Abstract
Background
Left atrial appendage (LAA) is the origin of most heart thrombi which can lead to stroke or other cerebrovascular event in patients with non-valvular atrial fibrillation (AF). This study aimed to prove safety and low complication rate of surgical LAA amputation using cut and sew technique with control of its effectiveness.
Methods
303 patients who have undergone selective LAA amputation were enrolled in the study in a period from 10/17 to 08/20. The LAA amputation was performed concomitant to routine cardiac surgery on cardiopulmonary bypass with cardiac arrest with or without previous history of AF. The operative and clinical data were evaluated. Extent of LAA amputation was examined intraoperatively by transoesophageal echocardiography (TEE). Six months in follow up, the patients were controlled regarding clinical status and episodes of strokes.
Results
Average age of study population was 69.9 ± 19.2 and 81.9% of patients were male. In only three patients was residual stump after LAA amputation larger than 1 cm with average stump size 0.28 ± 0.34 cm. 3 patients (1%) developed postoperative bleeding. Postoperatively 77 (25.4%) patients developed postoperative AF (POAF), of which 29 (9.6%) still had AF at discharge. On 6 months follow up only 5 patients had NYHA class III and 1 NYHA class IV. Seven patients reported with leg oedema and no patient experienced any cerebrovascular event in early postoperative follow up.
Conclusion
LAA amputation can be performed safely and completely leaving minimal to no LAA residual stump.
Similar content being viewed by others
Introduction
The left atrial appendage (LAA) is a protuberance of the left atrium, which represents a 2–4 cm large, tubular structure that has a narrow connection to the left atrium and rests against the free wall of the left ventricle [1]. The use of transoesophageal echocardiography has made clear imaging of the LAA possible, so that its size, shape, flow patterns, and content can be assessed in health and disease. The LAA normally has a pulsatile blood flow in the sinus rhythm, whereby stasis and thus clot formation are prevented [2]. If necessary, clot formation can be detected using transoesophageal echocardiography (TEE) [1].
Atrial fibrillation (AF) is the most common abnormal heart rhythm (arrhythmia) caused by disorganized atrial depolarizations without effective atrial contraction and irregular AV conduction [3]. Its occurrence after cardiac surgery is common with prevalence of 10–65% associated with higher risk of mortality [4]. Although paroxysmal AF after cardiac surgery is often self-limiting [5], many patients after cardiac surgery with recurrent AF without suitable anti-coagulation remain at risk for stroke [6]. Left atrial appendage can be ligated or amputated as part of ablation procedure for atrial amputation or oversewn from inside as concomitant procedure during mitral valve surgery [7]. In the recent years the interest in LAA increased and led to larger number of different LAA occlusion devices, endocardial and epicardial which as such lead to further increase of operational costs [8].
Despite the fact that 90% of thrombi in non-valvular AF and 60% in valvular AF develop in the LAA, and being on site during open heart surgery it still has not become routine part of surgical prophylaxis during most of cardiac surgery procedures [9]. Most surgeons avoid LAA amputation, if atrial ablation is not planed due to risk of bleeding, risk of injury to circumflex artery and concerns for hemodynamic consequences as natriuretic hormones are primarily produced in LAA [10].
In this study we explored the safety and invasiveness of LAA amputation and its completeness as concomitant procedure during routine open-heart surgery.
Patients and methods
Study design and patients
We identified total of 303 patients between 10/17 and 12/20 who had LAA amputation performed. After institutional ethics review committee approval all the patients presenting for routine cardiac surgery were screened for eligibility and assigned for concomitant LAA amputation. The reason is that the resection of the LAA is part of SEIDC trial performed in our institution with prospective patient inclusion and all the surgeons followed this protocol. We analysed the patients enrolled in trial regarding the clinical aspects and consequences of LAA amputation [11,12,13]. The study was approved by the University Hospital ethics committee (IRB approval: 143/17-sc 6.10.2017). The inclusion and exclusion criteria for the study are as follows: patients undergoing routine open-heart surgery for the first time were included, while patients with a history of previous cardiac surgery or severe adhesions were excluded. Both, patients with history of AF and those signed for non-atrial fibrillation cardiac surgery were included. All patients gave informed consent.
Operative technique
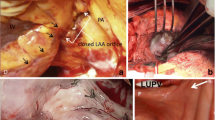
After placing the patient under general anaesthesia and performing median sternotomy patient was placed on cardiopulmonary bypass. Concomitant to planed cardiac surgery procedure LAA amputation was performed with cardioplegic arrest at a convenient time during the operation at the operating surgeon’s discretion. Amputation is performed under direct visualization provided by heart luxation and its effectiveness is controlled and confirmed using intraoperative transoesophageal echocardiography. LAA is excided direct at the basis and oversewn using a double-layered technique with 4 − 0 polypropylene suture. Meticulous inspection for remnants of bleeding is required and pledgeted-reinforced extra 4 − 0 Prolene stitch was placed if necessary. Fibrin sealant Tisseel (Baxter Healthcare Corp., Deerfield, IL) was used at surgeon´s discretion to cover the suture line.
Postoperative care and outcome variables
All patients were admitted to surgical intensive care unit and monitored with continuous telemetry. ECG telemetry was kept during the whole hospital stay until to discharge. 12-lead ECG was obtained directly after operation and at discharge. Postoperative atrial fibrillation (POAF) was defined as AF occurring after operation during the hospitalization time with no previous history of AF. If occurred, AF was treated with rate control, antiarrhythmic drug therapy (almost exclusively amiodaron therapy), or electric cardioversion if the medical therapy alone failed. Anticoagulation was initiated in patients with POAF persisting for > 48 h.
All patients received a routine preoperative echocardiographic examination (Philips Epiq 7, Philips Health System, Hamburg, Germany). Measurements and analysis were performed by trained echocardiography technician and board-certified cardiothoracic attending surgeon blinded to patients and in accordance with the standardized echocardiography protocol and the American Society of Echocardiography.
Transthoracic echocardiography was performed at admission and before discharge. Transoesophageal echocardiography was performed as standard procedure during each surgery. Measurements and analysis were performed by trained and by German Society for Anaesthesiology and Intensive Care Medicine certified attending anaesthesiologist and in accordance with the standardized echocardiography protocol. The primary outcome variable was completeness of amputation (residual stump < 1 cm) which was controlled directly after discontinuation of cardiopulmonary bypass using transoesophageal echocardiography and bleeding complications. Further on, we investigated incidence of postoperative cerebrovascular events (CVEs); this included transient ischemic attack. Secondary variables were incidence of myocardial infarction, deterioration of renal function, changes in echocardiographic measurements.
At 6 months follow up the patients were interviewed regarding CVEs, NYHA status and signs of volume overload (legs oedema).
Statistical analysis
Continuous variables are presented as mean and standard deviation and categorical variables as numbers with percentage. The normality of the continuous variables was assessed with the Shapiro-Wilk test. The preoperative and postoperative data were compared using t-test for parametric and Wilcoxon’s signed-rank sum test for non-parametric data; and categorical variables are compared using the chi-square or the Fisher’s exact test. A P value of < 0.05 was considered significant. All statistics were performed using SPSS software (IBM SPSS Statistics for Windows, Version 23.0, IBM Corp., Armonk, NY, USA).
Results
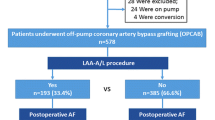
A total of 303 patients had LAA amputation performed concomitant to routine cardiac surgery procedure. Table 1. describes the preoperative and demographic data. Most of the patients included in the study were males 249 (81.9%), and average patient was 69.9 ± 19.2 years old. As described surgical operative time was 114.4 ± 38.9 min. on cardio-pulmonary bypass and 82.2 ± 27.7 min cross clamp time as all procedures were performed on cardioplegic arrested hearts. The procedure most often performed was aortocoronary bypass 286 (94.4%). Surgical ablation or maze procedure was performed in 40 (13.2%) patients, although preoperative AF was present in 72 patients (23.7%) and only 1 (0.3%) patient had left atrial appendage thrombus. On admission 29 (9.5%) patient had history of stroke and 14 (4.6%) history of TIA, whereas carotid artery stenosis was present in 47 (15.5%) patients. 120 (39.5%) of patients reported NYHA class III or IV at admission and euroscore II was 3.09 ± 12.11. The mean CHA2DS2-VASc score was 3.43 ± 1.63, with 213 males having a score higher than 1 and 50 females having a score higher than 2. The mean HAS-BLED score was 3.29 ± 0.99, with 65 patients having a score between 0 and 2 and 238 patients having a score higher than 2 as shown in Table 1.
In our study, there were three patients requiring reoperation and only one patient who required acute reoperation due to bleeding from LAA stump. No deaths or strokes were reported during the postoperative course. Regarding postoperative data as shown in Table 2. we detected POAF in 77 (25.4%) patients of which total of 29 (9.6%) were discharged with AF. Postoperative bleeding occurred in 3 (1%) patients and only in one case (0.33%) it was connected to LAA amputation. In this 81 year old patient repeated cross clamping was needed and tear was repaired with two pericardial strips. There were no patients with postoperative ECG signs of myocardial ischemia and average postoperative CK-MB was 59.5 ± 37.9 U/l.
After LAA amputation was performed and cardiopulmonary bypass disconnected a final check of residual stump was performed and measured as shown in Fig. 1. In our patient group we identified 3 (1%) patients with LAA residual stump larger than 1 cm, with average stump size 0.28 ± 0.34 cm.
At 6 months follow up only 6 (1.9%) patients reported NYHA class III or IV, of which only one patient still in NYHA class IV. Seven patients (2.3%) had leg oedema and not one patient experienced cerebrovascular event during the first 6 months after surgery. In our study, 15 patients (4.9%) were on NOAC and 51 (16.8%) were on OAC according to standard practice at our institution. Specifically, patients were started on anticoagulation with heparin during the procedure, followed by oral anticoagulation with warfarin or DOACs postoperatively.
In Fig. 2. we showed changes in renal function before and after surgery. We noticed slight reduction in GFR (72.28 ± 23.22 vs. 69.63 ± 24.52 mL/min/1.73m2, p = 0.02) and increase in serum creatine levels (1.18 ± 0.73 vs. 1.25 ± 0.67 mg/dl, p = 0.113).
Further on we analysed perioperative changes in transthoracic echocardiography which are listed in Table 3. Stroke volume reduced after surgery (92.4 ± 23.5 vs. 78.5 ± 19.5 ml, p = 0.000), while EF remained almost constant (49.9 ± 17.1 vs. 48.9 ± 11.3%, p = 0.113). TAPSE was significantly reduced after performed surgery (22.8 ± 4.5 vs. 14.4 ± 2.8 mm, p = 0.000). Most of the patients had mild degree of diastolic dysfunction already preoperatively with E/A ratio 0.98 ± 0.69 vs. 1.38 ± 0.73 (p = 0.000) and E/e´ 12.9 ± 7.9 vs. 13.1 ± 5.1 (p = 0.101). sPAP values remained in normal or slightly increased range (30.9 ± 11.4 vs. 28.7 ± 8.2 mmHg; p = 0.288). We noticed that NT-proBNP increased postoperatively (1.64 ± 4.3 vs. 2.38 ± 3.89 ng/ml, p = 0.000).
Comment
In our study we showed in consequent transoesophageal echocardiography that complete resection of LAA with residual stump < 1 cm can be achieved in 99% of patients with stump size 0.28 ± 0.34 cm. Despite being more aggressive in LAA amputation we had no cases of postoperative myocardial infarction and bleeding risk with only 3 patients remained low. The surgical method used in our study was a cut and sew technique for LAA amputation. We chose this technique because it is a safe and effective method for LAA amputation and has been used in other clinical settings. However, it may have some disadvantages, such as the potential for incomplete closure of the LAA, which has not been thoroughly investigated so far. Overall, the cut and sew technique offers a viable option for LAA amputation during open-heart surgery. It is a cost-effective and safe procedure that showed a high rate of completeness of amputation in our study. As such cut and sew technique can be considered safe and sufficient, and more cost effective compared to staplers or occlusion devices.
Prevalence of AF after cardiac surgery ranges between 10 and 65% [14]. Most of these patients are asymptomatic, still if not receiving anti-coagulation after surgery they remain at risk of stroke. Since the patients being operated are getting older every day this represents a major problem in long term outcomes and increases risk of cerebro-vascular events [6]. Some of the problems regarding the oral anticoagulation are high risk of bleeding or insufficient anticoagulation during outpatient management [15, 16]. The new LAAOS III trial showed that concomitant LAA amputation reduced stroke in addition to oral anticoagulation. In this trial different techniques were used for left atrial appendage occlusion beyond cut and sew technique including stapler, closure devices and other approved techniques [17]. Therefore, LAA closure using surgical or percutaneous techniques is gaining tremendous interest. Knowing that most of cardiac emboli origin in left atrial appendage, most logical option for reduction of thromboembolic risk would be its exclusion from circulation during open heart surgery [8, 18]. Some of concerns are risk of bleeding using cut and sew technique, not complete exclusion and recanalization when oversewn from inside or occlude device migration during follow up [19, 20]. In most modern health systems a cost effectiveness of different techniques plays also an important role. Further on, leaving a residual stump larger than 1 cm after LAA excision remains of concern as it poses a risk of harbouring the thrombus [21]. In our study we found that only one patient (0.33%) had a postoperative bleeding connected to LAA amputation and only 3 patients (1%) had a residual stump larger than 1 cm. Moreover, electrical isolation of the LAA during surgical ablation cannot safely be achieved by suture and ligature techniques.
There are still some controversies regarding hemodynamic consequences after LAA amputation most important of it regarding secretion of natriuretic hormones which are primarily produced in LAA [10]. Initial animal experiments raised concerned due to impairment of mechanism to compensate the fluid overload, due to loss of atrium natriuretic peptides but showed no implication in humans [22]. Majunke et al. showed that LAA closure resulted in a significant increase in the ANP and BNP levels after the procedure [23]. This trend in the BNP is the same as in our study. It remains unclear if this is due to LAA amputation alone or if it might be influenced through other concomitant procedures performed. Nevertheless, on long term follow up BNP levels tend to get back to baseline levels up to 2 years postoperatively after LAA amputation having no or less clinically relevant effect on natriuretic peptide levels and severity of heart failure [24].
We also have not seen changes in left atrial volume in our patient series and left atrial diameter decreased after procedure. Of importance is also that NYHA class reduced at 6 months follow up and only 7 (2.3%) patients reported with leg oedemas. No significant change in EF was noted, but we did see higher E/A ratio which might be result of diastolic dysfunction of postcardioplegic myocardium. Also, we noted decreased TAPSE in postoperative control, this is well known phenomenon after cardiac surgery and opening of pericardial sack and postcardioplegic myocardium, so it is unclear if it is induced by LAA amputation alone [25].
It remains unclear if LAA exclusion can reduce or increase postoperative AF. Some studies advocate that LAA exclusion leads to less arrhythmogenic substrate and reduction of AF during follow up [26]. As such there are studies addressing the problem of prophylactic LAA exclusion during routine cardiac surgery, but most of them use heterogenic techniques such as closure from inside, using a stapler or device occlusion [27]. Direct suture is usually performed during mitral valve surgery either as purse string suture or as over-and-over suture. Direct suture has high risk of recanalization or incomplete closure which goes up to 30% [28]. Second method is ligation of LAA, but this can cause bleeding complications or central leakage [29]. Furthermore, in the last years clipping devices became available such as AtriClip device (AtriCure, Mason, OH, USA). The first reports show that AtriClip occlusion appears to be a reproducible and safe surgical method with a high success rate [30]. It is not always easy to apply device in patients with large LAA and the other considerable problem is cost effectiveness if used routinely, especially in times when many health systems cope with expenses cuts. Fast way of LAA excision is use of stapler devices. This again is more suitable in case of minimally invasive procedures when it can be performed thoracoscopically [31].
Kanderian et al. reported that high percentage of patients with suture exclusion still have persistent flow into appendage and high percentage of those with stapler occlusion had a residual LAA stump > 1 cm. In their study even with excision of LAA residual stump was > 1 cm in 27% of patients [21]. Other groups reported complete exclusion in only 45% of patients using sutures [18]. It is possible that due to anatomical closeness of circumflexes artery some surgeons tend to leave more appendage tissue when amputating, having more material for safe closure. Also, simple ligation or purse string suture can be time effective sparing precious cross clamp time. It is important to note that incompletely excluded LAA can be more thromboembolic as blood is more stagnant than left alone at first place [32].
We must comment on the limitations of the study. It is a single centre observational study without any control group. The lack of a control group for comparison is a limitation of our study. We understand that a randomized controlled trial or a propensity-matched cohort study could provide stronger evidence on the effectiveness of the surgical method used for LAA amputation. However, our study aimed to assess the safety and invasiveness of the procedure and to control its effectiveness in terms of completeness of amputation. Despite the absence of a control group, our study provides valuable insights into the feasibility and safety of the cut and sew technique for LAA amputation. Further studies are needed to confirm our findings and to compare the effectiveness of different surgical methods for LAA amputation. Further on, effectiveness and completeness of LAA amputation was measured by intraoperative TEE. All studies and measurements are reproducible and measurements and analysis were performed by trained echocardiography anaesthesiologist and board-certified cardiothoracic attending surgeon blinded to patients and in accordance with the standardized echocardiography protocol. Nevertheless, TEE as such remains subjective diagnostic method dependable of examiner.
LAA amputation does not increase the risk of bleeding and do not affect the heart function. It can be performed safely and completely leaving minimal to no LAA residual stump having as such best cost effectiveness ratio of all occlusion techniques. LAA amputation should therefore be aggressively considered in applicable cases as part of routine open heart surgery.
Data availability
The datasets generated and analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
atrial fibrillation
- ANP:
-
Atrial natriuretic peptide
- BNP:
-
brain natriuretic peptide
- CVE:
-
cerebro-vascular event
- LAA:
-
left atrial appendage
- NYHA:
-
New York Heart Association Class
- POAF:
-
postoperative atrial fibrillation
- sPAP:
-
systolic pulmonary artery pressure
- TAPSE:
-
tricuspid annular plane systolic excursion
- TEE:
-
transoesophageal echocardiography
- TIA:
-
transient ischemic attack
References
Crystal E, Lamy A, Connolly SJ, Kleine P, Hohnloser SH, Semelhago L, et al. Left atrial appendage occlusion study (LAAOS): a randomized clinical trial of left atrial appendage occlusion during routine coronary artery bypass graft surgery for long-term stroke prevention. Am Heart J. 2003;145(1):174–8.
Whitlock R, Healey J, Vincent J, Brady K, Teoh K, Royse A, et al. Rationale and design of the left atrial appendage occlusion study (LAAOS) III. Ann Cardiothorac Surg. 2014;3(1):45–54.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic surgery (EACTS). Eur Heart J. 2021;42(5):373–498.
Saxena A, Dinh D, Dimitriou J, Reid C, Smith J, Shardey G, et al. Preoperative atrial fibrillation is an independent risk factor for mid-term mortality after concomitant aortic valve replacement and coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg. 2013;16(4):488–94.
Kowey PR, Stebbins D, Igidbashian L, Goldman SM, Sutter FP, Rials SJ, et al. Clinical outcome of patients who develop PAF after CABG surgery. Pacing Clin Electrophysiol. 2001;24(2):191–3.
Almahameed ST, Khan M, Zuzek RW, Juratli N, Belden WA, Asher CR, et al. Left atrial appendage exclusion and the risk of thromboembolic events following mitral valve surgery. J Cardiovasc Electrophysiol. 2007;18(4):364–6.
Nagpal AD, Torracca L, Fumero A, Denti P, Cioni M, Alfieri O. Concurrent prophylactic left atrial appendage exclusion: results from a randomized controlled trial pilot study. Eur J Cardiothorac Surg. 2009;36(3):553–7.
Reddy VY, Doshi SK, Kar S, Gibson DN, Price MJ, Huber K, et al. 5-Year Outcomes after Left Atrial Appendage Closure: from the PREVAIL and PROTECT AF trials. J Am Coll Cardiol. 2017;70(24):2964–75.
Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755–9.
Tabata T, Oki T, Yamada H, Abe M, Onose Y, Thomas JD. Relationship between left atrial appendage function and plasma concentration of atrial natriuretic peptide. Eur J Echocardiogr. 2000;1(2):130–7.
Bening C, Alhussini K, Mazalu EA, Yaqub J, Hamouda K, Radakovic D, et al. Impact of diabetes mellitus on the contractile properties of the left and right atrial myofilaments. Eur J Cardiothorac Surg. 2018;54(5):826–31.
Bening C, Mazalu EA, Yaqub J, Alhussini K, Glanowski M, Kottmann T, et al. Atrial contractility and fibrotic biomarkers are associated with atrial fibrillation after elective coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2020;159(2):515–23.
Bening C, Sales VL, Alhussini K, Radakovic D, Benitez RC, Madrahimov N, et al. Clinically inapparent right heart dysfunction is associated with reduced myofilament force development in coronary artery disease. BMC Cardiovasc Disord. 2021;21(1):125.
Conte SM, Florisson DS, De Bono JA, Davies RA, Newcomb AE. Management of atrial fibrillation after cardiac surgery. Intern Med J. 2019;49(5):656–8.
Kirchhof P, Ammentorp B, Darius H, De Caterina R, Le Heuzey JY, Schilling RJ, et al. Management of atrial fibrillation in seven european countries after the publication of the 2010 ESC Guidelines on atrial fibrillation: primary results of the PREvention oF thromboemolic events–european Registry in Atrial Fibrillation (PREFER in AF). Europace. 2014;16(1):6–14.
Ogilvie IM, Newton N, Welner SA, Cowell W, Lip GY. Underuse of oral anticoagulants in atrial fibrillation: a systematic review. Am J Med. 2010;123(7):638–45e4.
Whitlock RP, Belley-Cote EP, Paparella D, Healey JS, Brady K, Sharma M, et al. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med. 2021;384(22):2081–91.
Healey JS, Crystal E, Lamy A, Teoh K, Semelhago L, Hohnloser SH, et al. Left atrial appendage occlusion study (LAAOS): results of a randomized controlled pilot study of left atrial appendage occlusion during coronary bypass surgery in patients at risk for stroke. Am Heart J. 2005;150(2):288–93.
El-Gabry M, Shehada S-E, Wendt D, Mourad F. Emergent surgical removal of a migrated left atrial appendage occluder†. Eur J Cardiothorac Surg. 2018;54(1):191–2.
Lynch M, Shanewise JS, Chang GL, Martin RP, Clements SD. Recanalization of the left atrial appendage demonstrated by transesophageal echocardiography. Ann Thorac Surg. 1997;63(6):1774–5.
Kanderian AS, Gillinov AM, Pettersson GB, Blackstone E, Klein AL. Success of surgical left atrial appendage closure: assessment by transesophageal echocardiography. J Am Coll Cardiol. 2008;52(11):924–9.
Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82(5):547–54.
Majunke N, Sandri M, Adams V, Daehnert I, Mangner N, Schuler G, et al. Atrial and brain natriuretic peptide Secretion after Percutaneous Closure of the Left Atrial Appendage with the Watchman device. J Invasive Cardiol. 2015;27(10):448–52.
Grieshaber P, Arneth B, Steinsberger F, Niemann B, Oswald I, Renz H, et al. Influence of left atrial appendage amputation on natriuretic Peptides-A Randomized Controlled Trial. Thorac Cardiovasc Surg; 2019.
Maus TM. TAPSE: a Red Herring after Cardiac surgery. J Cardiothorac Vasc Anesth. 2018;32(2):779–81.
Di Biase L, Burkhardt JD, Mohanty P, Mohanty S, Sanchez JE, Trivedi C, et al. Left atrial appendage isolation in patients with Longstanding Persistent AF undergoing catheter ablation: BELIEF trial. J Am Coll Cardiol. 2016;68(18):1929–40.
Bedeir K, Warriner S, Kofsky E, Gullett C, Ramlawi B. Left atrial appendage Epicardial Clip (AtriClip): essentials and Post-Procedure Management. J Atr Fibrillation. 2019;11(6):2087.
Katz ES, Tsiamtsiouris T, Applebaum RM, Schwartzbard A, Tunick PA, Kronzon I. Surgical left atrial appendage ligation is frequently incomplete: a transesophageal echocardiograhic study. J Am Coll Cardiol. 2000;36(2):468–71.
Pillarisetti J, Reddy YM, Gunda S, Swarup V, Lee R, Rasekh A, et al. Endocardial (Watchman) vs epicardial (Lariat) left atrial appendage exclusion devices: understanding the differences in the location and type of leaks and their clinical implications. Heart Rhythm. 2015;12(7):1501–7.
Toale C, Fitzmaurice GJ, Eaton D, Lyne J, Redmond KC. Outcomes of left atrial appendage occlusion using the AtriClip device: a systematic review. Interact Cardiovasc Thorac Surg. 2019;29(5):655–62.
Inoue T, Suematsu Y. Left atrial appendage resection can be performed minimally invasively with good clinical and echocardiographic outcomes without any severe risk. Eur J Cardiothorac Surg. 2018;54(1):78–83.
García-Fernández MA, Pérez-David E, Quiles J, Peralta J, García-Rojas I, Bermejo J, et al. Role of left atrial appendage obliteration in stroke reduction in patients with mitral valve prosthesis: a transesophageal echocardiographic study. J Am Coll Cardiol. 2003;42(7):1253–8.
Acknowledgements
This publication was supported by the Open Access Publication Fund of the University of Würzburg.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
I) Conception and design: DR, CB; (II) Administrative support: RL; (III) Provision of study materials or patients: ML, CS, CB; (IV) Collection and assembly of data: DR, KH, NM, KP; (V) Data analysis and interpretation: DR, RL, CB; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics committee of University Wuerzburg (IRB approval: 143/17-sc 6.10.2017). Both, patients with history of AF and those signed for non-atrial fibrillation cardiac surgery were included. All patients gave informed consent. Authors reporting results confirm that all experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki).
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Radakovic, D., Penov, K., Lazarus, M. et al. The completeness of the left atrial appendage amputation during routine cardiac surgery. BMC Cardiovasc Disord 23, 308 (2023). https://doi.org/10.1186/s12872-023-03330-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03330-8