikonomou EK, Antoniades C. The role of adipose tissue in cardiovascular health and disease. Nat Rev Cardiol. 2019;16(2):83–99.
Harms M, Seale P. Brown and beige fat: Development, function and therapeutic potential. Nat Med. 2013;19(10):1252–63.
Villarroya F, Cereijo R, Villarroya J, et al. Brown adipose tissue as a secretory organ. Nat Rev Endocrinol. 2017;13(1):26–35.
Messaggio F, Mendonsa AM, Castellanos J, et al. Adiponectin receptor agonists inhibit leptin induced pstat3 and in vivo pancreatic tumor growth. Oncotarget. 2017;8(49):85378–91.
Kim AY, Park YJ, Pan X, et al. Obesity-induced DNA hypermethylation of the adiponectin gene mediates insulin resistance. Nat Commun. 2015;6:7585.
Satoh K, Nagasawa K, Takebe N, et al. Adiponectin paradox more evident in non-obese than in obese patients with diabetic microvascular complications. Diabetes Metab Syndr Obes. 2023;16:201–12.
Peng J, Chen Q, Wu C. The role of adiponectin in cardiovascular disease. Cardiovasc Pathol. 2023;64.
Khan RS, Kato TS, Chokshi A, et al. Adipose tissue inflammation and adiponectin resistance in patients with advanced heart failure: Correction after ventricular assist device implantation. Circ Heart Fail. 2012;5(3):340–8.
Scheller EL, Burr AA, MacDougald OA, et al. Inside out: Bone marrow adipose tissue as a source of circulating adiponectin. Adipocyte. 2016;5(3):251–69.
Cawthorn WP, Scheller EL, Learman BS, et al. Bone marrow adipose tissue is an endocrine organ that contributes to increased circulating adiponectin during caloric restriction. Cell Metab. 2014;20(2):368–75.
Hamzeh B, Pasdar Y, Mirzaei N, et al. Visceral adiposity index and atherogenic index of plasma as useful predictors of risk of cardiovascular diseases: Evidence from a cohort study in iran. Lipids Health Dis. 2021;20(1):82.
Jiang K, Luan H, Pu X, et al. Association between visceral adiposity index and insulin resistance: A cross-sectional study based on us adults. Front Endocrinol (Lausanne). 2022;13:921067.
Amato MC, Giordano C, Pitrone M, et al. Cut-off points of the visceral adiposity index (vai) identifying a visceral adipose dysfunction associated with cardiometabolic risk in a caucasian sicilian population. Lipids Health Dis. 2011;10:183.
Amato MC, Giordano C, Galia M, et al. Visceral adiposity index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–2.
Guenther M, James R, Marks J, et al. Adiposity distribution influences circulating adiponectin levels. Transl Res. 2014;164(4):270–7.
Begum M, Choubey M, Tirumalasetty MB, et al. Adiponectin: A promising target for the treatment of diabetes and its complications. Life (Basel). 2023;13(11).
Qin Y, Qiao Y, Wang D, et al. Visceral adiposity index is positively associated with fasting plasma glucose: A cross-sectional study from national health and nutrition examination survey 2017–2020. BMC Public Health. 2023;23(1):313.
Ma W, Huang T, Wang M, et al. Two-year changes in circulating adiponectin, ectopic fat distribution and body composition in response to weight-loss diets: The pounds lost trial. Int J Obes (Lond). 2016;40(11):1723–9.
Gariballa S, Alkaabi J, Yasin J, et al. Total adiponectin in overweight and obese subjects and its response to visceral fat loss. BMC Endocr Disord. 2019;19(1):55.
Hassler EM, Deutschmann H, Almer G, et al. Distribution of subcutaneous and intermuscular fatty tissue of the mid-thigh measured by mri-a putative indicator of serum adiponectin level and individual factors of cardio-metabolic risk. PLoS One. 2021;16(11):e0259952.
Booth AD, Magnuson AM, Fouts J, et al. Subcutaneous adipose tissue accumulation protects systemic glucose tolerance and muscle metabolism. Adipocyte. 2018;7(4):261–72.
Frederiksen L, Nielsen TL, Wraae K, et al. Subcutaneous rather than visceral adipose tissue is associated with adiponectin levels and insulin resistance in young men. J Clin Endocrinol Metab. 2009;94(10):4010–5.
Gustafson B, Hedjazifar S, Gogg S, et al. Insulin resistance and impaired adipogenesis. Trends Endocrinol Metab. 2015;26(4):193–200.
Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020;7:22.
Turer AT, Khera A, Ayers CR, et al. Adipose tissue mass and location affect circulating adiponectin levels. Diabetologia. 2011;54(10):2515–24.
Vega GL, Grundy SM. Metabolic risk susceptibility in men is partially related to adiponectin/leptin ratio. J Obes. 2013;2013:409679.
Ma X, Lee P, Chisholm DJ, et al. Control of adipocyte differentiation in different fat depots; implications for pathophysiology or therapy. Front Endocrinol (Lausanne). 2015;6:1.
Kwok KH, Lam KS, Xu A. Heterogeneity of white adipose tissue: Molecular basis and clinical implications. Exp Mol Med. 2016;48(3):e215.
Amato MC, Giordano C. Visceral adiposity index: An indicator of adipose tissue dysfunction. Int J Endocrinol. 2014;2014:730827.
Gholami F, Karimi Z, Samadi M, et al. The association between dietary pattern and visceral adiposity index, triglyceride-glucose index, inflammation, and body composition among iranian overweight and obese women. Sci Rep. 2023;13(1):13162.
Han M, Qie R, Li Q, et al. Chinese visceral adiposity index, a novel indicator of visceral obesity for assessing the risk of incident hypertension in a prospective cohort study. Br J Nutr. 2021;126(4):612–20.
Wang K, Xia F, Li Q, et al. The associations of weekend warrior activity patterns with the visceral adiposity index in us adults: Repeated cross-sectional study. JMIR Public Health Surveill. 2023;9:e41973.
Matsuzawa Y. The role of fat topology in the risk of disease. Int J Obes (Lond). 2008;32(Suppl 7):S83–92.
Ross R, Janssen I, Dawson J, et al. Exercise-induced reduction in obesity and insulin resistance in women: A randomized controlled trial. Obes Res. 2004;12(5):789–98.
Irwin ML, Yasui Y, Ulrich CM, et al. Effect of exercise on total and intra-abdominal body fat in postmenopausal women: A randomized controlled trial. JAMA. 2003;289(3):323–30.
Kim SH, Lee SH, Ahn KY, et al. Effect of lifestyle modification on serum chemerin concentration and its association with insulin sensitivity in overweight and obese adults with type 2 diabetes. Clin Endocrinol (Oxf). 2014;80(6):825–33.
Bradley RL, Jeon JY, Liu FF, et al. Voluntary exercise improves insulin sensitivity and adipose tissue inflammation in diet-induced obese mice. Am J Physiol Endocrinol Metab. 2008;295(3):E586–94.
Bluher M, Bullen JW Jr, Lee JH, et al. Circulating adiponectin and expression of adiponectin receptors in human skeletal muscle: Associations with metabolic parameters and insulin resistance and regulation by physical training. J Clin Endocrinol Metab. 2006;91(6):2310–6.
Oberbach A, Tonjes A, Kloting N, et al. Effect of a 4 week physical training program on plasma concentrations of inflammatory markers in patients with abnormal glucose tolerance. Eur J Endocrinol. 2006;154(4):577–85.
Waragai M, Ho G, Takamatsu Y, et al. Adiponectin paradox in alzheimer’s disease; relevance to amyloidogenic evolvability? Front Endocrinol (Lausanne). 2020;11:108.
Dezonne RS, Pereira CM, de Moraes MCJ, et al. Adiponectin, the adiponectin paradox, and alzheimer’s disease: Is this association biologically plausible? Metab Brain Dis. 2023;38(1):109–21.
Choi CHJ, Cohen P. Adipose crosstalk with other cell types in health and disease. Exp Cell Res. 2017;360(1):6–11.
Clemente-Suarez VJ, Redondo-Florez L, Beltran-Velasco AI, et al. The role of adipokines in health and disease. Biomedicines. 2023;11(5).
Villarroya F, Gavalda-Navarro A, Peyrou M, et al. Brown adipokines. Handb Exp Pharmacol. 2019;251:239–56.
von Schnurbein J, Manzoor J, Brandt S, et al. Leptin is not essential for obesity-associated hypertension. Obes Facts. 2019;12(4):460–75.
Zheng F, Mu S, Rusch NJ. Leptin activates trpm7 channels in the carotid body as a mechanism of obesity-related hypertension. Circ Res. 2019;125(11):1003–5.
Lingappan K. Does the epigenome hold clues to leptin-associated hypertension in obesity? Am J Respir Cell Mol Biol. 2021;65(2):132–3.
Luo L, Liu M. Adiponectin: Friend or foe in obesity and inflammation. Med Rev. 2021;2(4):349–62.
Ohman-Hanson RA, Cree-Green M, Kelsey MM, et al. Ethnic and sex differences in adiponectin: From childhood to adulthood. J Clin Endocrinol Metab. 2016;101(12):4808–15.
Bottner A, Kratzsch J, Muller G, et al. Gender differences of adiponectin levels develop during the progression of puberty and are related to serum androgen levels. J Clin Endocrinol Metab. 2004;89(8):4053–61.
Song HJ, Oh S, Quan S, et al. Gender differences in adiponectin levels and body composition in older adults: Hallym aging study. BMC Geriatr. 2014;14:8.
Tsou PL, Jiang YD, Chang CC, et al. Sex-related differences between adiponectin and insulin resistance in schoolchildren. Diabetes Care. 2004;27(2):308–13.
Gardener H, Crisby M, Sjoberg C, et al. Serum adiponectin in relation to race-ethnicity and vascular risk factors in the northern manhattan study. Metab Syndr Relat Disord. 2013;11(1):46–55.
Pereira RI, Low Wang CC, Wolfe P, et al. Associations of adiponectin with adiposity, insulin sensitivity, and diet in young, healthy, mexican americans and non-latino white adults. Int J Environ Res Public Health. 2015;13(1):ijerph13010054.
Pereira RI, Wang CC, Hosokawa P, et al. Circulating adiponectin levels are lower in latino versus non-latino white patients at risk for cardiovascular disease, independent of adiposity measures. BMC Endocr Disord. 2011;11:13.
Vucic Lovrencic M, Geric M, Kosuta I, et al. Sex-specific effects of vegetarian diet on adiponectin levels and insulin sensitivity in healthy non-obese individuals. Nutrition. 2020;79–80:110862.
Janiszewska J, Ostrowska J, Szostak-Wegierek D. The influence of nutrition on adiponectin-a narrative review. Nutrients. 2021;13(5).
Poret JM, Gaudet DA, Braymer HD, et al. Sex differences in markers of metabolic syndrome and adipose tissue inflammation in obesity-prone, osborne-mendel and obesity-resistant, s5b/pl rats. Life Sci. 2021;273:119290.
Bedard A, Tchernof A, Lamarche B, et al. Effects of the traditional mediterranean diet on adiponectin and leptin concentrations in men and premenopausal women: Do sex differences exist? Eur J Clin Nutr. 2014;68(5):561–6.
Izadi V, Azadbakht L. Specific dietary patterns and concentrations of adiponectin. J Res Med Sci. 2015;20(2):178–84.
Alves-Santos NH, Cocate PG, Eshriqui I, et al. Dietary patterns and their association with adiponectin and leptin concentrations throughout pregnancy: A prospective cohort. Br J Nutr. 2018;119(3):320–9.
Martinez-Fernandez L, Laiglesia LM, Huerta AE, et al. Omega-3 fatty acids and adipose tissue function in obesity and metabolic syndrome. Prostaglandins Other Lipid Mediat. 2015;121(Pt A):24–41.
Ferguson CC, Knol LL, Ellis AC. Visceral adiposity index and its association with dietary approaches to stop hypertension (dash) diet scores among older adults: National health and nutrition examination surveys 2011–2014. Clin Nutr. 2021;40(6):4085–9.
Li G, Zhong L, Han L, et al. Genetic variations in adiponectin levels and dietary patterns on metabolic health among children with normal weight versus obesity: The bcams study. Int J Obes (Lond). 2022;46(2):325–32.
Gao S, Li G, Willi SM, et al. 1316-p: Adiponectin-related genetic variation and dietary pattern associations with metabolic health in children across weight status: From a large cohort study. Diabetes. 2019;68(Supplement_1).
Imhof A, Plamper I, Maier S, et al. Effect of drinking on adiponectin in healthy men and women: A randomized intervention study of water, ethanol, red wine, and beer with or without alcohol. Diabetes Care. 2009;32(6):1101–3.
Garcia-Garcia MR, Morales-Lanuza MA, Campos-Perez WY, et al. Effect of the adipoq gene -11391g/a polymorphism is modulated by lifestyle factors in mexican subjects. J Nutrigenet Nutrigenomics. 2014;7(4–6):212–24.
Wu Y, Zhong L, Li G, et al. Puberty status modifies the effects of genetic variants, lifestyle factors and their interactions on adiponectin: The bcams study. Front Endocrinol (Lausanne). 2021;12:737459.
Szabo R, Borzsei D, Hoffmann A, et al. The interplay of lifestyle and adipokines in the non-obese stroke-prone spontaneously hypertensive rats. Antioxidants (Basel). 2023;12(7).
Cantini G, Quartararo G, Ghezzi N, et al. Visceral adipose tissue adiponectin predicts excess weight loss after bariatric surgery in females with severe obesity. Int J Obes (Lond). 2024;48(2):247–53.
Adela R, Reddy PNC, Ghosh TS, et al. Serum protein signature of coronary artery disease in type 2 diabetes mellitus. J Transl Med. 2019;17(1):17.
Gul E, Gul Y, Yildirim E, et al. The diagnostic role of adiponectin in pulmonary embolism. Biomed Res Int. 2016;2016:6121056.
Lambert M, O’Loughlin J, Delvin EE, et al. Association between insulin, leptin, adiponectin and blood pressure in youth. J Hypertens. 2009;27(5):1025–32.
Mallamaci F, Zoccali C, Cuzzola F, et al. Adiponectin in essential hypertension. J Nephrol. 2002;15(5):507–11.
Atzmon G, Pollin TI, Crandall J, et al. Adiponectin levels and genotype: A potential regulator of life span in humans. J Gerontol A Biol Sci Med Sci. 2008;63(5):447–53.
Lei X, Qiu S, Yang G, et al. Adiponectin and metabolic cardiovascular diseases: Therapeutic opportunities and challenges. Genes Dis. 2023;10(4):1525–36.
Yannakoulia M, Yiannakouris N, Bluher S, et al. Body fat mass and macronutrient intake in relation to circulating soluble leptin receptor, free leptin index, adiponectin, and resistin concentrations in healthy humans. J Clin Endocrinol Metab. 2003;88(4):1730–6.
Manieri E, Herrera-Melle L, Mora A, et al. Adiponectin accounts for gender differences in hepatocellular carcinoma incidence. J Exp Med. 2019;216(5):1108–19.
Cnop M, Havel PJ, Utzschneider KM, et al. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: Evidence for independent roles of age and sex. Diabetologia. 2003;46(4):459–69.
Sawaguchi T, Nakajima T, Haruyama A, et al. Association of serum leptin and adiponectin concentrations with echocardiographic parameters and pathophysiological states in patients with cardiovascular disease receiving cardiovascular surgery. PLoS One. 2019;14(11):e0225008.
Chen HY, Chiu YL, Hsu SP, et al. Reappraisal of effects of serum chemerin and adiponectin levels and nutritional status on cardiovascular outcomes in prevalent hemodialysis patients. Sci Rep. 2016;6:34128.
Abdollahi A, Dowden BN, Buhman KK, et al. Albumin knockout mice exhibit reduced plasma free fatty acid concentration and enhanced insulin sensitivity. Physiol Rep. 2022;10(5):e15161.
Uetani E, Tabara Y, Igase M, et al. Liver enzyme and adipocytokine profiles are synergistically associated with insulin resistance: The j-shipp study. J Atheroscler Thromb. 2012;19(6):577–84.
Kazumi T, Kawaguchi A, Hirano T, et al. Serum alanine aminotransferase is associated with serum adiponectin, c-reactive protein and apolipoprotein b in young healthy men. Horm Metab Res. 2006;38(2):119–24.
Ezenwaka CE, Kalloo R, Uhlig M, et al. Serum adiponectin levels and enzyme markers of liver dysfunction in diabetic and non-diabetic caribbean subjects. Br J Biomed Sci. 2006;63(3):117–22.
Martin-Rodriguez JL, Gonzalez-Cantero J, Gonzalez-Cantero A, et al. Diagnostic accuracy of serum alanine aminotransferase as biomarker for nonalcoholic fatty liver disease and insulin resistance in healthy subjects, using 3t mr spectroscopy. Medicine (Baltimore). 2017;96(17):e6770.
Burgert TS, Taksali SE, Dziura J, et al. Alanine aminotransferase levels and fatty liver in childhood obesity: Associations with insulin resistance, adiponectin, and visceral fat. J Clin Endocrinol Metab. 2006;91(11):4287–94.
Al-Jiffri OH, Alsharif FM. Levels of circulating adipokines and their relation with glycemic control and insulin resistance in saudi patients with non-alcoholic fatty liver disease. Electron J Gen Med. 2017;14(4).
Guo R, Nair S, Zhang Y, et al. Adiponectin deficiency rescues high-fat diet-induced hepatic injury, apoptosis and autophagy loss despite persistent steatosis. Int J Obes (Lond). 2017;41(9):1403–12.
Yamamoto Y, Hirose H, Saito I, et al. Correlation of the adipocyte-derived protein adiponectin with insulin resistance index and serum high-density lipoprotein-cholesterol, independent of body mass index, in the japanese population. Clin Sci (Lond). 2002;103(2):137–42.
Matsubara M, Maruoka S, Katayose S. Decreased plasma adiponectin concentrations in women with dyslipidemia. J Clin Endocrinol Metab. 2002;87(6):2764–9.
Christou GA, Tellis KC, Elisaf MC, et al. High density lipoprotein is positively correlated with the changes in circulating total adiponectin and high molecular weight adiponectin during dietary and fenofibrate treatment. Hormones (Athens). 2012;11(2):178–88.
Ezenwaka CE, Kalloo R, Uhlig M, et al. Relationship between adiponectin and metabolic variables in caribbean offspring of patients with type 2 diabetes mellitus. Horm Metab Res. 2004;36(4):238–42.
Kazumi T, Kawaguchi A, Hirano T, et al. Serum adiponectin is associated with high-density lipoprotein cholesterol, triglycerides, and low-density lipoprotein particle size in young healthy men. Metabolism. 2004;53(5):589–93.
Shetty GK, Economides PA, Horton ES, et al. Circulating adiponectin and resistin levels in relation to metabolic factors, inflammatory markers, and vascular reactivity in diabetic patients and subjects at risk for diabetes. Diabetes Care. 2004;27(10):2450–7.
Kangas-Kontio T, Huotari A, Ruotsalainen H, et al. Genetic and environmental determinants of total and high-molecular weight adiponectin in families with low hdl-cholesterol and early onset coronary heart disease. Atherosclerosis. 2010;210(2):479–85.
Oku H, Matsuura F, Koseki M, et al. Adiponectin deficiency suppresses abca1 expression and apoa-i synthesis in the liver. FEBS Lett. 2007;581(26):5029–33.
Matsuura F, Oku H, Koseki M, et al. Adiponectin accelerates reverse cholesterol transport by increasing high density lipoprotein assembly in the liver. Biochem Biophys Res Commun. 2007;358(4):1091–5.
Qiao L, Zou C, van der Westhuyzen DR, et al. Adiponectin reduces plasma triglyceride by increasing vldl triglyceride catabolism. Diabetes. 2008;57(7):1824–33.
Tsubakio-Yamamoto K, Matsuura F, Koseki M, et al. Adiponectin prevents atherosclerosis by increasing cholesterol efflux from macrophages. Biochem Biophys Res Commun. 2008;375(3):390–4.
Kitajima K, Miura S, Yamauchi T, et al. Possibility of increasing cholesterol efflux by adiponectin and its receptors through the atp binding cassette transporter a1 in hek293t cells. Biochem Biophys Res Commun. 2011;411(2):305–11.
Hafiane A, Daskalopoulou SS. Adiponectin’s mechanisms in high-density lipoprotein biogenesis and cholesterol efflux. Metabolism. 2020;113:154393.
Ghoshal K, Chatterjee T, Chowdhury S, et al. Adiponectin genetic variant and expression coupled with lipid peroxidation reveal new signatures in diabetic dyslipidemia. Biochem Genet. 2021;59(3):781–98.
Ghoshal K, Bhattacharyya M. Adiponectin: Probe of the molecular paradigm associating diabetes and obesity. World J Diabetes. 2015;6(1):151–66.
Halberg N, Schraw TD, Wang ZV, et al. Systemic fate of the adipocyte-derived factor adiponectin. Diabetes. 2009;58(9):1961–70.
Sowka A, Dobrzyn P. Role of perivascular adipose tissue-derived adiponectin in vascular homeostasis. Cells. 2021;10(6).
Ran J, Xiong X, Liu W, et al. Increased plasma adiponectin closely associates with vascular endothelial dysfunction in type 2 diabetic patients with diabetic nephropathy. Diabetes Res Clin Pract. 2010;88(2):177–83.
Menzaghi C, Xu M, Salvemini L, et al. Circulating adiponectin and cardiovascular mortality in patients with type 2 diabetes mellitus: Evidence of sexual dimorphism. Cardiovasc Diabetol. 2014;13:130.
Wang Y, Ma XL, Lau WB. Cardiovascular adiponectin resistance: The critical role of adiponectin receptor modification. Trends Endocrinol Metab. 2017;28(7):519–30.
Przybycinski J, Dziedziejko V, Puchalowicz K, et al. Adiponectin in chronic kidney disease. Int J Mol Sci. 2020;21(24).
van Andel M, Heijboer AC, Drent ML. Adiponectin and its isoforms in pathophysiology. Adv Clin Chem. 2018;85:115–47.
Ruan H, Dong LQ. Adiponectin signaling and function in insulin target tissues. J Mol Cell Biol. 2016;8(2):101–9.
Kita S, Fukuda S, Maeda N, et al. Native adiponectin in serum binds to mammalian cells expressing t-cadherin, but not adipors or calreticulin. Elife. 2019;8.
Clark JL, Taylor CG, Zahradka P. Exploring the cardio-metabolic relevance of t-cadherin: A pleiotropic adiponectin receptor. Endocr Metab Immune Disord Drug Targets. 2017;17(3):200–6.
Sun Y, Zhao D, Yang Y, et al. Adiponectin exerts cardioprotection against ischemia/reperfusion injury partially via calreticulin mediated anti-apoptotic and anti-oxidative actions. Apoptosis. 2017;22(1):108–17.
Okada-Iwabu M, Iwabu M, Yamauchi T, et al. Structure and function analysis of adiponectin receptors toward development of novel antidiabetic agents promoting healthy longevity. Endocr J. 2018;65(10):971–7.
Kersten S, Desvergne B, Wahli W. Roles of ppars in health and disease. Nature. 2000;405(6785):421–4.
Straub LG, Scherer PE. Metabolic messengers: Adiponectin. Nat Metab. 2019;1(3):334–9.
Walowski CO, Herpich C, Enderle J, et al. Analysis of the adiponectin paradox in healthy older people. J Cachexia Sarcopenia Muscle. 2023;14(1):270–8.
Uetani E, Tabara Y, Kawamoto R, et al. Cdh13 genotype-dependent association of high-molecular weight adiponectin with all-cause mortality: The j-shipp study. Diabetes Care. 2014;37(2):396–401.
Kalkman HO. An explanation for the adiponectin paradox. Pharmaceuticals (Basel). 2021;14(12).
Furuhashi M, Ura N, Higashiura K, et al. Blockade of the renin-angiotensin system increases adiponectin concentrations in patients with essential hypertension. Hypertension. 2003;42(1):76–81.
Bidulescu A, Choudhry S, Musani SK, et al. Associations of adiponectin with individual european ancestry in african americans: The jackson heart study. Front Genet. 2014;5:22.
Acknowledgements
The authors would like to give special thanks to all participants in this study.
Funding
This work was supported by Zhejiang Shuren University Basic Scientific Research Special Funds (2024XZ012), grants from the National Natural Science Foundation of China (81102200/H2610), and “Teacher professional development project” for domestic visiting scholars in colleges and universities of Zhejiang Province in 2020 (043).
Author information
Authors and Affiliations
Contributions
Ou Wu: Conceptualization, Data curation, Writing – original draft, Methodology, Supervision, Validation, Funding acquisition, Project administration, Formal analysis. Xi Lu: Conceptualization, Data curation, Writing – original draft, Methodology, Supervision, Validation. Jianhang Leng: Project administration, Data curation. Xingyu Zhang: Writing – review & editing, Software. Wei Liu: Project administration, Data curation. Fenfang Yang: Project administration, Data curation. Hu Zhang: Project administration, Data curation. Jiajia Li: Project administration, Data curation. Saber Khederzadeh: Writing – review & editing, Software. Xiaodong Liu: Resources. Chengda Yuan: Conceptualization, Project administration, Investigation, Writing – review & editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study involving human participants were in accordance with ethical standards of institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional ethics committee of Hangzhou Center for Disease Control and Prevention approved the study. Informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, O., Lu, X., Leng, J. et al. Reevaluating Adiponectin’s impact on obesity hypertension: a Chinese case-control study. BMC Cardiovasc Disord 24, 208 (2024). https://doi.org/10.1186/s12872-024-03865-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03865-4