Abstract
Background
ST-elevation myocardial infarction (STEMI) is a major public health problem. This study aimed to determine the prevalence and identify the determinants of STEMI-related complications in the Cardiology Intensive Care Unit of the Sud Francilien Hospital Center (SFHC).
Methods
We retrospectively analyzed the data of 315 patients with STEMI aged ≥ 18 years. Logistic regression was used to identify factors independently associated with the occurrence of complications.
Results
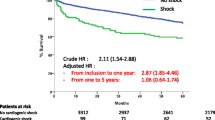
Overall, 315 patients aged 61.7 ± 13.4 years, of whom 261 were men, had STEMI during the study period. The hospital frequency of STEMI was 12.7%. Arrhythmias and acute heart failure were the main complications. Age ≥ 75 years (adjusted odds ratio [aOR], 5.18; 95% confidence interval [CI], 3.92–8.75), hypertension (aOR, 3.38; 95% CI, 1.68–5.82), and cigarette smoking (aOR, 3.52; 95% CI, 1.69–7.33) were independent determinants of acute heart failure. Meanwhile, diabetes mellitus (aOR, 1.74; 95% CI, 1.09–3.37), history of atrial fibrillation (aOR, 2.79; 95% CI, 1.66–4.76), history of stroke or transient ischemic attack (aOR, 1.99; 95% CI, 1.31–2.89), and low high-density lipoprotein-cholesterol (HDL-C) levels (aOR, 3.70; 95% CI, 1.08–6.64) were independent determinants of arrhythmias.
Conclusion
STEMI is a frequent condition at SFHC and is often complicated by acute heart failure and arrhythmias. Patients aged ≥ 75 years, those with hypertension or diabetes mellitus, smokers, those with a history of atrial fibrillation or stroke, and those with low HDL-C levels require careful monitoring for the early diagnosis and management of these complications.
Similar content being viewed by others
Background
The prevalence of cardiovascular diseases (CVDs) has almost doubled in the previous three decades, from 271 million in 1990 to 523 million in 2019. Mortality from these diseases also increased steadily during this period, from 12.1 million in 1990 to 18.6 million in 2019 [1],which is one-third of the total global mortality [1,2,3].
Ischemic heart disease (IHD) is undoubtedly the most common form of CVD [4]. Despite tremendous achievements in its management, IHD remains one of the leading causes of premature death, disability, and human suffering worldwide [4, 5]. The global prevalence of IHD is rising, with the 2017 prevalence rate of 1,655 per 100,000 individuals expected to exceed 1,845 by 2030 [5]. Furthermore, IHD is recognized as a real threat to sustainable development in the 21st century [6].
Acute coronary syndrome (ACS) is the most severe and life-threatening manifestation of IHD, with an annual incidence of approximately 7 million worldwide [7].
Since the European Society of Cardiology (ESC)/American College of Cardiology Foundation/American Heart Association/World Heart Federation expert consensus of 2012 [8], ACS has been distinguished into two main types: ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (non-STEMI). The two categories have differences in terms of clinical manifestations, pathology, pathogenesis, treatment, and prognosis [9,10,11,12,13]. The study by Vernon et al., demonstrating a substantial increase in the number of patients with STEMI without standard modifiable cardiovascular risk factors (CVRFs) [14], has shown that there remain gray areas in our understanding of the pathogenic mechanisms of STEMI. Besides, a recent French population-based registry analyses from the Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) project has shown that the vital prognosis is worse in the short term in patients with STEMI than in those with non-STEMI [15].
The emergence of new therapies, particularly the advent of thrombolytics, the rise of coronary units, the development of pre- and per-procedural pharmacological support, and the organization of pre- and intra-hospital care have significantly reduced hospital mortality from STEMI [16,17,18].
Despite this recent decrease in mortality, STEMI remains a diagnostic and therapeutic emergency involving short-, medium-, and long-term vital prognosis and requires early, rapid, and appropriate management [19].
The complexity of acute STEMI management lies in the many unexpected complications that can enamel its evolution, particularly heart failure [20], rhythmic disorders [21, 22], and mechanical complications [23]. These complications decline over time, without completely disappearing, with the advent of the aforementioned new management strategies, and are always accompanied by an exceptionally high mortality rate and are one of the main causes of death in the early phase following MI [24].
Nowadays, due to the revolution and modernization of ACS management, only a few studies have addressed these complications and resulted in divergent results, both for the frequency and for the factors associated with the occurrence of these complications; some of the most cited factors for the occurrence of these complications were as follows: race/ethnicity [25, 26] and sex disparities [26]; the existence of chronic kidney disease; diabetes mellitus; high total cholesterol, low-density lipoprotein (LDL) cholesterol, and high-sensitivity C-reactive protein levels [27]; prior heart failure; anemia; multivessel disease; and anterior location [28].
Not only the different methodological approaches used in these different studies but also the large regional variation in clinical profiles demonstrated in patients with STEMI [29] could explain these discrepancies.
Of note, most studies have addressed both STEMI and non-STEMI simultaneously. In the scientific literature, information on both the frequency and determinants of acute complications specific to STEMI in Essonne, France, is lacking. Thus, this study aimed to determine the in-hospital prevalence and factors associated with the occurrence of acute complications of STEMI. This information could be considered in developing decision-making algorithms for managing STEMI and could contribute to reducing mortality.
Methods
Study design and setting
This retrospective single-center analysis of the records of patients with STEMI admitted to the Cardiology Intensive Care Unit (CICU) of the Sud Francilien Hospital Center (SFHC), in the French Republic, was conducted from January 1, 2020 to December 31, 2021. The SFHC is located in Essonne, in the cities of Corbeil-Essonnes and Yerres. It provides hospital coverage for approximately 600,000 inhabitants (all of Essonne, south of Seine-et-Marne, and southeast of Val-de-Marne, France).
Sample size calculation
A sample size of 322 was estimated taking the frequency of STEMI as 40% of French MONICA registries [30] (confidence level = 95% and margin of error = 5%).
Patient selection
This study included all men and women aged at least 18 years who had been hospitalized for STEMI between January 1, 2020 and December 31, 2021.
Patients admitted for STEMI but who arrived ≥ 24 h after the onset of symptoms and those whose medical records lacked variables of interest were excluded from the study.
Study procedures
All medical records of the patients admitted for STEMI were retrieved and carefully reviewed by two researchers (JMMM and AK) to obtain relevant data on the parameters of interest, which included sociodemographic data (i.e., age, sex, and occupation); CVRFs (i.e., hypertension, diabetes mellitus, dyslipidemia, cigarette smoking, obesity, and coronary heredity); history (i.e., IHD, obliterating arterial disease of the lower limbs, carotid angioplasty or coronary artery bypass surgery, heart rhythm disorder, stroke/TIA, heart failure, chronic renal failure, neoplasia, pulmonary embolism, and coronavirus disease 2019 [COVID-19]); clinical data (i.e., blood pressure, heart rate, and oxygen saturation); electrocardiographic aspects (i.e., ST segment elevation, presumed recent left bundle brunch, rhythm, and conduction disorders); echocardiographic characteristics (i.e., left ventricular ejection fraction using Simpson’s biplane method and kinetic disorders); biological data (i.e., serum creatinine, renal creatinine clearance according to the Modification of Diet in Renal Disease equation, glycated hemoglobin (HbA1c), total cholesterol, LDL-cholesterol, high-density lipoprotein [HDL]-cholesterol, and triglycerides); coronary angiographic lesions (i.e., type and number of occluded coronaries [i.e., monotroncular, bitroncular, and tritroncular]); the number of stents implanted; rhythmic and conductive post-coronarography disorders (i.e., atrial, junctional, and ventricular arrhythmias); and hemodynamic (i.e., acute heart failure with or without acute pulmonary edema or cardiogenic shock), mechanical and embolic (i.e., ischemic stroke) complications.
All patients underwent primary percutaneous coronary intervention and were continuously evaluated and monitored for temperature, systolic and diastolic blood pressure, SpO2, heart rate frequency, and 12-lead electrocardiogram ECG within 24 h of admission to the CICU. These parameters were remotely monitored using a multi-parameter portable vital signs monitor (BeneVision N22/N19, Mindray, Mahwak, USA). Moreover, a follow-up examination was performed, which included symptoms (such as dyspnea, chest pain, and palpitations) and biological parameters (such as complete blood count, creatinine, ionogram, glycaemia, troponin, creatinine phosphokinase, C-reactive protein, prothrombin time, and activated partial thromboplastin time). All complications from the initial contact with emergency medical services up 24 h after the admission to the CICU were considered in this study. All patients were treated according to the ESC guidelines for managing acute MI in patients presenting with ST elevation [31].
Operational definitions
The following definitions were used in this study:
According to the 2017 recommendations of the ESC [31], STEMI was defined as chest pain associated with the following: A new ST elevation at the J point in at least two contiguous or adjacent leads: in V2–V3 ≥ 0.2 mV (2 mm) in men after 40 years (≥ 0.25 mV before 40 years)) and ≥ 0.15 mV (1.5 mm) in females or ≥ 0.1 mV (1 mm) in other leads; a left bundle branch block in the presence of the Smith criteria [32, 33]; or new ST depression from V1 to V3 (V4) on a 12-lead tracing, associated with ST elevation ≥ 0.5 mm in at least two leads from V7 to V9.
Dyslipidemia was defined as an LDL-cholesterol level ≥ 1.6 g/L and/or an HDL-cholesterol level ≤ 0.40 g/L in men and ≤ 0.50 g/L in women and/or a total cholesterol level ≥ 2 g/L and/or a triglyceride level ≥ 1.5 g/L [34]. LDL-cholesterol was calculated using the Friedewald method as LDL-cholesterol (g/L) = CT (g/L) − HDL-cholesterol (g/L) − triglyceride (g/L)/5 (if the triglyceride level was ≤ 3.4 g/L) [34, 35]. It was directly dosed using the dextran sulfate filtration technique if the triglyceride level was > 3.4 g/L [34, 36].
Left ventricular ejection fraction (LVEF) values were categorized into three groups according to the 2021 ESC recommendations [37], as follows: “reduced” when the LVEF was ≤ 40%; “mildly reduced” when the LVEF was between 40% and 49%; and “preserved” when the LVEF was ≥ 50%.
Statistical analyses
The qualitative data are represented as absolute (n) and relative frequencies (%), and the quantitative data are presented in the form of means ± standard deviations (if the distribution is normal) or medians with their quartile interquartile ranges (if the distribution is asymmetric). The distribution of each variable was assessed using the Kolmogorov–Smirnov test. Simple logistic regression was used to determine which factors were predictive of complications. The following variables were entered into the univariate analysis: age group (< 55, 55–75, and > 75 years), CVRFs (i.e., hypertension, diabetes mellitus, dyslipidemia, obesity, cigarette smoking, and coronary heredity), medical history (i.e., stented IHD, coronary artery bypass surgery, previous atrial fibrillation, previous stroke, heart failure, chronic kidney disease, peripheral artery occlusive disease, neoplasia, pulmonary embolism, and COVID-19), the number of occluded vessels (i.e., monovessel, bivessel, and trivessel), and LVEF (i.e., reduced, moderately reduced, and preserved). The odds ratios (ORs) and their 95% confidence intervals (95% CIs) were finally calculated to assess the degree of association between the variables and occurrence of complications. When the associations were observed between complications and these independent variables, the effects of potential confounders were examined by adjustment in a conditional logistic regression (multivariate analysis). The significance threshold retained was p < 0.05. All data were analyzed using Statistical Package for the Social Sciences (version 24; IBM Corp., Armonk, NY).
Results
Characteristics of the study population
The study population consisted of 315 patients, with a mean age of 61.7 ± 13.4 years; of the 315 patients, 261 were men and 54 were women, with a sex ratio of 4.8 (in favor of men).
Hospital frequency of STEMI
Overall, 2,479 patients were hospitalized in the CICU-SFHC during the study period. Among them, 315 presented with STEMI, with a frequency of 12.7%.
Sociodemographic characteristics of the study population according to sex
Table 1 shows the sociodemographic characteristics of the population. The mean age of patients was 61.7 ± 13.4 years, and 47.6% were aged 55–75 years. The same table shows that retirees were the most represented professional category.
CVRFs of the study population
As illustrated in Table 2, the main CVRFs were cigarette smoking (58.4%), hypertension (42.9%), dyslipidemia (25.4%), and obesity (19.4%).
Medical history
The patients’ medical history is shown in Table 3. It was dominated by stented IHD (15.2%), followed by neoplasia (7%), atrial fibrillation (3. 5%), and chronic kidney disease (2.5%).
Coronagraphic characteristics of the patients
The coronary angiographic characteristics of the patients are shown in Table 4. Monovessel lesions were the most common (59%), followed by bivessel lesions (27.3%) and trivessel lesions (13.7%). The left anterior descending artery (LADA) was the most often affected artery (49.46%) in patients with monovessel lesions. Regarding bivessel lesions, the LADA and right coronary artery (RCA) were the most often affected blood vessels (44.18%). As for trivessel lesions, the LADA, left coronary artery, and RCA was the most affected blood vessels (58.13%).
Echocardiographic characteristics
The distribution of the patients’ echocardiographic findings is reported in Table 5. The mean LVEF was 50.61 ± 10.9%. Furthermore, 62.86% of the patients had an LVEF ≥ 50%, 24.13% had an LVEF between 40% and 49%, and 13.02% had an LVEF ≤ 40%. Overall, segmental kinetics disorders predominated in the anterior parts (41.9%) followed by the inferior parts (38.71%).
Clinical and biological characteristics of the patients
The clinical and biological characteristics of the patients are shown in Table 6. On admission, the average values for the biological parameters, systolic and diastolic blood pressure, heart rate, and oxygen saturation were all within the normal range.
Kinetics of cardiac enzymes
The cardiac enzyme kinetics of all patients studied are present in Table 7. Notably, troponin levels at admission increased seven-fold before subsequently decreasing, whereas creatinine phosphokinase levels tripled before decreasing.
Distribution of complications
The patient complications are listed in Table 8. Arrhythmias (22.85%) and Killip class ≥ 2 acute heart failure (13.01%) were the most frequent complications.
Among the rhythm disorders, ventricular rhythm disorders accounted for 13.64% and supraventricular rhythm disorders accounted for 9.21%, including atrial fibrillation (8.57%).
Bivariate and multivariate analyses of the factors associated with the occurrence of hemodynamic disorders
Table 9 shows that age ≥ 75 years, hypertension, cigarette smoking, and previous atrial fibrillation were the factors associated with the onset of acute heart failure. After adjustment in the multivariate analysis, only age ≥ 75 years, hypertension, and cigarette smoking emerged as independent determinants of the occurrence of acute heart failure. The risk of developing acute heart failure was increased by five in the presence of an age ≥ 75 years, by three in the presence of hypertension, and by four in the presence of cigarette smoking.
Bivariate and multivariate analyses of factors associated with arrhythmias
Table 10 shows that diabetes mellitus, stroke history, atrial fibrillation history, chronic kidney disease, and low HDL-C levels were the factors associated with the onset of arrhythmias.
After adjustment in the multivariate analysis, diabetes mellitus, history of atrial fibrillation, history of stroke, and low HDL-C levels persisted as the independent factors for the onset of arrhythmias. Low HDL-C levels multiplied this risk by four, history of AF multiplied this risk by three, and diabetes mellitus and stroke multiplied this risk by two.
Discussion
This study aimed to evaluate the frequency and identify the determinants of complications occurring in patients admitted to the CICU-SFHC for STEMI, in the French Republic, from January 1 to December 31, 2021.
The hospital frequency of STEMI was 12.7%. The main complications were rhythmic (22.85%) and hemodynamic (13.1%). Age ≥ 75 years, hypertension, and cigarette smoking emerged as independent determinants of hemodynamic complications. Meanwhile, diabetes mellitus, history of atrial fibrillation, stroke/TIA, and low HDL-C levels have emerged as independent determinants of arrhythmias.
This is one of the few studies to examine the prevalence of acute complications of STEMI in the era of structured and modernized organization of emergency and cardiac intensive care units.
Before the use of early reperfusion therapy (1960 to 1980 s), the frequency of arrhythmias was elevated following ACS [38,39,40,41,42]. However, a marked decrease in their incidence and an improvement in life expectancy was noted, starting from the late 1980s, with the advent of early reperfusion therapy [43].
Nowadays, arrhythmias and conduction disorders remain among the most common complications of ACS, particularly during STEMI [21]. In this study, 22.8% of the patients had arrhythmias. Other studies have reported an overall incidence of arrhythmias after STEMI as high as 78–83% [44,45,46,47]. This difference could be explained by certain characteristics of the patients under study, notably the LVEF, which was reduced in the aforementioned studies. In this study, the average LVEF was 50.61% ± 10.9%. Decrease in the ejection fraction is a well-known significant risk factor for the development of arrhythmias [48]. The duration of follow-up was longer in most aforementioned studies than our study, and the comorbidities and age of the patients enrolled in various studies could also explain the difference in the frequency of arrhythmia, as this frequency increases with the age of patients [49]. According to Gorenek’s report, ventricular arrhythmias and atrial fibrillation were the most common arrhythmias found in this study [50].
The frequency of ventricular arrhythmias found in this study (13.6%) is close to 11% found by Podolecki et al. [51] and the frequency of atrial fibrillation found in this study is similar to that found by other authors [52, 53].
The mechanisms involved in the occurrence of rhythm disorders during ACS include genetic predisposition, which would be an essential condition for early arrhythmogenesis [54], sympathetic nervous system stimulation [55, 56], hypoxia, possible electrolyte imbalances, and damaged myocardium that acts as a substrate for the incoming circuits, due to changes in refractory periods. Furthermore, transmural infarction can interrupt the afferent and efferent branches of the sympathetic nervous system that innervates the myocardium downstream of the infarction zone. This autonomous imbalance promotes arrhythmias and conduction disorders [50, 57].
This study identified diabetes mellitus, history of atrial fibrillation, stroke, and low HDL-C levels as the determinants of arrhythmias.
The finding of diabetes mellitus being a determinant of arrhythmia in STEMI is according to the results from the Thai ACS Registry [58]. A recent study by Karthikeyan has also found diabetes mellitus as a factor associated with STEMI and its complications [27]. Diabetes mellitus is a well-established risk factor for arrhythmias [59,60,61]. The pathophysiology of diabetes mellitus-related arrhythmias is not fully understood; however, it is related to not only structural, electrical, electromechanical, autonomic remodeling but also oxidative stress and inflammation [62,63,64].
A history of atrial fibrillation presupposes the existence of arrhythmogenic factors that are, as schematized by Philippe Coumel, electrophysiological substrate, trigger, and pejorative modulating factors [65]. In this field, which is already susceptible to arrhythmias, ACS can be formed as an arrhythmogenic substrate (the ischemic zone), as a modulating factor (by the discharge of catecholamines and by metabolic factors, such as ischemia and acidosis), and as a trigger factor (by accelerating the heart rate).
Arrhythmias, particularly atrial fibrillation, are well-known causes of stroke. The inverse is less well-known: indeed, damage to the central nervous system following a stroke often leads to a disturbance of the autonomic nervous system, which plays an important role in arrhythmogenesis [66]. Furthermore, neural necrosis activates a systemic inflammatory response, which also contributes to arrhythmogenesis [67].
Studies have found that dyslipidemia increases the risk of developing tachyarrhythmia in the acute phase of STEMI [68] and that patients with low HDL-C levels during hospitalization with ACS have an increased risk of developing cardiac rhythm disturbances, independent of other risk factors [69], suggesting a possible protective role of HDL-C against the onset of arrhythmias in the context of ACS. Indeed, HDL-C has been reported to have anti-inflammatory, antioxidant, and antithrombotic properties [70].
The rate of acute heart failure during STEMI reported in the literature ranges from 5% [53] to 20% [28] depending on the studies. The 13.1% frequency found in the current study falls within this range. Acute heart failure, as described by Killip and Kimball in 1967 [71], is one of the most frequent complications of STEMI. The occurrence of heart failure in the acute phase of ACS can be attributed to several intricate mechanisms, including microcirculatory dysfunction, myocardial hypoxia, myocytic necrosis, inflammation, hemorrhage, edema, decompensation of pre-existing heart failure, acute mitral regurgitation due to papillary muscle dysfunction, and remodeling [72]. It may also involve increased complement activation [73] and genetic factors [74].
The determinants of Killip ≥ 2 acute heart failure found in this study have also been found in other studies, as follows: older age [28], hypertension [75], and cigarette smoking [76].
Aging is a debilitating condition in which a conglomerate of cellular and molecular mechanisms underlies the effects of aging on cardiovascular function. The most important mechanisms are oxidative stress and low-grade chronic inflammation, superimposed on the limited capacity of cardiac regeneration; together, these processes promote the occurrence of heart failure in the dramatic context of ACS.
A recent study by Haig et al. has found that smoking independently predicted heart failure events after acute STEMI [76]. In a recent cohort of patients admitted for acute heart failure, most of whom had IHD, Dokoupil et al. have found that hypertension was the most common comorbidities [77]. Acar et al. have identified cigarette smoking as an independent predictor of deterioration in the LVEF in patients with STEMI [78]. Hypertension could increase the risk of acute heart failure probably by pre-existing hypertensive heart disease.
Study limitations
Our study must be interpreted in the context of its potential limitations, including the limitations inherent in the cross-sectional study design, excluding the assessment of cause-and-effect relationships, and potential selection bias due to recruitment in a single hospital, thus excluding all cases that did not come to the CICU-SFHC or did not seek care during the study. Finally, generalizing the results to different populations is impossible.
Conclusions
STEMI is a frequent condition at the SFHC and is often complicated by acute heart failure and arrhythmias. Patients aged ≥ 75 years, those with hypertension, those with diabetes mellitus, smokers, those with a history of atrial fibrillation or stroke, and those with low HDL-C levels require careful monitoring for early diagnosis and management of these complications.
Data Availability
Because the consent given by study participants did not include data sharing with third parties, anonymized data can be made available to investigators for analysis on reasonable request to the corresponding author.
Abbreviations
- ACS:
-
Acute coronary syndrome
- AF:
-
Atrial fibrillation
- AIVR:
-
Accelerated idioventricular rhythm
- aOR:
-
Adjusted odds ratio
- AV bloc:
-
Atrioventricular bloc
- CI:
-
Confidence interval
- CICU:
-
Cardiology Intensive Care Unit
- CKD:
-
Chronic kidney disease
- COVID-19:
-
Coronavirus disease 2019
- CRP:
-
C-reactive protein
- CVDs:
-
Cardiovascular diseases
- CVRFs:
-
Cardiovascular risk factors
- D:
-
Diagonal
- DBP:
-
Diastolic blood pressure
- ESC:
-
European Society of Cardiology
- GFR:
-
Glomerular filtration rate
- HbA1c:
-
Glycated haemoglobin
- HbA1c:
-
Glycated hemoglobin
- HDL-C:
-
High-density lipoprotein-cholesterol
- IHD:
-
Ischemic heart disease
- K+:
-
Potassium
- LADA:
-
Left anterior descending artery
- LCA:
-
Left coronary artery
- LDL-C:
-
Low-density lipoprotein cholesterol
- LVEF:
-
Left ventricular ejection fraction
- MI:
-
Myocardial infarction
- MONICA:
-
Monitoring of Trends and Determinants in Cardiovascular Disease
- Na+:
-
Sodium
- non-STEMI:
-
Non-ST-elevation myocardial infarction
- OM:
-
Obtuse marginal
- ORs:
-
Odds ratios
- PAOD:
-
Peripheral arterial occlusive disease
- PDA:
-
Posterior descending artery
- PLA:
-
Posterolateral artery
- RCA:
-
Right coronary artery
- SBP:
-
Systolic blood pressure
- RI:
-
Ramus intermedius
- SFHC:
-
Sud Francilien Hospital Center
- SpO2:
-
Oxygen saturation
- STEMI:
-
ST-elevation myocardial infarction
- TIA:
-
Transient ischemic attack
- VF:
-
Ventricular fibrillation
- VSD:
-
Ventricular septal defect
- uVT:
-
Unsustained ventricular tachycardia
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular Diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Barquera S, Pedroza-Tobias A, Medina C, Hernandez-Barrera L, Bibbins-Domingo K, Lozano R, et al. Global overview of the Epidemiology of Atherosclerotic Cardiovascular Disease. Arch Med Res. 2015;46(5):328–38.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics-2017 update: a Report from the American Heart Association. Circulation. 2017;135(10):e146–e603.
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25.
Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi S, AlKatheeri R, et al. Global epidemiology of Ischemic Heart Disease: results from the global burden of Disease Study. Cureus. 2020;12(7):e9349.
India State-Level Disease Burden Initiative CVDC. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the global burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1339–e51.
Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of Acute Coronary Syndromes: a review. JAMA. 2022;327(7):662–75.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. 2012;126(16):2020–35.
Ishihara M, Nakao K, Ozaki Y, Kimura K, Ako J, Noguchi T, et al. Long-term outcomes of Non-ST-Elevation myocardial infarction without creatine kinase Elevation- the J-MINUET study. Circ J. 2017;81(7):958–65.
Terkelsen CJ, Lassen JF, Norgaard BL, Gerdes JC, Jensen T, Gotzsche LB, et al. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005;26(1):18–26.
Puymirat E, Simon T, Cayla G, Cottin Y, Elbaz M, Coste P, et al. Acute myocardial infarction: changes in patient characteristics, management, and 6-Month Outcomes over a period of 20 years in the FAST-MI program (French Registry of Acute ST-Elevation or Non-ST-Elevation myocardial infarction) 1995 to 2015. Circulation. 2017;136(20):1908–19.
Rogers WJ, Frederick PD, Stoehr E, Canto JG, Ornato JP, Gibson CM, et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of myocardial infarction from 1990 to 2006. Am Heart J. 2008;156(6):1026–34.
Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27(7):789–95.
Vernon ST, Coffey S, D’Souza M, Chow CK, Kilian J, Hyun K, et al. ST-Segment-Elevation myocardial infarction (STEMI) patients without Standard Modifiable Cardiovascular risk factors-how common are they, and what are their outcomes? J Am Heart Assoc. 2019;8(21):e013296.
Bouisset F, Ruidavets JB, Dallongeville J, Moitry M, Montaye M, Biasch K et al. Comparison of short- and long-term prognosis between ST-Elevation and Non-ST-Elevation myocardial infarction. J Clin Med. 2021;10(2).
Gale CP, Allan V, Cattle BA, Hall AS, West RM, Timmis A, et al. Trends in hospital treatments, including revascularisation, following acute myocardial infarction, 2003–2010: a multilevel and relative survival analysis for the National Institute for Cardiovascular Outcomes Research (NICOR). Heart. 2014;100(7):582–9.
Jernberg T, Johanson P, Held C, Svennblad B, Lindback J, Wallentin L, et al. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA. 2011;305(16):1677–84.
Belle L, Cayla G, Cottin Y, Coste P, Khalife K, Labeque JN, et al. French Registry on Acute ST-elevation and non-ST-elevation myocardial infarction 2015 (FAST-MI 2015). Design and baseline data. Arch Cardiovasc Dis. 2017;110(6–7):366–78.
Menozzi A. An overview on STEMI. Minerva Cardioangiol. 2018;66(4):391.
Bueno H, Martin-Asenjo R. Acute heart failure after STEMI. Still a problem, still an opportunity for improving care quality. Int J Cardiol. 2017;248:274–5.
Jones DE, Braun M, Kassop D. Acute Coronary Syndrome: common complications and conditions that mimic ACS. FP Essent. 2020;490:29–34.
Frampton J, Ortengren AR, Zeitler EP. Arrhythmias after Acute myocardial infarction. Yale J Biol Med. 2023;96(1):83–94.
Figueras J, Alcalde O, Barrabes JA, Serra V, Alguersuari J, Cortadellas J, et al. Changes in hospital mortality rates in 425 patients with acute ST-elevation myocardial infarction and cardiac rupture over a 30-year period. Circulation. 2008;118(25):2783–9.
Tran HV, Ash AS, Gore JM, Darling CE, Kiefe CI, Goldberg RJ. Twenty-five year trends (1986–2011) in hospital incidence and case-fatality rates of ventricular tachycardia and ventricular fibrillation complicating acute myocardial infarction. Am Heart J. 2019;208:1–10.
Murray CSG, Zamora C, Shitole SG, Christa P, Lee UJ, Bortnick AE, et al. Race-ethnic differences of ST-Elevation myocardial infarction: findings from a New York Health System Registry. Ethn Dis. 2022;32(3):193–202.
Ya’qoub L, Lemor A, Dabbagh M, O’Neill W, Khandelwal A, Martinez SC, et al. Racial, ethnic, and sex disparities in patients with STEMI and cardiogenic shock. JACC Cardiovasc Interv. 2021;14(6):653–60.
Karthikeyan T, Raja M, Radha D, Gaur TA, Geetha J, Sakthivadivel V. Risk factors and inflammatory markers in acute coronary syndrome-ST elevation myocardial infarction (STEMI). Horm Mol Biol Clin Investig. 2023.
Vicent L, Velasquez-Rodriguez J, Valero-Masa MJ, Diez-Delhoyo F, Gonzalez-Saldivar H, Bruna V, et al. Predictors of high Killip class after ST segment elevation myocardial infarction in the era of primary reperfusion. Int J Cardiol. 2017;248:46–50.
Rossello X, Huo Y, Pocock S, Van de Werf F, Chin CT, Danchin N, et al. Global geographical variations in ST-segment elevation myocardial infarction management and post-discharge mortality. Int J Cardiol. 2017;245:27–34.
Machta S, Gauthier V, Ferrieres J, Montaye M, Huo Yung Kai S, Gbokou S, et al. Comparison of clinical profiles and care for patients with incident versus recurrent acute coronary syndromes in France: data from the MONICA registries. PLoS ONE. 2022;17(2):e0263589.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med. 2012;60(6):766–76.
Cravens MG, Ali SF, Gibbs MA, Littmann L. Real-time validation of the Sgarbossa and modified Sgarbossa criteria in intermittent left bundle branch block. J Electrocardiol. 2020;63:24–7.
Berberich AJ, Hegele RA. A Modern Approach to Dyslipidemia. Endocr Rev. 2022;43(4):611–53.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Ahmadi SA, Boroumand MA, Gohari-Moghaddam K, Tajik P, Dibaj SM. The impact of low serum triglyceride on LDL-cholesterol estimation. Arch Iran Med. 2008;11(3):318–21.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Julian DG, Valentine PA, Miller GG. Disturbances of rate, rhythm and conduction in Acute myocardial infarction: a prospective study of 100 consecutive unselected patients with the aid of Electrocardiographic Monitoring. Am J Med. 1964;37:915–27.
Jewitt DE, Balcon R, Raftery EB, Oram S. Incidence and management of supraventricular arrhythmias after acute myocardial infarction. Lancet. 1967;2(7519):734–8.
Stock E, Goble A, Sloman G. Assessment of arrhythmias in myocardial infarction. Br Med J. 1967;2(5554):719–23.
Dubois C, Smeets JP, Demoulin JC, Pierard L, Foidart G, Henrard L, et al. Incidence, clinical significance and prognosis of ventricular fibrillation in the early phase of myocardial infarction. Eur Heart J. 1986;7(11):945–51.
Adgey AA, Allen JD, Geddes JS, James RG, Webb SW, Zaidi SA, et al. Acute phase of myocardial infarction. Lancet. 1971;2(7723):501–4.
Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356(23):2388–98.
Patil PR, Khatana P, Patil DR. Incidence of cardiac arrhythmias in patients with acute myocardial infarction during the first 48 hours of the onset of chest pain. Int J Adv Med. 2017;4(4):1144–49.
Terkelsen CJ, Sørensen JT, Kaltoft AK, Nielsen SS, Thuesen L, Bøtker H-E, et al. Prevalence and significance of accelerated idioventricular rhythm in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol. 2009;104(12):1641–6.
Bloch Thomsen PE, Jons C, Raatikainen MP, Moerch Joergensen R, Hartikainen J, Virtanen V, et al. Long-term recording of cardiac arrhythmias with an implantable cardiac monitor in patients with reduced ejection fraction after acute myocardial infarction: the Cardiac Arrhythmias and Risk Stratification after Acute myocardial infarction (CARISMA) study. Circulation. 2010;122(13):1258–64.
Tatli E, Alicik G, Buturak A, Yilmaztepe M, Aktoz M. Arrhythmias following revascularization procedures in the course of acute myocardial infarction: are they indicators of reperfusion or ongoing ischemia? The Scientific World Journal. 2013;2013.
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346(12):877–83.
Zhao J, He F, Hu DY, Ding RJ, Yu XJ, Gou JJ, et al. [Types and risk factors of arrhythmia on young patients with acute coronary syndrome in Henan province]. Zhonghua xin xue guan bing za zhi. 2013;41(7):572–6.
Gorenek B, Lundqvist CB, Terradellas JB, Camm AJ, Hindricks G, Huber K, et al. Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. Eur Heart J Acute Cardiovasc Care. 2015;4(4):386.
Podolecki T, Lenarczyk R, Kowalczyk J, Jedrzejczyk-Patej E, Chodor P, Mazurek M, et al. Prognostic significance of Complex Ventricular Arrhythmias complicating ST-Segment Elevation myocardial infarction. Am J Cardiol. 2018;121(7):805–9.
Shah JA, Naz F, Kumar R, Hassan M, Shah G, Ahmed K, et al. Incidence of Cardiac Arrhythmias in Acute myocardial infarction patients undergoing primary percutaneous coronary intervention and Associated Outcomes during the first 24 hours. Cureus. 2021;13(1):e12599.
Petrosyan H, Hayrapetyan H, Torozyan S, Tsaturyan A, Tribunyan S. In-hospital complications in acute ST-elevation myocardial infarction depending on renal function. Herzschrittmacherther Elektrophysiol. 2021;32(3):359–64.
Bezzina CR, Pazoki R, Bardai A, Marsman RF, de Jong J, Blom MT, et al. Genome-wide association study identifies a susceptibility locus at 21q21 for ventricular fibrillation in acute myocardial infarction. Nat Genet. 2010;42(8):688–91.
de la Perez RA, Swieszkowski SP, Cintora FM, Aladio JM, Papini CM, Matsudo M, et al. Neuroendocrine System Regulatory Mechanisms: Acute Coronary syndrome and stress hyperglycaemia. Eur Cardiol. 2018;13(1):29–34.
Nito I, Waspadji S, Harun S, Markum HM. Correlation between cortisol levels and myocardial infarction mortality among intensive coronary care unit patients during first seven days in hospital. Acta Med Indones. 2004;36(1):8–14.
Pena Escobar JA, Aung M, Amin S, Gulraiz A, Gandhi FR, Malik BH. Pathogenesis of ventricular arrhythmias and its effect on long-term prognosis in patients with Takotsubo Cardiomyopathy. Cureus. 2020;12(10):e11171.
Boonsom W, Ratanasumawong K, Hutayanon P, Tungsabutra W. Implications of diabetes mellitus in patients with STEMI: data from Thai ACS Registry. J Med Assoc Thai. 2007;90(Suppl 1):12–20.
Junttila MJ, Kiviniemi AM, Lepojarvi ES, Tulppo M, Piira OP, Kentta T, et al. Type 2 diabetes and coronary artery disease: preserved ejection fraction and sudden cardiac death. Heart Rhythm. 2018;15(10):1450–6.
Yeung CY, Lam KS, Li SW, Lam KF, Tse HF, Siu CW. Sudden cardiac death after myocardial infarction in type 2 diabetic patients with no residual myocardial ischemia. Diabetes Care. 2012;35(12):2564–9.
Junttila MJ, Barthel P, Myerburg RJ, Makikallio TH, Bauer A, Ulm K, et al. Sudden cardiac death after myocardial infarction in patients with type 2 diabetes. Heart Rhythm. 2010;7(10):1396–403.
Guckel D, Sohns C, Sommer P. [Rhythm and metabolic control]. Herz. 2022;47(5):410–8.
Al Kury LT, Chacar S, Alefishat E, Khraibi AA, Nader M. Structural and electrical remodeling of the Sinoatrial Node in Diabetes: New Dimensions and Perspectives. Front Endocrinol (Lausanne). 2022;13:946313.
Karam BS, Chavez-Moreno A, Koh W, Akar JG, Akar FG. Oxidative stress and inflammation as central mediators of atrial fibrillation in obesity and diabetes. Cardiovasc Diabetol. 2017;16(1):120.
Coumel P, Leenhardt A. Mental activity, adrenergic modulation, and cardiac arrhythmias in patients with heart disease. Circulation. 1991;83(4 Suppl):II58–70.
Chen PS, Chen LS, Fishbein MC, Lin SF, Nattel S. Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ Res. 2014;114(9):1500–15.
Chung MK, Martin DO, Sprecher D, Wazni O, Kanderian A, Carnes CA, et al. C-reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation. 2001;104(24):2886–91.
Liu YB, Wu CC, Lee CM, Chen WJ, Wang TD, Chen PS, et al. Dyslipidemia is associated with ventricular tachyarrhythmia in patients with acute ST-segment elevation myocardial infarction. J Formos Med Assoc. 2006;105(1):17–24.
Boudi FB, Kalayeh N, Movahed MR. High-density lipoprotein cholesterol (HDL-C) levels independently correlates with Cardiac Arrhythmias and Atrial Fibrillation. J Intensive Care Med. 2020;35(5):438–44.
Karabacak M, Kahraman F, Sert M, Celik E, Adali MK, Varol E. Increased plasma monocyte chemoattractant protein-1 levels in patients with isolated low high-density lipoprotein cholesterol. Scand J Clin Lab Invest. 2015;75(4):327–32.
Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967;20(4):457–64.
Cahill TJ, Kharbanda RK. Heart failure after myocardial infarction in the era of primary percutaneous coronary intervention: mechanisms, incidence and identification of patients at risk. World J Cardiol. 2017;9(5):407–15.
Orrem HL, Nilsson PH, Pischke SE, Grindheim G, Garred P, Seljeflot I, et al. Acute heart failure following myocardial infarction: complement activation correlates with the severity of heart failure in patients developing cardiogenic shock. ESC Heart Fail. 2018;5(3):292–301.
Xu J, Yang Y. Integrated Gene expression profiling analysis reveals potential molecular mechanisms and candidate biomarkers for early risk stratification and prediction of STEMI and Post-STEMI Heart failure patients. Front Cardiovasc Med. 2021;8:736497.
Carrick D, Haig C, Maznyczka AM, Carberry J, Mangion K, Ahmed N, et al. Hypertension, Microvascular Pathology, and Prognosis after an Acute Myocardial Infarction. Hypertension. 2018;72(3):720–30.
Haig C, Carrick D, Carberry J, Mangion K, Maznyczka A, Wetherall K, et al. Current smoking and prognosis after Acute ST-Segment Elevation myocardial infarction: New Pathophysiological Insights. JACC Cardiovasc Imaging. 2019;12(6):993–1003.
Dokoupil J, Hrecko J, Cermakova E, Adamcova M, Pudil R. Characteristics and outcomes of patients admitted for acute heart failure in a single-centre study. ESC Heart Fail. 2022;9(4):2249–58.
Acar B, Ozeke O, Unal S, Karakurt M, Kara M, Kirbas O, et al. Change in left ventricular systolic function in patients with ST elevation myocardial infarction: evidence for smoker’s paradox or pseudo-paradox? Indian Heart J. 2016;68(6):816–20.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Design and concept of study: JMMM, BKP, and AK; Acquisition of data: JMMM and AK; Manuscript draft: JMMM, BKP, and AK; Analysis and interpretation of data: ANN, JMMM, BKP, PG, LM and AK; All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Declarations
Not applicable.
Ethics approval and consent to participate
This study was reviewed and approved by the Centre Hospitalier Sud Francilien Ethics Committee, and all the included patients signed written informed consent (to avoid introducing selection bias, waiver of written informed consent for deceased patients was approved by Centre Hospitalier Sud Francilien Ethics Committee. The rules of confidentiality and ethics have been respected according to the 1964 Declaration of Helsinki.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mavungu Mbuku, JM., Mukombola Kasongo, A., Goube, P. et al. Factors associated with complications in ST-elevation myocardial infarction: a single-center experience. BMC Cardiovasc Disord 23, 468 (2023). https://doi.org/10.1186/s12872-023-03498-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03498-z