Abstract
Background
Post-COVID-19 syndromes have associated with female sex, but the pathophysiological basis is uncertain.
Aim
There are sex differences in myocardial inflammation identified using cardiac magnetic resonance (CMR) in post-COVID-19 patients, and in patient reported health outcomes following COVID-19 infection.
Design
This prospective study investigated the time-course of multiorgan injury in survivors of COVID-19 during convalescence.
Methods
Clinical information, blood biomarkers, and patient reported outcome measures were prospectively acquired at enrolment (visit 1) and 28–60 days post-discharge (visit 2). Chest computed tomography (CT) and CMR were performed at visit 2. Follow-up was carried out for serious adverse events, including death and rehospitalization.
Results
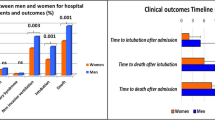
Sixty-nine (43%) of 159 patients recruited were female. During the index admission, females had a lower peak C-reactive protein (74 mg/l (21,163) versus 123 mg/l (70, 192) p = 0.008) and peak ferritin (229 μg/l (103, 551) versus 514 μg/l (228, 1122) p < 0.001). Using the Modified Lake-Louise criteria, females were more likely to have definite evidence of myocardial inflammation (54% (37/68) versus 33% (30/90) p = 0.003). At enrolment and 28–60 days post-discharge, enhanced illness perception, higher levels of anxiety and depression and lower predicted maximal oxygen utilization occurred more commonly in women. The mean (SD, range) duration of follow-up after hospital discharge was 450 (88) days (range 290, 627 days). Compared to men, women had lower rates of cardiovascular hospitalization (0% versus 8% (7/90); p = 0.018).
Conclusions
Women demonstrated worse patient reported outcome measures at index admission and 28–60 days follow-up though cardiovascular hospitalization was lower.
Similar content being viewed by others
Introduction
Immune response to infection is sex-specific and likely to drive infection severity risk and mortality risk [1, 2]. This has been reported for the severe acute respiratory syndrome coronavirus-1 (SARS-CoV1) epidemic [3] and the middle eastern respiratory syndrome (MERS) outbreak [4]. Recently, a similar male bias towards severe disease has been reported with SARS-CoV-2 [5,6,7,8] despite similar infection rates between sexes [9]. Registry data reports that this mortality difference is only partly due to sex and gender differences in high risk characteristics [7, 8] and is independent of age [10]. Men were also more likely to have symptomatic COVID-19 illness compared with women [11].
Despite the higher morbidity and mortality in men with acute SARS-CoV-2 infection, a larger percentage of women tend to be at greater risk for long-term COVID-19 manifestations irrespective of baseline severity of disease [12, 13]. In fact, women were less likely to report a recovery back to baseline, and seven times as likely to report dyspnea, and twice as likely to report fatigue [14].
Prior studies using cardiovascular magnetic resonance imaging in COVID-19 have reported imaging features of myocardial inflammation in 27–60%, [15,16,17,18] of patients but the presence and nature of sex associations are incompletely understood.
Our hypotheses were that there are sex differences in myocardial inflammation identified using cardiac magnetic resonance (CMR) in post-COVID-19 patients scanned at 28–60 days, and in patient reported health outcomes following COVID-19 infection.
Methods
Design
The design and the main findings of the CISCO-19 study have been reported [19, 20]. In this manuscript the terms male and female have been used when referring to biological sex, whereas man and woman are used when referring to psychosocial gender, or when these factors are not clear.
In summary, this study involved a prospective, observational, longitudinal, cohort design to assess the time-course of multiorgan injury in survivors of COVID-19 during convalescence [19]. Clinical information, a 12-lead digital ECG, blood and urine biomarkers, and patient reported outcome measures were acquired at enrolment (visit 1) and again during convalescence, 28–60 days post-discharge (visit 2). Chest computed tomography (CT), including pulmonary and coronary angiography, and cardiac MRI were carried out at visit 2. This sex-based analysis of the primary and secondary outcomes was prespecified.
Participant identification
Patients who received hospital care for COVID-19, with or without admission, and were alive, were prospectively screened in real time using an electronic healthcare information system (TrakCare®, InterSystems®, USA) and daily hospital reports identifying inpatients with laboratory-positive results for COVID-19.
Eligibility criteria
The inclusion criteria were: (1) age ≥ 18 years old; (2) history of an unplanned hospital visit e.g., emergency department, or hospitalization > 24 h for COVID-19 confirmed by a polymerase chain reaction (PCR) test; (3) ability to comply with study procedures; and (4) ability to provide written informed consent. Imaging results were reported by accredited radiologists according to contemporary, national guidelines [21].
The exclusion criteria were: (1) contra-indication to magnetic resonance (MR) imaging (e.g., severe claustrophobia, metallic foreign body); and (2) lack of informed consent.
Diagnosis of COVID-19
A diagnosis of COVID-19 was based on laboratory evidence of SARS-CoV-2 infection using a PCR test (Roche Cobas 6800 or Seegene SARS-CoV-2 PCR) on a biospecimen [22].
Research schedule
The protocol involved two visits. The first visit involved informed consent and assessments during the initial hospitalization, or as soon as possible after discharge. The second visit occurred 28–60 days post-discharge. This window was positioned to reflect the convalescent phase and give sufficient scope to schedule the patients.
The procedures involved prospective collection of clinical data and a time-course of research investigations. Clinical data included demographics, medical and cardiovascular history, findings from clinical examinations, laboratory and radiological tests, cardiology tests (including an electrocardiogram (ECG) and an echocardiogram if available) and treatment. The research investigations at both visits included blood and urine samples, a 12-lead ECG, health status questionnaires, and assessments of adverse events. Heart, lung, and kidney imaging were acquired at the second visit.
Biomarkers
Blood samples were collected at enrolment (visit 1) and 28–60 days post discharge (visit 2). Circulating biomarkers of cardiac injury (troponin I, N-terminal (NT)-pro hormone brain natriuretic peptide (NT-proBNP), inflammation (C-reactive protein, ferritin, interleukin-6), thrombosis (TCT ratio, D-Dimer, fibrinogen, Factor VIII, antithrombin, protein C, protein S), endothelial activation (von Willebrand factor (vWF):GP1bR, VWF:Ag, ICAM-1, VCAM-1, p-selectin, ST2) and renal function (serum creatinine, glomerular filtration rate (GFR) was estimated using the Chronic Kidney Disease Epidemiology (CKD-EPI) Equation [23]), and their changes over time, were investigated. The measurements were undertaken in a central laboratory, blinded to the other clinical data.
Multimodality imaging
CT
A 320-detector CT scanner (Aquilion ONE, Canon Medical Systems Corp.) provided full heart coverage within a single heartbeat. Non-contrast and contrast-enhanced angiographic breath-hold ECG-gated volumes were acquired and timed for optimum pulmonary and systemic arterial (coronary) opacification. Patients with severe renal dysfunction underwent non-contrast CT.
Cardiovascular MRI
Cardiovascular MRI was undertaken to measure heart structure and function and assess for persisting evidence of myocardial injury and/or myocardial infarction using multi-parametric techniques. All patients underwent protocol-directed MRI in the convalescent phase, 28–60 days after discharge. The scan protocol included cine-imaging of cardiac anatomy and function and myocardial tissue characterization using multiparametric techniques. They included 1) mapping myocardial native longitudinal relaxation time (T1 in milliseconds) using the modified Look-Locker inversion recovery technique (T1-mapping) before and after intravenous administration of gadolinium contrast media (0.15 mmol/kg of Magnevist, Bayer Healthcare), 2) mapping transverse relaxation time (T2 in milliseconds), 3) first pass contrast-enhanced perfusion and 4) late gadolinium-enhancement imaging.
The expert consensus recommendations for the MRI diagnostic criteria of non-ischemic myocardial inflammation (modified Lake Louise criteria) were used to diagnose definite myocardial inflammation (abnormal T2 and T1 (native T1, late gadolinium enhancement or extracellular volume)) or probable myocardial inflammation (abnormal: T2 or T1) [24] To limit selection bias, patients with severe renal dysfunction (GFR < 45 ml/kg/m2) were not excluded but did not have gadolinium contrast. Quantitative analyses were undertaken in a central laboratory, blinded to the other clinical data.
Health status and patient reported outcome measures
Questionnaires were completed by participants at visit 1 (enrolment) and visit 2 (28–60 days after the last episode of hospital care). Self-reported health status was assessed using EuroQOL EQ-5D-5L and the Brief Illness Perception Questionnaire (Brief-IPQ). The Patient Health Questionnaire-4 (PHQ–4) was utilized to assess for anxiety and depressive disorders. The Duke Activity Status Index (DASI) was used to assess predicted maximal oxygen utilization. The International Physical Activity Questionnaire—Short Form (IPAQ-SF) measures the forms and intensity of physical activity and sitting time that participants do as part of their daily lives.
Longitudinal follow-up for clinical outcomes
Clinical research team members assessed study participants’ electronic health records. Serious adverse events (SAE), (comprising death and rehospitalization), outpatient clinic visits were assessed as part of follow-up.
Cardiovascular and respiratory SAE were independently reviewed and adjudicated by the clinical event committee team members.
Statistics
Statistical analysis was carried out by the Robertson Centre for Biostatistics. Summary statistics are presented as Mean ± SD, Median (IQR), or N (%). Normally distributed continuous variables, non-normally distributed continuous variables, and categorical variables were analysed by T-Test, Wilcoxon-Mann–Whitney Test, or Fisher's Exact Test respectively.
Linear mixed effects models for patient reported outcome measures (PROMs) include random effects for subjects, fixed effects for age and sex, fixed effects for study visits, and an interaction between sex and visit. Model-derived estimates are reported for differences between women and males at each study visit, and for mean changes between study visits in women and men, with 95% confidence intervals and two-sided p-values. P-values for sex-by-visit interactions are also reported. Duration of follow-up is summarised as Median (IQR), and compared between groups using a Wilcoxon-Mann–Whitney test. Clinical outcomes by sex are summarised, and compared between groups using log rank tests of the time to first event. No adjustments were made for multiplicity, and a p-value of less than 0.05 was considered statistically significant.
Trial management and timelines
The study was conducted in line with the current Guidelines for Good Clinical Practice in Clinical Trials and STrengthening the Reporting of OBservational studies in Epidemiology guidelines, and coordinated by a Study Management Group. A Scientific Steering Group had oversight of the study.
Ethics
The study was approved by the UK National Research Ethics Service (Reference 20/NS/0066).
Registration
ClinicalTrials.gov: NCT04403607.
Results
One thousand three hundred and six patients were screened between 22 May 2020 and 16 March 2021 and 267 patients provided written informed consent (Cognitive impairment, n = 87; frailty, n = 341; death, n = 101; no consent, n = 356; non-compliance with protocol, n = 154).
One hundred and fifty-nine patients were evaluated at 28–60 days after the last episode of hospital care. Most of this population was unvaccinated. 2 (1.3%) had first dose of SARS-CoV-2 vaccination prior to admission, and 11 (6.9%) had the first dose of vaccination prior to Visit 2. Sixty-nine (43%) of them were female. Compared with males, females were younger (52.8 (12.3) years vs. 55.8 (11.5) years; p = 0.113) and were more often healthcare workers (26 (38%) vs. 10 (11%); p < 0.001). There was no difference in ethnic background (p = 0.641). Females had a higher body mass index (32.1 (8.7) kg/m2 vs. 29.2 (5.4) kg/m2; p = 0.012) and lower 10-year percentage cardiovascular risk (%, Q risk 3 calculator, https://qrisk.org/) (9.1 (9.4) vs. 16.5 (11.2); p < 0.001). More males had a history of hypertension (46%, 41/90 versus 22%, 15/69; p = 0.002), myocardial infarction (17%, 15/90 versus 3%, 2/69; p = 0.008) and heart failure (7%, 6/90 versus 0%; p = 0.036). There were no differences in other co-morbidities, presenting characteristics, or treatment (Table 1).
Multisystem phenotyping and adjudicated myocarditis
Biochemistry
During the index admission, females had a lower peak C-reactive protein (74 mg/l (21,163) versus 123 mg/l (70, 192) p = 0.008) and peak ferritin (229 μg/l (103, 551) versus 514 μg/l (228, 1122) p < 0.001).
Electrocardiology
There were no differences in ECG criteria by sex (Table 2).
CT chest, coronary and pulmonary angiography
There were no differences in pulmonary parameters by sex (Table 2). Women were less likely to have obstructive coronary artery disease (6% (4/67) versus 19% (17/90), p = 0.031.
Cardiovascular magnetic resonance imaging
Differences in volumes in keeping with accepted sex specific ranges were observed in ventricular dimensions [25]. Females had higher global T1 values compared to males (50%, 34/68 versus 23%, 21/90; p < 0.001) and increased global extracellular volume values (65% 40/68 versus 38%, 31/90; p = 0.002).
Females had less myocardial late gadolinium enhancement in a non-ischemic distribution, when compared to males (3% (2/68) versus 27% (22/90); p < 0.001).
Using the Modified Lake-Louise criteria [24], females were more likely to have definite evidence of myocardial inflammation (54% (37/68) versus 33% (30/90) p = 0.003).
Health status
Compared to men, at enrolment and 28–60 days post-discharge, women demonstrated enhanced illness perception, higher levels of anxiety and depression and lower predicted maximal oxygen utilization (ml/kg/min) (Table 3). Furthermore, at 28–60 days post-discharge women had lower health-related quality of life, and lower levels of physical activity (Table 3).
Adjusting for age and study visits, health-related quality of life, enhanced illness perception, higher levels of anxiety and depression, lower levels of physical activity and lower predicted maximal oxygen utilization were evident in women (Table 4).
Serious adverse events
Follow-up was continued to December 13, 2021 for all participants. The mean (SD, range) duration of follow-up after hospital discharge was 450 (88) days (range 290, 627 days).
Compared to men, women had lower rates of cardiovascular hospitalization (0% versus 8% (7/90); p = 0.018)(Table 5).
Discussion
This study assessed sex and gender differences in a deeply phenotyped cohort of patients utilizing serum and urine biochemistry, patient reported outcomes and electrocardiograms at baseline and 28–60 days after hospital discharge; cross sectional imaging with computed tomography and magnetic resonance imaging and clinical follow-up up to a mean of 450 days after hospital discharge.
The main findings were:
-
1.
No difference in COVID-19 illness severity between women and men with regards to length of stay or therapy (including intensive care).
-
2.
Male sex was associated with history of hypertension, myocardial infarction and heart failure
-
3.
Female sex was associated with lower peak markers of inflammation during their admission (ferritin, C-reactive protein)
-
4.
There was no sex difference in myopericarditis criteria on ECG.
-
5.
Female sex was associated with lower rates of obstructive coronary artery disease on computed tomography.
-
6.
Female sex was associated with higher cardiac T1 and extracellular volume fraction values. Female sex was associated with higher rates of definitive myocardial inflammation utilizing the Modified Lake-Louise criteria.
-
7.
Worse patient reported outcome measures at index admission and 28–60 days follow-up were demonstrated in women compared to men.
-
8.
Female sex was associated with lower rates of hospitalization for cardiovascular disease in the longer term after COVID-19 infection.
Unlike the meta-analysis reported by Peckham et al. [9], where men had higher odds of requiring intensive care admission or death, we did not identify a difference in acute disease severity for women and men in our smaller study. However, we report persisting changes identified on magnetic resonance imaging and patient reported outcome measures associated with female sex. These findings complement data reported by Bai et al. [12] Sylvester et al. [13] and others that women tend to be at higher risk for COVID-19 manifestations persisting in the longer term irrespective of baseline severity of disease [12, 13].
Women had lower rates of hypertension, myocardial infarction or heart failure, and no difference in other past medical history parameters commonly reported as being associated with worse outcomes in COVID-19 infection including diabetes or smoking status [26]. There was no sex difference in various pulmonary computed tomographic parameters including consolidation, reticulation, atelectasis or thrombosis. A retrospective study looking at 1165 patients reported that female sex was associated with less severe lung involvement [27]. These differences could be due to study design (prospective versus retrospective) and different inclusion criteria (all hospitalized patients) and data analyses (lung involvement quantified utilizing an AI system [28]).
In this study, female sex was associated with lower peak markers of inflammation when compared with male sex, consistent with data reported from the MGH COVID-19 patient registry (n = 781) [29]. These observations point to an immunological basis in the different course of the disease according to sex as per Brodin [30].
To date, there are no reports describing sex- and/or gender- specific differences in myocardial injury utilizing cardiac magnetic resonance imaging in COVID-19 patients in the acute or longer-term [15,16,17,18]. Whilst elevated T1 values per se may be a non-specific finding on its own (elevated in patients with hypertensive heart disease, diabetes), when analyzed as part of the modified Lake-Louise criteria [24] i.e. having both a positive T2-based marker and a T1-based marker (T1 value (ms), extra cellular volume fraction, myocardial late gadolinium enhancement) will increase specificity for diagnosing acute myocardial inflammation, having only one (T2 or T1) marker may still support a diagnosis of acute myocardial inflammation in an appropriate clinical scenario, albeit with less specificity.
A number of studies looking at both hospitalized and non-hospitalized patients [13, 31,32,33] with COVID-19 reported higher rates of depression, anxiety and illness perception in women participants.
There were similar rates of outpatient healthcare uptake between men and women, and similar rates of serious adverse events (death or rehospitalization). In our study, female sex was associated with lower rates of hospitalization for cardiovascular disease in the longer term after COVID-19 infection.
The apparent discrepancy between higher rates of patient reported outcomes in women and increased hospitalization for cardiovascular causes in men could be explained by the small sample size in our study (possible type 1 error), the higher, pre-exisiting cardiovascular disease burden in men, or the possibility that the hospitalization events for cardiovascular causes were not related to COVID-19 infection.
Imaging was carried out from day 28 post discharge to align with the International Severe Acute Respiratory and Emerging Infection Coronavirus Clinical Characterisation Consortium (ISARIC4C) study [34]. Most of the study participants were unvaccinated and the results cannot be extrapolated to vaccinated individuals.
Conclusion
Despite there being no difference in COVID-19 illness severity between women and men with regards to length of stay or therapy, female sex was associated with lower peak markers of inflammation during hospital admission, worse patient reported outcome measures at index admission and 28–60 days follow-up though cardiovascular hospitalization was lower.
Female sex was associated with higher rates of definitive myocardial inflammation on CMR utilizing the Modified Lake-Louise criteria.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. Data requests will be considered by the Steering Group which includes representatives of the Sponsor, the University of Glasgow, senior investigators independent of the research team, and the chief investigator. The Steering Group will take account of the scientific rationale, ethics, logistics, and resource implications. Data access requests should be initially submitted by email to the Chief Investigator (Colin Berry, corresponding author). The source data includes the deidentified numerical data used for the statistical analyses and deidentified imaging scans (MRI, CT) and ECGs. Data access will be provided through the secure analytical platform of the Robertson Centre for Biostatistics. This secure platform enables access to deidentified data for analytical purposes, without the possibility of removing the data from the server. Requests for transfer of deidentified data (including source imaging scans) will be considered by the Steering Group and if approved, a collaboration agreement would be expected. The Steering Group will consider any cost implications and cost recovery would be expected on a not-for-profit basis.
References
Abdullah M, Chai PS, Chong MY, Tohit ERM, Ramasamy R, Pei CP, et al. Gender effect on in vitro lymphocyte subset levels of healthy individuals. Cell Immunol. 2012;272(2):214–9.
Hewagama A, Patel D, Yarlagadda S, Strickland FM, Richardson BC. Stronger inflammatory/cytotoxic T-cell response in women identified by microarray analysis. Genes Immun. 2009;10(5):509–16.
Karlberg J, Chong DSY, Lai WYY. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol. 2004;159(3):229–31.
Alghamdi IG, Hussain II, Almalki SS, Alghamdi MS, Alghamdi MM, El-Sheemy MA. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417–23.
Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020;20(7):442–7.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID-19 in the New York City area. JAMA. 2020;323(20):2052–9.
Singh S, Chowdhry M, Chatterjee A, Khan A. Gender-based disparities in COVID-19 patient outcomes: a propensity-matched analysis. medRxiv; 2020. p. 2020.04.24.20079046. Available from: https://www.medrxiv.org/content/10.1101/2020.04.24.20079046v2. [Cited 2022 Feb 16].
Kragholm K, Andersen MP, Gerds TA, Butt JH, Østergaard L, Polcwiartek C, et al. Association between male sex and outcomes of coronavirus disease 2019 (COVID-19)—a Danish nationwide register-based study. Clinical Infectious Diseases. 2021;73(11):e4025–30.
Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):6317.
Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8. Available from: https://www.frontiersin.org/article/10.3389/fpubh.2020.00152. [Cited 2022 Feb 16].
Abate BB, Kassie AM, Kassaw MW, Aragie TG, Masresha SA. Sex difference in coronavirus disease (COVID-19): a systematic review and meta-analysis. BMJ Open. 2020;10(10):e040129.
Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2021. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8575536/. [Cited 2022 Feb 16].
Sylvester SV, Rusu R, Chan B, Bellows M, O’Keefe C, Nicholson S. Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: a review. Curr Med Res Opin. 2022;0(0):1–9.
Sigfrid L, Drake TM, Pauley E, Jesudason EC, Olliaro P, Lim WS, et al. Long Covid in adults discharged from UK hospitals after Covid-19: a prospective, multicentre cohort study using the ISARIC WHO clinical characterisation protocol. medRxiv; 2021. p. 2021.03.18.21253888. Available from: https://www.medrxiv.org/content/10.1101/2021.03.18.21253888v3. [Cited 2022 Feb 16].
Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021:ehab075. Available from: https://doi.org/10.1093/eurheartj/ehab075. [Cited 2021 Mar 10].
Joy G, Artico J, Kurdi H, Seraphim A, Lau C. Prospective case-control study of cardiovascular abnormalities six months following mild COVID-19 in healthcare workers. JACC Cardiovasc Imaging. 2021;14:2155.
Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020. Available from: https://jamanetwork.com/journals/jamacardiology/fullarticle/2768916. [Cited 2020 Sep 15].
Singh T, Kite TA, Joshi SS, Spath NB, Kershaw L, Baker A, et al. MRI and CT coronary angiography in survivors of COVID-19. Heart. 2021. Available from: https://heart.bmj.com/content/early/2021/10/11/heartjnl-2021-319926. [Cited 2021 Oct 17].
Mangion K, Morrow A, Bagot C, Bayes H, Blyth KG, Church C, et al. The chief scientist office cardiovascular and pulmonary imaging in SARS coronavirus disease-19 (CISCO-19) study. Cardiovasc Res. 2020. Available from: https://academic.oup.com/cardiovascres/advance-article/doi/10.1093/cvr/cvaa209/5875604. [Cited 2020 Aug 13].
Morrow AJ, Sykes R, McIntosh A, Kamdar A, Bagot C, Bayes HK, et al. A multisystem, cardio-renal investigation of post-COVID-19 illness. Nat Med. 2022;23:1–11.
Hare SS, Rodrigues JCL, Nair A, Jacob J, Upile S, Johnstone A, et al. The continuing evolution of COVID-19 imaging pathways in the UK: a British Society of Thoracic Imaging expert reference group update. Clin Radiol. 2020;75(6):399–404.
Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295(1):202–7.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72(24):3158–76.
Petersen SE, Aung N, Sanghvi MM, Zemrak F, Fung K, Paiva JM, et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J Cardiovasc Magn Reson. 2017;19(1):18.
Mahamat-Saleh Y, Fiolet T, Rebeaud ME, Mulot M, Guihur A, El Fatouhi D, et al. Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies. BMJ Open. 2021;11(10):e052777.
Statsenko Y, Al Zahmi F, Habuza T, Almansoori TM, Smetanina D, Simiyu GL, et al. Impact of age and sex on COVID-19 severity assessed from radiologic and clinical findings. Front CellInfect Microbiol. 2022;11. Available from: https://www.frontiersin.org/articles/10.3389/fcimb.2021.777070. [Cited 2022 Aug 30].
MedSeg - free medical segmentation online. MedSeg. Available from: https://www.medseg.ai/. [Cited 2022 Aug 31].
Lau ES, McNeill JN, Paniagua SM, Liu EE, Wang JK, Bassett IV, et al. Sex differences in inflammatory markers in patients hospitalized with COVID-19 infection: Insights from the MGH COVID-19 patient registry. PLoS ONE. 2021;16(4):e0250774.
Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nat Med. 2021;27(1):28–33.
Brotto LA, Chankasingh K, Baaske A, Albert A, Booth A, Kaida A, et al. The influence of sex, gender, age, and ethnicity on psychosocial factors and substance use throughout phases of the COVID-19 pandemic. PLoS One. 2021;16(11):e0259676.
Fernández-de-las-Peñas C, Martín-Guerrero JD, Pellicer-Valero ÓJ, Navarro-Pardo E, Gómez-Mayordomo V, Cuadrado ML, et al. Female sex is a risk factor associated with long-term post-COVID related-symptoms but not with COVID-19 symptoms: the LONG-COVID-EXP-CM multicenter study. J Clin Med. 2022;11(2):413.
Fugazzaro S, Denti M, Mainini C, Accogli MA, Bedogni G, Ghizzoni D, et al. Sex differences and rehabilitation needs after hospital discharge for COVID-19: an Italian cross-sectional study. BMJ Open. 2022;12(5):e055308.
ISARIC 4C (Coronavirus Clinical Characterisation Consortium). isaric4c.github.io. Available from: https://isaric4c.net/index.html. [Cited 2020 May 15].
Acknowledgements
We would like to take the study participants for taking part.
CISCO-19 Investigators
Chief Investigator: Colin Berry1,9
Kenneth Mangion1,9, Pauline Hall Barrientos1,8, Kevin G. Blyth1, Michael Briscoe1, Colin Church1, Christian Delles1,9, Stephen Dobbin1, Keith Gillis1, Antonia Ho1,10, Anna Kamdar1, David J. Lowe1, Kaitlin J. Mayne1,9, Patrick B. Mark1,9, Christopher McGinley1, Connor McKee1, Andrew Morrow1,9, Oliver Peck1, Alastair J Rankin1, Giles Roditi1,3,6, Claire Rooney1, Sarah A. Spiers1, David Stobo1,6, Ryan Wereski1, Sylvia Wright1, Lynn Abel2, Douglas Grieve2. Catherine Bagot3, Hannah Bayes3, Jaclyn Carberry3, Daniel Doherty3, Ian Ferguson3, Vivienne B. Gibson3, Fraser Goldie3, Laura Knox3, Katherine Scot3, David Stobo3, Varun Sharma3, Robert Sykes3,9. Ammani Brown4, Andrew Dougherty4, Kirsty Fallon4, Lesley Gilmour4. Chloe Cowan4, Lynsey Gillespie4, Sharon Kean4, Jurgen Van-Melckebeke4, Kim Moran-Jones4, Debra Stuart4, Maureen Travers4 Tracey Hopkins5, Laura Dymock5, Evonne McLennan5, Rosemary Woodward, 5 Fiona Savage5, Nicola Tynan5. Sau Lee Chang6, Mhairi Dupre6, Lindsey Norton6, Liam Peng6.
Clare Orange7, Rory Gunson7. Sarah Allwood-Spiers8, George Bruce8, Rosario Gonzalez-Lopez8, Rebecca Stace8. Elaine Butler9, Jennifer S Lees9, Naveed Sattar9, Robert Sykes9, Rhian M. Touyz9, Paul Welsh9. Massimo Palmarini10. John G.F. Cleland11, Sharon Kean11, Bernard Kelly11, Alex McConnachie11, Alasdair McIntosh11, Dionne Russell11, Sarah Weeden11. Peter W. Macfarlane12, Louise Inglis12, Jean Watt12, Kathryn McLaren, 12 Shahid Latif (now deceased) 12. Nick Hill13, Dirk Husmeier13, Xiaoyu Luo13. Peter Kellman14, Hui Xue14. Amy Collinsworth15, Sarah Mullen15, Campbell Rogers15. Heerajnarain Bulluck16, David Carrick16, David Corcoran16, Iain Findlay16, Ninian N. Lang16, Vera Lennie16, Ross McGeoch16, Sabrina Nordin16, Alexander Payne16, Keith Robertson16, Nicola Ryan16, Gruschen Veldtman16, Robin P. Weir16, Stuart Watkins16. Neil Basu17, Iain McInnes17, Stefan Siebert.17
1 Queen Elizabeth University Hospital, Glasgow, UK
2 Royal Alexandra Hospital, Paisley, UK
3. Glasgow Royal Infirmary, Glasgow, UK
4 Glasgow Clinical Research Facility and Study Management Group, Queen Elizabeth University Hospital, Glasgow, UK
5 Glasgow Clinical Research Imaging Facility, Imagine Centre of Excellence, Queen Elizabeth University Hospital, UK
6 Radiology, NHS Greater Glasgow and Clyde Health Board, UK
7 Laboratory Medicine and Biorepository, NHS Greater Glasgow and Clyde Health Board, UK
8 Medical Physics, NHS Greater Glasgow and Clyde, UK
9 Institute of Cardiovascular and Medical Sciences, University of Glasgow, UK
10 MRC Centre for Virology Research Institute of Infection, Immunity and Inflammation, University of Glasgow, UK
11 Robertson Centre for Biostatistics, Institute of Health and Wellbeing, University of Glasgow
12 Electrocardiology Core Laboratory, Glasgow Royal Infirmary, UK
13 Departments of Mathematics and Statistics, University of Glasgow, UK
14 National Institutes of Health, Bethesda, US
15 Heartflow, inc, California, US.
16 Clinical Event Committee, UK.
17 Steering Committee, College of Medical, Veterinary and Life Sciences, University of Glasgow, UK.
Funding
This was an investigator-initiated clinical study that was funded by the Chief Scientist Office of the Scottish Government (COV/GLA/Portfolio project number 311300). The funder had no role in the design, conduct (non-voting TSC member), data analysis and interpretation, manuscript writing, or dissemination of the results. C.B, C.D., N.S., R.M.T. were supported by the British Heart Foundation (RE/18/6/34217).
The MRI study involved technologies provided by Siemens Healthcare and the National Institutes of Health. HeartFlow (HeartFlow, Redwood City, CA) provided FFRCT. The study was co-sponsored by NHS Greater Glasgow & Clyde Health Board and the University of Glasgow.
Author information
Authors and Affiliations
Consortia
Contributions
KM, CB made substantial contributions to conception and design. All authors made substantial contributions to acquisition of data; KM, AMC made substantial contributions to the analysis and interpretation of data; KM drafted the article; All authors were involved in revising it critically for important intellectual content; All authors gave final approval of the version to be submitted and any revised version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the UK National Research Ethics Service (Reference 20/NS/0066). All methods were carried out in accordance with relevant guidelines and regulations (Declaration of Helsinki). Informed consent was obtained from all subjects.
Consent for publication
N/A.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mangion, K., Morrow, A.J., Sykes, R. et al. Post-COVID-19 illness and associations with sex and gender. BMC Cardiovasc Disord 23, 389 (2023). https://doi.org/10.1186/s12872-023-03412-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03412-7