Abstract
Background
Arterial stiffness has been shown to be an independent risk factor for adverse events and all-cause mortality in patients. Although PWV is the gold standard for pulse wave velocity, its application in clinical practice is limited by the high cost and complexity. ePwv is a new, simple, non-invasive indicator of arterial stiffness. The aim of this study was to assess the relationship between ePwv and all-cause mortality in patients with coronary artery disease.
Methods
This is a cohort study, selected from NHANES 2005 to 2008, 402 patients with coronary artery disease were included. The ePWV was divided into two groups and KM survival curves were used to calculate cumulative mortality in patients with coronary artery disease. Restricted cubic spline were used to represent the relationship between ePWV and all-cause mortality in patients with coronary artery disease. Cox regression was used to diagnose the relationship between ePwv and all-cause mortality.
Results
The mean age of the study subjects was 68.5 ± 11.8 years, of which 282 (70.1%) were men and 120 (29.9%) were women. During 180 months of follow-up, 160 all-cause mortality occurred. KM survival curves indicated that all-cause mortality increased with increasing ePWV. The relationship between ePWV and all-cause mortality in patients with coronary artery disease was verified by cox models. Patients in higher ePWV tertile tended to have higher all-cause mortality. After complete multivariate adjustment, an increase in ePWV was positively associated with all-cause mortality (HR = 1.180, 95% confidence interval (CI): 1.056–1.320). The multivariate-adjusted HR and 95% CI for the highest ePWV tertile was 1.582 (95% CI: 0.968–2.587) compared to the lowest tertile. In addition, the association between ePWV and mortality was visualized employing restricted spline curves, in which we found curves indicating a possible threshold for the effect of ePWV on all-cause mortality, with HR less than 1 when ePWV was less than 11.15 m/s; thereafter, there was a tendency for HR to increase with enhanced ePWV. Subgroup analysis showed that the correlation between ePWV and mortality persisted in population subgroups.
Conclusion
Our findings suggest that higher ePWV is associated with increased all-cause mortality in patients with coronary artery disease, particularly when ePWV exceeds 11.15 m/s.
Similar content being viewed by others
Introduction
Cardiovascular disease, as one of the main causes of mortality in the world today, affects millions of people every year. The most notable of these is coronary artery disease. This is a heart disease caused by atherosclerotic lesions of the coronary artery, ultimately resulting in myocardial ischemia, hypoxia, or necrosis due to stenosis or obstruction of the vascular cavity. Coronary artery disease is a leading cause of morbidity and mortality worldwide and is considered to be a chronic immune-inflammatory and fibroproliferative disorder caused by lipids[1,2,3,4,5,6,7,8,9].
Studies have shown that arterial stiffness increases in patients with coronary artery disease and that early changes in arterial stiffness are very important for the long-term prognosis of patients with coronary artery disease [10,11,12,13]. Although pulse wave velocity (PWV) can be the gold standard for arteriosclerosis, it is both a traditional risk factor and an independent risk factor for adverse cardiovascular events and all-cause mortality [14,15,16,17,18]. However, due to the high cost and complexity in testing, PWV has not been widely used in clinical practice [19, 20].
Estimated pulse wave velocity (ePWV), a new index of response arterial arteriosclerosis, is in good agreement with PWV. However, studies on the relationship between ePWV and all-cause mortality in patients with known coronary artery disease are still limited. And they use mostly linear models while the use of nonlinear models is still limited. Restricted cubic spline can better fit the nonlinear relationship and identify important key points. This exploration of critical points is important for early intervention in patients with coronary artery disease. Therefore, we selected 402 patients with coronary artery disease from NHANES and explored the relationship between ePWV and all-cause mortality in patients with coronary artery disease by calculating ePWV data and survival status at follow-up to 2019, to guide early intervention in patients with coronary artery disease.
Methods
Study population
In this study, we analyzed the data from NHANES (n = 20,497) from 2005 to 2008. NHANES estimates the prevalence of major diseases and identifies hazards for the disease by using a complex multi-stage probability sampling design. It aims to gather information about the health and nutrition of the US household population to achieve the goals of disease prevention and health promotion. the official website of NHANES provides data on the design of the study, interview epidemiology, dietary assessment, physical examination, and laboratory tests. The present study sample was limited to patients with coronary artery disease, excluding those without calculating ePWV or with an uncertain presence of coronary artery disease. coronary artery disease diagnosis: doctor or other health experts told you that you have coronary artery disease. There were 453 patients with coronary artery disease, 51 patients with ePWV who could not be calculated. This study includes factors such as gender, age, hypertension, diabetes, Stroke, smoking, drinking, PIR, education level, marital status, BMI, HbA1c, lipids, creatinine, eGFR, ALT, and AST. Ethical consent could be obtained from the CDC, and informed consent has been obtained from all participants. See Fig. 1.
Calculation of ePWV
The ePWV was calculated from age and MBP using the formula obtained from the collaborative reference value of arterial stiffness described by Greve et al. in their study[21, 22]. ePWV = 9.587–0.402age + 4.5610^(-3)age^2–2.62110^(-5)age^2MAP + 3.17610^(-3)ageMAP − 1.83210^(-2)*MAP. Mean BP was calculated as diastolic BP (DBP) + 0.4(SBP − DBP).
Covariates
After evaluating the relationship between ePWV and the survival status of patients with coronary artery disease, indicators associated with survival status were selected and controlled. The following covariates were collected and considered: age, sex, body mass index, education level, PIR, marital status, HbA1c, smoking, drinking, hypertension, diabetes mellitus, stroke, ALT ,AST ,HDL ,LDL, TC, triglycerides, eGFR,, creatinine. The BMI was calculated by dividing the body weight by the square of the height. Diabetes diagnosed with an FPG equal to or greater than 7 mmol/L or self-reported current use of anti-diabetic drugs. Hypertension was defined based on prior diagnosis, current use of antihypertensive medication, or SBP/DBP 140/90 mmHg. PIR was defined as the family income to poverty line ratio after adjusting for inflation and family size. The selection of covariates was based on previously published studies and available variables.
Statistical analysis
Categorical variables are reported as frequency and percentage, whereas numerical variables with normally distributed distributions are given as mean ± standard deviation. We used chi-square tests, analysis of variance, or Kruskal-Wallis tests depending on the kind of data to identify variations between individuals in various ePWV tertile. To avoid multicollinearity among independent variables, we considered Variance Inflation Factor (VIF) > 10 as a sign of severe collinearity and excluded the TC indicator. See supplement 1.
For the purpose of analyzing the relationship between ePWV and all-cause mortality, we built three COX regression models. To investigate the relationship between ePWV and all-cause mortality, we constructed three Cox regression models. Prior to conducting the statistical analysis, we performed a proportional hazards (PH) test to assess the validity of the proportional hazards assumption for the Cox regression model. (Supplement 2) It is an untuned model, Model 1. In model 2, marital status and gender were adjusted. Gender, BMI, Education, marital status, smoking, drinking, Hypertension, diabetes mellitus, stroke, ALT, AST, HbA1C, creatinine, eGFR, HDL, triglycerides, and LDL are all taken into account in Model 3. In order to evaluate any potential nonlinear link between ePWV and mortality, restricted cubic splines (RCS) were applied.
In addition, we used the maxstat package in R to determine the optimal grouping for ePWV. The maxstat package is a maximum statistic method based on quantiles, which automatically determines the best grouping scheme based on the distribution of the data and the optimal quantile in the population. We used this method to group the ePWV variable and used it for subsequent statistical analysis. Supplement 3.
In order to examine the relationship between survival time and survival probability at various ePWV values, we also conducted a Kaplan-Meier survival analysis. The effects of sex, age, hypertension, diabetes, smoking, stroke, PIR, and eGFR on the link between ePWV and mortality were examined using stratified analyses. Statistical significance was defined as a p-value 0.05. R program (version 4.1, Vienna, Austria) and IBM SPSS statistics version 23.0 are required for all statistical studies (Chicago, IL, USA).
Results
Characteristics of the study population
Table 1 presents the baseline characteristics of the included participants. Almost all characteristics were significantly different across ePWV tertiles except for gender, PIR, education, BMI, DM, HbA1c, AST, and HDL. Participants with higher ePWV (T3) were more likely to be older adults, cigarette smokers, drinkers, and single individuals compared to those with lower ePWV (T1, T2). Additionally, patients with a history of hypertension and stroke were more prevalent among those with higher ePWV. These participants had higher creatinine and LDL levels but lower ALT, eGFR, and triglyceride levels. Furthermore, we observed that participants with higher ePWV tertiles tended to have a higher mortality rate (tiles 1:33.2%, 2:43.7%, 3:67.9%, p < 0.001). The distribution of ePWV in the general population is shown in Fig. 2A, and the stratification of ePWV according to survival status is shown in Fig. 2B. As we can see, the majority of the deceased patients had higher ePWV.
Association between ePWV and death
The results of the univariate and multivariate COX regression analysis are presented in Table 2. The results of the Bonferroni correction can be seen in the supplementary material(Supplement 4). When ePWV was considered as a continuous variable, the unadjusted COX regression model showed that an increase in ePWV seemed to lead to a higher risk of mortality, but this association was not significant (hazard ratio (HR) = 1.045, 95% confidence interval (CI): 0.968–1.128). The association in Model 2 and Model 3 has statistical significance. Participants in the second and third tertiles had a higher risk of mortality in all three models when ePWV was used as a tertile-based categorical variable, with the first tertile serving as a reference. In particular, the risk of mortality was significantly higher in patients in the third tertile.
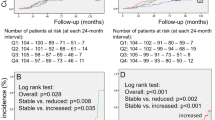
This study used a restricted cubic spline plot and found a non-linear relationship between estimated pulse wave velocity (ePWV) and mortality (Fig. 3). Additionally, we calculated the inflection point to be 11.15 m/s using the maxstat package and ROC curve( see supplement 3). On the curve, we found that the hazard ratio (HR) was less than 1 when ePWV was relatively low (less than 11.15 m/s ). However, the HR tended to increase with an increase in ePWV. We also used Kaplan-Meier survival analysis to evaluate the correlation between survival time and survival probability at different ePWV levels. As shown in Fig. 4, higher ePWV was associated with a higher mortality rate compared to lower ePWV (Log-rank, p<0.01).
Data are presented as odds ratios, 95% CIs (confidence intervals), and p-value. Model 1 adjusted for none. Model 2 adjusted for Sex、Marital status, smoking and drinking. Model 3 adjusted for all covariates expect for age. ePWV, estimated Pulse Wave Velocity.
Stratification analysis
We conducted subgroup analyses based on characteristics such as sex, age, hypertension, diabetes, smoking, stroke, PIR, and eGFR. In these analyses, ePWV was treated as a continuous variable. We found a statistically significant positive correlation between ePWV and mortality in individuals over 70 (HR = 1.270, 95% CI: 1.133–1.424) and in those without hypertension (HR = 1.324, 95% CI: 1.138–1.541), as illustrated in the forest plot (See Fig. 5).
Discussion
Our study has found a positive association between ePWV and all-cause mortality, which is consistent with previous reports [23,24,25,26,27]. By conducting a sensitivity analysis grouping ePWV into three levels, we found that as ePWV increased, the all-cause mortality predominance ratio showed a statistically significant positive association with p for trend < 0.05. Moreover, restricted cubic splines have visualized the relationship between ePWV and all-cause mortality. Interestingly, we discovered that the risk of mortality did not increase in the curve until ePWV reached about 11.15 m /s. This finding suggests that there might be a threshold for the effect of ePWV patterns on all-cause mortality. The risk of mortality is relatively low when ePWV is less than 11.15 m/s. However, when patients had higher ePWV levels, the risk of all-cause mortality increased significantly. Therefore, we need to pay more attention to patients with coronary artery disease with an ePWV of more than 11.15 m/s to reduce the burden of all-cause mortality.
Our study has also shown that patient risk of mortality was positively associated with ePWV, and the subgroup analysis revealed that ePWV was associated with all-cause mortality at different levels. Most of the patients with higher ePWV observed in this study had higher age and a history of hypertension, which is related to the formula we used to calculate ePWV [28]. Moreover, our study has found that nonsmokers were overrepresented in the population with higher ePWV, which is related to the fact that our study population was a coronary artery disease population. In addition, the high ePWV group had poorer indicators of renal function and higher lipid levels, factors that may also increase the risk of all-cause mortality.
Our study is consistent with the findings reported by Po-ChaoHsu et al. [29,30,31], who included 881 Taiwanese patients with a median follow-up of 94 months and evaluated ePWV and baPWV as independent predictors of cardiovascular prognosis and all-cause mortality. However, our analysis differs significantly from their study in that their study focused more on the assessment of the cumulative predictive value of ePWV, whereas our work focused on the predictive value of ePWV for all-cause disease and the close relationship between them. Both studies argued that ePWV could be used as a predictor of all-cause mortality in coronary artery disease, and our findings are in line with Esben Laugesen [32], who argued that ePWV can be used as an independent predictor of all-cause mortality in coronary artery disease.
Despite the important findings of our study, there are still some limitations that need to be addressed. First, our analysis can only predict the association between ePWV and all-cause mortality of coronary artery disease, and the causality of this association needs to be verified with more prospective data. This cohort study primarily focuses on patients with coronary heart disease, and analyzes all-cause mortality as the primary outcome. In subsequent studies, the competitive risk model can be used to investigate the competing relationship between cardiovascular death and all-cause mortality. Second, our study was designed to assess fatal events and therefore did not examine the effect of ePWV on nonfatal MACE events. Third, our data were obtained from the NHANES database of adult Americans, and further research is needed to assess whether the results of this study are applicable to other populations with different economic and geographical statuses. Finally, although we adjusted for relevant confounders, there are still possible relevant potential confounders that were not adjusted for. Therefore, studies with larger sample sizes and more variables are needed to confirm the association between ePWV and all-cause mortality from coronary artery disease.
Conclusions
To sum up, patients with coronary artery disease who undergo long-term follow-up show a significant association between ePWV and all-cause mortality. The risk of all-cause mortality increases considerably when ePWV is higher than 11.15 m/s. Given this, it is crucial to adjust the risk assessment and management plan based on ePWV when managing patients with coronary artery disease.
Availability of data and materials
The data of this study are public data and can be obtained on the official website of NHANES : https://www.cdc.gov/nchs/nhanes.
References
van Sloten TT, Tafflet M, Perier MC, Dugravot A, Climie R, Singh-Manoux A, Empana JP. Association of Change in Cardiovascular Risk factors with Incident Cardiovascular events. JAMA. 2018;320(17):1793–804.
Shaya GE, Leucker TM, Jones SR, Martin SS, Toth PP. Coronary heart disease risk: low-density lipoprotein and beyond. Trends Cardiovasc Med. 2022;32(4):181–94.
Yayan J. Emerging families of biomarkers for coronary artery disease: inflammatory mediators. Vasc Health Risk Manag. 2013;9:435–56.
Matsuzawa Y, Lerman A. Endothelial dysfunction and coronary artery disease: assessment, prognosis, and treatment. Coron Artery Dis. 2014;25(8):713–24.
Medina-Leyte DJ, Zepeda-Garcia O, Dominguez-Perez M, Gonzalez-Garrido A, Villarreal-Molina T, Jacobo-Albavera L. Endothelial dysfunction, inflammation and coronary artery disease: potential biomarkers and promising therapeutical approaches. INT J MOL SCI 2021, 22(8).
Khera AV, Kathiresan S. Genetics of coronary artery disease: discovery, biology and clinical translation. NAT REV GENET. 2017;18(6):331–44.
Bansilal S, Castellano JM, Fuster V. Global burden of CVD: focus on secondary prevention of cardiovascular disease. INT J CARDIOL. 2015;201(Suppl 1):1–S7.
De Backer GG. Prevention of cardiovascular disease in the working population at high cardiovascular risk. EUR J PREV CARDIOL. 2017;24(14):1541–3.
Wu W, Li X, Zuo G, Pu J, Wu X, Chen S. The role of Angiogenesis in Coronary Artery Disease: a double-edged Sword: Intraplaque Angiogenesis in Physiopathology and Therapeutic Angiogenesis for treatment. Curr Pharm Des. 2018;24(4):451–64.
Sato H, Hayashi J, Harashima K, Shimazu H, Kitamoto K. A population-based study of arterial stiffness index in relation to cardiovascular risk factors. J ATHEROSCLER THROMB. 2005;12(3):175–80.
Amar J, Ruidavets JB, Chamontin B, Drouet L, Ferrieres J. Arterial stiffness and cardiovascular risk factors in a population-based study. J HYPERTENS. 2001;19(3):381–7.
Harloff A, Mirzaee H, Lodemann T, Hagenlocher P, Wehrum T, Stuplich J, Hennemuth A, Hennig J, Grundmann S, Vach W. Determination of aortic stiffness using 4D flow cardiovascular magnetic resonance - a population-based study. J Cardiovasc Magn Reson. 2018;20(1):43.
Gkaliagkousi E, Douma S. The pathogenesis of arterial stiffness and its prognostic value in essential hypertension and cardiovascular diseases. HIPPOKRATIA. 2009;13(2):70–5.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37(5):1236–41.
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113(5):664–70.
Fiori G, Fuiano F, Scorza A, Conforto S, Sciuto SA. Non-invasive methods for PWV Measurement in Blood Vessel Stiffness Assessment. IEEE Rev Biomed Eng. 2022;15:169–83.
Hametner B, Wassertheurer S, Mayer CC, Danninger K, Binder RK, Weber T. Aortic pulse Wave Velocity Predicts Cardiovascular events and mortality in patients undergoing coronary angiography: a comparison of invasive measurements and noninvasive estimates. Hypertension. 2021;77(2):571–81.
Kubozono T, Miyata M, Kawasoe S, Ojima S, Yoshifuku S, Miyahara H, Maenohara S, Ohishi M. High pulse Wave Velocity has a strong impact on early carotid atherosclerosis in a japanese General Male Population. CIRC J. 2017;81(3):310–5.
Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cifkova R, Cosentino F, De Carlo M, Gallino A, Landmesser U, Laurent S, et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation: endorsed by the Association for Research into arterial structure and physiology (ARTERY) society. ATHEROSCLEROSIS. 2015;241(2):507–32.
Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. EUR HEART J. 2018;39(33):3021–104.
Greve SV, Blicher MK, Kruger R, Sehestedt T, Gram-Kampmann E, Rasmussen S, Vishram JK, Boutouyrie P, Laurent S, Olsen MH. Estimated carotid-femoral pulse wave velocity has similar predictive value as measured carotid-femoral pulse wave velocity. J HYPERTENS. 2016;34(7):1279–89.
Determinants of pulse wave velocity. In healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. EUR HEART J. 2010;31(19):2338–50.
Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, Boutouyrie P, Cameron J, Chen CH, Cruickshank JK, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J AM COLL CARDIOL. 2014;63(7):636–46.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J AM COLL CARDIOL. 2010;55(13):1318–27.
Georgianos PI, Vaios V, Eleftheriadis T, Zebekakis PE, Liakopoulos V. Pulse Wave Velocity Assessment for Cardiovascular Risk Prognostication in ESKD: weighting recent evidence. CURR VASC PHARMACOL. 2021;19(1):4–11.
Sequi-Dominguez I, Cavero-Redondo I, Alvarez-Bueno C, Pozuelo-Carrascosa DP, Nunez DAS, Martinez-Vizcaino V. Accuracy of pulse Wave Velocity Predicting Cardiovascular and all-cause mortality. A systematic review and Meta-analysis. J CLIN MED 2020, 9(7).
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, Inoguchi T, Maeda Y, Kohara K, Tabara Y, et al. Brachial-ankle pulse Wave Velocity and the risk prediction of Cardiovascular Disease: an individual Participant Data Meta-Analysis. Hypertension. 2017;69(6):1045–52.
Vlachopoulos C, Terentes-Printzios D, Laurent S, Nilsson PM, Protogerou AD, Aznaouridis K, Xaplanteris P, Koutagiar I, Tomiyama H, Yamashina A, et al. Association of estimated pulse Wave Velocity with Survival: a secondary analysis of SPRINT. JAMA Netw Open. 2019;2(10):e1912831.
Hsu PC, Lee WH, Tsai WC, Chen YC, Chu CY, Yen HW, Lin TH, Voon WC, Lai WT, Sheu SH, et al. Comparison between estimated and brachial-ankle pulse wave velocity for cardiovascular and overall mortality prediction. J Clin Hypertens (Greenwich). 2021;23(1):106–13.
Wong CW, Kwok CS, Narain A, Gulati M, Mihalidou AS, Wu P, Alasnag M, Myint PK, Mamas MA. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart. 2018;104(23):1937–48.
Vlachopoulos C, Aznaouridis K, Bratsas A, Ioakeimidis N, Dima I, Xaplanteris P, Stefanadis C, Tousoulis D. Arterial stiffening and systemic endothelial activation induced by smoking: the role of COX-1 and COX-2. INT J CARDIOL. 2015;189:293–8.
Laugesen E, Olesen K, Peters CD, Buus NH, Maeng M, Botker HE, Poulsen PL. Estimated pulse Wave Velocity is Associated with all-cause Mortality during 8.5 years follow-up in patients undergoing elective coronary angiography. J AM HEART ASSOC. 2022;11(10):e25173.
Acknowledgements
Not applicable.
Funding
This study was sponsored by the Xuzhou Science and Technology Bureau (grant number: KC19181).
Author information
Authors and Affiliations
Contributions
Chunwei Chen and Wei Bao designed this study. Chengwen Chen, Lingyao Chen and Liudi Wang conducted data cleaning and statistical analysis. Chengwen Chen and Liudi Wang made the result interpretation. Lingyao Chen participated in the discussion; Chunwei Chen drafted the manuscript, and Haibin Gong revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The National center for Health Statistics Research Ethics Review Board approved all protocols, and informed permission was acquired from all participants included in the investigation.
Consent for publication
Not applicable.
Ethical Statement
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, C., Bao, W., Chen, C. et al. Association between estimated pulse wave velocity and all-cause mortality in patients with coronary artery disease: a cohort study from NHANES 2005–2008. BMC Cardiovasc Disord 23, 412 (2023). https://doi.org/10.1186/s12872-023-03435-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03435-0