Abstract
Background
The present study aimed to detect subtle left ventricular (LV) dysfunction in patients with severe rheumatic mitral stenosis (MS) by measuring global and segmental longitudinal strain with a two-dimensional speckle tracking echocardiography (2D-STE) method.
Methods
In this case-control study, 65 patients with severe rheumatic MS and preserved ejection fraction (EF ≥ 50% measured by conventional echocardiographic methods) were compared with 31 otherwise healthy control subjects. All patients underwent LV strain measurement by the 2D-STE method in addition to conventional echocardiography using a VIVID S60 echocardiography device.
Results
Absolute strain values in myocardial segments 1–8, 10, and 12 (all basal, mid anterior, mid anteroseptal, mid inferior, and mid anterolateral segments) were significantly lower in patients with severe MS compared with the control group (P < 0.05 for all). The absolute global longitudinal strain (GLS) value was higher in the control group (-19.56 vs. -18.25; P = 0.006). After adjustment for age, gender, and systolic blood pressure, the difference in GLS between the two groups was as follows: mean difference=-1.16; 95% CI: -2.58–0.25; P = 0.110.
Conclusion
In patients with severe rheumatic MS and preserved EF, the absolute GLS tended to be lower than healthy controls. Furthermore, the segmental strain values of LV were significantly lower in most of the basal and some mid-myocardial segments. Further studies are warranted to investigate the underlying pathophysiology and clinical implications of this subclinical dysfunction in certain segments of patients with severe rheumatic MS.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Mitral stenosis (MS) is a hemodynamic abnormality of the mitral valve, usually resulting from thickened valve leaflets with restricted motion impeding normal blood flow [1]. In developing countries, MS is commonly caused by rheumatic heart disease, an autoimmune reaction to untreated streptococcal infection [2]. Previous studies have demonstrated that patients with MS may have concomitant left ventricular (LV) systolic dysfunction in conventional echocardiography using two-dimensional (2D) and M-mode measurements [3, 4].
Evaluation of LV ejection fraction (LVEF) is a simple global measurement of ventricular function. Still, it is associated with many limitations, such as dependency on the operator performing the study, the patient’s volume loading condition, and the chamber’s geometry. In addition, in many patients, using only routine parameters of conventional echocardiography is insufficient to demonstrate subtle LV dysfunction of the disease [5].
Speckle tracking echocardiography (STE) is a method of assessing cardiac function in which an echocardiographic device with the capability of identifying and tracking a certain point in the myocardium with specific echocardiographic characteristics within a block of speckles is used to determine the displacement of this speckle through the cardiac cycle. STE can calculate parameters like longitudinal, radial, or circumferential myocardial strain, global longitudinal strain (GLS), and strain rate [6,7,8,9]. However, longitudinal strain is generally believed to be a better predictor for various outcomes than other myocardial strain indices [10, 11]. Despite this advantage, segmental longitudinal strain measurement may be subject to high variability and intervendor bias compared to GLS. Nevertheless, it can be utilized alongside GLS to provide a more complete picture of myocardial strain [12]. GLS measurement is a sensitive method to evaluate LV dysfunction that can demonstrate myocardial abnormality without any reduction in ejection fraction (EF), and it can be used in risk stratification of patients [13,14,15].
Therefore, in the current study, we aimed to detect the presence and distribution of subclinical LV dysfunction in patients with severe MS but preserved EF by segmental and global longitudinal strain measurement using 2D-STE method.
Methods
Study population
The target population of our study was patients with severe rheumatic MS who were referred to the echocardiography laboratory at our medical center from June 2020 to June 2021. The inclusion criteria were EF ≥ 50% and echocardiographic features of rheumatic mitral valve stenosis. Exclusion criteria included atrial fibrillation rhythm, known coronary artery disease, concomitant moderate or severe mitral regurgitation, aortic stenosis or insufficiency (according to 2020 ACC/AHA guidelines) [16], previous balloon mitral valvotomy (BMV) or any open cardiac surgery, end-stage renal failure, hepatic cirrhosis, metastatic cancer, diabetes or uncontrolled hypertension, poor standard echocardiographic views to obtain all needed variables as well as beta-blocker therapy. In addition, patients with cardiomyopathies such as hypertrophic cardiomyopathy or cardiac amyloidosis, and bundle branch or any other conduction block in ECG were not included.
A total of 65 patients with severe rheumatic MS were selected as the case group, and 31 otherwise healthy subjects as the control group. The study protocol was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.THC.REC.1399.035) and was performed under the Declaration of Helsinki. All patients provided written informed consent before enrollment.
Examinations
Demographic characteristics were registered for all subjects. Systolic and diastolic blood pressure (SBP and DBP) were measured from both arms after 15 min of rest in a sitting position, and the mean values were recorded. Heart rate was counted in one minute after 15 min of rest.
Complete trans-thoracic echocardiography, including strain study by 2D speckle tracking method in two, three, and four-chamber views, was performed by an experienced echocardiologist using the same echocardiography device (VIVID S60, GE Healthcare, US with 3SC transducer) for all participants. We used the modified Simpson method (biplane method of disks) with the tracing of LV cavity area in both apical four-chamber and apical two-chamber views to measure LVEF according to ASE recommendations [17]. The analysis was performed on the scanner directly using automated function imaging. The software version was Echopac 202.
Echocardiographic data, including other valvular heart diseases, data related to mitral annular tissue velocities (septal é and lateral é), LV end-systolic and end-diastolic dimensions and left atrial area (by biplane area-length method) were all obtained for both groups. In addition, the mitral valve area (MVA) was measured by 2D planimetry, and the Wilkins score was calculated for the case group. MS severity was determined based on the MVA measurement. Patients with MVA < 1.5 cm² were included in the study (severe MS) [18].
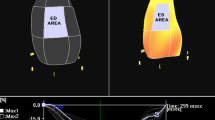
Segmental longitudinal strain measurement was performed in both groups using the 2D-STE method. GLS was calculated by automatically averaging the strain values of all myocardial segments obtained by the device [7, 19]. Segmentation of LV myocardium was based on the American Heart Association’s (AHA) 17-segment model as follows: (1) Basal anterior (2) Basal anteroseptal (3) Basal inferoseptal (4) Basal inferior (5) Basal inferolateral (6) Basal anterolateral (7) Mid anterior (8) Mid anteroseptal (9) Mid inferoseptal (10) Mid inferior 11. Mid inferolateral 12. Mid anterolateral 13. Apical anterior 14. Apical septal 15. Apical inferior 16. Apical lateral 17. Apex (Fig. 1) [20]. Figure 2 demonstrates our strain measurement method using Bull’s eye plot in a patient with severe rheumatic MS. The image was taken after the study completion and is from a patient referred to our center but not included in this study.
Bull’s eye plot in a patient with severe rheumatic MS showing reduced segmental longitudinal strain values in basal and some mid myocardial segments despite good global longitudinal strain. As presented in the image, three 2-D echocardiographic views, including 4, 3, and 2 chamber apical views with a focus on LV, were used to assess global and longitudinal strain values. To perform, in each view, three points were plotted manually at the base of each opposing wall as well as the apex using a point-and-click technique, and then the endocardial border was automatically traced by the software. The software divides the region of interest in each view into six segments, and the quality of tracing of each segment is automatically scored as either acceptable or unacceptable with the possibility of further correction manually. Finally, the software calculates global and segmental strains, displaying the values. (The figure is only for demonstration of the technique and was not taken from an included patient in the study)
Statistical analysis
Continuous variables were presented as mean (standard deviation) and were compared between two groups using the independent t-test. Categorical variables were expressed as frequency (percentage) and were compared between groups applying Chi2 or Fisher’s exact test, as appropriate. The adjusted effect of severe MS on segmental and global longitudinal strain was evaluated using an ANOVA-ANCOVA model. Age, gender, and SBP were considered potential confounders, so the adjustment was applied for these items.
Cohen’d and Partial Eta squared were also reported. Since all patients with severe MS in this study had moderate Wilkins scores between 8 and 12, no adjustment was applied based on this score. The sample size was measured using an alpha error probability of 5%, statistical power of 95%, and “effect size d” of 0.75. A 2:1 ratio (cases: controls) was employed for sample size calculation, resulting in 59 cases and 29 controls. Sample size calculation was performed using G power software version 3.1. All other statistical analyses were conducted with IBM SPSS for Windows, version 23.0 (IBM Corp., Armonk, N.Y., USA).
Results
From 210 MS patients referred to our echocardiography lab, 65 (30.9%) were included. We analyzed 65 severe MS patients (83% female, 54 ± 11 years old) and 31 control subjects (48% female, 42 ± 12). Severe MS patients had an MVA of 1.15 ± 0.21 cm2 by 2D planimetry, a mean gradient of 7.12 ± 3.24 mmHg by Doppler assessment, and a Wilkins score of 9.48 ± 0.92. The average heart rate was 70.49 ± 14.20 at the time of gradient assessment. Aortic insufficiency (AI) and mitral regurgitation (MR) with less than moderate severity were more prevalent in patients with severe MS in comparison with the control group (p value < 0.001). Subjects with moderate or more severe mitral or aortic regurgitation were already excluded from the study. Tissue velocities were significantly lower in severe MS patients than in normal subjects (P < 0.001). Additionally, the left atrial area was significantly larger in severe MS patients compared to the controls (25.48 cm² vs. 15.13 cm², P < 0.001, Table 1).
Absolute value for GLS and strain in myocardial segments 1–8, 10, and 12 (all basal, mid anterior, mid anteroseptal, mid inferior, and mid anterolateral segments) were significantly lower in patients with severe MS in comparison with the controls (P < 0.05 for all), while only in segment 13 (apical anterior segment) segmental strain in the case group showed higher absolute value than the control group. Differences in other segments were not statistically significant (Table 2). Figure 1 compares the differences in strain values of different heart segments between the case and control groups.
On average, the absolute value of GLS in severe MS patients was 1.31 lower than in controls (P = 0.006, 95%CI: -2.24 – -0.39, Cohen’s d= -0.5). The differences in segments 1–8, 10, and 12 were also statistically significant. Cohen’s d analysis also showed medium to large effect size differences in these segments. After statistical adjustment, the absolute value of GLS in severe MS patients was still 1.16 lower than in control subjects, but this difference was not statistically significant anymore (P = 0.110, 95% CI: -2.58–0.25). Differences in segments 1, 2, 3, 4, 6, 8, 10, and 12 were still significant after adjustment for confounding factors (Tables 2 and 3).
Discussion
In brief, we conducted a case-control study of MS patients and otherwise healthy subjects, all with normal EF. Patients underwent 2D-STE exam. Longitudinal strain and GLS were measured and compared between the two groups. The absolute average value for GLS was lower in MS patients than in controls but did not reach statistical significance. On the other hand, the absolute strain values for basal and mid-myocardial segments were significantly lower in the MS subjects.
It is estimated that MS has a prevalence of 51.21 per 100,000 in developing countries [21]. It has been suggested that a subset of MS patients, despite normal EF, may have some degree of LV dysfunction [22]. This myocardial dysfunction can be detected in STE by a lower absolute value of segmental and global strain [13,14,15]. Gerede et al. proposed that MS patients with a GLS value of under − 16.98 or a GLS rate of under − 1.45 had a faster disease progression [23]. This highlights the need for closer follow-up in MS patients with lower strain rates.
In a study by Sengupta et al., 57 patients with severe MS and 19 healthy controls underwent 2D speckle tracking-based GLS measurement. Patients with severe MS had lower LVEF and absolute GLS values than the control group. GLS in 48 (84.2%) patients with severe MS was below the 25th percentile of controls. After BMV, GLS was significantly improved (before: -14.6 ± 3.3% vs. after: -17.8 ± 3.5%) [24]. In a similar study on 72 patients with isolated MS and 31 controls, no significant difference was found in LVEF and LV end-systolic or diastolic dimensions between the two groups. Absolute GLS in patients with MS was significantly lower than in the control group. Interestingly, no significant differences in GLS measurements among MS sub-groups (mild, moderate, and severe) were reported [25].
In our study, MS patients had lower absolute strain values compared to controls in the basal and middle segments (1–4, 6, 8, 10, and 12). While some studies have had similar results, others have reported differences in strain values of all segments. For instance, Simsek et al. study on 32 patients with isolated MS and 25 healthy controls demonstrated that absolute values of peak systolic strain and strain rate of all heart segments in patients with MS were significantly lower than in healthy subjects. This study used a different method of heart segmentation with 12 segments [26]. On the other hand, Ozdemir et al. showed that patients with severe MS had a reduced longitudinal peak strain and strain rate in all basal and some mid-segments of the left ventricle [27]. In Roushdy et al. investigation, left and right ventricular GLS measurements were performed on 32 patients with MS and 30 healthy subjects. It noted that left and right ventricular absolute GLS values in patients with MS were lower than the control group (-16.5 ± 2.7% vs. -21.0 ± 1.5 and − 18.3 ± 4.7 vs. -19.8 ± 1.3, respectively). The strain measurements in basal and septal segments and RV free wall were significantly decreased. After BMV, examinations were repeated within 24 h and three months later in patients with MS. Compared with baseline values, left and right ventricular absolute GLS were significantly increased within 24 h after BMV. This increase was maintained after three months [22].
LV dysfunction is frequently observed in MS patients [28]. Although LV dysfunction can present with reduced EF, some MS patients may have subclinical LV dysfunction with preserved EF. The exact underlying mechanisms are still up for debate. Some studies, like Sengupta et al., suggested that LV dysfunction is mainly due to hemodynamic abnormality of the heart and can be reversible after valvulotomy [24]. A possible explanation is valvulotomy increases the preload, thus increasing LV end-diastolic volume (LVED). Increased LVED is then believed to improve LV function. Other studies suggest that there may be an intrinsic LV abnormality in MS that may not be completely reversible with valvulotomy [29]. McKay et al. showed that there was either no change or minimal increase in LVED volume after balloon valvuloplasty in MS patients [30]. These findings contradict the reduced LVED theory [28, 31]. Regardless of the mechanism, LV-GLS measurement can aid in detecting subclinical LV dysfunction in rheumatic MS patients with preserved EF.
There is also some pathological evidence on the topic. Waller et al. described the histology of excised stenotic mitral valves and reported evidence of Aschoff bodies in the interstitial tissue of the myocardium [32]. Although the clinical significance of Aschoff bodies is unknown, Waller et al. suggested that they may represent previous fibrinoid necrosis in the heart. This hypothesis may also be reasonable from a pathophysiological point of view. Rheumatic MS is a delayed complication of acute rheumatic fever attack involving all three heart layers (endocardium, myocardium, and pericardium). Although the attack is acute, the inflammation appears to continue and cause fibrosis and scarring of the mitral apparatus. It may be presumable that similar mechanisms also result in endocardium and myocardium fibrosis, as Klein et al. suggested [28]. It has been hypothesized that this fibrosis may extend from the mitral apparatus to the adjacent myocardium, explaining the difference in strain values of basal segments between MS patients and the normal population [22, 27, 33]. Still, there is no conclusive evidence confirming these assumptions. Another hypothesis is that the fibrotic mitral valve can cause poster-basal wall motion abnormality by having a tethering effect [34].
It is noteworthy that segments 13–15 and 17 showed slightly higher absolute strains in severe MS patients than in controls. While the difference in the strain value of these segments was mainly negligible, the strain value for segment 13 was notably higher in the cases. We believe this contradictory finding in this single myocardial segment may be due to some technical error in accurate image acquisition of the apical-anterior segment in the apical two-chamber view and should be assessed more in future studies. Another explanation is that there may be inaccuracies in tracking because of poor image quality or the operator missing control of the tracking.
Limitations
A major limitation of the current study was the non-matched case-control design. ANOVA-ANCOVA statistical adjustment was used to overcome the important differences in baseline characteristics, and the final results were mainly expectable and compatible with the pathophysiology of rheumatic MS. In addition, we showed that while the absolute strain value was lower in the basolateral segments in the cases compared to controls, in some apical segments, such as segment 13, it might be higher among the cases. Thus, it is presumable that the GLS index alone may not be accurate enough to identify myocardial dysfunction, and longitudinal strain of other segments is required to provide a complete picture.
Another limitation was the rather small sample size of the study, which stems from the rarity of severe rheumatic MS patients. However, this was a common shortcoming among similar studies on this topic. Additionally, intraobserver variability was not measured in the current study. Finally, the imaging artifacts due to respiration may have affected strain measurements’ quality. To solve this issue, we performed image acquisitions at the end of expiration with three registered cycles.
Conclusion
In patients with severe rheumatic MS and preserved EF, the absolute GLS tended to be lower than healthy controls. Furthermore, the segmental strain values of LV were significantly lower in most of the basal and some mid-myocardial segments. Further studies are warranted to investigate the underlying pathophysiology and clinical implications of this subclinical dysfunction in certain segments of patients with severe rheumatic MS.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to Tehran Heart Center’s policy but are available from the corresponding author upon reasonable request.
References
Iung B, Vahanian A. Epidemiology of acquired Valvular Heart Disease. Can J Cardiol. 2014;30:962–70.
Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A. A prospective survey of patients with valvular Heart Disease in Europe: the Euro Heart Survey on Valvular Heart Disease. Eur Heart J. 2003;24:1231–43.
Shikano M, Nakatani S, Kim J, et al. Impaired left ventricular systolic function in mitral stenosis. J Cardiol. 2003;42:75–9.
Park KJ, Woo JS, Park JY, et al. Clinical effect of left ventricular dysfunction in patients with mitral stenosis after mitral valve replacement. Korean J Thorac Cardiovasc Surg. 2016;49:350–55.
Younan H. Role of two dimensional strain and strain rate imaging in assessment of left ventricular systolic function in patients with rheumatic mitral stenosis and normal ejection fraction. Egypt Heart J. 2015;67:193–98.
Tryfou ES, Kostakou PM, Kostopoulos VS, et al. Pathophysiological alterations of left ventricular myocardial systolic function during normal pregnancy assessed by speckle tracking echocardiography: a prospective cohort echocardiography study. Int J Cardiovasc Imaging. 2022;38:2677–86.
Yang H, Wright L, Negishi T, et al. Research to practice: Assessment of Left Ventricular Global Longitudinal strain for Surveillance of Cancer Chemotherapeutic-Related Cardiac Dysfunction. JACC Cardiovasc Imaging. 2018;11:1196–201.
Blessberger H, Binder T. Two dimensional speckle tracking echocardiography: clinical applications. Heart. 2010;96:2032–40.
Battel O, Newsome K, Izquierdo-Pretel G. Global longitudinal strain as an efficient Prognostic Tool in Hypertrophic Cardiomyopathy with preserved left ventricular ejection Fraction. Cureus. 2022;14:e30573.
Zhang K, Sheu R, Zimmerman NM, et al. A comparison of global longitudinal, circumferential, and Radial strain to predict outcomes after cardiac Surgery. J Cardiothorac Vasc Anesth. 2019;33:1315–22.
Aarsaether E, Rösner A, Straumbotn E, et al. Peak longitudinal strain most accurately reflects myocardial segmental viability following acute Myocardial Infarction - an experimental study in open-chest pigs. Cardiovasc Ultrasound. 2012;10:23.
Mirea O, Pagourelias ED, Duchenne J, et al. Variability and reproducibility of segmental longitudinal strain measurement: a Report from the EACVI-ASE strain standardization Task Force. JACC: Cardiovasc Imaging. 2018;11:15–24.
Potter E, Marwick TH. Assessment of Left ventricular function by Echocardiography: the case for routinely adding global longitudinal strain to Ejection Fraction. JACC Cardiovasc Imaging. 2018;11:260–74.
Smiseth OA, Torp H, Opdahl A, et al. Myocardial strain imaging: how useful is it in clinical decision making? Eur Heart J. 2016;37:1196–207.
Voigt J-U, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2015;16:1–11.
Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the management of patients with Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation. 2021;143:e72–e227.
Douglas PS, Carabello BA, Lang RM et al. 2019 ACC/AHA/ASE Key Data Elements and Definitions for Transthoracic Echocardiography: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Clinical Data Standards for Transthoracic Echocardiography) and the American Society of Echocardiography. Circulation: Cardiovascular Imaging 2019;12:e000027.
Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the management of patients with Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. Circulation. 2014;129:2440–92.
Norum IB, Ruddox V, Edvardsen T, et al. Diagnostic accuracy of left ventricular longitudinal function by speckle tracking echocardiography to predict significant coronary artery stenosis. A systematic review. BMC Med Imaging. 2015;15:25.
Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42.
Moghaddam VK, Dickerson AS, Bazrafshan E, et al. Socioeconomic determinants of global distribution of multiple sclerosis: an ecological investigation based on global burden of Disease data. BMC Neurol. 2021;21:145.
Roushdy AM, Raafat SS, Shams KA, et al. Immediate and short-term effect of balloon mitral valvuloplasty on global and regional biventricular function: a two-dimensional strain echocardiographic study. Eur Heart J Cardiovasc Imaging. 2016;17:316–25.
Gerede DM, Ongun A, Tulunay Kaya C, et al. Use of strain and strain rate echocardiographic imaging to predict the progression of mitral stenosis: a 5-year follow-up study the progression of mitral stenosis: a 5-year follow-up study. Anatol J Cardiol. 2016;16:772–77.
Sengupta SP, Amaki M, Bansal M, et al. Effects of percutaneous balloon mitral valvuloplasty on left ventricular deformation in patients with isolated severe mitral stenosis: a speckle-tracking strain echocardiographic study. J Am Soc Echocardiogr. 2014;27:639–47.
Bilen E, Kurt M, Tanboga IH, et al. Severity of mitral stenosis and left ventricular mechanics: a speckle tracking study. Cardiology. 2011;119:108–15.
Simşek Z, Karakelleoğlu S, Gündoğdu F, et al. Evaluation of left ventricular function with strain/strain rate imaging in patients with rheumatic mitral stenosis. Anadolu Kardiyol Derg. 2010;10:328–33.
Ozdemir AO, Kaya CT, Ozcan OU, et al. Prediction of subclinical left ventricular dysfunction with longitudinal two-dimensional strain and strain rate imaging in patients with mitral stenosis. Int J Cardiovasc Imaging. 2010;26:397–404.
Klein AJP, Carroll JD. Left ventricular dysfunction and mitral stenosis. Heart Fail Clin. 2006;2:443–52.
FEIGENBAUM H, CAMPBELL RW, WUNSCH CM, et al. Evaluation of the left ventricle in patients with mitral stenosis. Circulation. 1966;34:462–72.
McKay CR, Kawanishi DT, Kotlewski A, et al. Improvement in exercise capacity and exercise hemodynamics 3 months after double-balloon, catheter balloon valvuloplasty treatment of patients with symptomatic mitral stenosis. Circulation. 1988;77:1013–21.
Venkateshvaran A, Govind SC. Left ventricular diastolic function in mitral stenosis. Echocardiography. 2020;37:1944–50.
Waller BF, Howard J, Fess S. Pathology of mitral valve stenosis and pure mitral regurgitation–part I. Clin Cardiol. 1994;17:330–36.
Leitman M, Vered Z. Speckle-tracking imaging for the progression of mitral stenosis. Anatol J Cardiol. 2016;16:778.
Galli E, Lancellotti P, Sengupta PP, et al. LV mechanics in mitral and aortic valve Diseases: Value of Functional Assessment Beyond Ejection Fraction. JACC: Cardiovasc Imaging. 2014;7:1151–66.
Acknowledgements
This study was supported by Tehran Heart Center, Cardiovascular Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
Funding
None.
Author information
Authors and Affiliations
Contributions
S.N and S.MP wrote the manuscript.S.N and R.H revised the manuscript.R.H and M.G designed the study.A.J and A.VB performed the statistical analysis.A.S prepared the figures.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Tehran University of Medical Sciences ethics committee (IR.TUMS.THC.REC.1399.035). All methods were performed in accordance with the Helsinki Declaration. Informed consent was obtained from all participants at the start of the study.
Consent for publication
Informed consent for publication of clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mehrabi-Pari, S., Nayebirad, S., Shafiee, A. et al. Segmental and global longitudinal strain measurement by 2-dimensional speckle tracking echocardiography in severe rheumatic mitral stenosis. BMC Cardiovasc Disord 23, 584 (2023). https://doi.org/10.1186/s12872-023-03624-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03624-x