Abstract
Background
There is a paucity of information about the clinical features and angiographic findings in young patients with acute myocardial infarction (MI), especially in the Arab Peninsula countries.
Objective
The aim of this study was to assess the proposed risk factors, clinical presentation, and angiographic findings of acute myocardial infarction in young adults.
Methods
This prospective study included young (range, 18 to 45 years) patients who presented with acute MI based on clinical evaluation, laboratory investigation, and electrocardiogram, and they underwent a coronary angiography procedure.
Key findings
Data of 109 patients with a diagnosis of acute MI were collected. Patients’ mean age was 39.98 ± 7.52 years (range, 31 to 45 years), and 92.7% (101) were male. Smoking was the highest risk factor in 67% of patients, obesity and overweight in 66%, sedentary lifestyle in 64%, dyslipidaemia in 33%, and hypertension in 28%. Smoking was the most common risk factor for acute MI in males (p = 0.009), whereas sedentary lifestyle was the most common risk factor in females (p = 0.028). Chest pain typical of acute MI was the most common presenting symptom in 96% of patients (p < 0.001). On admission, 96% of patients were conscious, and 95% were oriented. On angiography, the left anterior descending artery (LAD) was affected in 57%, the right coronary artery (RCA) was affected in 42%, and the left circumflex artery (LCX) was affected in 32% of patients. The LAD was severely affected in 44%, the RCA was severely affected in 25.7%, and the LCX was severely affected in 19.26% of patients (p < 0.001).
Conclusion
Smoking, obesity, sedentary lifestyle, dyslipidaemia, and hypertension were the most common risk factors for acute MI. Smoking was the most common risk factor in males and sedentary lifestyle in females. The LAD was the most commonly affected coronary artery, followed by the RCA and LCX arteries, with the same order for severity of stenosis.
Similar content being viewed by others
Introduction
Myocardial infarction (MI) is defined as a myocardial injury that involves cell death due to prolonged ischemia as a result of an imbalance between the oxygen (O2) supply and demand of the myocardial wall. Acute MI occurs mostly due to insufficient blood flow to the myocardial tissue caused by atherothrombotic coronary artery disease (CAD), coronary artery embolism, and coronary spasm, as well as sustained tachyarrhythmias, severe blood loss, severe anaemia, or respiratory failure [1]. Acute MI is a common disease and remains a leading cause of morbidity and mortality worldwide. Although MI is a disease of old age, recent studies found that the incidence of MI is 12.9 and 38.2 per 1,000 in males and 2.2 and 5.2 per 1,000 in females in the age groups of 30–34 and 35–44 years, respectively [2]. Diabetes mellitus (DM), depression, hypertension, smoking, a family history of MI, low household income, hypercholesterolemia, obesity, sedentary life, previous MI, and previous percutaneous coronary intervention (PCI) are the risk factors of acute MI in young male and female patients [2, 3].
Diagnosis of acute MI can be made based on clinical presentation, cardiac biomarkers, and electrocardiogram (ECG). In young adults, a clinical presentation of acute MI is similar to that of older patients, and most patients present with chest pain. Due to a lower suspicion of acute MI and atypical presentation in some patients, there is more likely to be a delay in diagnosis of acute MI in young adults [4, 5]. Cardiac troponin I (cTnI) and cardiac troponin T (cTnT) are components of the contractile apparatus of myocardial cells, which are expressed almost exclusively in the heart. Elevated cTnI values occur exclusively in an injury to cardiac tissues. Both cTnI and cTnT are the preferred biomarkers for evaluation of myocardial injury and are recommended for routine use [6].
ECG is a pivotal tool in the diagnosis of acute MI, and it can be used to determine the presence, location, and extent of MI in acute coronary occlusion. ECG manifestations that suggest acute MI, in the absence of left ventricular hypertrophy or bundle branch block, are as follows: (1) ST elevation, which is the presence of new ST elevation at the J-point in two contiguous leads with the cut-point of 1 mm in all leads other than leads V2–V3, where the following cut-points apply: > 2 mm in males > 40 years, > 2.5 mm in males < 40 years, or > 1.5 mm in females regardless of age; (2) ST depression and T-wave changes: the presence of new horizontal or down-sloping ST depression > 0.5 mm in two contiguous leads and/or T inversion > 1 mm in two contiguous leads with prominent R wave or R/S ratio > 1 [6, 7].
Acute MI occurs after critical or total occlusion of the coronary arteries, mostly due to thrombosis or atherosclerotic plaque rupture or erosion, and manifests with a similar clinical presentation. However, determining acute MI type and understanding the similarities and differences between ST-elevation MI (STEMI) and non-ST-elevation MI (NSTEMI) is an essential step for proper management [8]. STEMI is defined as acute coronary thrombosis or persistent ST-segment elevation of ≥ 1 mm in ≥ 2 contiguous ECG leads. NSTEMI is defined as ischemic symptoms at rest, lasting ≥ 10 min, which arises from an acute coronary plaque rupture or erosion, occurring within 24 h before hospital admission and displaying either elevated creatinine kinase or cardiac troponin (cTn) cardiac biomarkers within 24 h of the initial clinical presentation [9].
Despite the relatively low prevalence of acute MI in young adults, the potential of death and long-term disability makes it a highly significant clinical problem. In the literature, there is a paucity of information about the clinical features and angiographic findings in young patients with acute MI, especially in the Arab Peninsula countries. The aim of this study was to assess the proposed risk factors, clinical presentation, and angiographic findings of acute MI in young adults, who were defined as patients under 45 years old. The significance of this study lies in highlighting the significant proportion of acute MI patients with modifiable risk factors who could benefit from more intensive prevention strategies.
Patients and methods
Study design
This observational prospective study was conducted from November 2021 to September 2022 at Prince Mohammed bin Nasser Hospital (PMBNH) Cardiac Center in Jazan Region, Southern Province, of Kingdom of Saudi Arabia (KSA). Patients presented or referred to the centre underwent clinical evaluation, laboratory investigation of cardiac biomarkers, ECG, echocardiogram (echo), and coronary angiography for diagnostic and therapeutic purposes. The data of these patients were collected for this study, and the inclusion criteria were the following: each young patient who presented to PMBNH, Jazan, with acute MI, either STEMI or NSTEMI, and for whom informed consent was obtained to enrol in this study.
Exclusion criteria were as follows: patients with acute MI older than 45 years old, patients with acute MI younger than 18 years old, and patients with other heart diseases. Patients’ information on clinical presentation, risk factors, ECG changes, echo, and angiographic findings were collected by using a questionnaire filled out for each patient.
Diagnosis of MI
In this study, patients were diagnosed with MI based on clinical symptoms, signs, ECG findings, and cardiac biomarker values, and they underwent coronary angiography with possible PCI at the same centre.
Statistical analysis
The collected data were analysed using the Statistical Package for Social Sciences (SPSS) (IBM Corp., Armonk, NY, USA). Categorical variables were reported as numbers and percentages, and continuous variables were reported as means ± standard deviation. A binomial test was used to present the variables. Binary logistic regression was performed to determine the correlation between acute MI and the proposed risk factors. The receiver operator characteristic (ROC) curve was applied to study the sensitivity and specificity of clinical presentation to diagnose acute MI.
Results
For this study, the data of 109 young patients with a diagnosis of acute MI were collected. Patients’ mean age was 39.98 ± 7.52 years (range, 31 to 45 years); 92.7% (101) were male, and 7.3% (8) were female. The sociodemographic data of the enrolled patients in this study are provided in Table 1.
Smoking was a risk factor in 67% of patients, obesity and overweight in 66%, sedentary lifestyle in 64%, dyslipidaemia in 33%, hypertension in 28%, family history of CAD in 14%, previous history of MI in 6%, and history of previous PCI in 4% (Table 2).
Chest pain typical of MI was the presenting symptom in 96% of patients (OR = 8.634, 95% CI 1.047–71.218), followed by shortness of breath (45%), atypical pain (8%), cardiac arrest (4%), syncope (3%), and palpitation (2%) (Table 3).
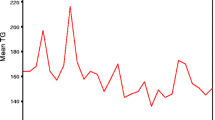
The ROC curve shows significant sensitivity for typical chest pain as a presentation of acute MI (area under the curve [AUC] = 0.681). However, it reveals low sensitivity for shortness of breath as a presentation of acute MI (AUC < 0.5) (Fig. 1).
On admission, 96% of patients were conscious, 95% were oriented, and 74% of cases were diagnosed with STEMI. However, mechanical ventilation, focal neurological signs, congestive heart failure (CHF), rales and high jugular venous pressure, and cardiogenic shock were rarely present (Table 4).
Our study showed that STEMI was the most common type of acute MI, and the most common type of STEMI was anterior (34.86%), followed by inferior (25.7%) (Table 5).
On the angiography, the LAD was affected in 57% of patients, the RCA was affected in 42% of patients, the LCX was affected in 32% of patients, and other arteries were less likely to be affected (p < 0.001) (Table 6, Fig. 2).
Angiographic images of a) a 41-year-old male patient presenting with acute anterior myocardial infarction (MI), with the images showing total occlusion of the proximal left anterior descending artery (LAD) (arrow) and, a +) after percutaneous coronary intervention (PCI), large LAD (arrow) that was occluded; b) a 42-year-old man presenting with posterior MI, with the coronary angiogram showing total occlusion of the left circumflex artery (LCX) (arrow) and b +) the left coronary angiogram after PCI showing patent LCX (arrow); c) a 38-year-old man presenting with non-ST elevation MI (NSTEMI), with the right coronary angiogram showing 80% stenosis in the mid-right coronary artery (RCA) (arrow) and c +) the right coronary angiogram after PCI showing complete resolution of the mid RCA stenosis (arrow)
On the angiography, the LAD was severely affected in 44% of patients, the RCA was severely affected in 25.7% of patients, and the LCX was severely affected in 19.26% of patients (p < 0.001) (Table 7).
Table 8 shows that 33.9% of PCIs were routine, 22.9% were primary, and 19.3% were rescue (p = 0.044).
Discussion
Acute MI occurs primarily in older patients. However, young adults can be affected, which constitutes an important diagnostic problem for physicians. Many previous studies have used 40 to 45 years as an age cut-off to define young patients with acute MI [4]. In this study, we used 45 years old as a cut-off to define young patients, and we collected the data of 109 patients diagnosed with acute MI who underwent diagnostic coronary angiography and possible PCI. We found that 93% of the affected patients were male. This result is in line with Bhardwaj et al., who reported that young adult acute MI occurs almost exclusively in males [10]. The low incidence of acute MI in young premenopausal females is related to the positive effect of female hormones on the patient’s lipid profile, vascular activity, and vascular endothelial function [11]. Another previous study reported that there are sex differences in risk factors for MI, and females who have MI are often postmenopausal [12]. In their previous cohort study on thousands of participants, Millet et al. reported that sex-specific associations between MI and risk factors declines with age, and the incidence of MI in females tends to be similar to that in males [13].
Regarding risk factors, the American Heart Association (AHA), in conjunction with the National Institute of Health (NIH) statistics related to heart disease, stroke, and cardiovascular disease (CVD) risk factors, reported a sharp increase in electronic cigarette use among adolescents between 2011 and 2020. Persons who are physically active are at a 25–40% lower risk of CVD mortality. Daily intake of 5 (versus 2) servings of fruit and vegetables is associated with 13% lower total mortality and 12% lower total CVD mortality. Higher intake of total fat and unsaturated fatty acids is associated with lower total mortality. Risk of ischemic stroke increases consistently with metabolic syndrome severity. The death rate attributable to high blood pressure increased 34.2% from 2009 to 2019 [14]. Our results indicated that smoking, obesity and overweight, and a sedentary lifestyle are highly significant risk factors for acute MI. This result is in line with Rathore et al., who reported that smoking is a strong risk factor for acute MI, increased body mass index is directly related to increased incidence of acute MI, and physical activity may contribute to reducing risk of CAD by 20–30% [15].
Our study indicated a significant association between MI and male smoker patients and a significant association between MI and female patients with a sedentary lifestyle. Similar to our study, Azab et al. reported that smoking is the second most significant risk factor in male patients, and hypertriglyceridemia is the second most significant risk factor in females [16]. Nyström et al. reported that hyperlipidaemia was the only traditional risk factor more frequent among females than males [17]. In contrast to our results, Ilic et al. reported that risk of acute MI increases with obesity and stressful life in male patients and with DM and menopause in female patients [12]. We explain that the discrepancy in risk factors associated with gender is attributed to the difference in habits in different societies and areas around the world. In their previous study, Nyström et al. reported that social factors, such as serious life events, strained economy, stress, depression, and sleep deprivation, were stronger potential risk factors for acute MI among females than among males [17]. In their previous case control study, Lu et al. reported that potential modifiable risk factors including DM, depression, hypertension, current smoking, low household income, and hypercholesterolemia accounted for 85% of the risk of acute MI in young adult male and female patients [18]. These risk factors can be controlled to decrease the incidence of acute MI in young adults.
The current study shows that typical chest pain is the predominant presenting symptom of acute MI. The ROC curve revealed that chest pain is the only reliable presenting symptom of acute MI. This result is consistent with several previous studies, including Nyström et al., who reported that the dominant prodromal symptom of acute MI is chest pain in both males and females [17]. Ferry et al. also reported that chest pain was the most common presenting symptom in both females and males (approximately 93%) diagnosed with type-1 MI [19]. Malik et al. reported that chest pain is the most common presenting complaint of acute MI, and it is classically described as a heavy chest pressure or squeezing, a burning feeling, or difficulty breathing. The pain often radiates to the left shoulder, neck, or arm. However, acute MI pain may be atypical and cause an overlap in cardiac as well as non-cardiac pain, which requires a vigilant history evaluation of chest pain parameters to overcome this dilemma [20]. In the current study, typical chest pain, shortness of breath (SOB), and epigastric/shoulder/back/neck pain were the three most common symptoms of acute MI. These symptoms are consistent to some extent, especially the first symptom, with those reported in a previous study conducted by Mahajan et al., who reported that chest pain or discomfort, SOB, and pain or discomfort in arms or shoulders were the most common presenting symptoms of acute MI, with 91.8%, 87%, and 85.7%, respectively [21].
In our study, all enrolled patients were primarily diagnosed with acute MI using clinical features, ECG, and cTn, especially troponin I. In addition to presenting clinical features, ECG is an important non-invasive diagnostic tool for patients with acute MI [22], with 95–97% specificity for diagnosis of MI [23]. Current guidelines recommend serial ECGs for persisting symptoms [22], which can increase ECG sensitivity [23]. Due to the fact that cardiac troponin is the laboratory biomarker of choice for detection of cardiac injury [24], troponin I, which is highly sensitive to exclude acute MI [25], was used to confirm the diagnosis of acute MI in all patients of the current study. Diagnoses of acute MI were made based on the facts reported in previous studies that strategies using a single troponin I measured with a high-sensitivity assay on admission, combined with a normal or low-risk ECG, can safely rule out acute MI [26, 27]. Furthermore, echo is a highly valuable tool in establishing the diagnosis of acute MI, and it gives substantial information regarding risk stratification, detection, and follow-up mechanical complications of acute MI [28]. Echo can generate images of the inside and outside of the heart and is used to assess cardiac wall motion, valve abnormalities, ischemic mitral regurgitation, and cardiac tamponade [23]. In the current study, echo provides good information about wall movements and ejection fraction in most patients of the study.
Ultimately, definitive acute MI requires coronary catheterization, which monitors both blockage and flow of blood through the coronary arteries and serves both diagnostic and therapeutic purposes. All of the patients in our study were undergoing coronary catheterization. The LAD, which is the largest branch of the left main coronary artery and carries oxygenated blood to the left side of the heart, was the most commonly affected, followed by the RCA then LCX. This result is consistent with a previous study conducted by Ahmed et al., who reported that the LAD is the most commonly affected in both STEMI and NSTEMI [29]. The significance of the LAD, RCA, and LCX lie in the fact that they are the three largest coronary arteries [30]. Occlusion of the LAD may cause ischemia in the anterior wall of the left ventricle (LV) and manifests as precordial ST-segment elevation on ECG [31]. Occlusion of the RCA may cause ischemia of the inferior wall of the LV with or without the right ventricle and manifests as ST-segment elevation in inferior wall leads (II, III, and aVF) [32, 33]; however, it is exceptional to show ST-segment elevation in V1 to V3 [33]. Occlusion of the LCX or one of its branches may cause lateral wall infarction [34], which may manifest as ST-segment elevation in I and aVL [35]. ECG can determine the culprit occluded artery with high sensitivity and acceptable specificity [36]. However, diagnostic angiography is still the cornerstone in determining the affected arteries and the extent and percentage of occlusion, as well as providing a chart for interventional therapy.
Limitations
This study is limited in that it included a small sample size. The prevalence of other significant suspected risk factors, such as serious life events, the strained economy, stress, depression, and sleep deprivation, were not involved in this study because we could not get such information from the patients, and no accurate medical records about them were available in our region.
Conclusion
In this study, smoking, obesity, sedentary life, dyslipidaemia, and hypertension were the most common risk factors of acute MI, with a significant association of acute MI with male gender and khat chewing. Smoking was the most common risk factor in males and sedentary lifestyle in females. Acute MI patients were almost always conscious and oriented on presentation. LAD, followed by RCA and LCX, was the most commonly affected coronary artery, with the same order in severity of stenosis.
Availability of data and material
The datasets used/or generated during the current study are available from the corresponding author on reasonable request.
References:
Lodrini AM, Goumans MJ. Cardiomyocytes Cellular Phenotypes After Myocardial Infarction. Front Cardiovasc Med. 2021; 8:750510. https://doi.org/10.3389/fcvm.2021.750510.
Lu Y, Li SX, Liu Y, Rodriguez F, Watson KE, Dreyer RP, Khera R, Murugiah K, D'Onofrio G, Spatz ES, Nasir K, Masoudi FA, Krumholz HM. Sex-Specific Risk Factors Associated With First Acute Myocardial Infarction in Young Adults. JAMA Netw Open. 2022;5(5):e229953. https://doi.org/10.1001/jamanetworkopen.2022.9953.
Zasada W, Bobrowska B, Plens K, Dziewierz A, Siudak Z, Surdacki A, Dudek D, Bartuś S. Acute myocardial infarction in young patients. Kardiol Pol. 2021;79(10):1093–8. https://doi.org/10.33963/KP.a2021.0099.
Gulati R, Behfar A, Narula J, Kanwar A, Lerman A, Cooper L, Singh M. Acute Myocardial Infarction in Young Individuals. Mayo Clin Proc. 2020;95(1):136–56. https://doi.org/10.1016/j.mayocp.2019.05.001.
Safdar B, et al. Clues to Diagnose Myocardial Infarction in the Young. J Am Coll Cardiol. 2019;73(5):585–8. https://doi.org/10.1016/j.jacc.2018.11.034.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–2264. https://doi.org/10.1016/j.jacc.2018.08.1038.
Kashou AH, Basit H, Malik A. ST Segment. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459364/
Mitsis A, Gragnano F. Myocardial Infarction with and without ST-segment Elevation: a Contemporary Reappraisal of Similarities and Differences. Curr Cardiol Rev. 2021;17(4):e230421189013. https://doi.org/10.2174/1573403X16999201210195702.
Hilliard AL, Winchester DE, Russell TD, Hilliard RD. Myocardial infarction classification and its implications on measures of cardiovascular outcomes, quality, and racial/ethnic disparities. Clin Cardiol. 2020;43(10):1076–83. https://doi.org/10.1002/clc.23431.
Bhardwaj R, Kandoria A, Sharma R. Myocardial infarction in young adults-risk factors and pattern of coronary artery involvement. Niger Med J. 2014;55(1):44–7. https://doi.org/10.4103/0300-1652.128161.
Albrektsen G, Heuch I, Løchen ML, Thelle DS, Wilsgaard T, Njølstad I, Bønaa KH. Lifelong Gender Gap in Risk of Incident Myocardial Infarction: The Tromsø Study. JAMA Intern Med. 2016;176(11):1673–9. https://doi.org/10.1001/jamainternmed.2016.5451.
Ilic I, Ilic M. Risk Factors for Myocardial Infarction in Women and Men: A Case-Control Study. Biol Life Sci Forum. 2021;9:13. https://doi.org/10.3390/ECCM-10876.
Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ. 2018;363: k4247. https://doi.org/10.1136/bmj.
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Ferguson JF, Generoso G, Ho JE, Kalani R, Khan SS, Kissela BM, Knutson KL, Levine DA, Lewis TT, Liu J, Loop MS, Ma J, Mussolino ME, Navaneethan SD, Perak AM, Poudel R, Rezk-Hanna M, Roth GA, Schroeder EB, Shah SH, Thacker EL, VanWagner LB, Virani SS, Voecks JH, Wang NY, Yaffe K, Martin SS. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145(8):e153-e639. https://doi.org/10.1161/CIR.0000000000001052. Epub 2022 Jan 26. Erratum in: Circulation. 2022 Sep 6;146(10):e141. PMID: 35078371.
Rathore V, Singh N, Mahat RK. Risk Factors for Acute Myocardial Infarction: A Review. EJMI. 2018;2(1):1–7. https://doi.org/10.14744/ejmi.2018.76486.
Azab AE, Elsayed ASI. Acute myocardial infarction risk factors and correlation of its markers with serum lipids. J Appl Biotechnol Bioeng. 2017;3(4):385–91. https://doi.org/10.15406/jabb.2017.03.00075.
Nyström A, Strömberg S, Jansson K, Faresjö ÅO, Faresjö T. Cardiovascular risks before myocardial infarction differences between men and women. BMC Cardiovasc Disord. 2022;22(1):110. https://doi.org/10.1186/s12872-022-02555-3.
Lu Y, Li SX, Liu Y, Rodriguez F, Watson KE, Dreyer RP, Khera R, Murugiah K, D'Onofrio G, Spatz ES, Nasir K, Masoudi FA, Krumholz HM. Sex-Specific Risk Factors Associated With First Acute Myocardial Infarction in Young Adults. JAMA Netw Open. 2022;5(5):e229953. https://doi.org/10.1001/jamanetworkopen.2022.9953.
Ferry AV, Anand A, Strachan FE, Mooney L, Stewart SD, Marshall L, Chapman AR, Lee KK, Jones S, Orme K, Shah ASV, Mills NL. Presenting Symptoms in Men and Women Diagnosed With Myocardial Infarction Using Sex-Specific Criteria. J Am Heart Assoc. 2019 Sep 3;8(17):e012307. https://doi.org/10.1161/JAHA.119.012307.
Malik MA, Alam Khan S, Safdar S, Taseer IU. Chest Pain as a presenting complaint in patients with acute myocardial infarction (AMI). Pak J Med Sci. 2013;29(2):565–8. https://doi.org/10.12669/pjms.292.2921.
Mahajan S, Valero-Elizondo J, Khera R, Desai NR, Blankstein R, Blaha MJ, Virani SS, Kash BA, Zoghbi WA, Krumholz HM, Nasir K. Variation and Disparities in Awareness of Myocardial Infarction Symptoms Among Adults in the United States. JAMA Netw Open. 2019;2(12):e1917885. https://doi.org/10.1001/jamanetworkopen.2019.17885.
Lehmacher J, Neumann JT, Sörensen NA, Goßling A, Haller PM, Hartikainen TS, Clemmensen P, Zeller T, Blankenberg S, Westermann D. Predictive Value of Serial ECGs in Patients with Suspected Myocardial Infarction. J Clin Med. 2020;9(7):2303. https://doi.org/10.3390/jcm9072303.
Mechanic OJ, Gavin M, Grossman SA. Acute Myocardial Infarction. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459269/. [Updated 2022 Aug 8].
Babuin L, Jaffe AS. Troponin: the biomarker of choice for the detection of cardiac injury. CMAJ. 2005 Nov 8;173(10):1191-202. doi: https://doi.org/10.1503/cmaj/051291. Erratum in: CMAJ. 2005 Dec 6;173(12):1490. Erratum in: CMAJ. 2006;174(3):353.
Chapman AR, Mills NL. High-sensitivity cardiac troponin and the early rule out of myocardial infarction: time for action. Heart. 2020;106(13):955–7. https://doi.org/10.1136/heartjnl-2020-316811.
Sandoval Y, Smith SW, Love SA, Sexter A, Schulz K, Apple FS. Single High-Sensitivity Cardiac Troponin I to Rule Out Acute Myocardial Infarction. Am J Med. 2017;130(9):1076-1083.e1. https://doi.org/10.1016/j.amjmed.2017.02.032.
Neumann JT, Sörensen NA, Ojeda F, Schwemer T, Lehmacher J, Gönner S, Jarsetz N, Keller T, Schaefer S, Renné T, Landmesser U, Clemmensen P, Makarova N, Schnabel RB, Zeller T, Karakas M, Pickering JW, Than M, Parsonage W, Greenslade J, Cullen L, Westermann D, Blankenberg S. Immediate Rule-Out of Acute Myocardial Infarction Using Electrocardiogram and Baseline High-Sensitivity Troponin I. Clin Chem. 2017;63(1):394–402. https://doi.org/10.1373/clinchem.2016.262659.
Sia YT, O’Meara E, Ducharme A. Role of echocardiography in acute myocardial infarction. Curr Heart Fail Rep. 2008;5(4):189–96. https://doi.org/10.1007/s11897-008-0029-6.
Ahmed IAM, Khalid NHM, Abd-Elmagid AEM, Abdullah MAM, Musa AMI, Al-Qarni NO. Common coronary artery occlusions in patients with myocardial infarction. Pan Afr Med J. 2022;42:254. https://doi.org/10.11604/pamj.2022.42.254.34762.
Nordlund D, Heiberg E, Carlsson M, Fründ ET, Hoffmann P, Koul S, Atar D, Aletras AH, Erlinge D, Engblom H, Arheden H. Extent of Myocardium at Risk for Left Anterior Descending Artery, Right Coronary Artery, and Left Circumflex Artery Occlusion Depicted by Contrast-Enhanced Steady State Free Precession and T2-Weighted Short Tau Inversion Recovery Magnetic Resonance Imaging. Circ Cardiovasc Imaging. 2016;9(7):e004376. https://doi.org/10.1161/CIRCIMAGING.115.004376.
Honda T, Fujimoto K, Miyao Y, Koga H, Ishii M. Acute myocardial infarction caused by left anterior descending artery occlusion presenting as inferior ST elevation and anterior ST depression. J Cardiol Cases. 2013;9(2):67–70. https://doi.org/10.1016/j.jccase.2013.10.003.
Zheng J, Lin J, Shen N, Qu B. Proximal complete occlusion of right coronary artery presenting with precordial ST-segment elevation: A case report. Medicine (Baltimore). 2016;95(41):e5113. https://doi.org/10.1097/MD.0000000000005113.
Kim SE, Lee JH, Park DG, Han KR, Oh DJ. Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography. Korean Circ J. 2010;40(10):536–8. https://doi.org/10.4070/kcj.2010.40.10.536.
Ludhwani D, Chhabra L, Goyal A, et al. Lateral Wall Myocardial Infarction. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 .Available from: https://www.ncbi.nlm.nih.gov/books/NBK537228/. [Updated 2022 Sep 12].
Rafla S, Kamal A. Localization of the occluded vessel in acute myocardial infarction. J Cardiol Cardiovasc Med. 2020;5:029–33. https://doi.org/10.29328/journal.jccm.1001082.
Daly M, Finlay D, Guldenring D, Nugent C, Tomlin A, Smith B, Adgey A, Harbinson M. Detection of acute coronary occlusion in patients with acute coronary syndromes presenting with isolated ST-segment depression. Eur Heart J Acute Cardiovasc Care. 2012;1(2):128–35. https://doi.org/10.1177/2048872612448977.
Acknowledgements
The authors would like to thank Dr Ahmed A. Babikr for his help in data collection. The authors also would like to thank Scribendi.com for their effort in language editing
Funding
The authors state that this work has not receive any funding.
Author information
Authors and Affiliations
Contributions
K.H.H. conceived the study, provided some cases of angiographic procedures, and performed data collection; S.A.A. conducted data analysis and wrote the article; I.A.A. interpreted the data; M.G., and O.M.A. and A.G. revised the data analysis; W.M.A. and F.H.A. edited the language and revised the article; A.A.Q., K.M.A., and A.I.S. performed final revision of the article. All authors have read and agreed with the published version of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by IRB of the Jazan Health Ethics Committee, Ministry of Health, Saudi Arabia (No. 2206). Informed consent was taken from each of the participants in ethics approval and Consent to Participant in Declaration.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Ethics approval and consent to participate section.
Consent for publication
This study was approved by the IRB of the Jazan Health Ethics Committee, Ministry of Health, Saudi Arabia (No. 2206).
Competing interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haider, K.H., Alshoabi, S.A., Alharbi, I.A. et al. Clinical presentation and angiographic findings of acute myocardial infarction in young adults in Jazan region. BMC Cardiovasc Disord 23, 302 (2023). https://doi.org/10.1186/s12872-023-03335-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03335-3