Abstract
Objective
This study aimed to examine the effects of mindfulness-based stress reduction (MBSR) in patients with acute myocardial infarction (AMI) after primary percutaneous coronary intervention (PPCI).
Methods
A retrospective study was conducted with data collected from AMI patients who underwent successful PPCI. The study included 61 cases that received 8-week MBSR intervention (MBSR group) and 61 cases that received weekly health education (control group) over the same period. Outcome measures, including hemodynamic parameters, psychosocial characteristics [Hospital Anxiety and Depression Scale (HADS), Perceived Stress Scale (PSS), Perceived Social Support Scale (PSSS)], health-related quality of life [HRQoL, 7-item Seattle Angina Questionnaire (SAQ-7)], and major adverse cardiovascular events (MACE), were assessed at baseline (T1), post-intervention (T2), 1 month after the post-intervention (T3) and 3 months after the post-intervention (T4).
Results
Compared to the control group, the MBSR group showed improvements in blood pressure, specifically in systolic blood pressure (SBP) at T4, and diastolic blood pressure (DBP) at T3 and T4, and mean arterial blood pressure (MABP) at T3 and T4. Additionally, the MBSR group had lower scores of anxiety and perceived stress (HADS, PSS) and higher scores of perceived social support (PSSS) after the intervention. Furthermore, the MBSR group had higher scores on the SAQ-7 at all measurement points. The control group had a significantly higher total MACE rate compared to the MBSR group (26.23% vs. 9.84%).
Conclusions
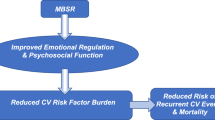
This study provides support for the potential benefits of MBSR as an adjunctive treatment for AMI patients undergoing PPCI.
Similar content being viewed by others
Introduction
Negative emotions such as depression, anxiety, and stress, are commonly experienced by cardiac patients following a myocardial infarction (MI), contributing to poorer mental health and increased risk for adverse outcomes [1, 2]. Primary percutaneous coronary intervention (PPCI), despite being a standard procedure for AMI, is still perceived as risky and stressful by patients due to nervousness, distress, and fear of the unknown [3,4,5]. Furthermore, psychopathologies like anxiety and depression are independent risk factors for cardiac morbidity and mortality [6]. Therefore, there is a need to identify psychological interventions that can alleviate negative emotions in AMI patients after PPCI.
Mindfulness, an popular psychological intervention worldwide originally designed in the 1970s by Jon Kabat-Zinn for chronic pain patients [5], involves cultivating conscious awareness and attention in the present moment, without judgment [7, 8]. One well-known form of mindfulness-based interventions (MBI) is the mindfulness-based stress reduction (MBSR) program, which consists of eight-week session aimed at reducing stress in clinical and non-clinical populations [9, 10]. The core elements of the program include mindfulness exercises during daily activities, such as body scanning, mental exercises, and physical exercises [7].
Over the past decade, several studies have investigated the effectiveness of the MBSR program in cardiac patients. Lundgren O et al. examined the feasibility of MBSR for CAD patients with depressive symptoms and found positive changes in depressive symptoms and mastery scores [11]. Another study conducted on male CHD patients demonstrated significant reductions in anxiety, depression, perceived stress, blood pressure, and BMI after receiving MBSR, with maintained therapeutic gains at the 3-month follow-up [12]. Additionally, a recent study explored the benefits of a modified MBSR intervention delivered via telephone for PCI patients experiencing psychological distress, highlighting the potential of this accessible approach in improving mental well-being [13]. Furthermore, a brief MBSR intervention was found to be beneficial for post-PCI patients younger than 60 years, aiming to reduce psychological symptoms of distress [14]. However, the specific contribution of MBSR in AMI patients after PPCI remains unclear.
Therefore, this study aimed to fill the research gap by conducting a robust evaluation of the effectiveness of MBSR in AMI patients after PPCI, providing valuable insights into the potential benefits of MBSR in this specific population. The study utilized a retrospective design and compares two groups: an MBSR group receiving 8 weekly sessions of 2.5 h each and a 1-day retreat, and a control group receiving weekly health education. Various outcome measures, including hemodynamic parameters, psychosocial characteristics, health-related quality of life (HRQoL), and major adverse cardiovascular events, are assessed at four time points. This study’s innovative approach and focus on the specific population of AMI patients after PPCI contribute to the existing literature and are highly relevant to post-AMI cardiac care.
Methods
Ethical statement
The study was approved by the ethics committee of our hospital, and the informed consent was waived due to the retrospective nature of the study.
Study population
This retrospective analysis collected data between June 2019 and June 2022 on AMI patients who underwent successful PPCI, were moved to an internal medicine ward, and then discharged from our hospital. AMI was defined as acute symptoms of ischemia persisting for more than 30 min within 24 h from the onset of symptoms, with elevations in cardiac biomarker values (preferably cardiac troponin) and eventual detection of coronary artery disease by emergency coronary angiography [15]. The inclusion criteria were as follows: (1) aged ≥ 18 years; (2) successful PPCI, defined as final TIMI (Thrombolysis in Myocardial Infarction) flow grade 3 [16]; and (3) willingness to participate in all assessments. The study excluded patients with the following criteria: heart failure, valvular heart disease classified as more than moderate, moderate pulmonary hypertension, hypertrophic cardiomyopathy, significant renal impairment with an estimated glomerular filtration rate less than 15 mL/min/1.73 m2, attendance of mindfulness training or a stress reduction course (such as relaxation training or cognitive behavioral therapy) within the past two years, presence of psychosis, dementia or communication disturbances, and a history of alcoholism or other substance abuse.
MBSR program
The study included 61 cases that received 8-week MBSR intervention (MBSR group) and 61 cases that received weekly health education (control group). Following a previously standard protocol [1, 17], the MBSR program lasted for 8 weeks and consisted of 8 weekly sessions, each lasting 2.5 h. Additionally, there was a full day of practice (6 h) in week 6. The program was facilitated by an experienced mindfulness trainer and scheduled 4 weeks after the PPCI procedure [18]. Participants were instructed to dedicate 45 min to formal homework exercises, which included mindfulness meditation, breathing practices, and gentle yoga. These exercises were to be completed on a minimum of 6 days per week, and participants were provided with taped audio instructions to guide their practice. As informal practices posed challenges in quantification, they were not specifically assigned. To ensure compliance with the homework requirements, a telephone-based monitoring system was employed on a weekly basis. The regular phone calls served as an opportunity for participants to report their progress, including the frequency and duration of their completed exercises. Outcome data were collected at 4 time points throughout the study: baseline (T1), post-intervention (T2), 1 month after the post-intervention (T3) and 3 months after the post-intervention (T4).
Hemodynamic parameters
Impedance cardiography was used to measure hemodynamic parameters, including heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial blood pressure (MABP).
Psychosocial characteristics
The perceived Stress Scale (PSS) and Perceived Social Support Scale (PSSS) were used to assess the degree of perceived stress and perceived social support from family, friends and significant others, respectively. The 14-item PSS questionnaire examined stress levels using a 4-point scale (score = 0: never; score = 4: very often), with a total score ranging from 0 to 56 [19]. The 12-item PSSS questionnaire was rated on a 7-point Likert scale (score = 1: strongly disagree; score = 7: strongly agree), with higher scores indicating higher levels of perceived support [20]. Levels of anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS), which consists of subscales with a total possible score range of 0–21 each. The HADS uses a 4-point rating scale, with 0 representing “none” and 3 representing “severe”.
Measurement of HRQoL
HRQoL was measured using the 7-item Seattle Angina Questionnaire (SAQ-7), which includes three domains: physical limitation, angina frequency, and quality of life [21]. Higher scores indicate better HRQoL.
Clinical endpoints during the follow-up
Major adverse cardiovascular events (MACE) during the follow-up period were defined as heart failure (HF) requiring hospitalization, recurrent MI, repeat revascularization, and cardiac death. Hospitalization and death due to non-cardiac cause was not considered events.
Calculation of sample size
A post hoc sample size calculation was performed using G*Power 3.1.9.2 software to determine the appropriate sample size for a t-test comparing the means of two independent groups. The calculation was based on the variable SBP at T4. The MBSR group consisted of 61 participants, with a mean SBP of 129.6 mmHg and a standard deviation (SD) of 11.61. The control group also comprised 61 participants, with a mean SBP of 135.9 mmHg and a SD of 12.83. The effect size (d) was determined to be 0.514. With an α error (significance level) set at 0.05, a post hoc sample size calculation was conducted, yielding a power of 80.53%.
Statistical analysis
All statistical analyses were performed using Prism (version 8.0, GraphPad, San Diego, California, USA). Continuous data were summarized as means ± standard deviation (SD) or median ± interquartile range (IQR) after testing for normality using the Shapiro-Wilk test. Between-group comparisons were conducted using t-test or Mann-Whitney test, depending on the distribution of the data. Categorical variables were presented as n (%) and compared using chi-square or Fisher’s exact test. Two-tailed tests were performed for each comparison, with a P value of less than 0.05 considered statistically significant.
Results
Demographic and baseline characteristics
A total of 122 patients participated in this study, with a mean age of 58.69 ± 14.80 years (ranging from 18 to 72 years). The majority of the patients were male (68.03%), married (91.80%), and had a high school education or higher (68.85%). Table 1 provided detailed characteristics of the participants in the MBSR and control groups, showing no significant differences in gender (P = 0.244), age (P = 0.395), marital status (P = 0.788) and level of education (P = 0.320). Additionally, there were no significant differences in comorbidities, clinical presentation, lesion characteristics, culprit vessel, procedural characteristics, in-hospital adverse events, medication use at discharge, and length of hospital stay between the MBSR group and control group (all P > 0.05).
Comparison of hemodynamic parameters in AMI patients undergoing PPCI between MBSR and control groups
As shown in Table 2, there was no significant difference in HR between the MBSR and control groups at baseline and follow-up (all P > 0.05). However, the MBSR group showed decreased blood pressure compared to the control group at specific time points: SBP at T4 (P = 0.005), DBP at T3 (P = 0.018) and T4 (P < 0.001), and MABP at T3 (P = 0.003) and T4 (P < 0.001).
Effectiveness of MBSR intervention on psychosocial characteristics in AMI patients undergoing PPCI
Figure 1 illustrated a comparison of psychosocial characteristics between the two groups. Independent-sample t-tests revealed no differences in the scores of HADS, PSS and PSSS between the MBSR and control groups at baseline (T1) (all P > 0.05). However, significant differences were observed between the MBSR and control groups at T2, T3, and T4, with lower scores of HADS and PSS and a higher score of PSSS in the MBSR group compared to the control group (all P < 0.05).
Effectiveness of MBSR intervention on psychosocial characteristics in patients with acute myocardial infarction (AMI) undergoing primary percutaneous coronary intervention (PPCI)
Note: The psychosocial characteristics assessed include the Hospital Anxiety and Depression Scale (HADS, A-B), Perceived Social Support Scale (PSSS, C) and Perceived Stress Scale (PSS, D). The measurements were taken at baseline (T1), post-intervention (T2), 1 month after post-intervention (T3), and 3 months after post-intervention (T4). The significance levels are indicated as follows: * P < 0.05; *** P < 0.005; **** P < 0.001
Improvement of MBSR intervention on HRQoL in AMI patients undergoing PPCI
The independent-sample t-test with the SAQ-7 total score and its three domains showed no difference between the MBSR and control groups at baseline (all P > 0.05). However, significant improvements in physical limitation, angina frequency, and quality of life were observed in the MBSR group at T2-T4 compared to the control group (Fig. 2A-C). Furthermore, the overall SAQ-7 total score was higher in the MBSR group than the control group at all measurement points (Fig. 2D).
Improvement of MBSR intervention on Health-related quality of life (HRQoL) in patients with acute myocardial infarction (AMI) undergoing primary percutaneous coronary intervention (PPCI)
Note: The comparison of HRQoL assessed by SAQ-7 score in AMI patients after PPCI between the 2 groups, including physical limitation (A), angina frequency (B), and quality of life (C) and total score (D). The measurements were taken at baseline (T1), post-intervention (T2), 1 month after post-intervention (T3), and 3 months after post-intervention (T4). The significance levels are indicated as follows: * P < 0.05; **** P < 0.001
Clinical endpoints in AMI patients undergoing PPCI after MBSR intervention
The occurrence of MACE was evaluated (Table 3). During the 3-month follow-up, 22 patients experienced MACE, including 11 cases of HF requiring hospitalization, 4 cases of recurrent MI, and 7 cases requiring repeated revascularization. No cardiac deaths were reported. Although a slightly lower proportions of AMI patients in the MBSR group developed heart failure requiring hospitalization, recurrent MI and repeated revascularization compared to the weekly health education group, the differences were not statistically significant (all P > 0.05). However, the total MACE rate was significantly higher in the control group as compared to the MBSR group (26.23% vs. 9.84%, P = 0.032).
Discussion
A growing body of research evidence suggested that MBSR has measurable and long-lasting benefits in medical and psychological well-being in various conditions [22, 23]. Consistent with previous literature, our study found that MBSR had positive effects on BP regulation. We observed a trend for improvement in SBP at the 3-month follow-up in the MBSR group, with decreased DBP and MABP at 1 month and 3 months post-intervention. These findings align with studies demonstrating the potential of in lowering BP in clinical populations such as cancer and hypertension [24, 25] as well as non-clinical populations like healthcare workers and victims of gun violence [26, 27]. Additionally, a previous study found sustained decreases in cholesterol levels after MBSR in older adults at risk for coronary artery disease [28], and which may further impact blood pressure regulation [29].
The ability of patients to track and cope with stress was also found to increase with greater awareness of their emotions and bodily sensations [5]. Our study demonstrated that AMI patients after PPCI who participated in the MBSR program showed improved psychosocial characteristics at post-intervention (T2), 1 month (T3), and 3 months (T4) follow-up compared to those who received weekly health education over the same period. The MBSR group exhibited lower perceived stress, anxiety and depression, as well as higher levels of perceived social support. These findings are consistent with previous studies reporting improved psychosocial characteristics following MBSR in cardiac patients. For example, Parswani M J et al. found the significant reductions in negative emotions and perceived stress in patients with coronary heart disease (CHD) who underwent an 8-week MBSR program, with therapeutic gains maintained at the 3-month follow-up [12]. Similarly, Lundgren O et al. demonstrated immediate and sustained improvement in depressive symptoms after an 8-week MBSR course in CAD patients following a coronary event [11]. These findings highlight the added benefits of using MBSR techniques to manage stress and psychosocial symptoms in cardiac patients, including those with AMI undergoing PPCI.
SAQ-19 was designed to be a more sensitive measure of recent changes in angina, and SAQ-7 was to assess patients’ satisfaction with the care they received for their coronary disease, which was more appropriate for most applications as reported by Thomas M et al. [30]. The MBSR group showed significant improvements in physical limitation, angina frequency, and overall QoL as measured by the SAQ-7 compared to the control group at all measurement points (T2-T4). These findings align with other studies examining the effects of MBSR on HRQoL. Jalali D et al. found stable HRQoL improvement in cardiovascular disease patients at the post-test and 3-month follow-up using the 36-item Short Form Survey (SF-36) after a MBSR program [31]. Nijjar et al. observed a similar trend in HRQoL between MBSR and control groups at 3 months in a pilot randomized controlled trial with cardiac patients eligible for cardiac rehabilitation [1]. These studies collectively demonstrated the effectiveness of MBSR in improving HRQoL. Finally, we evaluated the impact of MBSR on the occurrence of MACE. Despite having a small number of participants, our results revealed a significantly lower total MACE rate in the MBSR group compared to the control group (9.84% vs. 26.23%). This finding suggests that MBSR may have a positive effect on clinical endpoints in AMI patients after PPCI, which is an underexplored topic in the literature.
A major limitation of our study was its retrospective observational design instead of a randomized controlled trial. Furthermore, despite observing differences in blood pressure between the MBSR and control groups during the 3-month follow-up, it is crucial to acknowledge several limitations in our study. Firstly, the 3-month follow-up period may not fully capture the long-term effects of MBSR on blood pressure. It is possible that the observed differences might diminish or disappear beyond this time frame, as most AMI patients without complications tend to return to baseline or normal life and have stable hemodynamics after 3 months. Future studies with longer follow-up durations are needed to provide more comprehensive insights into the sustained effects of MBSR on blood pressure. Secondly, individual variations in response to MBSR could have influenced the observed differences in blood pressure. Some patients may have experienced more pronounced improvements, while others may not have shown significant changes. The influence of these individual differences should be considered when interpreting the results. It would be valuable to explore potential factors that may contribute to differential responses to MBSR, such as baseline characteristics or psychological factors. Lastly, it is essential to note that our study focused on a specific population of AMI patients without complications. The generalizability of our findings to other populations or individuals with different clinical profiles should be approached with caution. Future research should aim to replicate these findings in larger and more diverse samples to determine the broader applicability of MBSR in different patient populations.
Conclusion
In summary, this study provides evidence that MBSR can be a beneficial adjunctive treatment in AMI patients undergoing PPCI, as it shows positive effects on alleviating negative emotion and perceived stress, increasing perceived social support, and reducing MACE. However, it is important to recognize that these findings are specific to the studied population and caution should be exercised in extrapolating the results to all cardiac patients.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Nijjar PS, Connett JE, Lindquist R, Brown R, Burt M, Pergolski A, Wolfe A, Balaji P, Chandiramani N, Yu X, et al. Randomized Trial of Mindfulness-Based stress reduction in Cardiac Patients Eligible for Cardiac Rehabilitation. Sci Rep. 2019;9(1):18415.
Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21(1):30–8.
Saito Y, Tateishi K, Kanda M, Shiko Y, Kawasaki Y, Kobayashi Y, Inoue T. Volume-Outcome Relationships for Percutaneous Coronary intervention in Acute myocardial infarction. J Am Heart Assoc. 2022;11(6):e023805.
Shibayama K. Factors related to the improvement of quality of life at 6 months after discharge for myocardial infarction patients treated with percutaneous coronary intervention. J Rural Med. 2012;7(1):33–7.
Chacko E, Ling B, Avny N, Barak Y, Cullum S, Sundram F, Cheung G. Mindfulness-based cognitive therapy for stress reduction in Family Carers of People living with dementia: a systematic review. Int J Environ Res Public Health 2022, 19(1).
Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, Bennett P, Liu Z, West R, Thompson DR, et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2017;4(4):CD002902.
Taub R, Horesh D, Rubin N, Glick I, Reem O, Shriqui G, Agmon-Levin N. Mindfulness-based stress reduction for systemic lupus erythematosus: a mixed-methods pilot randomized controlled trial of an adapted protocol. J Clin Med 2021, 10(19).
Kriakous SA, Elliott KA, Lamers C, Owen R. The effectiveness of mindfulness-based stress reduction on the psychological functioning of Healthcare Professionals: a systematic review. Mindfulness (N Y). 2021;12(1):1–28.
Hoge EA, Bui E, Mete M, Dutton MA, Baker AW, Simon NM. Mindfulness-based stress reduction vs Escitalopram for the treatment of adults with anxiety Disorders: a Randomized Clinical Trial. JAMA Psychiatry 2022.
Guendelman S, Bayer M, Prehn K, Dziobek I. Towards a mechanistic understanding of mindfulness-based stress reduction (MBSR) using an RCT neuroimaging approach: Effects on regulating own stress in social and non-social situations. NeuroImage. 2022;254:119059.
Lundgren O, Garvin P, Nilsson L, Tornerefelt V, Andersson G, Kristenson M, Jonasson L. Mindfulness-based stress reduction for coronary artery Disease Patients: potential improvements in mastery and depressive symptoms. J Clin Psychol Med Settings. 2022;29(3):489–97.
Parswani MJ, Sharma MP, Iyengar S. Mindfulness-based stress reduction program in coronary heart disease: a randomized control trial. Int J Yoga. 2013;6(2):111–7.
Hou Y, Zhao X, Lu M, Lei X, Wu Q, Wang X. Brief, one-on-one, telephone-adapted mindfulness-based stress reduction for patients undergoing percutaneous coronary intervention: a randomized controlled trial. Transl Behav Med. 2019;9(6):1216–23.
Nyklicek I, Dijksman SC, Lenders PJ, Fonteijn WA, Koolen JJ. A brief mindfulness based intervention for increase in emotional well-being and quality of life in percutaneous coronary intervention (PCI) patients: the MindfulHeart randomized controlled trial. J Behav Med. 2014;37(1):135–44.
Kawamura Y, Yoshimachi F, Murotani N, Karasawa Y, Nagamatsu H, Kasai S, Ikari Y. Comparison of Mortality Prediction by the GRACE score, multiple biomarkers, and their combination in all-comer patients with Acute myocardial infarction undergoing primary percutaneous coronary intervention. Intern Med 2022.
Nishihira K, Kuriyama N, Kadooka K, Honda Y, Yamamoto K, Nishino S, Ebihara S, Ogata K, Kimura T, Koiwaya H, et al. Outcomes of Elderly patients with Acute myocardial infarction and heart failure who undergo percutaneous coronary intervention. Circ Rep. 2022;4(10):474–81.
Kabatzinn J. Using the wisdom of your body and mind to face stress, pain and illness. 1990.
Kim Y. Health-Related quality of life in patients with coronary artery Disease undergoing percutaneous coronary intervention: a cross-sectional study. J Nurs Res. 2021;30(1):e186.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Huang Y, Su X, Si M, Xiao W, Wang H, Wang W, Gu X, Ma L, Li J, Zhang S, et al. The impacts of coping style and perceived social support on the mental health of undergraduate students during the early phases of the COVID-19 pandemic in China: a multicenter survey. BMC Psychiatry. 2021;21(1):530.
Chan PS, Jones PG, Arnold SA, Spertus JA. Development and validation of a short version of the Seattle angina questionnaire. Circ Cardiovasc Qual Outcomes. 2014;7(5):640–7.
Marske C, Shah S, Chavira A, Hedberg C, Fullmer R, Clark CJ, Pipitone O, Kaiser P. Mindfulness-based stress reduction in the management of Chronic Pain and its Comorbid Depression. J Am Osteopath Assoc. 2020;120(9):575–81.
Marotta M, Gorini F, Parlanti A, Berti S, Vassalle C. Effect of mindfulness-based stress reduction on the Well-Being, Burnout and stress of italian Healthcare Professionals during the COVID-19 pandemic. J Clin Med 2022, 11(11).
Lengacher CA, Reich RR, Paterson CL, Shelton M, Shivers S, Ramesar S, Pleasant ML, Budhrani-Shani P, Groer M, Post-White J, et al. A large Randomized Trial: Effects of Mindfulness-Based stress reduction (MBSR) for breast Cancer (BC) survivors on salivary cortisol and IL-6. Biol Res Nurs. 2019;21(1):39–49.
Conversano C, Orru G, Pozza A, Miccoli M, Ciacchini R, Marchi L, Gemignani A. Is mindfulness-based stress reduction effective for people with hypertension? A systematic review and Meta-analysis of 30 years of evidence. Int J Environ Res Public Health 2021, 18(6).
Green AA, Kinchen EV. The Effects of Mindfulness Meditation on stress and burnout in nurses. J Holist Nurs. 2021;39(4):356–68.
Khatib L, Riegner G, Dean JG, Oliva V, Cruanes G, Mulligan BA, Zeidan F. The Effects of Mindfulness-Based stress reduction on trauma in victims of Gun Violence: a pilot study. Mindfulness (N Y). 2022;13(4):1032–41.
Gentile C, Starnino L, Dupuis G, D’Antono B. Mindfulness-based stress reduction in older adults at risk for coronary artery disease: a pilot randomized Trial. Clin Gerontol. 2022;45(2):272–86.
Ferrara LA, Guida L, Iannuzzi R, Celentano A, Lionello F. Serum cholesterol affects blood pressure regulation. J Hum Hypertens. 2002;16(5):337–43.
Thomas M, Jones PG, Arnold SV, Spertus JA. Interpretation of the Seattle Angina Questionnaire as an Outcome measure in clinical trials and clinical care: a review. JAMA Cardiol. 2021;6(5):593–9.
Jalali D, Abdolazimi M, Alaei Z, Solati K. Effectiveness of mindfulness-based stress reduction program on quality of life in cardiovascular disease patients. Int J Cardiol Heart Vasc. 2019;23:100356.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JJG: design of the work, the acquisition, analysis, interpretation of data; XST: analysis, interpretation of data; SSM: design of the work, interpretation of data; SHX: analysis, interpretation of data; JYH: design of the work, analysis, interpretation of data. All the authors were actively involved in writing different portions of the manuscript. All authors have reviewed and proofread the manuscript and approved final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of Hangzhou First People’s Hospital, and the informed consent was waived due to retrospective nature of the study. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gu, JJ., Tong, XS., Meng, SS. et al. Effect of mindfulness-based stress reduction in patients with acute myocardial infarction after successful primary percutaneous coronary intervention: a retrospective study. BMC Cardiovasc Disord 23, 315 (2023). https://doi.org/10.1186/s12872-023-03346-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03346-0