Abstract
Background
There is a lack of evidence regarding contemporary implantable cardioverter-defibrillator (ICD) battery longevity. Our aim was to assess battery longevity in ICDs in a real-world setting.
Methods
Retrospective cross-sectional single center study of a prospectively collected database of consecutive patients who underwent ICD implantation from January 2010 to December 2015. Clinical data and battery longevity of all manufacturers were collected.
Results
A total of 351 patients (84.6% males, mean age of 61 ± 12 years) were included in the study (292 VVI; 6 VDD; 53 DDD). All manufacturers (Abbott, Biotronik, Boston, Medtronic and Microport) were equally represented in the study (p = 0.110). Median battery longevity was 10.8 years (11 years for VVI and 8.5 for DDD). After a follow-up time of 5 years, 98% of VVI and DDD were still in service (vs. industry-projected longevity of 98%). During this time, 89 patients (25.4%) underwent device replacement − 69 patients (77.5%) due to battery depletion, 6 patients due to infection, 3 patients due to dysfunction and 13 patients due to upgrade to CRT-D. Patients with Medtronic or Biotronik ICDs had a greater probability of being replaced earlier due to battery depletion (Biotronik HR 6.87, 95% CI 2.54–18.58, p < 0.001; Medtronic HR 6.08, 95% CI 2.45–15.06 p < 0.001).
Conclusions
VVI and DDD ICD battery longevity matched industry-projected longevity after 5 years of follow-up. Medtronic and Biotronik ICDs appeared to have an earlier battery depletion. Further randomized studies are required to ensure optimal care.
Similar content being viewed by others
Introduction
The implantable cardioverter-defibrillator (ICD) has become an indispensable tool in the primary and secondary prevention of sudden cardiac death (SCD). The number of indications for an ICD has vastly increased and its impact on cardiac morbidity and mortality is now universally recognized [1, 2].
Despite all its proven benefits, this technological advance entails very high costs [3]. The implantation of an ICD is often considered a lifelong therapy and since patient survival often exceeds device lifetime, device replacement is frequent. Therefore, two major aspects arise regarding the longevity of these products: the impact on patients’ lives and the effective cost to public health systems [4]. Some studies have analyzed which factors can influence the lifespan of devices in clinical practice, including the manufacturer and type of device. Nevertheless, their results are inconsistent [1, 4,5,6,7,8,9,10,11]. Moreover, most manufacturers project the longevity of their ICDs at 5–9 years [12,13,14,15,16]. However, “real-world” battery longevity data is scarce. Few studies have included devices released after 2010 and the follow-up period of this subset of patients was short [1].
Our goal was to assess contemporary battery longevity of ICDs in a “real-world” setting.
Materials & Methods
Study design and Setting
Retrospective, single center study of a prospectively constructed database of consecutive patients referred for ICD implantation from 2010 to 2015 in a tertiary referral center. Procedural endpoints and long-term follow-up were assessed.
This study was approved by the local Ethics Committee (Approval number 121/CES; OBS.SF.023-2022). The ethical principles from the Declaration of Helsinki were followed and respected. Due to the retrospective nature of the study, informed consent was waived.
Patient eligibility criteria
Patients were eligible for inclusion in the study if they had an indication for ICD implantation, irrespective of the pacing mode, according to current guidelines [2].
To achieve greater homogeneity, patients with previous devices or an indication for cardiac resynchronization therapy were excluded. Patients aged < 18 years or with subcutaneous ICD were also excluded from the analysis.
Data collection
Baseline data, clinical and laboratory variables and ICD characteristics (such as type of ICD, manufacturer and device model) were collected from a prospective database. The choice of manufacturer and model was up to the attending cardiologist as all manufacturers were available from the beginning of the studied period.
Follow-up data were retrieved from the internal database, outpatient clinical and emergency department admissions records as well as device monitoring consultation. All ICD replacements were identified and their replacement date and reason (elective replacement indicator [ERI], device dysfunction, early extraction and upgrade to another type of device) were assessed. The average percentage of pacing (calculated as the average of atrial and ventricular pacing divided by 2 for DDDs and the simple average of ventricular pacing for VVIs) was ascertained. The total number of shocks delivered (appropriate and inappropriate) and antitachycardia pacing (ATP) therapies were also surveyed. Sensing and pacing thresholds as well as impedance of leads from depleted generators were recorded. Device or pocket infection, heart transplant and mortality during follow-up were also evaluated. All remaining devices were censored at the date of the last database access. The date of last access of clinical follow-up was March 05, 2022.
Study endpoints
The primary endpoint was ICD battery longevity, defined as time from implantation to replacement due to ERI.
The secondary endpoint was longevity according to manufacturer.
Industry-projected longevity
Data was collected from product performance reports (PPRs) for all generators included [12,13,14,15,16]. Survival probability was retrieved at yearly increments from the reports for all generators in our sample and the average of these probabilities was calculated. This result was used as the overall industry-projected longevity and compared to the survival probability of our sample.
Statistical analysis
Analysis was performed with the use of IBM® SPSS® 26 and MedCalc® statistical software 19.6.3. Categorical variables are presented as frequencies and percentages. Continuous variables are expressed as means ± standard deviation or medians and interquartile ranges (IQR) for variables with or without normal distribution, respectively. Normal distribution was verified through the Kolmogorov-Smirnov test or by Skewness and Kurtosis measurements (maximum tolerated interval of -1 to 1). Bivariate analysis was performed using the χ2 test for categorical variables and t-test/ANOVA or Kruskal-Wallis test for continuous variables as appropriate.
Device longevity was defined as time in years from implantation to replacement due to ERI. Kaplan-Meier survival analysis was used to calculate median longevity by ICD type and manufacturer. Furthermore, comparison with industry-projected longevity was performed. Hazard ratios (HR), confidence intervals (95% CI), and p-values were calculated using the Cox proportional-hazards model, with adjustment for relevant variables (manufacturer, type of ICD, number of shocks, ATPs and pacing percentage) [1, 4, 5, 17, 18]. ICD replacements due to ERI battery status were considered events. Patients who were transplanted, died, underwent device upgrade or removal due to infection were censored at that respective date. ICDs still in service were censored at the date of last database access. Longevity was determined using Kaplan-Meier curves. Statistical significance was accepted for p values < 0.05.
Patient and public involvement
Patients were not involved in the design or conduction of this study.
Results
Patient and ICD characteristics
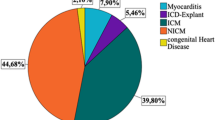
The final study sample included 351 patients (84.6% men, mean age of 60.6 ± 11.9 years) (Fig. 1). It was found that 109 patients (31.1%) died and 13 patients (4.0%) underwent heart transplantation before ICD battery end of life. ICDs were implanted in the majority of the patients for primary prevention (79.8%). Single chamber devices were the most commonly implanted type (83.2%). Baseline characteristics are depicted in Table 1.
All manufacturers are equally represented in the study (p = 0.110) and no differences were found regarding pacing modes (p = 0.176) (Table 2). Additionally, all manufacturers were available from the first year of enrolment, with no significant differences between years (p = 0.572). The remaining characteristics of patients by manufacturer and ICD type are presented in Supplemental Tables 1 and 2 respectively. Defibrillator threshold testing was not performed on any patient.
Primary endpoint
Overall median follow-up time was 7.5 years (IQR 4.38). During this period, 89 patients (25.4%) underwent device replacement. Of these, 67 were due to battery depletion. (Fig. 1).
Patients with battery depletion were less likely to have heart failure (p = 0.042), more likely to have a diagnosis of hypertrophic cardiomyopathy (p = 0.004), had higher glomerular filtration rates (p = 0.043), higher implantation of Medtronic (p < 0.001) and Biotronik (p 0.039) ICDs as well as more dual chamber pacing mode (p = 0.026) compared to patients without battery depletion.
Overall median longevity was 10.8 years. Median longevity by manufacturer and type of ICD determined by survival curves is shown in Table 3.
Regarding industry-projected longevity, our cohort showed a similar longevity to that reported in the product performance reports (PPRs) (Fig. 2). After a follow-up time of 5 years, 98% of VVI and DDD were still in service (vs. industry-projected longevity of 98%). These results persisted after 7 years of follow-up with 94% of VVI still in service (vs. industry-projected longevity of 93%) (Fig. 2A). Regarding DDD, our cohort showed a 81% survival of the devices in contrast to an industry-projected longevity of 89%. (Fig. 2B) Nevertheless, all estimates provided by the industry fell inside the 95% confidence interval.
Median atrial impedance was 551 Ohm (IQR 404) whereas ventricular impedance was 494 Ohm (IQR 446). Median atrial sensing and pacing thresholds for leads from depleted generators are shown in Fig. 3A and B.
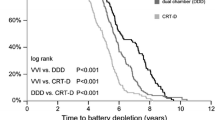
Secondary endpoint
Battery longevity between manufacturers was statistically different (p < 0.001; Fig. 4). Compared to the other manufacturers, patients with Medtronic or Biotronik ICDs had a higher risk of being replaced earlier due to battery depletion even after adjustment for ATP therapies, shocks and other confounders (Table 4). ATP and shocks had a non-significant impact on longevity (p = 0.980 and p = 0.307 respectively) whereas pacing percentage was the only other significant influence besides manufacturer (p 0.047; HR 1.27; 95% CI 1.01–1.61).
Discussion
To the best of our knowledge this is the first study that evaluates long-term follow-up of devices implanted solely in the last decade using real-world data and where all manufacturers were included. Our findings suggest that (1) single chamber and dual chamber ICD battery longevity is similar to the estimation provided by manufacturers and (2) Biotronik and Medtronic ICDs may present a higher risk of being replaced due to earlier battery depletion.
There are few articles published comparing the battery longevity of ICD devices from different manufacturers. Many of the models analyzed in previous studies have already been discontinued [7]. This makes scientific information about the current longevity of devices from different manufacturers even more scarce [8]. Previous studies reported an average battery longevity for VVIs of 5–7 years and DDDs of 5–6 years [1, 6, 7, 19]. At the present time, manufacturers estimate a longevity of 8 to 10 years in single-chamber ICDs and 6 to 9 years in double-chamber ICDs according to the product performance reports (PPRs) [12,13,14,15,16]. Industry-projected longevity at 5 and 7 years was similar to the longevity of the studied cohort. Overall battery longevity was 10.8 years. When analyzing by subtype, VVI longevity was slightly higher than previously reported, with a median battery longevity of 11.0 years. DDD median longevity was 8.5 years. This sharp contrast with previous studies is probably the result of improved battery and lead technologies [10].
In our population, patients with ICDs from Medtronic and Biotronik had a lower longevity, in line with previous studies [4, 6, 18]. These differences may be the result of lower battery capacities present in Medtronic and Biotronik devices [10]. A recent single study using PPRs concluded that Boston DDD-ICDs had longer battery longevity, whereas in VVI devices, Abbot and Medtronic’s were superior [9]. Nevertheless, longevity in PPRs may not represent real-world experiences as it is often overestimated due to underreporting as well as not all manufacturers available in Europe having been studied [6, 9, 11, 17]. Furthermore, there is great heterogeneity in the assumptions made by the manufacturers in order to estimate device longevity [10]. It is also worth noting that other studies have shown superior battery longevity of Medtronic devices [1, 7, 20]. This discrepancy between manufacturers does not seem to be justified by battery chemistry alone since Boston and Biotronik used preferably LiMnO2 batteries in contrast to the remaining manufacturers that use Li/SVO-CFx batteries. Our study takes into consideration the pacing percentage and ICD therapies, providing new information regarding devices implanted in the last decade that were previously unavailable. We hypothesize that these differences among studies may result from an asymmetric number of implantations among different manufacturers, differences in current battery and device technologies and lack of adjustment for device therapies.
It is clear that a shorter battery life contributes to morbidity and mortality [10]. Reinterventions have been linked to device-related infections and other complications [21]. As such, it is of the utmost importance that battery longevity be improved to minimize reinterventions. Ultimately, a lower rate of reinterventions may even culminate in a better quality of life and improved mental health. This is an essential issue in this population since anxiety and depression are particularly prevalent [2]. In fact, a National Institute of Health and Care Excellence (NICE) guidance document reports that battery longevity improvement is the main factor for more significant clinical benefit [10, 22]. An additional impact of reduced longevity is financial burden. As health-services around the world are increasingly under strain, greater longevity and consequently fewer reinterventions and complications are crucial in order to ensure their sustainability. It is paramount to have information about the newer devices because only then will it be possible to make an ICD choice with the best cost-benefit ratio [10]. Our study provides an update on the literature data and new information regarding newer devices released after 2010.
Limitations
We acknowledge some limitations in the present study. First, this was a single-center retrospective study. However, this was mitigated since data was collected from our prospective database. Second, ICD indications differed significantly between manufacturers which may have led to asymmetries in therapies and pacing percentage. Thirdly, the number of patients included for each manufacturer in this study was insufficient to allow more robust conclusions. Nonetheless, the study size was comparable to other similar studies. Randomized, large-scale studies are required to confirm the results obtained in our study and to assess their clinical implications even though they are unlikely to be made. Fourthly, the sample is comprised mainly of men. This underrepresentation of women is probably justified by the high prevalence of ischemic heart disease in men. Two meta-analyses showed that women received less appropriate ICD therapies [23, 24]. Ultimately this fact could mean greater battery longevity even though it remains to be studied. Finally, we recognize that different ICD models of the same brand were analyzed, which have different intrinsic characteristics that may affect the longevity of the device [12,13,14,15,16]. Nevertheless, battery and lead technology as well as programming are similar throughout all devices of a given manufacturer and as such we believe the validity of these findings still holds.
Conclusion
In conclusion, the battery longevity of single and dual chamber ICDs in the real-world appears to be in agreement with estimations provided by manufacturers. Further studies are required, given that these results have important clinical implications for both patients and hospitals.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- ATP:
-
antitachycardia pacing
- CI:
-
confidence interval
- ERI:
-
elective replacement indicator
- HR:
-
hazard ratio
- ICD:
-
Implantable cardioverter-defibrillator
- IQR:
-
interquartile ratio
- NICE:
-
National Institute of Health and Care Excellence
- PPR:
-
product performance reports
- SCD:
-
sudden cardiac death
References
Thijssen J, Borleffs CJW, Van Rees JB et al. Implantable cardioverter-defibrillator longevity under clinical circumstances: an analysis according to device type, generation, and manufacturer. Heart Rhythm 2012; 9.
Priori SG, Blomström-Lundqvist C, Mazzanti A et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of Sudden Cardiac Death: the Task Force for the management of patients with ventricular arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Europace 2015; 17.
Manolis AS, Rastegar H, Estes NAM. Automatic Implantable Cardioverter Defibrillator: current status. JAMA: The Journal of the American Medical Association 1989; 262.
Seegers J, Expósito PM, Lüthje L et al. Longevity of implantable cardioverter-defibrillators in a single-center population. J Interventional Cardiac Electrophysiol 2015; 44.
Siontis KC, Pantos I, Katritsis DG. Comparison of the longevity of implantable cardioverter-defibrillator devices by different manufacturers. Int J Cardiol 2014; 175.
Von Gunten S, Schaer BA, Yap SC et al. Longevity of implantable cardioverter defibrillators: a comparison among manufacturers and over time. Europace 2016; 18.
Manolis AS, Maounis T, Koulouris S, Vassilikos V. Real life longevity of implantable cardioverter-defibrillator devices. Clin Cardiol. 2017;40:759–64.
Alam MB, Munir MB, Rattan R et al. Battery longevity in cardiac resynchronization therapy implantable cardioverter defibrillators. Europace 2014; 16.
Hauser RG, Casey SA, Gitter CB et al. Reliability and longevity of implantable defibrillators. J Interventional Cardiac Electrophysiol 2021; 62.
Boriani G, Merino J, Wright DJ, Gadler F, Schaer B, Landolina M. Battery longevity of implantable cardioverter-defibrillators and cardiac resynchronization therapy defibrillators: Technical, clinical and economic aspects. An expert review paper from EHRA. Europace. 2018.
Shafat T, Baumfeld Y, Novack V, Konstantino Y, Amit G. Significant differences in the expected versus observed longevity of implantable cardioverter defibrillators (ICDs). Clin Res Cardiol 2013; 102.
Blunt R. Product performance report. Abbott 2022 (1st edition). Available at www.cardiovascular.abbott.com. Accessed 15 Jul 2022.
Borkowski R. Product performance report. Biotronik 2021 (December). Available at www.biotronik.com. Accessed 11 May 2022.
Hauge K. Cardiac rhythm and heart failure product performance report. Medtronic 2021 (2nd edition), Available at www.medtronic.com. Accessed 11 May 2022.
Vincon A. Product performance report: Cardiac rhythm management. Microport 2021 (November), Available at www.microport.com. Accessed 11 May 2022.
Naughton A. Rhythm management product performance report. Boston Scientific 2022 (Q1). Available at www.bostonscientific.com. Accessed 11 May 2022.
Boriani G, Ritter P, Biffi M et al. Battery drain in daily practice and medium-term projections on longevity of cardioverterdefibrillators: an analysis from a remote monitoring database. Europace 2016; 18.
Schaer BA, Koller MT, Sticherling C, Altmann D, Joerg L, Osswald S. Longevity of implantable cardioverter-defibrillators, influencing factors, and comparison to industry-projected longevity. Heart Rhythm 2009; 6.
HORLBECK FW, MELLERT F, KREUZ J, NICKENIG G. SCHWAB JO: Real-World Data on the Lifespan of Implantable Cardioverter-Defibrillators Depending on Manufacturers and the Amount of Ventricular Pacing. J Cardiovasc Electrophysiol [Internet] 2012; 23:1336–1342. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/j.1540-8167.2012.02408.x.
Biffi M, Ziacchi M, Bertini M et al. Longevity of implantable cardioverter-defibrillators: implications for clinical practice and health care systems. Europace 2008; 10.
Johansen JB, Jørgensen OD, Møller M, Arnsbo P, Mortensen PT, Nielsen JC. Infection after pacemaker implantation: Infection rates and risk factors associated with Infection in a population-based cohort study of 46299 consecutive patients. Eur Heart J 2011; 32.
Evans JM, Cleves A, Morgan H, Millar L, Carolan-Rees G. ENDURALIFE-Powered Cardiac Resynchronisation Therapy Defibrillator devices for Treating Heart Failure: a NICE Medical Technology Guidance. Appl Health Econ Health Policy; 2018.
Conen D, Arendacka B, Röver C et al. Gender differences in appropriate shocks and mortality among patients with primary prophylactic implantable Cardioverter-Defibrillators: systematic review and Meta-analysis. PLoS ONE 2016; 11.
Santangeli P, Pelargonio G, Russo A, Dello et al. Gender differences in clinical outcome and primary prevention defibrillator benefit in patients with severe left ventricular dysfunction: a systematic review and meta-analysis. Heart Rhythm 2010; 7.
Acknowledgements
Not applicable.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the concept and design of the article. DAF and LMP also collected the data and all authors performed its analysis and interpretation. DAF drafted the original article. All authors reviewed it. All authors approve this version of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local Ethics Comittee (Centro Hospitalar e Universitário de Coimbra Ethics Committee; Approval number 121/CES; OBS.SF.023-2022). The ethical principles from the Declaration of Helsinki were followed and respected. Due to the nature of the study, need for informed consent was waived by the local Ethics Comittee (Centro Hospitalar e Universitário de Coimbra Ethics Committee; Approval number 121/CES; OBS.SF.023-2022).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental table 1:
Baseline characteristics by manufacturer
Supplemental table 2:
Baseline characteristics by ICD type
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Almeida Fernandes, D., António, N., Sousa, P.A. et al. “Real-world” analysis of battery longevity of implantable cardioverter-defibrillators: an in-depth analysis of a prospective defibrillator database. BMC Cardiovasc Disord 23, 609 (2023). https://doi.org/10.1186/s12872-023-03653-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03653-6