Abstract
Background
Acute kidney injury (AKI) in patients with acute myocardial infarction (AMI) often indicates a poor prognosis.
Objective
This study aimed to investigate the association between the TyG index and the risk of AKI in patients with AMI.
Methods
Data were taken from the Medical Information Mart for Intensive Care (MIMIC) database. A 1:3 propensity score (PS) was set to match patients in the AKI and non-AKI groups. Multivariate logistic regression analysis, restricted cubic spline (RCS) regression and subgroup analysis were performed to assess the association between TyG index and AKI.
Results
Totally, 1831 AMI patients were included, of which 302 (15.6%) had AKI. The TyG level was higher in AKI patients than in non-AKI patients (9.30 ± 0.71 mg/mL vs. 9.03 ± 0.73 mg/mL, P < 0.001). Compared to the lowest quartile of TyG levels, quartiles 3 or 4 had a higher risk of AKI, respectively (Odds Ratiomodel 4 = 2.139, 95% Confidence Interval: 1.382–3.310, for quartile 4 vs. quartile 1, Ptrend < 0.001). The risk of AKI increased by 34.4% when the TyG level increased by 1 S.D. (OR: 1.344, 95% CI: 1.150–1.570, P < 0.001). The TyG level was non-linearly associated with the risk of AKI in the population within a specified range. After 1:3 propensity score matching, the results were similar and the TyG level remained a risk factor for AKI in patients with AMI.
Conclusion
High levels of TyG increase the risk of AKI in AMI patients. The TyG level is a predictor of AKI risk in AMI patients, and can be used for clinical management.
Similar content being viewed by others
Introduction
As the most serious ischaemic heart disease, acute myocardial infarction (AMI) is recognized as a leading cause of cardiovascular disease (CVD) morbidity and mortality worldwide [1, 2]. AMI causes more than 24 million deaths in the United States and more than 4 million deaths in Europe and Northern Asia each year [3], accounting for more than one-third of all deaths in developed countries [4]. In recent decades, evidence-based therapies and lifestyle interventions have significantly reduced mortality from coronary heart disease [3]. However, CVD and AMI still brough a huge economic burden, heavier in low- and middle-income countries [5, 6]. In 2010 alone, the direct cost of hospitalization for myocardial infarction in the United States exceeded $450 billion [7].
Acute kidney injury (AKI) is a common and serious complication of AMI [8], usually caused by comorbid factors, hemodynamic instability, and the use of nephrotoxic medications. Studies have shown that the prevalence of AKI ranges from 7.1–29.3% [9,10,11]. AKI during hospitalization was independently associated with a higher in-hospital and long-term mortality after AMI [12,13,14,15,16,17,18].
As a newly recognized indicator of insulin resistance (IR), triglyceride-glucose (TyG) shows a large diagnostic and predictive value for diabetes than blood glucose [19]. IR patients are prone to a variety of metabolic disorders, such as hyperglycemia, dyslipidemia, and hypertension, all of which are strongly associated with adverse CVD outcomes [20]. For example, the TyG level has a stable prognostic value for CAD patients [21, 22]. It can be used to stratify risks and predict the prognosis in patients with acute coronary syndrome (ACS), and predict future major adverse cardiovascular events (MACE) in patients with diabetes combined with ACS independent of known cardiovascular risk factors [23]. Moreover, it is an independent risk factor for in-hospital mortality in patients with acute ST-elevation myocardial infarction, and a criterion for Mitral annular calcification [24]. Meanwhile, the TyG level is significantly associated with heart failure (HF) in AMI patients [25]. The TyG level is also positively correlated with the prognosis of patients with chronic HF and diabetes mellitus: a higher TyG index indicates a higher risk of cardiovascular death or rehospitalization due to HF [26]. In AMI patients, AKI may lead to a worse prognosis. Depsite the development of AKI risk prediction models in AMI patients [27,28,29,30], the relationship between the TyG level and the risk of AKI in patients with AMI is unclear.
Therefore, this study aimed to investigate the association between the TyG level and the AKI risk in AMI patients. Our findings may be depended on to design new strategies to manage AMI-related AKI.
Materials and methods
Data source
AMI patient data were obtained from the Medical Information Mart for Intensive Care (MIMIC) v1.4 and MIMIC-IV v2.2 databases. Use of the MIMIC database was approved by the Beth Israel Deaconess Medical Center and the MIT Institutional Review Board. Approval was obtained after application and completion of courses and testing (record IDs: 44,703,031 and 44,703,032). Informed consent was not required, because all patients’ information in the database was anonymized [31].
Patient enrollment and data collection
Data extraction was programmed using Structured Query Language (SQL) in Navicat Premium (version 15.0.12). Patients with AMI were identified using ICD-9 and ICD-10 (International Classification of Diseases, Ninth and Tenth Revision) codes, and patients with AMI were identified using codes 41,000–41,092 and I21-I219. If the patient was admitted for multiple times, only the first admission was included. Exclusion criteria: (1) patients younger than 18 years or older than 90 years; (2) patients with incomplete test results of serum creatinine, glucose, and triglyceride; and (3) patients with data missed by more than 30%.
Clinical data were collected form eligible subjects, including demographics, comorbidities, vital signs, and laboratory parameters. Comorbidities included atrial fibrillation (AF), type 2 diabetes mellitus (T2DM), hypertension, chronic kidney disease, and obstructive sleep apnea (OSA). Vital signs were collected from the hospitalization records at the first admission, including heart rate (HR), respiratory rate (RR), temperature (T), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean blood pressure (MAP). Laboratory parameters were obtained from the first examination after hospitalization, including red blood cells (RBC), white blood cells (WBC), platelets, hemoglobin, hematocrit, hemoglobin, hematocrit, mean corpuscular volume (MCV), mean corpuscular hemoglobin volume (MCH), mean corpuscular hemoglobin concentration (MCHC), albumin, alanine aminotransferase (ALT), aspartate transaminase (AST), creatine kinase isoenzyme MB (CK-MB), troponin-T (TNT), total bilirubin (TB), alkaline phosphatase (AP), blood urea nitrogen (BUN), creatinine, fasting blood glucose (FBG), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), lactate, total carbon dioxide (T-CO2), arterial carbon dioxide partial pressure (PaCO2), arterial oxygen saturation (SaO2), anion gap (AG), base excess (BE), bicarbonate, potassium, sodium, chloride, total calcium (T-calcium), phosphorus, magnesium, activated partial thromboplastin time (APTT), prothrombin time (PT), international normalized ratio (INR).
Endpoint
The endpoint was AKI during hospitalization. The diagnosis of AKI was based on the latest international clinical practice guidelines for AKI [32], and accordance to any of the following three criteria: (a) creatinine rose ≥ 0.3 mg/dL (≥ 26.5 µmol/L) within 0 h; (b) creatinine rose to ≥ 1.5 times baseline within the 7 days; and (c) urine output < 0.5 mL/kg/hr over 6 h.
Statistical analysis
Categorical variables were described by frequencies and percentages, and differences between groups were determined by the chi-squared test or Fisher’s exact test. Continuous variables were described by mean (± SD) or median and interquartile range (IQR), and differences between groups were determined by Student’s t-test or Mann-Whitney U test. Multivariate analyses (binary logistic regression) were performed to examine the association between the TyG level and the risk of AKI. Results were expressed as odds ratio (OR) and 95% confidence interval (95% CI). We validated the sample size to a rule that the number of outcome events should be ten per independent risk factor [33, 34]. In our study, the sample size was calculated to be 1000 patients or more to allow unbiased accommodation of less than ten predictors in a multivariable regression analysis under an assumed AKI incidence of at least 20%.
Propensity score matching (PSM) was used to minimize confounding bias and promote comparability between groups. We corrected for variables in Table 1 that differed in baseline characteristics and still had an effect on outcome events after multifactorial regression analysis. The final variables, including atrial fibrillation, creatinine, heart rate, and blood magnesium, were included in the model as matched variables. A 1:3 ratio, greedy nearest-neighbor matching, and no replacement were used. Matching was performed with a caliper of 0.2 on the PS to eliminate bias and compensate for the effect of potential confounders. Standardized mean difference (SMD) was used to compare baseline characteristics between the two groups.
The TyG index was calculated based on triglyceride (TG) and fasting blood glucose (FBG) concentrations using the formula: \(\text{T}\text{y}\text{G}=\text{L}\text{n}\frac{\text{T}\text{G} (\text{m}\text{g}/\text{d}\text{L})\text{*} \text{F}\text{B}\text{G} (\text{m}\text{g}/\text{d}\text{L})}{2}\). We divided the population into four groups based on the magnitude of TyG levels. The first group was the reference group. To evaluate the relationship between TyG index and AKI risk, univariate and multivariate logistic regression analyses were performed before and after PSM. Model 1 included only TyG without any other adjustment. In model 2, sex, age and vital signs from Table 1 were added for adjustment. Model 3 was further adjusted for medications and comorbidities. Model 4 was additionally adjusted for laboratory test results. In addition, restricted cubic spline (RCS) regression was used to assess a possible nonlinear relationship between TyG level and AKI risk. Age, sex, atrial fibrillation, type 2 diabetes mellitus, and hypertension status were adjusted in the subgroup analysis.
R software (version 4.3.1) was used for statistical analysis, and GraphPad Prism (version 8.3.0) to generate graphs. All statistical tests were two-tailed, and P values less than 0.05 were considered statistically significant.
Results
Baseline characteristics
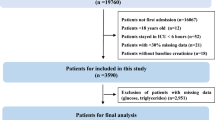
A total of 1831 patients with AMI were included into this study (Fig. 1). AKI presented in 302 (15.6%) patients. Before PSM, age and sex ratios were not different between the AKI and non-AKI groups (P = 0.066, P = 0.442) (Table 1). According to the non-AKI group, the AKI group had a faster heart rate, and lower overall blood pressure, incidence of shortness of breath, consumption of clopidogrel and renin-angiotensin-aldosterone system (RAAS) inhibitors (Pall < 0.05), as well as a higher rate of AF (P = 0.005). Other baseline characteristics of the patients are shown in Tables 1 and 2.
Relationship between TyG level and AKI risk
Before PSM, the mean TyG index was higher in the AKI group than in the non-AKI group (9.30 ± 0.71 mg/mL vs. 9.03 ± 0.73 mg/mL, P < 0.001). Table 3 shows the risk of AKI in patients with different quartiles of TyG levels. Four adjusted logistic models were constructed. Patients were divided into four categories according to TyG levels: Q1 (TyG ≤ 8.624 mg/mL), Q2 (8.624 mg/mL < TyG ≤ 9.030 mg/mL), Q3 (9.030 mg/mL < TyG ≤ 9.506 mg/mL), and Q4 (TyG > 9.506 mg/mL). A high TyG level increased the risk of AKI in adjusted terms (OR adjusted = 1.499, 95% CI 1.211–1.856) (Table 3). Compared with that in Q1 with the lowest TyG levels, the risks of AKI increased significantly in Q3 and Q4 adjusted (OR unadjusted = 2.535, 95% CI: 1.751–3.670, Ptrend < 0.001 for Q 4 vs. Q 1; OR model4 = 2.139, 95% CI: 1.382–3.310, for Q4 vs. Q1, Ptrend < 0.001) (Table 3). Specifically, the risk of AKI increased by 34.4% when the TyG level increased by 1 S.D. (OR = 1.344, 95%CI: 1.150–1.570, P < 0.001) (Table 3) after multivariate adjustment. A restricted RCS model revealed a non-linear relationship between TyG level and AKI risk. When the TyG level was greater than the cutoff value (approximately equal to 9 mg/mL), the AKI risk increased significantly with the TyG level (Fig. 2).
Subgroup analysis
A subgroup analysis was performed to confirm the relationship between TyG level and AKI risk in subgroups stratified by age, sex, atrial fibrillation, hypertension, and type 2 diabetes (Fig. 3). The study found that a higher TyG index was associated with an increased risk of AKI.
PSM analysis
Finally, 838 patients without AKI were PS-matched to 301 patients with AKI. The balance between the groups was checked (Fig. 4). After matching, the variables were less significantly different from the baseline before matching. Tables 1 and 2 show the matched data characteristics between the AKI and non-AKI groups.
Paired groups underwent logistic regression analysis. After PS matching and multivariate adjustment, the risk of AKI increased by 36.3% when the TyG index increased by 1 S.D. (OR = 1.363, 95% CI: 1.153–1.611, P < 0.001) (Supplementary Table 1). TyG index similarly increased the risk of AKI in the adjusted cohort (OR adjusted =1.546, 95% CI: 1.222–1.956); a higher TyG level was also associated with a higher risk of AKI in the adjusted matched cohort (OR adjusted = 2.206, 95% CI: 1.388–3.504 for Q 4 vs. Q 1, Ptrend = 0.001) (supplementary Table e1).
Subgroup analysis
Subgroup analyses were performed according to age, sex, atrial fibrillation, type 2 diabetes, and hypertension. It was further demonstrated that a high TyG index was associated with an increased risk of AKI in each subgroup (Fig. 5).
Discussion
In the current study, we found that within a certain range, the risk of AKI increased with the TyG level in AMI patients. We found that the incidence of AKI in AMI patients was 15.6%, similar to those reported in previous studies [9,10,11]. Independent predictors of AKI included heart rate, base excess, total carbon dioxide, serum magnesium, atrial fibrillation and TyG index.
AMI patients are prone to concurrent AKI, and the specific pathological mechanism is not fully understood, but suspected to involve renal hypoperfusion, inflammation and endothelial injury [35, 36]. AKI also increases the incidence of renal and cardiovascular adverse events [37]. Atrial fibrillation has been reported to increase the risk of renal replacement therapy in patients with AMI, and subsequent in-hospital mortality [38]. Several studies have shown that lower or higher serum magnesium levels also increased the risk of AKI [39,40,41,42,43]. Indicators, such as heart rate, residual base and total carbon dioxide, may predict early shock, and are closely associated with the risks of renal and cardiovascular adverse events and death [44].
Through multivariate regression analysis and subgroup analysis, we found that the TyG index was independently associated with the risk of AKI, either before or after PSM. The TyG index can serve as a simple predictor for assessing the extent of IR, which is strongly associated with kidney damage [45]. The mechanism accounting for this relationship is not fully understood, but may be explained by the lipid accumulation in the kidney due to IR [46]. Renal lipid accumulation and subsequent lipotoxicity can damage renal structure and function [47,48,49], mainly manifested by an increase in oxidative stress mediated by hydrogen peroxide and superoxide [50,51,52]. In addition, nephrolipotoxicity not only causes AKI but also drives the progression of chronic kidney disease [53]. Some studies have reported that the visceral adiposity index [54] can also be considered as an indicator of IR, and that IR resistance is closely associated with various disorders of glucose and lipid metabolism, such as hyperglycaemia, dyslipidaemia and hypertension, mitral annular calcification and cardiovascular prognosis [55, 56]. Therefore, resolving IR or hyperinsulinemia is expected to effectively reduce the risk of AKI in AMI patients. However, there still lack studies at the cellular and animal levels and multicentre prospective clinical trials with large sample sizes and long-term follow-ups.
Our findings have profound implications in clinical practice. In our study, a higher TyG index was associated with an increased risk of AKI in a specific AMI population, suggesting that the TyG index may be a valuable tool for risk stratification and clinical management. To reduce the AKI risk associated with high TyG levels, a comprehensive risk management approach can be adopted, involving active management of cardiovascular risk factors, such as lipid control, body mass index, fasting glucose and glycated haemoglobin, and smoking. Regular monitoring and timely intervention in patients with elevated TyG index levels are essential to reduce the occurrence of adverse outcomes.
However, this study is limited in several aspects. First, the sample size of this study was small and all subjects were not followed up in a short or long term to further clarify the effects of TyG index on renal function. Therefore, future studies with larger sample sizes and longer follow-up periods should be performed to provide stronger evidence to support our findings. Second, the MIMIC database has a high quality, but lacks the data about some clinical characteristics, such as contrast imaging and contrast use in patients with AMI, so our study could not adjust for all potential confounders.
Conclusions
A high TyG index level is associated with an increased risk of AKI in AMI patients. TyG index may be a valuable tool for risk classification and clinical management. Further studies are needed to confirm these results and determine the mechanism underlying the link between TyG index and AKI in AMI patients.
Data availability
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://physionet.org/content/mimiciii-demo/1.4/ and https://physionet.org/content/mimiciv/2.2/. In-hospital AKI diagnoses can also be accessed directly through the officially provided view codes https://github.com/MIT-LCP/mimic-code/.
References
Benjamin EJ, et al. Heart Disease and Stroke Statistics-2018 update: a Report from the American Heart Association. Circulation. 2018;137(12):e67–492.
Askin L, et al. Serum irisin: Pathogenesis and Clinical Research in Cardiovascular diseases. CVIA. 2020;4(3):195–200.
Nichols M, et al. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35(42):2929.
Yeh RW, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–65.
Murray CJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–91.
Murray CJ, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223.
Weintraub WS, et al. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation. 2011;124(8):967–90.
Bellomo R, et al. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):pR204–12.
Shacham Y, et al. Renal impairment according to acute kidney injury network criteria among ST elevation myocardial infarction patients undergoing primary percutaneous intervention: a retrospective observational study. Clin Res Cardiol. 2014;103(7):525–32.
Tsai TT, et al. Contemporary incidence, predictors, and outcomes of acute kidney injury in patients undergoing percutaneous coronary interventions: insights from the NCDR Cath-PCI registry. JACC Cardiovasc Interv. 2014;7(1):1–9.
Hwang SH, et al. Different clinical outcomes of acute kidney injury according to acute kidney injury network criteria in patients between ST elevation and non-ST elevation myocardial infarction. Int J Cardiol. 2011;150(1):99–101.
Chertow GM, et al. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35(6):1044–51.
Goldberg A, et al. Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J. 2005;150(2):330–7.
Hoste EA, et al. Acute renal failure in patients with sepsis in a surgical ICU: predictive factors, incidence, comorbidity, and outcome. J Am Soc Nephrol. 2003;14(4):1022–30.
de Mendonça A, et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 2000;26(7):915–21.
Thakar CV, et al. Influence of renal dysfunction on mortality after cardiac surgery: modifying effect of preoperative renal function. Kidney Int. 2005;67(3):1112–9.
Forman DE, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43(1):61–7.
Lassnigg A, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004;15(6):1597–605.
Chen CL, et al. Association between triglyceride glucose index and risk of New-Onset diabetes among Chinese adults: findings from the China Health and Retirement Longitudinal Study. Front Cardiovasc Med. 2020;7:610322.
Hill MA, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism. 2021;119:154766.
Jin JL, et al. Triglyceride glucose and haemoglobin glycation index for predicting outcomes in diabetes patients with new-onset, stable coronary artery disease: a nested case-control study. Ann Med. 2018;50(7):576–86.
Jin JL, et al. Triglyceride glucose index for predicting cardiovascular outcomes in patients with coronary artery disease. J Thorac Dis. 2018;10(11):6137–46.
Wang L, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. 2020;19(1):80.
Martínez-García G, et al. Triglyceride-glucose index impact on in-hospital mortality in acute myocardial infarction. Results from the RECUIMA multicenter registry. Gac Med Mex. 2022;158(2):83–9.
Hao Q, Yuanyuan Z, Lijuan C. The Prognostic Value of the triglyceride glucose index in patients with Acute myocardial infarction. J Cardiovasc Pharmacol Ther. 2023;28:10742484231181846.
Guo W, et al. The prognostic value of the triglyceride glucose index in patients with chronic heart failure and type 2 diabetes: a retrospective cohort study. Diabetes Res Clin Pract. 2021;177:108786.
Cai D, et al. Predicting acute kidney injury risk in acute myocardial infarction patients: an artificial intelligence model using medical information mart for intensive care databases. Front Cardiovasc Med. 2022;9:964894.
Sun L, et al. [Effects of hemoglobin level on the risk of acute kidney injury in patients with acute myocardial infarction]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2022;34(12):1243–7.
Zhou X, et al. Development and validation of Nomogram to Predict Acute kidney Injury in patients with Acute myocardial infarction treated invasively. Sci Rep. 2018;8(1):9769.
Sun L, et al. Machine learning to predict contrast-Induced Acute kidney Injury in patients with Acute myocardial infarction. Front Med (Lausanne). 2020;7:592007.
Han YQ, et al. Red blood cell distribution width provides additional prognostic value beyond severity scores in adult critical illness. Clin Chim Acta. 2019;498:62–7.
Kellum JA, Lameire N. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care. 2013;17(1):204.
Kuo, P.J., et al., Inhalation of volatile anesthetics via a laryngeal mask is associated with lower incidence of intraoperative awareness in non-critically ill patients. PLoS One. 2017;12(10):e0186337.
Bagdade JD, Albers JJ. Plasma high-density lipoprotein concentrations in chronic-hemodialysis and renal-transplant patients. N Engl J Med. 1977;296(25):1436–9.
Heyman SN, et al. Reactive oxygen species and the pathogenesis of radiocontrast-induced nephropathy. Invest Radiol. 2010;45(4):188–95.
Tanık VO, et al. Neutrophil-to-lymphocyte ratio predicts contrast-Induced Acute kidney Injury in patients with ST-Elevation myocardial infarction treated with primary percutaneous coronary intervention. J Tehran Heart Cent. 2019;14(2):59–66.
Zarbock A, et al. Sepsis-associated acute kidney injury: consensus report of the 28th Acute Disease Quality Initiative workgroup. Nat Rev Nephrol. 2023;19(6):401–17.
Marenzi G, et al. Renal replacement therapy in patients with acute myocardial infarction: rate of use, clinical predictors and relationship with in-hospital mortality. Int J Cardiol. 2017;230:255–61.
Li Q, et al. Analysis of the short-term prognosis and risk factors of elderly acute kidney injury patients in different KDIGO diagnostic windows. Aging Clin Exp Res. 2020;32(5):851–60.
Koh HB, et al. Preoperative ionized magnesium levels and risk of Acute kidney Injury after Cardiac surgery. Am J Kidney Dis. 2022;80(5):629–e6371.
Li Q, Zhao M, Zhou F. Hospital-acquired acute kidney injury in very elderly men: clinical characteristics and short-term outcomes. Aging Clin Exp Res. 2020;32(6):1121–8.
Shen D, et al. The effect of admission serum magnesium on the Acute kidney Injury among patients with malignancy. Cancer Manag Res. 2020;12:7199–207.
Cheungpasitporn W, Thongprayoon C, Erickson SB. Admission hypomagnesemia and hypermagnesemia increase the risk of acute kidney injury. Ren Fail. 2015;37(7):1175–9.
Tarvasmäki T, et al. Acute kidney injury in cardiogenic shock: definitions, incidence, haemodynamic alterations, and mortality. Eur J Heart Fail. 2018;20(3):572–81.
Tahapary DL, et al. Challenges in the diagnosis of insulin resistance: focusing on the role of HOMA-IR and Tryglyceride/glucose index. Diabetes Metab Syndr. 2022;16(8):102581.
Supruniuk E, Mikłosz A, Chabowski A. The implication of PGC-1α on fatty acid transport across plasma and mitochondrial membranes in the insulin sensitive tissues. Front Physiol. 2017;8:923.
Cobbs A, et al. Saturated fatty acid stimulates production of extracellular vesicles by renal tubular epithelial cells. Mol Cell Biochem. 2019;458(1–2):113–24.
Muller CR, et al. Post-weaning exposure to High-Fat Diet induces kidney lipid Accumulation and function impairment in adult rats. Front Nutr. 2019;6:60.
Munusamy S, et al. Obesity-induced changes in kidney mitochondria and endoplasmic reticulum in the presence or absence of leptin. Am J Physiol Ren Physiol. 2015;309(8):F731–43.
Krieger-Brauer HI, Kather H. Human fat cells possess a plasma membrane-bound H2O2-generating system that is activated by insulin via a mechanism bypassing the receptor kinase. J Clin Invest. 1992;89(3):1006–13.
Xu L, Badr MZ. Enhanced potential for oxidative stress in hyperinsulinemic rats: imbalance between hepatic peroxisomal hydrogen peroxide production and decomposition due to hyperinsulinemia. Horm Metab Res. 1999;31(4):278–82.
Kashiwagi A, et al. Endothelium-specific activation of NAD(P)H oxidase in aortas of exogenously hyperinsulinemic rats. Am J Physiol. 1999;277(6):E976–83.
Escasany E, Izquierdo-Lahuerta A, Medina-Gomez G. Underlying mechanisms of renal lipotoxicity in obesity. Nephron. 2019;143(1):28–32.
Gökalp G, Özbeyaz NB. The relationship between visceral adipose index and resistant hypertension in people living with diabetes. Postgrad Med. 2023;135(5):524–9.
Aydınyılmaz F et al. Effect of Atherogenic Index of Plasma on Pre-Percutaneous Coronary Intervention Thrombolysis in Myocardial Infarction Flow in Patients With ST Elevation Myocardial Infarction. Angiology, 2023: p. 33197231185204.
Gökalp G, Özbeyaz NB, Özilhan MO. Evaluation of the relationship between mitral annular calcification and triglyceride-glucose index. J Health Sci Med, 2023.
Acknowledgements
Thanks to all authors for their contributions in this study.
Funding
This study was supported by grants from National Natural Science Foundation of China (Grant No.82270328), Changzhou High-Level Medical Talents Training Project (2022CZBJ054), Natural Science Foundation of Jiangsu Province (BK20221229), Technology Development Fund of Nanjing Medical University (NMUB2020069), Major Research plan of Changzhou Health Commission of Jiangsu Province of China (ZD202215), Changzhou Sci&Tech Program (CE20225051) and China Postdoctoral Science Funding Program (2022M720544), Major Research plan of Wannan Medical College (WK2022F19), and Major Research plan of Anhui Education Commission (KJ2021A0822).
Author information
Authors and Affiliations
Contributions
DC and TX analyzed the data and wrote the paper. QC, QG and YW collect data. DC, TX, YW, QC and QG checked the integrity of the data and the accuracy of the data analysis. YJ, JW, LS and QW co-designed and revised this article. All authors read and approved the final manuscript for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Beth Israel Women’s Deaconess Medical Center and the MIT Institutional Review Board. The ethics committee waived the requirement of written informed consent for participation. We completed online courses and exams and gained access to the database (record IDs: 44703031 and 44703032).
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cai, D., Xiao, T., Chen, Q. et al. Association between triglyceride glucose and acute kidney injury in patients with acute myocardial infarction: a propensity score‑matched analysis. BMC Cardiovasc Disord 24, 216 (2024). https://doi.org/10.1186/s12872-024-03864-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03864-5