Abstract
Background
Approximately 90% of intracardial thrombi originate from the left atrial appendage in non-valvular atrial fibrillation patients. Even with anticoagulant therapy, left atrial appendage thrombus (LAAT) still occurs in 8% of patients. While left atrial appendage closure (LAAC) could be a promising alternative, the current consensus considers LAAT a contraindication to LAAC. However, the feasibility and safety of LAAC in patients with LAAT have yet to be determined.
Methods
This systematic review synthesizes published data to explore the feasibility and safety of LAAC for patients with LAAT.
Results
This study included a total of 136 patients with LAATs who underwent successful LAAC. The Amulet Amplatzer device was the most frequently utilized device (48.5%). Among these patients, 77 (56.6%) had absolute contraindications to anticoagulation therapy. Cerebral protection devices were utilized by 47 patients (34.6%). Transesophageal echocardiography (TEE) is the primary imaging technique used during the procedure. Warfarin and novel oral anticoagulants were the main anticoagulant medications used prior to the procedure, while dual antiplatelet therapy was primarily used post-procedure. During a mean follow-up period of 13.2 ± 11.5 months, there was 1 case of fatality, 1 case of stroke, 3 major bleeding events, 3 instances of device-related thrombus, and 8 cases of peri-device leakage.
Conclusions
This review highlights the preliminary effectiveness and safety of the LAAC procedure in patients with persistent LAAT. Future large-scale RCTs with varied LAAT characteristics and LAAC device types are essential for evidence-based decision-making in clinical practice.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is a rapid supraventricular arrhythmia characterized by irregular electrical activity and ineffective atrial contractions. The incidence of AF gradually increases with age and has emerged as a significant public health concern [1]. Stroke, as one of the severe complications of AF, often results in cardioembolic events that are not only severe but also have a high risk of recurrence. These strokes are frequently fatal or lead to permanent disability [2]. AF is associated with a 4- to fivefold increased risk of ischemic stroke and accounts for 25% of the 700 000 cerebrovascular accidents that occur in the United States annually [3]. Finding effective strategies to mitigate the risk of stroke associated with AF has become a crucial concern for cardiovascular physicians.
In patients with nonvalvular AF, approximately 90% of intracardiac thrombi originate from the left atrial appendage (LAA). Existing evidence indicates that the majority of strokes in patients with AF result from embolization of the left atrial appendage thrombus (LAAT) [4]. Oral anticoagulant (OAC) therapy is currently the primary approach for preventing and treating thrombosis associated with AF [5]. Despite anticoagulant treatment, LAAT still occurs in 8% of patients [6]. Moreover, a comprehensive assessment of the risk of drug-related bleeding is crucial for patients with renal dysfunction or active bleeding before initiating anticoagulant therapy. These factors limit the utilization of OACs.
For patients contraindicated for OAC therapy, a dilemma arises owing to the increased bleeding risk associated with OAC therapy and the consistently high risk of thrombosis resulting from LAAT. In such cases, the left atrial appendage closure (LAAC) procedure has emerged as a promising alternative. Recent clinical trials have established that LAAC procedure is not only noninferior to OAC therapy in terms of preventing thromboembolic events but also offers a significant reduction in bleeding complications. Furthermore, it is important to note that studies, such as the one published in JAMA 2014, have demonstrated a survival benefit for LAAC patients. This benefit, which was initially observed to be non-significant, became increasingly pronounced over the years, providing compelling evidence for the long-term efficacy of LAAC procedure over OAC therapy in certain patient populations [7, 8]. Previously, the presence of LAAT was considered a contraindication for LAAC, and landmark clinical trials on LAAC did not include this specific patient population [9,10,11]. The effectiveness and safety of LAAC in patients with LAAT have not been validated. However, recent studies have revealed that LAAC can effectively prevent stroke events in patients with LAAT, with minimal procedural complications [12, 13]. These findings suggest that LAAT may not be an absolute contraindication for LAAC. Currently, there are limited available data on the use of LAAC for patients with LAATs [14]. This systematic review compiles the most recent relevant studies to explore the feasibility and safety of LAAC in patients with LAAT.
Methods
Search strategy
This systematic review examined the available data on AF patients who underwent LAAT and LAAC procedures. A comprehensive search covering the period from January 1, 2000, to June 1, 2023, was conducted in the PubMed, EMBASE, Google Scholar, and SpringerLink databases to identify all relevant abstracts or full-text cases of LAAC in patients with LAAT. The search terms "left atrial appendage occlusion" OR "LAAO" OR "left atrial appendage closure" OR "LAAC" OR "Watchman" OR "Watchman-Flex" OR "Amplatzer cardiac plug" OR "ACP" OR "Amulet" and "left atrial appendage thrombus" were used to identify relevant articles. A manual search of the selected articles and relevant references in published reviews was performed to ensure comprehensive data collection.
Data extraction and statistical analysis
Studies and abstracts reporting cases of LAAC device placement in patients with LAAT were included in our analysis. We excluded articles lacking detailed procedures and essential follow-up data. Non-English language articles were also excluded. Clinical follow-up data, including thromboembolic events, major bleeding events, device-related thrombus (DRT), peri-device leakage (PDL), complications related to the closure device, transient ischemic attack, death and the use of anticoagulation or antiplatelet therapies, were collected from each study. Following a successful LAAC procedure, the physician decided to discontinue anticoagulation therapy and switch to antiplatelet agents. Continuous data are expressed as the mean ± standard deviation (M ± SD) for normally distributed variables or as the median (25th, 75th percentiles) for non-normally distributed variables. A statistical analysis using IBM SPSS version 26 was performed to analyze the pooled data. The study selection process is represented in Fig. 1.
Definition of terms
Device success was defined as the deployment of the occluder in the correct position with < 5 mm of a PDL. Adverse clinical outcomes included a composite of death, stroke or other systemic thromboembolism, DRT, major bleeding, PDL, transient ischemic attack and device-related complications during follow-up. Major bleeding events included gastrointestinal bleeding, cerebral hemorrhage, intramuscular bleeding, or active bleeding directly related to the OAC therapy. PDL refers to postprocedural leakage exceeding 5 mm. A DRT was defined as a thrombus that formed on the LAAC device. Anticoagulation therapy after the procedure includes warfarin or novel oral anticoagulants (NOACs).
Types of LAAC devices
The commonly used LAAC devices include Watchman, Watchman FLX, Amplatzer Cardiac Plug (ACP), Amulet Amplatzer, and Lambre devices. The Watchman device (Boston Scientific, MA) is the most extensively studied percutaneous LAAC device. It consists of a self-expanding nitinol frame with fixation anchors and is covered with a polyethylene terephthalate fabric membrane on the proximal face [15]. The implantation procedure typically involves a standard transseptal puncture after femoral vein access. Subsequently, the 14F Watchman Access Sheath is exchanged using a guidewire, and the pigtail catheter is used to deliver the device into the LAA. The release of the device must meet the "PASS" criteria [16].
The ACP is a dual-disc LAAC device that structurally resembles the Amplatzer atrial septal occluder. The distal disc is placed in the LAA to prevent displacement, while the proximal disc cap seals the orifice of the LAA. The Amulet Amplatzer device is a second-generation LAAC device based on the ACP design. Compared to the ACP, the Amulet Amplatzer device incorporates additional anchoring hooks, a deeper distal lobe, a longer waist, and a recessed distal screw to minimize exposed metal within the LAA and subsequently reduce the incidence of DRT [17].
Lifetech received CE Mark approval for the LAmbre closure system on 15 June 2016. The closure system has a double umbrella design with two layers of polyethylene terephthalate fabric in the cover and umbrella. The implant is a nitinol-based, self-expanding device comprising a hook-embedded umbrella with a short central waist. The waist acts as an articulating, compliant connection between the cover and the umbrella, allowing the cover to self-orient the cardiac wall [18].
Results
Baseline characteristics
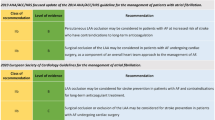
We conducted a comprehensive analysis of 136 patients from 26 publications. The median age was 64 years, and 86 (63.2%) of the patients were male. The most common comorbidities observed were hypertension (36%) and diabetes (36.8%). Permanent AF accounted for approximately 53.7% of the patients. A total of 47 patients (34.6%) received implantation of a cerebral protection device (CPD). The most frequently used device was the Amulet Amplatzer (48.5%), and Fig. 2 provides an overview of the types of LAAC devices used. Among the patients, 43.3% had absolute contraindications to anticoagulation therapy due to the risk of major bleeding, while 56.7% of patients had relative contraindications due to experienced thromboembolic events despite receiving OAC treatment or declining to adhere to anticoagulant medication. The detailed baseline characteristics of the patients are presented in Table 1.
Antiplatelet and anticoagulation therapy
Comparing the preprocedural and postprocedural antiplatelet and anticoagulation strategies for LAAC, it was noted that NOACs (38.1%) and warfarin (31%) were the primary OACs used before the procedure. Although the current guidelines do not recommend the use of antiplatelet drugs alone for the prevention or treatment of AF-related embolism, some patients still receive aspirin or clopidogrel as their OAC strategy. Dual antiplatelet therapy (DAPT) emerged as the most common postprocedural treatment approach and accounted for 40.3% of the patients. Detailed information about antiplatelet and anticoagulation therapy is presented in Fig. 3.
Procedural characteristics
In all patients, the occluder was successfully positioned in the correct location. While the majority of procedures adhered to a standard protocol, modifications were made in some cases to enhance safety, particularly in the presence of LAAT. These included the utilization of the 'no-touch technique', which is especially critical in avoiding manipulation within the LAA using any sheath, catheter, or guidewire. It is also important to note that the customary practice of employing a pigtail catheter for local injection in LAAC is contraindicated in these scenarios. This is due to the risks posed by retracting the pigtail catheter before the introduction of the LAAC device. Detailed descriptions of these procedural modifications are provided in Table 2.
Follow-up and clinical outcomes
The mean follow-up duration was 13.2 ± 11.5 months. Seven studies reported 16 cases (11.8%) of adverse clinical outcomes, and all patients who underwent CPD implantation were free from stroke events during both hospitalization and follow-up. PDL was the most common adverse clinical outcome, occurring in 8 patients (5.9%). Of these, six patients exhibited PDL measurements ≤ 3 mm, while two had measurements exceeding 5 mm. None of these patients underwent a secondary LAAC. DRT was reported in three patients (2.2%), all of whom were successfully managed with OACs. Major bleeding events were also documented in three patients (2.2%). One patient (0.7%), a 54-year-old male with persistent AF and a CHA2DS2-VASC score of 3, underwent ACP implantation without the use of a CPD. Subsequently, the patient experienced a stroke during the follow-up. Moreover, one patient (0.7%) died due to the progression of heart failure. The detailed data concerning the follow-up and clinical outcomes are presented in Table 3.
Discussion
This is a comprehensive systematic review of publications detailing LAAC procedures in patients presenting with LAAT. The main findings of this study were as follows: (i) The Amulet Amplatzer is currently the most commonly used LAAC device in patients with LAATs. (ii) Preprocedural OAC therapy and postprocedural DAPT are the main anticoagulation strategies for LAAT patients undergoing LAAC procedures, as these patients have a low rate of postprocedural stroke and DRT. (iii) The use of a no-touch technique, avoiding additional probing within the LAA, contributes to the safety of LAAC procedures. (iv) PDL is the most common adverse clinical outcome after LAAC procedures in LAAT patients; however, the overall incidence of adverse events is low. (v) While the combination of CPD with the LAAC procedure is associated with a low incidence of postprocedural stroke, the currently widespread implementation of CPD remains limited. In conclusion, the LAAC procedure is associated with preliminary effectiveness and safety in patients with persistent LAATs (Fig. 4).
Graphical abstract for LAAC in the treatment of LAAT. ACP, Amplatzer cardiac plug; DAPT, dual antiplatelet therapy; LAAC, left atrial appendage closure; LAAT, left atrial appendage thrombus; LMWH, low-molecular-weight heparin; NOACs, novel oral anticoagulants; SAPT, single antiplatelet therapy; TEE, transesophageal echocardiography; VKA, vitamin K antagonist
AF is associated with a 4- to fivefold increased risk of ischemic stroke. The annual stroke risk in patients with AF ranges from 0.5% to 9.3%, and approximately 15% of ischemic strokes are attributed to AF [43, 44]. Chronic AF often remains asymptomatic and can go undetected in clinical practice, resulting in an underestimation of stroke risk. OAC therapy is regarded as the cornerstone for stroke prevention in patients with AF, and these agents are commonly prescribed prior to the LAAC procedure. To date, the specific treatment effect of NOACs on the formation of intracardiac thrombi has not been extensively investigated in large-scale randomized controlled trials (RCTs). However, preliminary evidence from case series and reports suggests that NOACs may represent a safe and effective option for treating intracardiac thrombus, particularly in cases where warfarin has been shown to be ineffective [45]. Furthermore, Nelles et al. [46] conducted a study that demonstrated LAAT resolution rates comparable between warfarin and NOACs, with NOACs resulting in a shorter time to thrombus resolution. Nevertheless, it is crucial to acknowledge that OACs cannot entirely eliminate LAAT [19]. For patients with persistent LAAT despite OAC therapy or those with contraindications to OAC therapy, the LAAC procedure emerges as a potential and viable alternative. Traditionally, LAAT has been considered a contraindication for LAAC. However, studies by Sharma et al. [14] indicate that LAAC may be a feasible option for patients with LAAT. By challenging traditional contraindications, LAAC offers additional treatment options for patients with persistent LAAT.
Procedural embolization is a severe complication that can occur during LAAC in patients with LAAT. Catheter manipulation within the LAA can potentially dislodge or detach the LAAT, leading to stroke or peripheral embolization events. For patients with LAATs, the combination of the no-touch technique can greatly enhance the safety of the procedure in addition to standard deployment techniques [20]. The no-touch technique involves minimizing guidewire or catheter manipulation within the LAA by loading the closure device with the delivery sheath in the left superior pulmonary vein [19]. Lange et al. [21] proposed using transesophageal echocardiography (TEE) to measure the diameter of the partially opened occluder and compared it to the size of the middle part of the LAA. The release of the device was continued until the diameter of the opened corpus of the occluder was greater than the measured value. This approach helps prevent deeper protrusion of the device into the LAA and reduces the risk of procedure-related thrombus dislodgement. While the "no-touch" technique has demonstrated encouraging outcomes in certain patients, its intricate procedure requires a sophisticated understanding of the LAA anatomy and highly skilled maneuvering of the devices. This complex procedure restricts its wide implementation, making it seemingly impractical for novice operators. Despite the promise of reduced complications and increased closure efficacy, the technical difficulty lies in delicate navigation and precise device placement within the complex and highly variable anatomy of the LAA.
CPD was originally proposed and developed in transcatheter aortic valve replacement (TAVR) and has been linked to a notable reduction in cerebral ischemic burden [47]. Although the PROTECTED TAVR study [48] revealed that the use of the Sentinel device (the first TAVR intraoperative CPD approved by the United States Food and Drug Administration) did not decrease the incidence of clinical stroke during the TAVR periprocedural period, it did report a decreased occurrence of disabling strokes. Recent prospective studies and case reports have indicated that the combined use of LAAC and cerebral protection systems is a safe and effective treatment option for patients with LAAT [22, 49, 50]. It is important to highlight that the majority of the current research involved organized and securely attached LAATs within the fundus of the LAA. This finding underlines a key limitation in the current literature and practice. Significantly, even with the use of CPDs, an LAAT protruding out of the LAA remains a strict contraindication for LAAC due to the high risk associated with its potential mobility. Furthermore, we address complex scenarios involving thrombi located at the neck of the LAA. When these thrombi exhibit any degree of mobility, they present a considerable challenge, leading most interventional cardiologists to prudently avoid attempting LAAC in such cases. In the future, large-scale RCTs investigating the use of LAAC in combination with cerebral protection systems for stroke prevention in LAAT patients may provide further clinical evidence.
Cardiac imaging plays a crucial role in LAAC procedures. The data presented in this systematic review indicate that TEE is the most frequently utilized modality for procedural imaging. TEE is considered the gold standard for diagnosing LAATs [51], with a positive predictive value of 100%, a negative predictive value of 98.9%, and a diagnostic accuracy of 99.1% [52]. Traditional 2D TEE has limitations in accurately assessing LAA function. Real-time 3D TEE is a valuable tool that minimizes artifact interference and enables a more precise analysis of the association between LAA functional parameters and LAAT [53]. However, 3D technology is limited by its lower spatial and temporal resolution than 2D TEE [54]. Intracardiac echocardiography (ICE) is an efficient alternative to TEE for visualizing cardiac structures [55]. A study conducted by Nielsen-Kudsk et al. demonstrated the successful utilization of ICE as a guide for LAAC with the Watchman FLX device. The study reported excellent procedural success, a high rate of effective LAAC, and minimal periprocedural complications [56]. In a porcine model, both ICE and TEE demonstrated similar imaging capabilities for visualizing LAAT. However, in patients with AF, ICE imaging showed lower sensitivity in detecting LAAT than did TEE [57, 58]. Considering the potential interaction between ICE and the LAAC sheath during the procedure and its typical supplementation with LAA angiography [14], the use of ICE in patients with LAAT should be performed by experienced operators who have conducted a minimum of 20 LAAC procedures per year.
Limitations
This study has several limitations. 1) The retrospective design of this study introduces inherent known and unknown selection biases. Additionally, publication bias and outcome reporting bias may significantly influence the conclusions of our review. 2) The purpose of this study was primarily to assess the feasibility of LAAC in patients with LAAT. The applicability of these findings may be limited to experienced operators. 3) A notable limitation is the lack of detailed descriptions of LAAT characteristics in the included reports. The size, location, morphology, or mobility of LAATs significantly impacts the implantation and efficacy of LAAC devices. This gap underscores the need for more detailed investigations into LAAT characteristics in future RCTs. 4) The absence of long-term follow-up data in our study limits the ability to assess the extended-term effectiveness and safety of LAAC in patients with LAATs.
Future directions
Targeted investigations are crucial for advancing the understanding of LAAC in patients with LAAT. Subsequent research should delve into detailed analyses of LAAT characteristics, including size or location, aiming to enhance procedural considerations. Long-term follow-up studies are needed to evaluate the efficacy of LAAC therapy. Moreover, there is a pressing need for comparative studies among different LAAC devices and well-designed RCTs to establish a higher level of evidence, offering clarity on the optimal approach for patients with LAATs. These future directions are geared toward refining clinical strategies and contributing to evidence-based decision-making in this specific patient population.
Conclusion
In conclusion, this comprehensive systematic review elucidates the prospects of LAAC procedures in patients with LAATs. The Amulet Amplatzer is the most commonly used LAAC device in LAAT patients, and it achieves procedural effectiveness and safety through the combination of preprocedural OAC therapy and postprocedural DAPT. The no-touch technique has emerged as a crucial measure for enhancing the overall safety of LAAC procedures. Despite PDL being the primary adverse outcome, the overall incidence of adverse events remains low. Additionally, the incidence of postprocedural stroke is lower in LAAT patients with implanted CPDs, and CPD implementation is not widespread in this patient population. Our findings underscore the potential utility of LAAC in patients with LAAT. Future large-scale RCTs with long-term follow-up focusing on different LAAT characteristics and various LAAC device types may provide higher-quality clinical evidence for patients, guiding evidence-based decision-making in clinical practice.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- ACP:
-
Amplatzer cardiac plug
- CPD:
-
Cerebral protection device
- DAPT:
-
Dual antiplatelet therapy
- DRT:
-
Device-related thrombus
- ICE:
-
Intracardiac echocardiography
- LAA:
-
Left atrial appendage
- LAAC:
-
Left atrial appendage closure
- LAAT:
-
Left atrial appendage thrombus
- LMWH:
-
Low-molecular-weight heparin
- LSPV:
-
Left superior pulmonary vein
- NOACs:
-
Novel oral anticoagulants
- OAC:
-
Oral anticoagulant
- PDL:
-
Peri-device leakage
- RCTs:
-
Randomized controlled trials
- SAPT:
-
Single antiplatelet therapy
- TAVR:
-
Transcatheter aortic valve replacement
- TEE:
-
Transesophageal echocardiography
References
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS focused update of the 2014 aha/acc/hrs guideline for the management of patients with atrial fibrillation: a report of the american college of cardiology/american heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019;140(2):e125–51.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan G-A, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau J-P, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56–528. https://doi.org/10.1161/CIR.0000000000000659.
Glikson M, Wolff R, Hindricks G, Mandrola J, Camm AJ, Lip GYH, Fauchier L, Betts TR, Lewalter T, Saw J, Tzikas A, Sternik L, Nietlispach F, Berti S, Sievert H, Bertog S, Meier B. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion - an update. Europace. 2020;22(2):184.
Lip GYH, Banerjee A, Boriani G, Chiang CE, Fargo R, Freedman B, Lane DA, Ruff CT, Turakhia M, Werring D, Patel S, Moores L. Antithrombotic Therapy for Atrial Fibrillation: CHEST Guideline and Expert Panel Report. Chest. 2018;154(5):1121–201.
Zhan Y, Joza J, AlRawahi M, Barbosa RS, Samuel M, Bernier M, Huynh T, Thanassoulis G, Essebag V. Assessment and Management of the Left Atrial Appendage Thrombus in Patients With Nonvalvular Atrial Fibrillation. Can J Cardiol. 2018;34(3):252–61.
Bajwa RJ, Kovell L, Resar JR, Arbab-Zadeh A, Mandal K, Calkins H, Berger RD. Left atrial appendage occlusion for stroke prevention in patients with atrial fibrillation. Clin Cardiol. 2017;40(10):825–31.
Reddy VY, Sievert H, Halperin J, Doshi SK, Buchbinder M, Neuzil P, Huber K, Whisenant B, Kar S, Swarup V, Gordon N, Holmes D. Percutaneous left atrial appendage closure vs warfarin for atrial fibrillation: a randomized clinical trial. JAMA. 2014;312(19):1988–98.
Holmes DR, Reddy VY, Turi ZG, Doshi SK, Sievert H, Buchbinder M, Mullin CM, Sick P. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009;374(9689):534–42.
Holmes DR, Kar S, Price MJ, Whisenant B, Sievert H, Doshi SK, Huber K, Reddy VY. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014;64(1):1–12.
Osmancik P, Herman D, Neuzil P, Hala P, Taborsky M, Kala P, Poloczek M, Stasek J, Haman L, Branny M, Chovancik J, Cervinka P, Holy J, Kovarnik T, Zemanek D, Havranek S, Vancura V, Opatrny J, Peichl P, Tousek P, Lekesova V, Jarkovsky J, Novackova M, Benesova K, Widimsky P, Reddy VY. Left Atrial Appendage Closure Versus Direct Oral Anticoagulants in High-Risk Patients With Atrial Fibrillation. J Am Coll Cardiol. 2020;75(25):3122–35.
Bordignon S, Bologna F, Chen S, Konstantinou A, Tsianakas N, Tohoku S, Trolese L, Chun KJ, Schmidt B. Percutaneous left atrial appendage closure in the presence of thrombus: A feasibility report. J Cardiovasc Electrophysiol. 2019;30(12):2858–63.
Jin L-S, Ke J-Y, Lin Y-N, Li L, Fu J-Y, Chen Y-L, Qiu Y-X, Li X-W, Pan Y-Q, Li Y-C. Percutaneous left atrial appendage closure using the LAmbre device in patients with atrial fibrillation and left atrial appendage thrombus. Front Cardiovasc Med. 2022;9:1071119.
Sharma SP, Cheng J, Turagam MK, Gopinathannair R, Horton R, Lam YY, Tarantini G, DAmico G, Freixa Rofastes X, Lange M, Natale A, Lakkireddy DR. Feasibility of left atrial appendage occlusion in left atrial appendage thrombus a systematic review. JACC Clin Electrophysiol. 2020;6(4):414–24.
Meier B, Blaauw Y, Khattab AA, Lewalter T, Sievert H, Tondo C, Glikson M. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion. Europace. 2014;16(10):1397–416.
Wintgens LIS, Maarse M, Swaans MJ, Rensing BJWM, Van Dijk VF, Boersma LVA. The WATCHMAN left atrial appendage closure device for patients with atrial fibrillation: current status and future perspectives. Expert Rev Med Devices. 2020;17(7):615–26.
Messas N, Ibrahim R. The Amplatzer Amulet Device: Technical Considerations and Procedural Approach. Interv Cardiol Clin. 2018;7(2):213–8.
Schnupp S, Ajmi I, Brachmann J, Mahnkopf C. Lifetech LAmbre: a new promising and novel device in the interventional stroke prevention. Future Cardiol. 2019;15(6):405–10.
Marroquin L, Tirado-Conte G, Pracoń R, Streb W, Gutierrez H, Boccuzzi G, Arzamendi-Aizpurua D, Cruz-González I, Ruiz-Nodar JM, Kim JS, Freixa X, Lopez-Minguez JR, De Backer O, Ruiz-Salmeron R, Dominguez A, McInerney A, Peral V, Estevez-Loureiro R, Fernandez-Nofrerias E, Freitas-Ferraz AB, Saia F, Huczek Z, Gheorghe L, Salinas P, Demkow M, Delgado-Arana JR. Heart. 2022;108(14):1098–106.
Beneduce A, Ancona F, Marzi A, Radinovic A, D’Angelo G, Agricola E, Della Bella P, Mazzone P. Percutaneous treatment of persistent left atrial appendage thrombus using watchman FLX no-touch implantation technique and cerebral protection system. JACC Clin Electrophysiol. 2019;5(10):1231–2.
Lange M, Bültel H, Weglage H, Löffeld P, Wichter T. Closure of Left Atrial Appendage With Persistent Distal Thrombus using an Amplatzer Amulet Occluder. J Invasive Cardiol. 2016;28(9):E75–6.
Saccà S, Ferro J, Umemoto T, Turri R, Penzo C, Pacchioni A. A New Strategy for Transcatheter Left Atrial Appendage Closure With Cerebral Embolic Protection in Patient With Left Auricular Thrombosis and Total Contraindication to Long-Term Anticoagulation. J Invasive Cardiol. 2017;29(3):E37–8.
Jalal Z, Iriart X, Dinet M-L, Selly J-B, Tafer N, Renou P, Sibon I, Thambo J-B. Extending percutaneous left atrial appendage closure indications using the AMPLATZER™ Cardiac Plug device in patients with persistent left atrial appendage thrombus: The thrombus trapping technique. Arch Cardiovasc Dis. 2016;109(12):659–66.
Lee O-H, Kim J-S, Pak H-N, Hong G-R, Shim CY, Uhm J-S, Cho I-J, Joung B, Yu C-W, Lee H-J, Kang W-C, Shin E-S, Choi R-K, Lim D-S, Jang Y. Feasibility of Left Atrial Appendage Occlusion for Left Atrial Appendage Thrombus in Patients With Persistent Atrial Fibrillation. Am J Cardiol. 2018;121(12):1534–9.
Popescu SȘ, Heeger C-H, Keelani A, Tilz RR. Percutaneous Left Atrial Appendage Closure with the LAmbre Device Protected by a Cerebral Protection System in a 76-Year-Old Man with Persistent Left Atrial Appendage Thrombus. Am J Case Rep. 2022;23:e937063.
Tan BEX, Depta JP. Transcatheter cerebral embolic protection during WATCHMAN procedure in two patients with persistent left atrial appendage thrombus: Case report with review of the literature. Catheter Cardiovasc Interv. 2021;97(2):365–8.
Tsai C-F, Huang P-S, Chiu F-C, Chen J-J, Chang S-N, Hsu J-C, Chua S-K, Cheng H-L, Wang Y-C, Hwang J-J, Tsai C-T. Bailout left atrial appendage occluder for pulmonary vein isolation and electrical cardioversion in patients with atrial fibrillation and left atrial appendage thrombus: a pilot study. Clin Res Cardiol. 2023;112(6):772–83.
Bellmann B, Rillig A, Leistner DM, Kasner M, Skurk C, Landmesser U, Park J-W. Left atrial appendage closure in a patient with left atrial appendage thrombus using a novel fish ball technique. Int J Cardiol. 2017;234:146–9.
Aytemir K, Aminian A, Asil S, Canpolat U, Kaya EB, Şahiner L, Evranos B, Yorgun H, Özer N. First case of percutaneous left atrial appendage closure by amulet™ device in a patient with left atrial appendage thrombus. Int J Cardiol. 2016;223:28–30.
Dugo D, Bordignon S, Konstantinou A, Perrotta L, Fürnkranz A, Chun JKR, Schmidt B. Locked Away: Percutaneous Closure of a Malignant Left Atrial Appendage to Constrain an Unresolvable Thrombus. Circ Arrhythm Electrophysiol. 2016;9(8):e004127.
Lee O-H, Uhm J-S, Kim J-S, Cho I-J, Hong G-R, Pak H-N, Jang Y. Percutaneous isolation of left atrial appendage thrombus. J Cardiol Cases. 2017;16(3):67–9.
De Roeck F, Scott B, Verheye S, Vermeersch P. Percutaneous left atrial appendage occlusion in a lamin A/C gene mutation related cardiomyopathy patient with persistent left atrial appendage thrombus: a case report. Acta Cardiol. 2019;74(2):182–3.
Chang D, Kapur S, Romero J, Koplan BA, Tadros TM. CE-454611–3 High risk left atrial appendage closure in patients with a persistent left atrial appendage thrombus. Heart Rhythm. 2023;20(5):S9–10.
Mohandes M, Pernigotti A, Morr CI, Bardají A. Percutaneous Left Atrial Appendage Closure in the Presence of Thrombus Using LAmbre Device and Cerebral Protection System. Korean Circ J. 2020;50(3):281–3.
Kaczmarek K, Cygankiewicz I, Streb W, Plaksej R, Jakubowski P, Kalarus Z, Ptaszynski P, Wranicz JK, Babicz-Sadowska A, Markiewicz A, Grygier M. Percutaneous Occlusion of the Left Atrial Appendage with Thrombus Irresponsive to Antithrombotic Therapy. J Clin Med. 2021;10(4):726. https://doi.org/10.3390/jcm10040726.
Marcon L, Sicuso R, Galli S, Majocchi B, Carbucicchio C, Tondo C, Fassini GM. TriGuard Embolic Protection Device in percutaneous cardiac interventions with intracavitary cardiac thrombosis: A case series. Pacing Clin Electrophysiol. 2024;47(1):106–12. https://doi.org/10.1111/pace.14712.
CruzGonzalez I, Fuertes M, Barahona, MorenoSamos JC, Barreiro-Perez M, Rodríguez-Collado J, Gonzalez-Calle D, Sanchez PL. Left Atrial appendage occlusion in the presence of Thrombus With a LAmbre device. JACC Cardiovasc Interv. 2017;10(21):2224–6.
Cammalleri V, Ussia GP, Muscoli S, De Vico P, Romeo F. Transcatheter occlusion of left atrial appendage with persistent thrombus using a trans-radial embolic protection device. J Cardiovasc Med (Hagerstown). 2016;17(Suppl 2):e224.
Pak H-N, Shim C-Y, Kim JS, Park J-W, Jang Y. Self-expandable device for percutaneous closing of left atrial appendage with organized thrombus in a patient with permanent atrial fibrillation. Can J Cardiol. 2013;29(10):1329.e1-1329.e3.
Yadav PK, Wang DD, Eng MH, O’Neill WW. Watchman in ascending aorta for systemic protection (WAASP): Novel use of Watchman in ascending aorta for embolic protection-first in man. Catheter Cardiovasc Interv. 2018;92(2):433–6.
Martins JL, Paiva L, Costa M, Gonçalves L. Thrombus in left atrial appendage - Overcoming percutaneous closure limitations. Rev Port Cardiol (Engl Ed). 2018;37(3):269–70.
Del Furia F, Ancona MB, Giannini F, Jabbour RJ, Regazzoli D, Mangieri A, Latib A, Colombo A, Montorfano M. First-in-man Percutaneous LAA Closure With an Amplatzer Amulet and TriGuard Embolic Protection Device in a Patient With LAA Thrombus. J Invasive Cardiol. 2017;29(4):E51–2.
Warden BA, Diep C, Ran R, Thomas M, Cigarroa JE. The effect of heparin infusion intensity on outcomes for bridging hospitalized patients with atrial fibrillation. Clin Cardiol. 2019;42(10):995–1002.
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, Beaton AZ, Boehme AK, Buxton AE, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Fugar S, Generoso G, Heard DG, Hiremath S, Ho JE, Kalani R, Kazi DS, Ko D, Levine DA, Liu J, Ma J, Magnani JW, Michos ED, Mussolino ME, Navaneethan SD, Parikh NI, Poudel R, Rezk-Hanna M, Roth GA, Shah NS, St-Onge M-P, Thacker EL, Virani SS, Voeks JH, Wang N-Y, Wong ND, Wong SS, Yaffe K, Martin SS. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation. 2023;147(8):e93–621.
Ghaffarpasand E, Tehrani MD, Marszalek J, Chi G. Non-vitamin K antagonist oral anticoagulants for the treatment of intracardiac thrombosis. J Thromb Thrombolysis. 2018;46(3):332–8.
Nelles D, Lambers M, Schafigh M, Morais P, Schueler R, Vij V, Tiyerili V, Weber M, Schrickel JW, Nickenig G, Hammerstingl C, Sedaghat A. Clinical outcomes and thrombus resolution in patients with solid left atrial appendage thrombi: results of a single-center real-world registry. Clin Res Cardiol. 2021;110(1):72–83.
Haussig S, Mangner N, Dwyer MG, Lehmkuhl L, Lücke C, Woitek F, Holzhey DM, Mohr FW, Gutberlet M, Zivadinov R, Schuler G, Linke A. Effect of a Cerebral Protection Device on Brain Lesions Following Transcatheter Aortic Valve Implantation in Patients With Severe Aortic Stenosis: The CLEAN-TAVI Randomized Clinical Trial. JAMA. 2016;316(6):592–601.
Kapadia SR, Makkar R, Leon M, Abdel-Wahab M, Waggoner T, Massberg S, Rottbauer W, Horr S, Sondergaard L, Karha J, Gooley R, Satler L, Stoler RC, Messé SR, Baron SJ, Seeger J, Kodali S, Krishnaswamy A, Thourani VH, Harrington K, Pocock S, Modolo R, Allocco DJ, Meredith IT, Linke A. Cerebral Embolic Protection during Transcatheter Aortic-Valve Replacement. N Engl J Med. 2022;387(14):1253–63.
Limite LR, Radinovic A, Cianfanelli L, Altizio S, Peretto G, Frontera A, D’Angelo G, Baratto F, Marzi A, Ancona F, Ingallina G, Capogrosso C, Stella S, Melillo F, Agricola E, Della Bella P, Mazzone P. Outcome of left atrial appendage closure using cerebral protection system for thrombosis: no patient left behind. Pacing Clin Electrophysiol. 2022;45(1):23–34.
Boccuzzi GG, Montabone A, D’Ascenzo F, Colombo F, Ugo F, Muraglia S, De Backer O, Nombela-Franco L, Meincke F, Mazzone P. Cerebral protection in left atrial appendage closure in the presence of appendage thrombosis. Catheter Cardiovasc Interv. 2021;97(3):511–5.
Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Kay GN, Le Huezey J-Y, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann LS. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57(11):e101–98.
Hwang JJ, Chen JJ, Lin SC, Tseng YZ, Kuan P, Lien WP, Lin FY, Chu SH, Hung CR, How SW. Diagnostic accuracy of transesophageal echocardiography for detecting left atrial thrombi in patients with rheumatic heart disease having undergone mitral valve operations. Am J Cardiol. 1993;72(9):677–81.
Li J, Li Q, Alqahtany FS, Algahtani FH, Kim HJ, Li Y, Ock Kim Y. Evaluating the novel parameters for assessing the LAA function and thrombus formation with nonvalvular atrial fibrillation. Saudi J Biol Sci. 2021;28(1):560–5.
Romero J, Cao JJ, Garcia MJ, Taub CC. Cardiac imaging for assessment of left atrial appendage stasis and thrombosis. Nat Rev Cardiol. 2014;11(8):470–80.
Baran J, Stec S, Pilichowska-Paszkiet E, Zaborska B, Sikora-Frąc M, Kryński T, Michałowska I, Łopatka R, Kułakowski P. Intracardiac echocardiography for detection of thrombus in the left atrial appendage: comparison with transesophageal echocardiography in patients undergoing ablation for atrial fibrillation: the Action-Ice I Study. Circ Arrhythm Electrophysiol. 2013;6(6):1074–81.
Nielsen-Kudsk JE, Berti S, Caprioglio F, Ronco F, Arzamendi D, Betts T, Tondo C, Christen T, Allocco DJ. Intracardiac Echocardiography to Guide Watchman FLX Implantation: The ICE LAA Study. JACC Cardiovasc Interv. 2023;16(6):643–51.
Hutchinson MD, Jacobson JT, Michele JJ, Silvestry FE, Callans DJ. A comparison of intracardiac and transesophageal echocardiography to detect left atrial appendage thrombus in a swine model. J Interv Card Electrophysiol. 2010;27(1):3–7.
Saksena S, Sra J, Jordaens L, Kusumoto F, Knight B, Natale A, Kocheril A, Nanda NC, Nagarakanti R, Simon AM, Viggiano MA, Lokhandwala T, Chandler ML. A prospective comparison of cardiac imaging using intracardiac echocardiography with transesophageal echocardiography in patients with atrial fibrillation: the intracardiac echocardiography guided cardioversion helps interventional procedures study. Circ Arrhythm Electrophysiol. 2010;3(6):571–7.
Code availability
Figure 4 was created using the image bank of Servier Medical Art (http://smart.servier.com), licensed under the Creative Commons Attribution 3.0 Unported License (https://creativecommons.org/licenses/by/3.0/).
Funding
This work was supported by the National Natural Science Foundation of China [No. 82070356, 81770337], the Key Project of Hunan Provincial Science and Technology Innovation [No. 2020SK1013], the Hunan Provincial Natural Science Foundation of China [No. 2021JJ30033, 2023JJ30791], the Clinical Medical Technology Innovation Guidance Project of Hunan Science and Technology Agency [No. 2021SK53519], the Changsha Municipal Natural Science Foundation [No. kq2208306], the Hunan Provincial Health Commission Scientific Research Project [No. 20201302], the Fundamental Research Funds for the Central Universities of Central South University [No. 2024ZZTS0878] and the National Natural Science Foundation of China [No. 82200068].
Author information
Authors and Affiliations
Contributions
Under the guidance of Professor Qiming Liu and Yichao Xiao. Zixi Zhang, Jiabao Zhou, Qiuzhen Lin and Cancan Wang collected relevant information. Zixi Zhang wrote the manuscript, which was revised by Qiuzhen Lin, Yunying Huang, Yongguo Dai, Wanyun Zuo and Na Liu. All the authors contributed to the article and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
There are no conflicts of interest or competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Z., Zhou, J., Lin, Q. et al. Overcoming barriers for left atrial appendage thrombus: a systematic review of left atrial appendage closure. BMC Cardiovasc Disord 24, 175 (2024). https://doi.org/10.1186/s12872-024-03843-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03843-w