Abstract
Background
The development of new-onset atrial fibrillation (NOAF) after acute myocardial infarction (AMI) is a clinical complication that requires a better understanding of the causative risk factors. This study aimed to explore the risk factors and the expression and function of miR-1 and miR-133a in new atrial fibrillation after AMI.
Methods
We collected clinical data from 172 patients with AMI treated with emergency percutaneous coronary intervention (PCI) between October 2021 and October 2022. Independent predictors of NOAF were determined using binary logistic univariate and multivariate regression analyses. The predictive value of NOAF was assessed using the area under the receiver operating characteristic (ROC) curve for related risk factors. In total, 172 venous blood samples were collected preoperatively and on the first day postoperatively; the expression levels of miR-1 and miR-133a were determined using the polymerase chain reaction. The clinical significance of miR-1 and miR-133a expression levels was determined by Spearman correlation analysis.
Results
The Glasgow prognostic score, left atrial diameter, and infarct area were significant independent risk factors for NOAF after AMI. We observed that the expression levels of miR-1 and miR-133a were significantly higher in the NOAF group than in the non-NOAF group. On postoperative day 1, strong associations were found between miR-133a expression levels and the neutrophil ratio and between miR-1 expression levels and an increased left atrial diameter.
Conclusions
Our findings indicate that the mechanism of NOAF after AMI may include an inflammatory response associated with an increased miR-1-related mechanism. Conversely, miR-133a could play a protective role in this clinical condition.
Similar content being viewed by others
Background
Acute myocardial infarction (AMI) is the acute necrosis of coronary artery stenosis caused by corresponding myocardial ischemia. New-onset atrial fibrillation (NOAF) is a critical complication with an incidence rate of 6–22% [1]. Patients with NOAF have a 40% higher mortality rate than those with normal sinus rhythm [2]. Long-term follow-up results of relevant studies have shown a lower incidence of ischemic cerebrovascular disease or transient ischemic attacks in patients with non-valvular atrial fibrillation (NVAF) in the rhythm control group [3]. The specific mechanism of atrial fibrillation has not been defined but involves electrical and structural remodelling of the atrium. Structural remodelling includes increased atrial fibrosis, increasing ectopic electrical activity and conduction anisotropy within the atrial tissue [4, 5]. In patients with a mild reduction in ejection fraction (HFmrEF), a left atrial volume index (LAVI) > 30.5 can predict the presence of atrial fibrillation with a sensitivity of 64% and specificity of 66% [6]. However, electrical remodelling mainly involves changes in the expression of cardiac ion channels, leading to the shortening of the atrial action potential duration and effective refractory period and changes in atrial calcium homeostasis [7,8,9,10]. Previous studies have indicated that fragmented QRS (fQRS) is an independent determinant of atrial fibrillation in patients with ST-segment elevation myocardial infarction (STEMI) [11]. The P-wave peak times in V1 and D2 leads, which are obtained from surface electrocardiography (ECG), are highly predictive in determining the likelihood of patients developing atrial high-rate episodes (AHRE) [12].
MiRNAs are small noncoding RNAs that regulate gene and protein expression by causing mRNA degradation or translational repression [13]. Among these miRNAs, miR-1 and miR-133a are specifically expressed in adult heart and skeletal muscle tissues, and their expression patterns vary depending on the pathological condition [14]. This study aimed to investigate the risk factors for NOAF after AMI, assess the expression levels of miR-1 and miR-133a before and after AMI, and examine their potential clinical significance as risk factors for NOAF.
Methods
Study participants and specimen collection
Between October 2021 and October 2022, 172 patients with AMI who underwent emergency percutaneous coronary intervention (PCI) at the Affiliated Hospital of Guizhou Medical University were consecutively selected as participants for this study. The patients’ medical records were used to collect clinical data during hospitalisation. This data included various categorical and continuous variables such as age, gender, and biochemical indicators. In addition, the Glasgow Prognostic Score (GPS) was calculated to assess the inflammatory status and predict the prognosis of the patients. The GPS is determined by measuring two acute-phase proteins in the blood: C-reactive protein (CRP) and albumin.
Furthermore, the results of coronary angiography were also recorded for analysis. In this study, 172 blood samples were collected from the participants before undergoing PCI and on the first day after the intervention. These samples were used to analyse plasma miR1 and miR133a expression levels. The Ethics Committee of the Affiliated Hospital of Guizhou Medical University approved the study protocol, and the study was conducted following the principles outlined in the Declaration of Helsinki. Informed consent was obtained from all patients before collecting the samples.
Inclusion and exclusion criteria
AMI diagnostic criteria refer to the Fourth Global Unified Definition of Myocardial Infarction, published in 2018 [15], where acute myocardial injury exists and at least one of the following conditions is present: (1) symptoms of a lack of blood perfusion in the myocardium or chest pain lasting for > 30 min; (2) newly developed ischemic electrocardiogram (ECG) changes; (3) the formation of a new pathological Q wave on ECG; (4) imaging evidence confirming the presence of newly inactivated myocardium or ventricular wall motion abnormalities; and (5) angiography confirming an intracoronary thrombosis or an autopsy. The ECG diagnostic criteria for atrial fibrillation were: disappearing P wave, replaced with fibrillation wave (f wave) of different sizes and shapes; frequency of the f wave of 350–600 times/min; and irregular R–R interval. NOAF was defined as no history of paroxysmal or persistent atrial fibrillation, atrial flutter, or the first episode of atrial fibrillation on admission or during hospitalisation. The duration of atrial fibrillation was assessed under any of the following conditions: (1) the duration of atrial fibrillation could be determined by a complete 12-lead ECG or recorded by a Holter monitor and (2) ECG monitoring of atrial fibrillation for at least 30 s [16, 17]. The following exclusion criteria were applied: (1) a history of heart disease; (2) known malignant tumours; (3) thyroid disease or severe liver and renal insufficiency; (4) recent surgery and trauma; (5) combined acute and chronic infections and recent cerebrovascular diseases; (6) autoimmune diseases or a history of skeletal muscle trauma and other diseases; (7) history of atrial flutter, myocardial infarction, myocarditis, or cardiomyopathy; (8) history of radiofrequency ablation for arrhythmia, coronary artery bypass grafting, or other cardiac surgeries; and (9) severe valvular lesions or congenital heart disease.
Sample collection
Venous blood samples (5 mL) were collected from patients with AMI before PCI and on the first day after PCI using EDTA-K2 anticoagulant tubes. All blood samples were centrifuged at 4 °C (13,400×g, 10 min), and the plasma was transferred to RNase/DNA microcentrifuge tubes and stored at -80℃.
Quantitative real-time polymerase chain reaction (qRT-PCR) of miR1 and miR133a
Total RNA was isolated using a total RNA extraction kit (Tiangen Biochemical Technology Company, Beijing, China), and miR1 and miR133a expression levels were quantified using the Bulge-Loop™ miRNA qRT-PCR starter kit (Ruibo Biotechnology, Guangzhou, China) with the following reverse transcription program: 42 °C for 60 min and inactivated reverse transcriptase at 70 °C for 10 min. After terminating the reaction, the resulting product was cooled on ice and stored at -80℃. The reverse transcription and PCR reaction system was configured as previously described, and PCR reactions were performed using a fluorescent PCR instrument (Bio-Rad Laboratories, Hercules, CA, USA). The PCR reaction conditions were as follows: pre-denaturation at 95 °C for 10 min, denaturation at 95℃ for 2 s, annealing at 60℃ for 30 s, and extension at 70℃ for 10 s for 40 cycles. The ΔCT value was calculated, using cel-miR-39 as the control gene, as the difference between the target gene and cel-miR-39, as follows: ΔΔCT = [(CTtarget−gene-CTcel−miR−39) Experimental group] – [(CTtarget gene-CTcel−miR−39) Control group]. Therefore, 2−ΔΔCT represented the relative miRNA expression of the experimental and control groups.
Statistical analysis
All data analysed in this study were processed using the SPSS software (version 22.0; IBM Corporation, Armonk, NY, USA). The distribution of continuous variables was evaluated using the Kolmogorov-Smirnov normality test. The results are presented as “mean ± standard deviation” for normally distributed data, and an independent sample t-test was used to compare the groups. Non-normally distributed data are presented as median (interquartile range), and nonparametric tests were used to analyse these data. For categorical variables, the chi-squared test was used. Logistic regression analysis was employed to determine the predictive power of clinical data for NOAF after AMI. The diagnostic efficacy of clinical indicators of NOAF after AMI was analysed using the receiver operating characteristic (ROC) curve and the area under the curve (AUC). Correlations among the variables in patients with NOAF were analysed using Spearman’s rank correlation. All statistical tests were two-tailed, and statistical significance was set at a P-value < 0.05.
Results
Basic data of the selected population
A total of 172 patients were included in this study, with 97 and 32 in the non-NOAF and NOAF groups, respectively. There were no significant differences between the groups regarding age, sex, hypertension, diabetes, total white blood cell count upon admission, neutrophil ratio, glomerular filtration rate (GFR), and levels of uric acid, brain natriuretic peptide (BNP), creatinine, Mg2+, and K+ (P > 0.05). The proportion of patients with a Glasgow Prognostic Score of 0 points was significantly higher than those with a score of 1 point (P < 0.01), and the incidence of Glasgow Prognostic Score elevation was higher in the NOAF group compared with the non-NOAF group (P < 0.05). The erythrocyte sedimentation rate was higher in the NOAF group than in the non-NOAF group (P < 0.05). Furthermore, the increase in left atrial diameter was significantly greater in the NOAF group compared with the non-NOAF group (P < 0.01; Table 1).
Coronary artery lesion data
The enrolled patients diagnosed with myocardial infarction based on ECG examination were divided into two groups: the anterior wall group (including anterior, extensive anterior, lateral, lower, and posterior walls) and the non-ST elevation myocardial infarction (NSTEMI) group. The non-NOAF group had more NSTEMI infarctions compared with the NOAF group. Further analysis showed no significant difference between the number of patients with anterior and lower wall infarctions and those with NSTEMI (P > 0.05). Among patients with NOAF and non-NOAF, the number of single-, double-, and triple-branched coronary lesions was also not significantly different. (P > 0.05; Table 2).
Multivariate correlation analysis
The inclusion of NOAF-related risk factors in the logistic regression model showed that the Glasgow prognostic score (odds ratio [OR], 2.375, 95% confidence interval [CI], 1.091–5.171), left atrial diameter (OR, 1.065; 95% CI, 1.011–1.122), and infarct size (OR, 0.778; 95% CI, 0.625–0.967) were independent risk factors for NOAF (Table 3).
ROC curve
The Glasgow prognostic score demonstrated an AUC of 0.62 in predicting NOAF. When using a cut-off value of 0.5 for the Glasgow prognostic score, the sensitivity and specificity for predicting NOAF were 50% and 74.3%, respectively. Regarding the left atrial diameter, the AUC was 0.66. When using a cut-off value of 35.5 mm for the internal diameter of the left atrium, the sensitivity and specificity for predicting NOAF were 62.5% and 70%, respectively (Fig. 1; Tables 4 and 5).
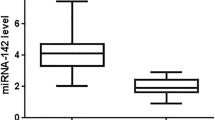
Quantitative plasma miR1 and miR133a expression
The plasma expression levels of miR1 and miR133a were determined using qRT-PCR. The normality of the miR1 and miR133a values was evaluated using the Shapiro-Wilk test. The nonparametric Mann-Whitney test was then used to compare the expression levels between the NOAF and non-NOAF groups. The Mann-Whitney test results indicated significantly higher expression levels of miR1 and miR133a in the NOAF group than in the non-NOAF group (P < 0.01; Table 6).
Correlation between the expression of miR1 and miR133a preoperatively and 1-day postoperatively and clinical indicators
The relationship between the expression of miR1 and miR133a and several clinical indicators was analysed using the Spearman statistical test. The left atrial diameter was moderately related to the preoperative expression of miR1 (r = 0.163); the miR133a expression on the first day after surgery was associated with the percentage of neutrophils (r = 0.205), which were significant overall (r = 0.264; Table 7).
Discussion
Inflammatory factors and NOAF
Inflammation is associated with structural and electrical remodelling in the atrium and the occurrence and persistence of atrial fibrillation (AF) [18, 19]. Infections, including their type, duration, and severity, may impact atrial remodelling [20]. Multicentre studies [21, 22] have found an increased proportion of AF in patients with sepsis, indicating that pro-inflammatory and inflammatory mediators of blood circulation are associated with AF development [23]. After acute myocardial infarction (AMI), the inflammatory response is vital in myocardial remodelling [23, 24]. The Glasgow Prognostic Score (GPS) assesses serum albumin and C-reactive protein levels [25]. A drop in serum albumin level indicates a severe inflammatory response in the patient [26]. Therefore, the GPS can accurately reflect the degree of the inflammatory response. In our study, after excluding severe infectious diseases, we found that new-onset AF (NOAF) was related to the GPS and increased blood sedimentation. This suggests that NOAF after AMI is associated with inflammatory mechanisms.
Infarct site and NOAF
Atrial ischemia or infarction can lead to electrical and structural remodelling of the atrium [27, 28]. Relevant studies suggest that ischemia can disrupt diastolic cytoplasmic Ca2 + flow. Notably, several factors, such as increased intracellular acidification and dephosphorylation of junction proteins, can result in local conduction blocks and facilitate the occurrence of atrial fibrillation [29, 30]. Furthermore, other studies indicate that proximal occlusion of the left spiral artery can cause reduced branch circulation in the atrioventricular node, contributing to the development of atrial fibrillation [31, 32]. In addition, a study found that coronary lesions originating from either the left or right coronary artery system could promote atrial fibrillation due to atrial ischemia [33]. In our study, patients with inferior and anterior wall infarctions were more likely to develop atrial fibrillation than those with non-ST-segment elevation myocardial infarction (NSTEMI). However, this association was not observed with diseased vessels, suggesting that the severity of ischemia is linked to new-onset atrial fibrillation (NOAF).
miR1, miR133a, and NOAF
Injured cardiomyocytes after AMI promote inflammatory responses by releasing miR-1 and increasing the number of monocytes in the blood [34]. The increase in miR-1 can regulate atrial specificity, improve heart conduction, repolarisation, and heart rate, and reduce atrial fibrillation through the double-pore domain potassium channel TASK-1. TASK-1 is a weak inwardly rectifying acid-sensitive K + channel encoded by KCNK3 [35,36,37]. Yang et al. [38] found that miR-1 overexpression can be inhibited by KCNJ2, which encodes the K + channel subunit Kir2.1, and GJA1, which encodes connexin-43. This inhibition slows the conduction and depolarisation of the cytoplasmic membrane and inhibits atrial fibrillation. In patients with persistent atrial fibrillation, miR-1 expression decreases, leading to increased inward rectifier current activity [39]. Yuan et al. [40] found that miR-1 levels were significantly lower in geriatric atrial fibrillation patients compared with non-atrial fibrillation patients. However, Terentyev et al. reported that increased miR-1 levels in cardiomyocytes lead to selectively decreased expression of the B56α regulatory subunit of protein phosphatase 2 A. This reduction causes reduced medium-mediated dephosphorylation of the L-type calcium channel (LTCC) and ryanodine receptor 2 (RyR2), resulting in increased calcium/calmodulin-dependent kinase II phosphorylation of LTCC and RyR2. Consequently, an inward endoplasmic reticulum Ca2 + current is induced, promoting arrhythmia development [41]. Wiedmann et al. [42] found that miR-1 was associated with the atrial collagen alpha-2(I) chain, and pro-apoptotic miR-1 was increased in the right atrial tissue of patients with NOAF after coronary atrial bypass graft compared with patients without atrial fibrillation. In this study, we observed that miR-1 was elevated in NOAF after AMI and was associated with increased atrial diameter, suggesting that increased miR-1 levels in patients were associated with myocardial structural remodelling, leading to atrial fibrillation. In addition, miR-133a levels were significantly higher before surgery and on the first day after surgery in the NOAF group compared with the non-NOAF group. Zhu et al. [43] discovered that miR-133a can activate macrophage migration inhibitory factors, resulting in increased Akt phosphorylation and Bcl-2 expression, and decreased caspase-3 expression, fibrosis, and apoptosis. Similarly, miR-133a can also promote the expression of vascular endothelial growth factor protein in human umbilical cord venous blood to reduce the occurrence of atrial fibrillation. Related studies suggested that miRNA-133a may be involved in downregulating CD47 in human HeLa cancer cells [44]. CD47 can inhibit the migration and adhesion of neutrophils [45]. Through a 1-year follow-up, research has shown that activating the miR-33/SIRT1 pathway increases inflammation and coagulation processes, thrombus burden, and the formation of distant embolisms [46]. In our analysis, elevated miR-133a levels were positively associated with the neutrophil percentage, inhibiting the inflammatory response. miR-133a reduced the occurrence of NOAF by stabilising myocardial structural remodelling and inhibiting the inflammatory response.
Overall, the Glasgow Prognostic Score and left atrial diameter were independent risk factors for NOAF after AMI. The mechanism associated with this condition may involve elevated miR-1 levels and an enlarged left atrial diameter. Conversely, miR-133a is protective in inhibiting the inflammatory response in cardiomyocytes. Administering non-vitamin K antagonist oral anticoagulants (NOACs) for anticoagulation therapy in patients with atrial fibrillation is recommended. In the AFTER-2 study conducted in Turkey, patients with high time in therapeutic range (TTR) on warfarin treatment showed no significant difference in the incidence of ischemic cerebrovascular disease/transient ischemic attacks (CVD/TIA), intracranial haemorrhage, and mortality as primary outcomes [47, 48]. Increasing the frequency of follow-up visits and minimising adverse events is recommended for patients with new-onset atrial fibrillation after acute myocardial infarction.
This was a single-centre retrospective study with a small sample size. Multicentre studies with large sample sizes are required to validate our findings. In addition, due to the short duration or delayed observation of atrial fibrillation, the results of previously asymptomatic patients with atrial fibrillation, and the influence of potential immune-related diseases on miRNA expression, could not be excluded entirely. Finally, the lack of further analysis of the onset of NOAF and miRNA changes in patients with AMI may have been a limitation of this study.
Conclusions
In this study, we identified a mechanism associated with NOAF after AMI that involves an inflammatory response and changes in miRNA expression. Specifically, we observed a detrimental role of miR-1 associated with an increased left atrial diameter. Conversely, miR-133a may play a protective role in NOAF by increasing the neutrophil ratio, thereby reducing the inflammatory response. These findings provide novel insights into the mechanism of NOAF after AMI, which could contribute to developing innovative therapeutic strategies for this condition.
Data Availability
The datasets and materials used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AMI:
-
Acute myocardial infarction
- AUC:
-
Area under the curve
- BNP:
-
Brain natriuretic peptide
- CI:
-
Confidence interval
- ECG:
-
Electrocardiogram
- GFR:
-
Glomerular filtration rate
- LTCC:
-
L-type calcium channel
- NOAF:
-
New-onset atrial fibrillation
- NSTEMI:
-
Non-ST elevation myocardial infarction
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- qRT-PCR:
-
Quantitative real-time polymerase chain reaction
- ROC:
-
Receiver operating characteristic
- RyR2:
-
Ryanodine receptor 2
References
Zarich SW, Nesto RW. Implications and treatment of acute hyperglycemia in the setting of acute myocardial infarction. Circulation. 2007;115:e436–9. https://doi.org/10.1161/CIRCULATIONAHA.105.535732.
Jabre P, Jouven X, Adnet F, Thabut G, Bielinski SJ, Weston SA, et al. Atrial fibrillation and death after myocardial infarction: a community study. Circulation. 2011;123:2094–100. https://doi.org/10.1161/CIRCULATIONAHA.110.990192.
Kiliç R, Güzel T, Aktan A, Demir M, Arslan B, Ertaş F. The effect of treatment strategy on long-term follow-up results in patients with nonvalvular atrial fibrillation in Turkey: AFTER-2 subgroup analysis. Aging Clin Exp Res. 2023;35:1695–704. https://doi.org/10.1007/s40520-023-02467-y.
Wang SS, Wu LJ, Li JJ, Xiao HB, He Y, Yan YX. A meta-analysis of dysregulated miRNAs in coronary heart disease. Life Sci. 2018;215:170–81. https://doi.org/10.1016/j.lfs.2018.11.016.
Frustaci A, Chimenti C, Bellocci F, Morgante E, Russo MA, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997;96:1180–4. https://doi.org/10.1161/01.cir.96.4.1180.
Güzel T, Kış M, Şenöz O. The correlation between the left atrial volume index and atrial fibrillation development in heart failure with mildly reduced ejection fraction and long-term follow-up results. Acta Cardiol. 2022;77:647–54. https://doi.org/10.1080/00015385.2022.2067674.
Xu J, Cui G, Esmailian F, Plunkett M, Marelli D, Ardehali A, et al. Atrial extracellular matrix remodeling and the maintenance of atrial fibrillation. Circulation. 2004;109:363–8. https://doi.org/10.1161/01.CIR.0000109495.02213.52.
Dobrev D, Friedrich A, Voigt N, Jost N, Wettwer E, Christ T, et al. The G protein-gated potassium current I(K,ACh) is constitutively active in patients with chronic atrial fibrillation. Circulation. 2005;112:3697–706. https://doi.org/10.1161/CIRCULATIONAHA.105.575332.
Voigt N, Heijman J, Wang Q, Chiang DY, Li N, Karck M, et al. Cellular and molecular mechanisms of atrial arrhythmogenesis in patients with paroxysmal atrial fibrillation. Circulation. 2014;129:145–56. https://doi.org/10.1161/CIRCULATIONAHA.113.006641.
Voigt N, Li N, Wang Q, Wang W, Trafford AW, Abu-Taha I, et al. Enhanced sarcoplasmic reticulum Ca2+ leak and increased Na+-Ca2+ exchanger function underlie delayed afterdepolarizations in patients with chronic atrial fibrillation. Circulation. 2012;125:2059–70. https://doi.org/10.1161/CIRCULATIONAHA.111.067306.
Yesin M, Kalçık M, Çağdaş M, Karabağ Y, Rencüzoğulları İ, Gürsoy MO, et al. Fragmented QRS may predict new onset atrial fibrillation in patients with ST-segment elevation myocardial infarction. J Electrocardiol. 2018;51:27–32. https://doi.org/10.1016/j.jelectrocard.2017.08.014.
Karakayali M, Artac I, Omar T, Rencuzogullari I, Karabag Y, Hamideyin S. Assessment of the efficacy of the electrocardiographic P-wave peak time in predicting atrial high rate episode in patients with cardiac implantable electronic devices. J Electrocardiol. 2023;80:40–4. https://doi.org/10.1016/j.jelectrocard.2023.05.001.
Lamichhane TN, Sokic S, Schardt S, Raiker RS, Lin JW, Jay SM. Emerging roles for extracellular vesicles in tissue engineering and regenerative medicine. Tissue Eng Part B Rev. 2015;21:45–54. https://doi.org/10.1089/ten.TEB.2014.0300.
Lee S, Choi E, Cha MJ, Hwang KC. Looking into a conceptual framework of ROS-miRNA-atrial fibrillation. Int J Mol Sci. 2014;15:21754–76. https://doi.org/10.3390/ijms151221754.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138:e618–51. https://doi.org/10.1161/CIR.0000000000000617.
Pizzetti F, Turazza FM, Franzosi MG, Barlera S, Ledda A, Maggioni AP, et al. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI-3 data. Heart. 2001;86:527–32. https://doi.org/10.1136/heart.86.5.527.
Vora AN, Wang TY, Li S, Chiswell K, Hess C, Lopes RD, et al. Selection of stent type in patients with atrial fibrillation presenting with acute myocardial infarction: an analysis from the ACTION (Acute Coronary treatment and intervention outcomes Network) registry-get with the guidelines. J Am Heart Assoc. 2017;6:e005280. https://doi.org/10.1161/JAHA.116.005280.
Nattel S, Harada M. Atrial remodeling and atrial fibrillation: recent advances and translational perspectives. J Am Coll Cardiol. 2014;63:2335–45. https://doi.org/10.1016/j.jacc.2014.02.555.
Korantzopoulos P, Letsas KP, Tse G, Fragakis N, Goudis CA, Liu T. Inflammation and atrial fibrillation: a comprehensive review. J Arrhythm. 2018;34:394–401. https://doi.org/10.1002/joa3.12077.
Bozza FA, Salluh JI, Japiassu AM, Soares M, Assis EF, Gomes RN, et al. Cytokine profiles as markers of disease severity in sepsis: a multiplex analysis. Crit Care. 2007;11:R49. https://doi.org/10.1186/cc5783.
Desai R, Hanna B, Singh S, Omar A, Deshmukh A, Kumar G, et al. Trends and outcomes in sepsis hospitalizations with and without atrial fibrillation: a nationwide inpatient analysis. Crit Care Med. 2019;47:e630–8. https://doi.org/10.1097/CCM.0000000000003806.
Walkey AJ, Hammill BG, Curtis LH, Benjamin EJ. Long-term outcomes following development of new-onset atrial fibrillation during sepsis. Chest. 2014;146:1187–95. https://doi.org/10.1378/chest.14-0003.
Frangogiannis NG. The inflammatory response in myocardial injury, repair, and remodelling. Nat Rev Cardiol. 2014;11:255–65. https://doi.org/10.1038/nrcardio.2014.28.
Seropian IM, Toldo S, Van Tassell BW, Abbate A. Anti-inflammatory strategies for ventricular remodeling following ST-segment elevation acute myocardial infarction. J Am Coll Cardiol. 2014;63:1593–603. https://doi.org/10.1016/j.jacc.2014.01.014.
Kikuchi R, Takoi H, Tsuji T, Nagatomo Y, Tanaka A, Kinoshita H, et al. Glasgow prognostic score for prediction of chemotherapy-triggered acute exacerbation interstitial lung disease in patients with small cell lung cancer. Thorac Cancer. 2021;12:1681–9. https://doi.org/10.1111/1759-7714.13900.
Edgar JD, Gabriel V, Gallimore JR, McMillan SA, Grant J. A prospective study of the sensitivity, specificity and diagnostic performance of soluble intercellular adhesion molecule 1, highly sensitive C-reactive protein, soluble E-selectin and serum amyloid A in the diagnosis of neonatal infection. BMC Pediatr. 2010;10:22. https://doi.org/10.1186/1471-2431-10-22.
Jayachandran JV, Zipes DP, Weksler J, Olgin JE. Role of the na(+)/H(+) exchanger in short-term atrial electrophysiological remodeling. Circulation. 2000;101:1861–6. https://doi.org/10.1161/01.cir.101.15.1861.
Sinno H, Derakhchan K, Libersan D, Merhi Y, Leung TK, Nattel S. Atrial ischemia promotes atrial fibrillation in dogs. Circulation. 2003;107:1930–6. https://doi.org/10.1161/01.CIR.0000058743.15215.03.
De Mello WC. Effect of intracellular injection of calcium and strontium on cell communication in heart. J Physiol. 1975;250:231–45. https://doi.org/10.1113/jphysiol.1975.sp011051.
Dekker LR, Fiolet JW, VanBavel E, Coronel R, Opthof T, Spaan JA, et al. Intracellular Ca2+, intercellular electrical coupling, and mechanical activity in ischemic rabbit papillary muscle. Effects of preconditioning and metabolic blockade. Circ Res. 1996;79:237–46. https://doi.org/10.1161/01.res.79.2.237.
James TN. Myocardial infarction and atrial arrhythmias. Circulation. 1961;24:761–76. https://doi.org/10.1161/01.cir.24.4.761.
Kyriakidis M, Barbetseas J, Antonopoulos A, Skouros C, Tentolouris C, Toutouzas P. Early atrial arrhythmias in acute myocardial infarction. Role of the sinus node artery. Chest. 1992;101:944–7. https://doi.org/10.1378/chest.101.4.944.
Motloch LJ, Reda S, Larbig R, Wolff A, Motloch KA, Wernly B, et al. Characteristics of coronary artery disease among patients with atrial fibrillation compared to patients with sinus rhythm. Hellenic J Cardiol. 2017;58:204–12. https://doi.org/10.1016/j.hjc.2017.03.001.
Saha P, Sharma S, Korutla L, Datla RS, Shoja-Taheri F, Mishra R, et al. Circulating exosomes derived from transplanted progenitor cells aid the functional recovery of ischemic myocardium. Sci Transl Med. 2019;11:eaau1168. https://doi.org/10.1126/scitranslmed.aau1168.
Decher N, Wemhöner K, Rinné S, Netter MF, Zuzarte M, Aller MI, et al. Knock-out of the potassium channel TASK-1 leads to a prolonged QT interval and a disturbed QRS complex. Cell Physiol Biochem. 2011;28:77–86. https://doi.org/10.1159/000331715.
Donner BC, Schullenberg M, Geduldig N, Hüning A, Mersmann J, Zacharowski K, et al. Functional role of TASK-1 in the heart: studies in TASK-1-deficient mice show prolonged cardiac repolarization and reduced heart rate variability. Basic Res Cardiol. 2010;106:75–87. https://doi.org/10.1007/s00395-010-0128-x.
Skarsfeldt MA, Jepps TA, Bomholtz SH, Abildgaard L, Sørensen US, Gregers E, et al. pH-dependent inhibition of K2P3.1 prolongs atrial refractoriness in whole hearts. Pflugers Arch. 2016;468:643–54. https://doi.org/10.1007/s00424-015-1779-0.
Yang B, Lin H, Xiao J, Lu Y, Luo X, Li B, et al. The muscle-specific microRNA miR-1 regulates cardiac arrhythmogenic potential by targeting GJA1 and KCNJ2. Nat Med. 2007;13:486–91. https://doi.org/10.1038/nm1569.
Girmatsion Z, Biliczki P, Bonauer A, Wimmer-Greinecker G, Scherer M, Moritz A, et al. Changes in microRNA-1 expression and IK1 up-regulation in human atrial fibrillation. Heart Rhythm. 2009;6:1802–9. https://doi.org/10.1016/j.hrthm.2009.08.035.
Yuan K, Zhao P, Wang L. Molecular mechanism of atrial remodeling in patients with aging atrial fibrillation under the expression of microRNA-1 and microRNA-21. Bioengineered. 2021;12:17205–916. https://doi.org/10.1080/21655979.2021.2008668.
Terentyev D, Belevych AE, Terentyeva R, Martin MM, Malana GE, Kuhn DE, et al. miR-1 overexpression enhances ca(2+) release and promotes cardiac arrhythmogenesis by targeting PP2A regulatory subunit B56alpha and causing CaMKII-dependent hyperphosphorylation of RyR2. Circ Res. 2009;104:514–21. https://doi.org/10.1161/CIRCRESAHA.108.181651.
Wiedmann F, Kraft M, Kallenberger S, Büscher A, Paasche A, Blochberger PL, et al. MicroRNAs regulate TASK-1 and are linked to myocardial dilatation in atrial fibrillation. J Am Heart Assoc. 2022;11:e023472. https://doi.org/10.1161/JAHA.121.023472.
Zhu W, Sun L, Zhao P, Liu Y, Zhang J, Zhang Y, et al. Macrophage migration inhibitory factor facilitates the therapeutic efficacy of mesenchymal stem cells derived exosomes in acute myocardial infarction through upregulating miR-133a-3p. J Nanobiotechnol. 2021;19:61. https://doi.org/10.1186/s17251-021-00808-5.
Huang X, Neckenig M, Sun J, Jia D, Dou Y, Ai D, et al. Vitamin E succinate exerts anti-tumour effects on human cervical cancer cells via the CD47-SIRPa pathway both in vivo and in vitro. J Cancer. 2021;12:3877–86. https://doi.org/10.7150/jca.52315.
Liu Y, O’Connor MB, Mandell KJ, Zen K, Ullrich A, Bühring HJ, et al. Peptide-mediated inhibition of neutrophil transmigration by blocking CD47 interactions with signal regulatory protein alpha. J Immunol. 2004;172:2578–85. https://doi.org/10.4049/jimmunol.172.4.2578.
D’Onofrio N, Sardu C, Paolisso P, Minicucci F, Gragnano F, Ferraraccio F, et al. MicroRNA-33 and SIRT1 influence the coronary thrombus burden in hyperglycemic STEMI patients. J Cell Physiol. 2020;235:1438–52. https://doi.org/10.1002/jcp.29064.
Aktan A, Güzel T, Aslan B, Kılıç R, Günlü S, Özbek M, et al. Comparison of the real-life clinical outcomes of warfarin with effective time in therapeutic range and non-vitamin K antagonist oral anticoagulants: insight from the AFTER-2 trial. Kardiol Pol. 2023;81:132–40. https://doi.org/10.33963/KP.a2022.0287.
Güzel T, Aktan A, Kılıç R, Arslan B, Arık B, Yentür M, et al. Oral anticoagulant Use and Long-Term Follow-Up results in patients with non-valvular atrial fibrillation in Turkey AFTER-2 study. Anatol J Cardiol. 2022;26:567–76. https://doi.org/10.5152/AnatolJCardiol.2022.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81960047, 82160086), China Postdoctoral Science Foundation (2022MD723769),the Science and Technology Fund of Guizhou Provincial Health Department (No.qiankehepingtairencai-GCC[2022]040-1,qiankehezhicheng[2019]2800,qiankehejichu-ZK[2022]zhongdian043,qiankehechengguo-LC[2022]013), the Health and Family Planning Commission of Guizhou Province (qianweijianhan[2021]160), Provincial Key Medical Subject Construction Project of Health Commission of Guizhou Province, and the National Key Medical Subject Construction Project of National Health Commission of China.
Author information
Authors and Affiliations
Contributions
QYZ wrote the main manuscript text and completed the experiment; WL, ZHL, and HYZ guided the experiment and reviewed and revised the manuscript; ZGD and XLX guided the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of the Affiliated Hospital of Guizhou Medical University, approval number [2021010 K]. The study was conducted in accordance with the principles outlined in the Declaration of Helsinki.All patients provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zeng, Q., Li, W., Luo, Z. et al. The role of miR1 and miR133a in new-onset atrial fibrillation after acute myocardial infarction. BMC Cardiovasc Disord 23, 448 (2023). https://doi.org/10.1186/s12872-023-03462-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03462-x