Abstract
Background
Extracorporeal circulation auxiliary to open heart surgery is a common procedure used to treat heart diseases. However, the optimal transfusion strategy for patients undergoing this surgery remains a subject of debate. This study aims to investigate the association between hemoglobin levels and clinical outcomes in patients undergoing extracorporeal circulation auxiliary to open heart surgery, with the ultimate goal of improving surgical success rates and enhancing patients' quality of life.
Methods
A retrospective analysis was conducted on data from the Medical Information Mart for Intensive Care IV 2.2 (MIMIC-IV 2.2) database, including 4144 patients. The patients were categorized into five groups based on their minimum hemoglobin levels during hospitalization. Baseline characteristics, clinical scores, laboratory results, and clinical outcome data were collected. Statistical analyses utilized descriptive statistics, ANOVA or Kruskal-Wallis tests, Kaplan-Meier method, and Log-rank test.
Results
The results revealed a significant correlation between hemoglobin levels and in-hospital mortality, as well as mortality rates at 30 days, 60 days, and 180 days (p < 0.001). Patients with lower hemoglobin levels exhibited higher mortality rates. However, once hemoglobin levels exceeded 7g/dL, no significant difference in mortality rates was observed (p = 0.557). Additionally, lower hemoglobin levels were associated with prolonged hospital stay, ICU admission time, and mechanical ventilation time (p < 0.001). Furthermore, hemoglobin levels were significantly correlated with complication risk, norepinephrine dosage, and red blood cell transfusion volume (p < 0.001). However, there was no significant difference among the groups in terms of major complications, specifically sepsis (p > 0.05).
Conclusion
The study highlights the importance of managing hemoglobin levels in patients undergoing heart surgery with extracorporeal circulation. Hemoglobin levels can serve as valuable indicators for predicting clinical outcomes and guiding treatment decisions. Physicians should carefully consider hemoglobin levels to optimize transfusion strategies and improve postoperative patient outcomes. Further research and intervention studies are warranted to validate and implement these findings in clinical practice.
Similar content being viewed by others
Introduction
The transfusion therapy strategy for critically ill patients has long been a central issue in clinical decision-making [1,2,3]. Hemoglobin, as the primary carrier of oxygen, plays a crucial role in maintaining tissue oxygen supply [4]. Consequently, low hemoglobin levels may affect oxygen delivery, leading to organ dysfunction or even organ failure [5,6,7]. Most current clinical guidelines recommend considering transfusion when hemoglobin levels in critically ill patients drop to 7 g/dL or below [8]. This recommendation is based on numerous studies involving patients in various clinical scenarios [9]. For example, certain studies focusing on different clinical contexts have found that hemoglobin levels below specific thresholds may be associated with adverse outcomes [10]. However, on the other hand, excessive transfusion may also lead to other complications, such as transfusion-related acute lung injury, infections, and other transfusion-related reactions [11]. Nevertheless, whether this recommendation still applies to patients undergoing extracorporeal circulation auxiliary to open heart surgery remains a question that needs to be explored. The heart plays a critical role in the oxygen delivery system of the human body [12]. For patients undergoing extracorporeal circulation auxiliary to open heart surgery(EC-AOHS ), the invasiveness of the procedure and associated systemic stress responses may affect their oxygen delivery and utilization. Additionally, EC-AOHS patients often have various underlying diseases, which may further increase their risk of developing anemia. The goal of red blood cell transfusion is to improve or maintain oxygen delivery in patients with hemorrhage or anemia [13]. The decision for transfusion becomes complex due to multiple factors; severe anemia and excessive blood loss are common, and cardiovascular disease patients may have different transfusion requirements compared to other patient populations. The decision for transfusion in cardiac surgery is often based on the severity of perioperative anemia. Guidelines (Grade C recommendation) suggest a highly restrictive transfusion threshold with a hemoglobin concentration of 60–70 g/L [8]. These thresholds are mainly derived from randomized controlled trials in non-cardiac surgery patients, which have demonstrated the equivalence of restrictive transfusion thresholds [14]. They have also drawn evidence from observational studies, which show that reversing severe anemia with red blood cell transfusions is associated with adverse clinical outcomes such as death, acute lung injury, acute kidney injury, stroke, myocardial infarction, sepsis, and surgical site infection [15]. Red blood cell transfusion carries significant morbidity. Hemolytic transfusion reactions and transfusion-related lung injury cause many deaths each year, but the causal relationship between red blood cell transfusions and observed adverse outcomes remains undetermined [16]. Severe anemia is the primary indication for transfusion and an important predictor of adverse outcomes in patients undergoing cardiac surgery, who may already be at the limits of their physiological reserve. Therefore, for EC-AOHS patients, a separate evaluation of the relationship between hemoglobin levels and clinical outcomes is needed to determine the optimal transfusion strategy.
We used the MIMIC-IV database to investigate the relationship between hemoglobin levels and clinical outcomes in EC-AOHS patients. The MIMIC-IV database is a large, publicly available critical care database that contains extensive clinical data from various healthcare institutions. Analyzing this data allows us to study a large number of patients efficiently and draw reliable conclusions. Such research is valuable for optimizing treatment strategies and improving postoperative outcomes for EC-AOHS patients.
Method
Data source
We conducted a large sample retrospective analysis using the MIMIC-IV database (version 2.2) [17]. This database is developed by the computational physiology laboratory of the Massachusetts Institute of Technology (MIT, Cambridge, MA, USA) with approval from the Institutional Review Boards (IRB) of MIT and Beth Israel Deaconess Medical Center (BIDMC), contains demographic data, vital signs, laboratory results, and prescriptions collected between 2008 and 2019 in the ICU or emergency department of BIDMC. Patient identifications were removed to comply with the Health Insurance Portability and Accountability Act’s (HIPAA) Safe Harbor provision [18, 19]. One author, Zhao kun Fan, completed the online course on Data or Specimens Only Research and gained access to the database for data extraction after passing the Collaborative Institutional Training Initiative (CITI) exam (Record ID: 55,303,422).
Study population and data collection
The study cohort consisted of 4,144 patients with extracorporeal circulation auxiliary to open heart surgery from the MIMIC-IV, who were identified based on the Ninth (ICD-9) and Tenth (ICD-10) Revision of Interna tional Classification of Diseases. We included patients who underwent extracorporeal circulation auxiliary to open heart surgery. Based on the minimum hemoglobin value during the hospitalization, patients were divided into five groups: Group 1 (≤ 7.0 g/dL), Group 2 (7.1-8.0 g/dL), Group 3 (8.1-9.0 g/dL), Group 4 (9.1–10.0 g/dL), and Group 5 (> 10.0 g/dL).
Patients with one of the following conditions were excluded: (1) lacked hemoglobin data; (2) less than 18 years old; (3) patients with repeated ICU admissions (If a patient was admitted to the ICU more than once, we used the date of the first admission); (4) less than 24 h of ICU stay; The detailed inclusion of our enrolled patients is shown in Fig. 1.
Data collection included the following: demographic data, comorbidities, vital signs, laboratory parameters, medication use, length of hospital stay, length of ICU stay (ICU LOS), and time of death. These data were collected using a PostgreSQL database.
-
(1)
Demographic data includes age, gender.
-
(2)
Complications include diabetes, hypertension, coronary heart disease (CAD), congestive heart failure (CHF), chronic kidney disease (CKD) and chronic obstructive pulmonary disease (COPD), tumors.
-
(3)
Vital signs include respiratory rate (RR), heart rate (HR), mean blood pressure (MBP) and transcutaneous oxygen saturation (SpO2).
-
(4)
Laboratory indicators include white blood cell count (WBC), red blood cell count (RBC), minimum value of hemoglobin (hemoglobin min) during admission, platelet count (PLT), international normalized ratio (INR), activated partial thromboplastin time ( PTT).
-
(5)
The scoring systems included the Sequential Organ Failure Assessment score (SOFA), the Oxford Acute Severity of Illness Score (OASIS), and the Acute Physiology Score III (APS III).
-
(6)
Treatment information included the dose of norepinephrine used, the amount of red blood cells transfused, and the duration of mechanical ventilation.
-
(7)
Additionally, the study recorded the length of hospital stay, ICU length of stay , and in-hospital, 30-day, 60-day, and 180-day all-cause mortality.
Statistical analysis
Descriptive statistics were used to summarize the baseline characteristics and clinical outcomes of the patients. The distribution differences of continuous variables among the groups were compared using ANOVA or Kruskal-Wallis test, while categorical variables were compared using Chi-squared or Fisher’s exact test. Survival analysis was performed using the Kaplan-Meier method, and differences among the groups were compared using the Log-rank test.
Outcomes
Definitions
The baseline hemoglobin is defined as the first recorded data upon admission, while the minimum hemoglobin represents the lowest value detected during the hospital stay. The hemoglobin change is calculated as the difference between the baseline value and the minimum value. Patients were divided into five groups: Group 1 (≤ 7.0 g/dL), Group 2 (7.1-8.0 g/dL), Group 3 (8.1-9.0 g/dL), Group 4 (9.1–10.0 g/dL), and Group 5 (> 10.0 g/dL).
Statistical analysis
Continuous variables were represented as mean ± standard deviation (SD) for data adhering to normal distribution and as median (25th, 75th percentiles) for non-normally distributed data. The analytical tools employed were one-way ANOVA and Kruskal-Wallis H-test, respectively. Categorical data were denoted as frequency (percentage) and assessed via Chi-square or, when applicable, Fisher’s exact tests. We presumed missing data to occur at random and thus employed multiple imputations for completion.
Survival distributions, contingent on different hemoglobin levels, were juxtaposed using the Kaplan-Meier method, accompanied by the log-rank test. The results were elucidated as cumulative incidence.
For a more intuitive understanding, we incorporated several visualization methodologies
Violin Plots were deployed for a granular understanding of hospital durations, encompassing metrics like the overall stay, ICU stay, and mechanical ventilation duration.
Box Plots were pivotal in extrapolating treatment specifics, with a keen focus on red blood cell transfusion quantities and the norepinephrine administration frequency.
Heatmaps vividly encapsulated the sepsis incidence data.
To further probe the interdependencies among variables, we leveraged Correlation Tools. The synergy of heatmaps and matrix plots was especially informative, casting light on correlations involving age, gender, in-hospital mortality, and diverse scores.
All statistical inferences were drawn using STATA (version 17.0), with the significance threshold earmarked at p < 0.05.
Results
Patient characteristics
This study enrolled a total of 4,144 patients who were stratified into five groups based on their minimum hemoglobin levels during hospitalization. The distribution of patients in each group was as follows: 381 patients in the group with hemoglobin ≤7.0 g/dL, 1,145 patients in the group with 7.1-8.0 g/dL, 1,312 patients in the group with 8.1-9.0 g/dL, 801 patients in the group with 9.1-10.0 g/dL, and 505 patients in the group with hemoglobin >10.0 g/dL. The baseline characteristics of these patients are presented in Table 1. Age: The average age across all groups is 67.86 years. The group with Hb>10.0g/dl has the lowest average age, at 62.40 years, while the Hb 7.1-8.0g/dl group has the highest average age, at 69.60 years. Based on the P-value, there's a statistically significant difference in age distribution between different Hb level groups. Gender: Overall, 68.07% of the sample are male.In the Hb>10.0g/dl group, the proportion of males is the highest, reaching 97%.
Basic illness: Myocardial Infarction: 1064 cases, with the Hb8.1-9.0g/dl group having the most at 341 cases.Congestive Heart Failure: 1154 cases, with the Hb7.1-8.0g/dl group having the most at 395 cases.Cerebrovascular Disease: 444 cases, with the Hb7.1-8.0g/dl group having the most at 168 cases.Renal Disease: 612 cases, with the Hb7.1-8.0g/dl group having the most at 252 cases.Chronic Pulmonary Disease: 1033 cases, with both the Hb7.1-8.0g/dl and Hb8.1-9.0g/dl groups having 345 cases each.Malignant Cancer: 126 cases, with the Hb8.1-9.0g/dl group having the most at 43 cases.
Other Indicators: OASIS Score: The average for all groups is 31.63. The Hb>10.0g/dl group has the lowest average score of 28.77.SOFA Score: The average for all groups is 5.43. The Hb>10.0g/dl group has the lowest average score of 4.96.APSIII Score: The average for all groups is 40.30. The Hb>10.0g/dl group has the lowest average score of 35.33.Respiratory Rate (R rate): The average for all groups is 17.47 bpm. The Hb≤7g/dl group has the highest average rate of 17.90 bpm. Heart Rate: The average for all groups is 82.88 bpm. The Hb≤7g/dl group has the highest average rate of 83.37 bpm.Mean Arterial Pressure (MAP): The average for all groups is 74.21 mmHg. The Hb>10.0g/dl group has the highest average at 75.97 mmHg.Oxygen Saturation (SpO2): The average for all groups is 97.88%. The Hb>10.0g/dl group has the lowest average at 97.41%.
Laboratory Test Indicators: Hemoglobin (Min) (g/dl): The overall average is 8.54 (1.25). The Hb>10.0g/dl group has the highest average value of 10.78 (0.58), while the lowest is 6.47 (0.66) for the Hb≤7g/dl group.Hemoglobin Change (g/dl): The overall average change is 2.62 (2.18). The Hb≤7g/dl group had the highest change with 3.30 (2.61).RBC (Min) (×10^12/L): The overall average is 2.82 (0.42). The Hb>10.0g/dl group recorded the highest average value of 3.92 (0.34). Platelet Mean (×10^9/L): The average across all groups is 183.88 (64.67). The Hb7.1-8.0g/dl group had the highest average value of 191.63 (75.15). WBC Mean (×10^9/L): The average white blood cell count across all groups is 11.25 (3.71). The Hb>10.0g/dl group recorded the highest average value of 11.88 (2.72). INR Mean (s): The overall average is 1.39 (0.34). The Hb≤7g/dl group had the highest average value of 1.48 (0.36). PTT Mean (s): The average across all groups is 38.12 (11.36). The Hb≤7g/dl group had the highest average value of 41.37 (11.53).
Top ten primary diagnoses
Additionally, Fig. 2 illustrates the top ten primary diagnoses observed among the study participants. From it, we can observe the frequency or count of different diagnoses. Notably, “coronary atherosclerosis of native coronary artery” has the highest number of patients, ranking it first. This indicates that within the given sample or dataset, this diagnosis is the most prevalent.
Comparison of outcome measures
In this study, patients with different hemoglobin levels were grouped, and multiple outcome measures were compared among the groups. The outcomes are presented in Table 2.
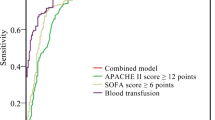
Additionally, we conducted survival analysis to explore the relationship between hemoglobin levels and survival time (Fig. 3). From the Kaplan-Meier survival curves, we observed that as hemoglobin levels increased, the survival probability seemed to improve. Particularly in the group with lower hemoglobin levels, the survival rate was significantly lower than in the other groups. However, the Log-rank test revealed no significant differences in survival time within 180 days between the four groups: 7.1-8.0, 8.1-9.0, 9.1–10, and > 10 (p-value = 0.557).
Visual comparison of secondary outcome measures
To visually display the differences in secondary outcome measures among different hemoglobin level groups, we used violin plots for visualization (Fig. 4).
Length of hospital stay
From the figure, it can be observed that the group with hemoglobin levels less than or equal to 7 g/dL had a wider distribution of hospital stay duration. In contrast, as hemoglobin levels increased, the median and distribution range of hospital stay duration decreased, especially in the group with hemoglobin levels greater than 10 g/dL.
Length of ICU stay
For ICU stay duration, the group with hemoglobin levels less than or equal to 7 g/dL had a relatively higher median. Similar to the trend in total hospital stay duration, as hemoglobin levels increased, the median and distribution range of ICU stay duration also decreased.
Mechanical ventilation time (duration hours)
Regarding mechanical ventilation time, the group with hemoglobin levels less than or equal to 7 g/dL had the widest distribution and a relatively higher median. However, when hemoglobin levels increased to above 10 g/dL, the median and distribution range of mechanical ventilation time significantly decreased.
Overall, lower hemoglobin levels (less than or equal to 7 g/dL) were associated with longer hospital stay, longer ICU stay, and longer mechanical ventilation time.
Differences between groups in other indicators
To further evaluate the differences between different hemoglobin level groups, we analyzed the amount of red blood cell transfusion, the use of norepinephrine, and the incidence of sepsis.
Amount of red blood cell transfusion
The box plots (Fig. 5) show that the group with hemoglobin levels less than or equal to 7 g/dL had a wide variation in the amount of red blood cell transfusion. As hemoglobin levels increased, the median and distribution range of red blood cell transfusion decreased.
Use of norepinephrine
For the use of norepinephrine (Fig. 6), the group with hemoglobin levels less than or equal to 7 g/dL had a relatively higher median, but with greater variation. As hemoglobin levels increased, the median and distribution range of norepinephrine use decreased.
Incidence of sepsis
The heatmap (Fig. 7) illustrates that different hemoglobin groups had some differences in the incidence of sepsis, although these differences did not reach statistical significance.
Relationship analysis of relevant variables
To further understand the relationship between hemoglobin levels and other relevant variables such as age, gender, in-hospital mortality, and various scores, we created a correlation heatmap (Fig. 8) and a matrix plot (Fig. 9). These figures show the degree of association between variables. The color intensity represents the strength of the correlation, and the size of the circles reflects the magnitude of the correlation.
Age and other variables
Age showed a mild negative correlation with gender and hemoglobin group, indicating that older patients might be more likely to have lower hemoglobin levels.
Age and SOFA, OASIS, and APSIII scores were positively correlated, suggesting that older patients might have higher disease severity.
Gender and other variables
Gender showed a moderate positive correlation with the hemoglobin group, indicating a certain association between gender and hemoglobin levels.
Relationship between scoring systems
SOFA, OASIS, and APSIII scores were positively correlated, suggesting that these scoring systems might share some common elements or factors when assessing disease severity.
Relationship between scoring systems and hemoglobin groups: All scoring systems showed negative correlations with hemoglobin groups, indicating that lower hemoglobin levels were associated with higher disease severity.
In-hospital mortality and other variables
In-hospital mortality showed a mild positive correlation with SOFA, OASIS, and APSIII scores, suggesting that higher scores might be associated with an increased risk of in-hospital mortality.
Discussion
With the advancement of medical research, transfusion strategies for critically ill patients have become a critical part of clinical decision-making. Transfusion is a crucial method to adjust hemoglobin levels in patients, but it also comes with potential adverse reactions and complications. Excessive transfusion may lead to fluid overload, electrolyte imbalances, and immune response activation, increasing the length of hospital stay and medical costs. Therefore, determining the optimal transfusion strategy is essential to balance treatment efficacy and risk and improve patient outcomes [20].
In current clinical practice, it is generally recommended to consider transfusion when hemoglobin levels in critically ill patients drop to 7 g/dL or below. However, whether this threshold is applicable to patients undergoing extracorporeal circulation auxiliary to open heart surgery remains a topic of exploration. The process of open heart surgery with extracorporeal circulation itself may cause a significant decrease in hemoglobin levels, compounded by postoperative factors such as inflammation and blood loss, potentially leading to lower hemoglobin levels in these patients. As such, determining an appropriate hemoglobin transfusion threshold is particularly crucial for this patient population.
In this study, we conducted an in-depth analysis of a large sample from the MIMIC-IV database to explore the relationship between hemoglobin levels and clinical outcomes in patients after open heart surgery with extracorporeal circulation. Our findings supported the correlation between hemoglobin levels and patient mortality. Lower hemoglobin levels were associated with higher mortality rates. However, it is noteworthy that when hemoglobin levels exceeded 7 g/dL, there was no significant difference in mortality rates among the groups. This might resonate with the red blood cell transfusion thresholds mentioned in the clinical practice guidelines by Carson JL et al. [8]. This suggests that maintaining hemoglobin levels above 7 g/dL may be a more reasonable and safe transfusion strategy, avoiding the potential adverse effects of excessive transfusion.
Additionally, our research indicated that lower hemoglobin levels were correlated with extended hospital stays, ICU admission durations, and mechanical ventilation times. This observation is consistent with the study by Murphy GJ et al., which showed that a liberal transfusion strategy post-cardiac surgery might result in prolonged hospital stays and a heightened risk of complications compared to a restrictive approach [21]. Furthermore, we identified a significant correlation between hemoglobin levels and complication risks, norepinephrine dosage, and red blood cell transfusion volume. This aligns with the findings of Hajjar LA et al., who observed a similar relationship in patients post-cardiac surgery [22].
Upon evaluating the data, we discerned that a higher hemoglobin (Hb) level is inversely related to age. This observation underscores the tendency for younger patients to manifest elevated hemoglobin concentrations. Remarkably, within the cohort characterized by Hb levels exceeding 10.0 g/dl, the male demographic predominates, accounting for 97%. This pronounced male predominance may hint at an inherent physiological predisposition enabling males to sustain elevated Hb levels. Consequently, it intimates an augmented susceptibility among males compared to their female counterparts. A disparate distribution was evident in conditions like myocardial infarction, congestive heart failure, and cerebrovascular diseases when assessed across varied Hb strata. Such disparities insinuate potential associations between hemoglobin levels and the predisposition to specific foundational ailments. Moreover, universally lower scores in assessment tools like OASIS, SOFA, and APSIII in the higher Hb cohorts allude to a relatively benign clinical presentation in these individuals. Furthermore, vital parameters, namely respiratory rate, heart rate, mean arterial pressure, and oxygen saturation, showcased discernible variations across the Hb categories. Such variances are conceivably linked to the interplay between an individual’s cardiopulmonary function and their corresponding hemoglobin levels. In encapsulation, our investigative outcomes resonate with numerous extant scholarly articles, thereby amplifying the credibility and potential clinical ramifications of our findings.
Potential mechanisms
One of the pivotal mechanisms underlying the relationship between hemoglobin levels and clinical outcomes is the capacity for oxygen delivery and utilization. Hemoglobin, being the primary transporter of oxygen in the blood, plays a crucial role in ensuring tissues receive adequate oxygen supply. Lower levels of hemoglobin could compromise this delivery, leading to tissue hypoxia. Tissue hypoxia, especially in vital organs such as the heart, brain, and kidneys, can result in impaired organ function and increased morbidity and mortality.
Another aspect to consider is the cardiovascular stress response, especially during surgeries assisted by extracorporeal circulation. The heart and vascular system are subjected to significant stress during such procedures. A diminished hemoglobin level might exacerbate this stress, potentially leading to heightened risks of complications.
Furthermore, while red blood cell transfusions can bolster the hemoglobin levels, they are not without risks. Transfusions can introduce risks such as transfusion reactions, infections, and inflammatory responses. These adverse effects of transfusions might, in some cases, outweigh the benefits, especially when transfusions are administered without clear indications. Karkouti K et al. discussed the interrelationship of preoperative anemia, intraoperative anemia, and red blood cell transfusion as potentially modifiable risk factors for acute kidney injury in cardiac surgery [23].
Other potential confounders that might influence the relationship between hemoglobin levels and clinical outcomes include the baseline health status of the patient, the complexity and complications of the surgery, and other treatment modalities employed during the care process.
Clinical implications
The clinical implications of our findings stretch across various domains of cardiac patient management
Transfusion Decisions: Our study provides valuable insights that could guide clinicians in making more informed transfusion decisions. Specifically, when hemoglobin levels fall below 7 g/dL, consideration for transfusion might be warranted.
Preoperative Assessment and Treatment: For patients slated for cardiac surgeries, a preoperative assessment of hemoglobin levels could be integral. Identifying and potentially treating those with reduced hemoglobin levels might better prepare them for the surgery, ensuring they have the best chances for favorable outcomes.
Risk Prediction for Complications: Hemoglobin levels can be employed as a marker to predict the risk of complications, thereby guiding subsequent clinical decisions and patient management. This is especially crucial as patients with lower hemoglobin levels might be at heightened risk for prolonged hospital stays, increased ICU admission durations, and extended mechanical ventilation times.
Postoperative Care and Management: Post-surgery, patients exhibiting lower hemoglobin levels might necessitate more vigilant monitoring and care. Recognizing and addressing these levels promptly could potentially mitigate the risk of complications and improve patient outcomes.
Incorporating these findings into clinical practice could greatly enhance the quality of care provided to cardiac patients, ensuring they receive the most appropriate and effective interventions tailored to their individual needs.
Limitations and future directions
Limitations:Data from MIMIC-IV 2.2 may not represent the broader population, introducing potential biases. Retrospective design may lead to recall bias and missing data affecting the outcomes. Unaccounted confounding factors could influence the results. Lack of randomization prevents establishing causal relationships.
Future Directions: Conduct prospective randomized controlled trials to establish causal relationships. Explore similar studies in diverse populations to validate generalizability. Investigate biological and physiological mechanisms underlying the hemoglobin-outcome relationship. Design and test targeted intervention strategies to improve patient outcomes after open heart surgery.
Conclusion
The study findings demonstrate that when hemoglobin levels are below 7 g/dl, there is an increase in mortality. However, when hemoglobin levels are above 7 g/dl, there is no significant change in mortality, providing support for guidelines that set transfusion alerts at this threshold. Nevertheless, there is a need for further exploration of other clinical outcomes, including hospital stay duration, ICU stay duration, mechanical ventilation duration, transfusion volume, and norepinephrine usage, among others. In-depth research into these outcome measures will enable a comprehensive understanding of the impact of hemoglobin levels on patients. This understanding can lead to the development of more effective treatment strategies, ultimately enhancing patient outcomes and improving their quality of life. Therefore, future research should prioritize and explore these directions to gain more insights into this field.
Availability of data and materials
The original data of our study are available from the corresponding author upon reasonable request. Publicly available datasets were analyzed in this study. This data can be found here:https://physionet.org/content/mimiciv.
References
Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, et al. Liberal or restrictive transfusion after cardiac Surgery. N Engl J Med. 2015;372:997–1008.
Stokes EA, Wordsworth S, Bargo D, Pike K, Rogers CA, Brierley RC, et al. Are lower levels of red blood cell transfusion more cost-effective than Liberal levels after cardiac Surgery? Findings from the TITRe2 randomised controlled trial. BMJ Open. 2016;6(8):e011311.
Tay J, Allan DS, Chatelain E, Coyle D, Elemary M, Fulford A, et al. Liberal versus restrictive red blood cell transfusion thresholds in hematopoietic cell transplantation: a randomized, open label, phase III, noninferiority trial. J Clin Oncol. 2020;38(13):1463–73.
Stanworth SJ, Killick S, McQuilten ZK, Karakantza M, Weinkove R, Smethurst H, et al. REDDS Investigators.Red cell transfusion in outpatients with myelodysplastic syndromes: a feasibility and exploratory randomised trial. Br J Haematol. 2020;189(2):279–90.
So-Osman C, Nelissen R, Brand R, Faber F, Slaa RT, Stiggelbout A, et al. The impact of a restrictive transfusion trigger on post-operative complication rate and well-being following elective orthopaedic Surgery: a post-hoc analysis of a randomised study. Blood Transfus (Trasfusione Del Sangue). 2013;11(2):289–95.
Møller A, Nielsen HB, Wetterslev J, Pedersen OB, Hellemann D, Winkel P, et al. Low vs high hemoglobin trigger for transfusion in vascular Surgery: a randomized clinical feasibility trial. Blood. 2019;133(25):2639–50.
Møller A, Shahidi S, Wetterslev J, Helleman D, Pedersen OB, Marcussen KV, et al. Cardiac output in the transfusion triggers in vascular Surgery trial. Acta Anaesthesiol Scand. 2019;63:e12.
Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. 2016;316(19):2025–35.
Bergamin FS, Almeida JP, Landoni G, Galas F, Fukushima JT, Fominskiy E, et al. Liberal versus restrictive transfusion strategy in critically ill oncologic patients: the transfusion requirements in critically ill oncologic patients: randomized controlled trial. Crit Care Med. 2017;45(5):766–73.
Carson JL, Sieber F, Cook DR, Hoover DR, Noveck H, Chaitman BR, et al. Liberal versus restrictive blood transfusion strategy: 3-year survival and cause of death results from the FOCUS randomised controlled trial. Lancet. 2015;385(9974):1183–9.
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip Surgery. N Engl J Med. 2011;365(26):2453–62.
Almeida JP, Vincent JL, Galas FR, Almeida EP, Fukushima JT, Osawa EA, et al. Transfusion requirements in surgical oncology patients: a prospective, randomized controlled trial. Anesthesiology. 2015;122(1):29–38.
Ducrocq G, Gonzalez-Juanatey JR, Puymirat E, Lemesle G, Cachanado M, Durand-Zaleski I, et al. Effect of a restrictive vs Liberal blood transfusion strategy on major cardiovascular events among patients with acute Myocardial Infarction and anemia: the REALITY randomized clinical trial. JAMA. 2021;325(6):552–60.
Gillies MA, Ghaffar S, Moppett IK, Docherty AB, Clarke S, Rea N, et al. A restrictive versus Liberal transfusion strategy to prevent myocardial injury in patients undergoing Surgery for fractured neck of femur: a feasibility randomised trial (RESULT-NOF). Br J Anaesth. 2020;126:77–86.
Gregersen M, Damsgaard EM, Borris LC. Blood transfusion and risk of Infection in frail elderly after hip fracture Surgery: the TRIFE randomized controlled trial. Eur J Orthop Surg Traumatol. 2015;25(6):1031–8.
Laine A, Niemi T, Schramko Al. Transfusion threshold of hemoglobin 80 g/L is comparable to 100 g/L in terms of bleeding in cardiac Surgery: a prospective randomized study. J Cardiothorac Vasc Anesth. 2018;32(1):131–9.
Johnson A, Bulgarelli L, Pollard T, Horng S, Celi LA, Mark R. (2023). MIMIC-IV (version 2.2). PhysioNet. https://doi.org/10.13026/6mm1-ek67.
Johnson AEW, Bulgarelli L, Shen L, et al. MIMIC-IV, a freely accessible electronic health record dataset. Sci Data. 2023;10:1. https://doi.org/10.1038/s41597-022-01899-x.
Goldberger A, Amaral L, Glass L, Hausdorff J, Ivanov PC, Mark R, Stanley HE. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation [Online]. 2000;101(23):e215–20.
Mazer CD, Whitlock RP, Fergusson DA, Belley-Cote E, Connolly K, Khanykin B, et al. TRICS investigators and Perioperative Anesthesia clinical trials Group.Restrictive or Liberal red-cell transfusion for cardiac Surgery. N Engl J Med. 2017;377(22):2133–44.
Murphy GJ, Pike K, Rogers CA, et al. Liberal or restrictive transfusion after cardiac Surgery. N Engl J Med. 2015;372(11):997–1008.
Hajjar LA, Vincent JL, Galas FR, et al. Transfusion requirements after cardiac Surgery: the TRACS randomized controlled trial. JAMA. 2010;304(14):1559–67.
Karkouti K, Grocott HP, Hall R, et al. Interrelationship of preoperative anemia, intraoperative anemia, and red blood cell transfusion as potentially modifiable risk factors for acute kidney injury in cardiac Surgery: a historical multicentre cohort study. Can J Anaesth. 2015;62(4):377–84.
Acknowledgements
We thank all those who have been helpful to this manuscript.
Funding
No.
Author information
Authors and Affiliations
Contributions
Zhaokun Fan was responsible for the data extraction and manuscript preparation. Yinyin Shen modified the code. Chengen Li analyzed the data. Ruqin Yi optimized the tables and figures. Wei Chen and Wen Feng carried out literature search. Zhirong Zhang supervised and revised the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project was approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center (BIDMC) and the Massachusetts Institute of Technology (MIT). The waiver of informed consent was approved by the Institutional Review Board of BIDMC due to the de-identification of all protected health information. One author, Zhao kun Fan, completed the online course on Data or Specimens Only Research and gained access to the database for data extraction after passing the Collaborative Institutional Training Initiative (CITI) exam (Record ID: 55,303,422). We followed all relevant guidelines and regulations during the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fan, Zk., Zhang, Zr., Yi, Rq. et al. Hemoglobin levels and clinical outcomes after extracorporeal circulation auxiliary to open heart surgery: a retrospective cohort study. BMC Cardiovasc Disord 23, 598 (2023). https://doi.org/10.1186/s12872-023-03647-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03647-4