Abstract
Background
The relationship between serum apolipoprotein A1 (APOA1) and atrial fibrillation (AF) is not known. Therefore, we sought to investigate the associations between APOA1 and AF in the Chinese population.
Methods
This case–control study included 950 patients with AF (29–83 years old, 50.42% male) who were hospitalized consecutively in China between January 2019 and September 2021. Controls with sinus rhythm and without AF were matched (1:1) to cases by sex and age. Pearson correlation analysis was performed to investigate the correlation between APOA1 and blood lipid profiles. Multivariate regression models were used to explore the association between APOA1 and AF. The receiver operator characteristic (ROC) curve was constructed to examine the performance of APOA1.
Results
Multivariate regression analysis showed that low serum APOA1 in men and women with AF was significantly associated with AF (OR = 0.261, 95% CI: 0.162–0.422, P < 0.001). Pearson correlation analysis indicated that serum APOA1 was positively correlated with total cholesterol (TC) (r = 0.456, p < 0.001), low-density lipoprotein cholesterol (LDL-C) (r = 0.825, p < 0.001), high-density lipoprotein cholesterol (HDL-C) (r = 0.238, p < 0.001), and apolipoprotein B (APOB) (r = 0.083, p = 0.011). ROC curve analysis showed that APOA1 levels of 1.105 g/L and 1.205 g/L were the optimal cut-off values for predicting AF in males and females, respectively.
Conclusion
Low APOA1 in male and female patients is significantly associated with AF in the Chinese population of non-statin users. APOA1 may be a potential biomarker for AF and contribute to the pathological progression of AF along with low blood lipid profiles. Potential mechanisms remain to be further explored.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF), the most common clinically significant persistent arrhythmia, affects more than 45 million people worldwide [1,2,3] and is associated with an increased risk of heart failure, stroke, systemic embolism, cognitive impairment, and even death [4,5,6,7,8]. As a growing health threat, AF has resulted in significant morbidity, mortality, and a significant health care burden [9]. Although catheter ablation is an effective treatment for AF, the success rate of a single operation is only 60–70%, and potential complications may also exist [10,11,12,13]. There is increasing evidence that risk factor screening strategies may contribute to reducing the incidence of AF [14, 15]. Therefore, exploring available blood biomarkers associated with early pathological changes in patients with AF may help us identify potential risk factors and better understand AF pathogenesis.
Apolipoprotein A1 (APOA1), a multifunctional apolipoprotein and the key protein structural component in high-density lipoprotein (HDL) particles with well-documented cardioprotective properties, especially atheroprotective function, has been considered a significant serum biomarker for predicting multiple cardiovascular events [16, 17]. Although previous studies have reported almost no relationship between lipids and inflammatory markers [18,19,20], it has still been suggested that HDL-C and APOA1 had important anti-inflammatory and anti-oxidative properties [21]. In addition, current evidence suggesting the effects of dyslipidemia on AF remains controversial. Several studies have shown a negative correlation between HDL-C and AF [22,23,24]. One study indicated that HDL-C was positively associated with ischemic stroke in patients with AF [25], and another study suggested that there was no significant association between HDL-C and AF [26]. The relationship between blood lipid profiles and AF and its potential mechanisms deserve further investigation.
To the best of our knowledge, few systematic studies have been conducted to explore the association between serum APOA1 and AF. Therefore, we conducted a case–control study to investigate the association between serum APOA1 and sex- stratified AF and investigated the correlation between APOA1 and blood lipid profiles to help explore early potential serum biomarkers for AF.
Methods
Study design
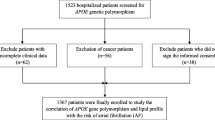
As shown in Fig. 1, we collected and analyzed clinical data from 1900 consecutive hospitalized patients (male/female: 949/951, 68.42 ± 10.87 years) from the Affiliated Hospital of Shandong University of Traditional Chinese Medicine between January 2019 and September 2021. 950 AF patients were included in the AF group, and 950 age- and sex-matched non-AF patients with sinus rhythm were used as controls. The criteria for inclusion in the AF group are: (1) 29–85 years of age; and (2) AF is the primary diagnosis; and (3) complete clinical records and no missing data. Exclusion criteria include: (1) patients with cardiac surgery, heart failure, valvular disease; or (2) patients with hyperthyroidism, malignancy, pregnant women; or (3) patients with alanine aminotransferase (ALT) > 40U/L, aspartate aminotransferase (AST) > 45U/L, or estimated glomerular filtration rate (eGFR) < 60 mL/(min 1.73m2); or (4) use of uric acid lowering drugs. We investigated the clinical characteristics of all participants in an electronic medical record review, including sex, age, laboratory data, AF subtypes, and complications. In addition, we stratified the information of patients with AF primarily by gender and APOB levels. We declare that this study has been reviewed by the Medical Research Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine (NO.20200512FA62) based on the principles of the Helsinki Declaration. The data is anonymous, so the requirement for informed consent has been waived.
Screened variables
We selected the baseline data of all participants including sex, age, AF type, AF complication, and laboratory data including serum apolipoprotein A1(APOA1), serum apolipoprotein B (APOB), blood lipid profiles, aspartate aminotransferase(AST), alanine aminotransferase (ALT), lipoprotein (a) (Lp (a)), serum uric acid (SUA), serum creatinine (SCr), serum albumin (ALB), pre-albumin (PAB), as well as medication situation including statins, CCBs, β-blockers, ACEI/ARB. All laboratory parameters involved were measured by experts in strict compliance with hospital standards before patients were admitted for systematic treatment. APOA1 levels were determined by turbidimetric inhibition immunoassay.
Statistical analysis
All statistical analyses were performed using SPSS software (version 26.0; SPSS Inc., Chicago, IL, USA) or GraphPad Prism software (version 9.0.0). Continuous variables were expressed as mean ± standard deviations (SD) and compared by Student t-test analysis and variance analysis (ANOVA). Categorical variables were presented as n(%) and compared by chi-square tests. Pearson correlation analyses were used to evaluate interrelationships and visualized as scatter plots. In addition, stepwise multivariate logistic regression analyses were performed to adjust for covariates, shown as odds ratios (ORs) and 95% confidence intervals (95% CIs). A p-value < 0.05 with two tails was considered significant.
Results
Baseline clinical characteristics of participants
As shown in Table 1, a total of 1900 consecutive hospitalized patients (M/F: 949/951, 68.42 ± 10.87 years) were divided into two groups, including 950 AF patients (M/F: 479/471, 68.61 ± 10.34 years) and 950 controls (M/F: 470/480, 68.23 ± 11.37 years). Compared with controls, AF patients were more likely to experience hypertension, CHD, diabetes and had a history of statins, CCBs, β-blockers, and ACEI/ARB (p < 0.001), as well as significantly lower levels of APOAl, APOB, TG, TC, LDL-C, HDL-C, ALB, and PAB(P < 0.05), significantly higher levels of AST, SCr, and SUA(P < 0.05), but no significant difference in serum levels of Lp(a), FBG, and ALT between the two groups (P > 0.05).
Correlation between serum APOA1 and AF
We established stepwise multivariate logistic regression models to explore the correlation between serum APOA1 and AF. Covariates were determined by combining the statistical differences between the two groups as shown in Table 1 with potential influencing factors reported in previous literature. As shown in Table 2, after adjusting for APOB, LDL-C, and AST, serum APOA1 was considered to be a related factor for AF (OR = 0.232, 95% CI: 0.154–0.350, P < 0.001). Further, after adjusting for hypertension, diabetes, CCBs, ACEI/ARB, and statins, serum APOA1 was still an associated factor for AF (OR = 0.269, 95% CI: 0.175–0.414, P < 0.001). Finally, after adjusting for all confounding factors, serum APOA1 remained a significant factor for AF (OR = 0.261, 95% CI:0.162–0.422, P < 0.001). In addition, serum APOA1 was negatively correlated with AF in both genders (P < 0.05). Meanwhile, we further explored the association between APOA1 and AF in statin recipients and non-statin recipients. Interestingly, as shown in Tables 3 and 4, an independent inverse association between APOA1 and AF was found only in non-statin users (P < 0.05).
Differences in APOA1 levels between AF patients and controls by sex and age
Figure 2 shows the difference in APOA1 levels between AF patients and controls by sex and age. Compared with controls, APOA1 levels in AF patients were significantly lower in men(1.07 ± 0.25 vs. 1.15 ± 0.24 g/L, P < 0.001; Fig. 2(A)) and women (1.19 ± 0.27 vs. 1.30 ± 0.23 g/L, P < 0.001; Fig. 2(A)), significantly lower in patients with age ≤ 60 years (1.14 ± 0.26 vs. 1.17 ± 0.22 g/L, P < 0.001; Fig. 2(B)) and age > 60 years (1.13 ± 0.27 vs. 1.24 ± 0.25 g/L, P < 0.001; Fig. 2(B)).
APOA1 levels in AF and control groups by sex and age. Compared with controls, APOA1 levels in AF patients were significantly lower in men( 1.07 ± 0.25 vs. 1.15 ± 0.24 g/L, P < 0.001; Fig. 2(A)) and women (1.19 ± 0.27 vs. 1.30 ± 0.23 g/L, P < 0.001; Fig. 2(A)), significantly lower in patients with age ≤ 60 years (1.14 ± 0.26 vs. 1.17 ± 0.22 g/L, P < 0.001; Fig. 2(B)) and age > 60 years (1.13 ± 0.27 vs. 1.24 ± 0.25 g/L, P < 0.001; Fig. 2(B)). Abbreviations as shown in Table 1
Difference in APOA1 levels between AF patients and controls by type and complication of AF
Figure 3 shows the difference in APOA1 levels between AF patients and controls by type and complication of AF. Compared with the permanent AF group and controls, APOA1 levels in the paroxysmal AF group were significantly lower in the men ( 1.05 ± 0. 26 vs.1.08 ± 0.24 vs. 1.15 ± 0.24 g/L, P < 0.001; Fig. 3(A)) and women ( 1.18 ± 0.28 vs.1.19 ± 0.26 vs. 1.30 ± 0.23 g/L, P < 0.001; Fig. 3(A)). However, there was no significant difference in APOA1 levels between men and women with AF complications (P > 0.05; Fig. 3(B)).
APOA1 levels in different types and complications of AF. Compared to the permanent AF group and controls, APOA1 levels in the paroxysmal AF group were significantly lower in men (1.05 ± 0. 26 vs.1.08 ± 0.24 vs. 1.15 ± 0.24 g/L, P < 0.001; Fig. 3(A)) and women ( 1.18 ± 0.28 vs. 1.19 ± 0.26 vs. 1.30 ± 0.23 g/L, P < 0.001; Fig. 3(A)). However, there was no significant difference in APOA1 levels between men and women with AF complications (P > 0.05; Fig. 3(B)). Abbreviations as shown in Table 1
Correlation between serum APOA1 and AF-related metabolic factors
Figure 4 shows the correlation between serum APOA1 and blood lipid profiles. Serum APOA1 was positively correlated with TC (r = 0.456, p < 0.001; Fig. 4(A)), LDL-C (r = 0.825, p < 0.001; Fig. 4(B)), HDL-C (r = 0.238, p < 0.001; Fig. 4(C)), and APOB (r = 0.083, p = 0.011; Fig. 4(D)).
Correlation between serum APOA1 and lipid profiles in AF patients. A Correlation between serum APOA1 and TC in AF patients (r = 0.456, p < 0.001). B Correlation between serum APOA1 and LDL-C in AF patients (r = 0.825, p < 0.001). C Correlation between serum APOA1 and HDL-C in AF patients (r = 0.238, p < 0.001). D Correlation between serum APOA1 and APOB in AF patients (r = 0.083, p = 0.011). Abbreviations as shown in Table 1
Subgroup analysis of serum APOA1 levels and lipid profiles in patients with paroxysmal AF
Table 5 shows the relationship between serum APOA1 levels and blood lipid profiles in patients with paroxysmal AF. These results suggested that lower serum APOA1 had lower TC, LDL-C, and HDL-C in both sexes (P < 0.001).
Subgroup analysis of the relationship between serum APOA1 levels and blood lipid profiles in patients with permanent AF
Table 6 shows the relationship between serum APOA1 levels and blood lipid profiles in patients with permanent AF. The present results showed that lower serum APOA1 had lower TC, LDL-C, and HDL-C in both sexes (P < 0.001).
ROC curve model for APOA1 levels predicting AF
Figure 5 shows the ROC curve model for APOA1 levels predicting AF by sex. The ROC curve analysis suggested that APOA1 levels = 1.105 g/L were the most optimal cut-off value for predicting AF in men. Area under the ROC curve for the model was 0.592 (0.557—0.628, P < 0.001, Fig. 5(A)), sensitivity was 0.591, specificity was 0.551; APOA1 levels = 1.205 g/L was the best cut-off value for predicting AF in women; area under the ROC curve for the model was 0.611 (0.576—0.647, P-0.05, Fig. 5(B)), sensitivity was 0.520, specificity was 0.640.
A ROC curve in males for APOA1 levels. The area under the ROC curve was 0.592 (0.557 to 0.628, P < 0.05). When the optimum cut-off value of APOA1 was 1.105 g/L, sensitivity was 0.591 and specificity was 0.551. B Female ROC curve for APOA1 levels. The area under the ROC curve was 0.611 (0.576 to 0.647, P < 0.05). When the optimum cut-off value of APOA1 was 1.205 g/L, sensitivity was 0.520 and specificity was 0.640. Abbreviations as shown in Table 1. The figure was developed by GraphPad Prism (version 9.0.0)
Discussion
This study is the first to investigate the association between serum APOA1 and AF in the Chinese population. These results indicated that low serum APOA1 in both male and female patients was associated with AF. Serum APOA1 in male patients was significantly lower than in female patients with AF. Further results showed that serum APOA1 was positively correlated with TC, LDL-C, HDL-C, and APOB. Subgroup analysis showed lower serum APOA1 in male and female patients who had lower TC, LDL-C, and HDL-C with paroxysmal AF and permanent AF. These detailed findings may contribute to our understanding of the relationship between serum APOA1 and sex in patients with AF. When the optimal cut-off value of APOA1 in males was 1.105 g/L, sensitivity was 0.591, specificity was 0.551; when the optimal cut-off value of APOA1 in females was 1.205 g/L, sensitivity was 0.520, specificity was 0.640.
As a major protein component of HDL, APOA1 has played an important role in HDL synthesis. Cholesterol acyltransferase (LCAT) is an enzyme secreted by the liver that circulates with HDL and increases HDL carrying capacity by esterifying cholesterol. Studies have shown that APOA1 not only mediated HDL synthesis but also participated in LCAT activation [17]. Clinical evidence indicated that HDL was atheroprotective, as well as having anti-inflammatory, anti-oxidative, and anti-thrombotic properties [27,28,29]. The oxidation of HDL mainly occurs in the inflammatory microenvironment and HDL-related paraoxonase activity may reduce systemic oxidative stress, which may be associated with a reduced risk of cardiovascular events [30, 31]. Furthermore, tryptophan oxidation of APOA1 may also contribute to promoting inflammation [32,33,34]. There is growing evidence that inflammation and oxidative stress play a significant role in AF pathogenesis [35,36,37]. In addition, oxidative modification of lipoproteins was thought to be key to atherosclerosis formation [38]. Lipid peroxidation induced damage to myocardial cells and electrophysiological changes formed the AF matrix [39,40,41]. From this perspective, APOA1 may maintain the pathological process of AF through pro-inflammatory and pro-oxidation chains and HDL-C.
To date, few studies have reported the association between serum APOA1 and AF. A prospective cohort study based on 35 PAF patients and 34 healthy participants showed that PAF participants had lower serum APOA1 levels [42]. Another study based on 11 women with paroxysmal lone AF and 10 women with non-AF indicated that compared with controls, there was an approximately 30% lower expression of serum APOA1 in women with AF [43]. Compared to previous studies, this study was conducted in a larger sample size and more systematically investigated the association between serum APOA1 and AF by sex, as well as blood lipid profiles. Our current results indicated that, after adjustment for confounding factors, serum APOA1 and AF were independently and negatively associated with both sexes who did not receive statins. Compared to women, APOA1 levels were significantly lower in men with AF, regardless of AF type, or AF complications. Three explanations may be suggested for this significant difference: sex hormones, arterial biochemical characteristics, and body shape [44].
In addition, we also found that serum APOA1 was correlated with blood lipid profiles. Current results showed lower blood lipid profiles in patients with AF, which was consistent with previous findings that reported significant decreases in TG and LDL-C in patients with persistent AF [45]; therefore, we speculate that our study may have included several patients with permanent AF, a phase in which patients noticed AF development and were taking lipid-lowering drugs, and thus showed lower lipid levels. Pearson correlation analysis indicated that serum APOA1 was positively correlated with TC, LDL-C, HDL-C, and APOB. Interestingly, serum APOA1 was more strongly associated with LDL-C than HDL-C, although APOA1 is a component of HDL particle, we suspect that it may be related to the stronger association between LDL-C and AF and the changes in patients' diet in the short term, this finding remains to be confirmed in future studies. Furthermore, subgroup analysis showed lower serum APOA1 in male and female patients who had lower TC, LDL-C, and HDL-C with paroxysmal AF and permanent AF. These findings suggest that the "cholesterol paradox" remains. Currently, the relationship between blood lipid profiles and AF, as well as gender differences, is still controversial. A meta-analysis of large cohort studies reported that TC, LDL-C, and HDL-C were negatively correlated with AF risk [23]. Another longitudinal study in Japan showed that low HDL-C was associated with a higher risk of new-onset AF only in women [46]. In addition, a large study from the Swedish database suggested that TC was negatively correlated with new-onset AF in men and women with hypertension [47]. Our partial results are supported by these studies, although there are some differences. Several possible reasons are worth mentioning. First, study populations are heterogeneous, due to regional differences. Second, the research and statistical methods used are different. Third, there were some confounding factors that interfered with the results. Finally, our patients were hospitalized with several complications, including hypertension, coronary heart disease, and diabetes. In addition, a relationship between low APOB and inflammation has also been established [48]. Low HDL-C is known to be associated with an increased risk of arteriosclerosis, inflammatory disorders, diabetes, and other diseases, which may lead to AF pathogenesis and risk factors [49]. Of course, the specific mechanism remains to be demonstrated in further research.
There were several potential limitations worth considering. First, this single-center case–control study cannot confirm causality. Second, we only investigated the population with paroxysmal AF and permanent AF, lacking a comparison of data for patients with persistent AF. Third, participants' status of inflammation and oxidative stress was not assessed. Fourth, some significant confounding factors may also be missing. In addition, the limited sample size was not friendly to our current results, and we gave up adjusting for several important influencing factors, such as family history, lifestyle, and exercise. However, it did provide us with a new perspective for understanding the pathology of AF. Further prospective cohort studies were encouraged, which may help further evaluate the association between serum APOA1 and AF. The effects of AF-related metabolic factors on serum APOA1 were also worth considering.
Conclusion
In conclusion, low serum APOA1 in male and female AF patients is independently associated with AF in the Chinese population of non-statin users. Serum APOA1 levels are positively correlated with blood lipid profiles. These findings suggest that low APOA1 and blood lipid profiles may be involved in AF initiation and maintenance. Prospective cohort designs are essential to explore causal relationships and potential mechanisms.
Availability of data and materials
Data sets are not publicly available because they contain information that could compromise the privacy of research participants, but minimal data is available from the corresponding author upon reasonable request.
References
Waldmann V, Jouven X, Narayanan K, Piot O, Chugh SS, Albert CM, et al. Association between atrial fibrillation and sudden cardiac death: pathophysiological and epidemiological insights. Circ Res. 2020;127:301–9. https://doi.org/10.1161/CIRCRESAHA.120.316756.
Zimetbaum P. Atrial Fibrillation [published correction appears in Ann Intern Med. 2017 Jun 20;166(12 ):920]. Ann Intern Med. (2017) 166:ITC33-ITC48. https://doi.org/10.7326/AITC201703070
Arbelo E, Dagres N. The 2020 ESC atrial fibrillation guidelines for atrial fibrillation catheter ablation, CABANA, and EAST. Europace. 2022;24(Suppl 2):ii3–7. https://doi.org/10.1093/europace/euab332.
Santhanakrishnan R, Wang N, Larson MG, Magnani JW, McManus DD, Lubitz SA, et al. Atrial fibrillation begets heart failure and vice versa: temporal associations and differences in preserved versus reduced ejection fraction. Circulation. 2016;133:484–92. https://doi.org/10.1161/CIRCULATIONAHA.115.018614.
Healey JS, Amit G, Field TS. Atrial fibrillation and stroke: how much atrial fibrillation is enough to cause a stroke? Curr Opin Neurol. 2020;33:17–23. https://doi.org/10.1097/WCO.0000000000000780.
Bruins Slot KM, Berge E. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2018;3(3):CD008980. https://doi.org/10.1002/14651858.CD008980.pub3.
Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res. 2017;120:1501–17. https://doi.org/10.1161/CIRCRESAHA.117.309732.
Lopes RD, Rordorf R, De Ferrari GM, Leonardi S, Thomas L, Wojdyla DM, et al. Digoxin and mortality in patients with atrial fibrillation. J Am Coll Cardiol. 2018;71:1063–74. https://doi.org/10.1016/j.jacc.2017.12.060.
Wong CX, Brooks AG, Leong DP, Roberts-Thomson KC, Sanders P. The increasing burden of atrial fibrillation compared with heart failure and myocardial infarction: a 15-year study of all hospitalizations in Australia. Arch Intern Med. 2012;172:739–41. https://doi.org/10.1001/archinternmed.2012.878.
Şaylık F, Çınar T, Akbulut T, Hayıroğlu Mİ. Comparison of catheter ablation and medical therapy for atrial fibrillation in heart failure patients: a meta-analysis of randomized controlled trials [published online ahead of print, 2022 Sep 6]. Heart Lung. 2022;57:69–74.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–104. https://doi.org/10.1161/CIR.0000000000000040.
Verma A, Jiang CY, Betts TR, Chen J, Deisenhofer I, Mantovan R, et al. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015;372:1812–22. https://doi.org/10.1056/NEJMoa1408288.
Link MS, Haïssaguerre M, Natale A. Ablation of atrial fibrillation: patient selection, periprocedural anticoagulation, techniques, and preventive measures after ablation. Circulation. 2016;134:339–52. https://doi.org/10.1161/CIRCULATIONAHA.116.021727.
Jiang Q, Wang K, Shi J, Li M, Chen M. No association between alcohol consumption and risk of atrial fibrillation: a two-sample Mendelian randomization study. Nutr Metab Cardiovasc Dis. 2020;30:1389–96. https://doi.org/10.1016/j.numecd.2020.04.014.
Tousoulis D. Biomarkers in atrial fibrillation; from pathophysiology to diagnosis and treatment. Curr Med Chem. 2019;26:762–4. https://doi.org/10.2174/092986732605190422092911.
Cochran BJ, Ong KL, Manandhar B, Rye KA. APOA1: a protein with multiple therapeutic functions. Curr Atheroscler Rep. 2021;23:11. https://doi.org/10.1007/s11883-021-00906-7.
Flores R, Jin X, Chang J, Zhang C, Cogan DG, Schaefer EJ, et al. LCAT, ApoD, and ApoA1 Expression and Review of Cholesterol Deposition in the Cornea. Biomolecules. 2019;9:785. https://doi.org/10.3390/biom9120785.
Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347:1557–65. https://doi.org/10.1056/NEJMoa021993.
Schlitt A, Blankenberg S, Bickel C, Meyer J, Hafner G, Jiang XC, et al. Prognostic value of lipoproteins and their relation to inflammatory markers among patients with coronary artery disease. Int J Cardiol. 2005;102:477–85. https://doi.org/10.1016/j.ijcard.2004.05.056.
Bermudez EA, Rifai N, Buring J, Manson JE, Ridker PM. Interrelationships among circulating interleukin-6, C-reactive protein, and traditional cardiovascular risk factors in women. Arterioscler Thromb Vasc Biol. 2002;22:1668–73. https://doi.org/10.1161/01.atv.0000029781.31325.66.
Trieb M, Kornej J, Knuplez E, Hindricks G, Thiele H, Sommer P, et al. Atrial fibrillation is associated with alterations in HDL function, metabolism, and particle number. Basic Res Cardiol. 2019;114:27. https://doi.org/10.1007/s00395-019-0735-0.
Harrison SL, Lane DA, Banach M, Mastej M, Kasperczyk S, Jóźwiak JJ, et al. Lipid levels, atrial fibrillation and the impact of age: Results from the LIPIDOGRAM2015 study. Atherosclerosis. 2020;312:16–22. https://doi.org/10.1016/j.atherosclerosis.2020.08.026.
Guan B, Li X, Xue W, Tse G, Waleed KB, Liu Y, et al. Blood lipid profiles and risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Clin Lipidol. 2020;14:133–42. https://doi.org/10.1016/j.jacl.2019.12.002.
Li ZZ, Du X, Guo XY, Tang RB, Jiang C, Liu N, et al. Association between blood lipid profiles and atrial fibrillation: a case-control study. Med Sci Monit. 2018;24:3903–8. https://doi.org/10.12659/MSM.907580.
Li F, Du X, He L, Jiang C, Xia S, Ma C, et al. Relationship between serum lipid levels and ischemic stroke in patients with atrial fibrillation: a nested case-control study based on the China Atrial Fibrillation Registry. BMC Cardiovasc Disord. 2021;21:424. https://doi.org/10.1186/s12872-021-02237-6.
Li X, Gao L, Wang Z, Guan B, Guan X, Wang B, et al. Lipid profile and incidence of atrial fibrillation: a prospective cohort study in China. Clin Cardiol. 2018;41:314–20. https://doi.org/10.1002/clc.22864.
Besler C, Lüscher TF, Landmesser U. Molecular mechanisms of vascular effects of High-density lipoprotein: alterations in cardiovascular disease. EMBO Mol Med. 2012;4:251–68. https://doi.org/10.1002/emmm.201200224.
Chistiakov DA, Orekhov AN, Bobryshev YV. ApoA1 and ApoA1-specific self-antibodies in cardiovascular disease. Lab Invest. 2016;96:708–18. https://doi.org/10.1038/labinvest.2016.56.
Barter PJ, Nicholls S, Rye KA, Anantharamaiah GM, Navab M, Fogelman AM. Antiinflammatory properties of HDL. Circ Res. 2004;95:764–72. https://doi.org/10.1161/01.RES.0000146094.59640.13.
Nazir S, Jankowski V, Bender G, Zewinger S, Rye KA, van der Vorst EPC. Interaction between high-density lipoproteins and inflammation: Function matters more than concentration! Adv Drug Deliv Rev. 2020;159:94–119. https://doi.org/10.1016/j.addr.2020.10.006.
Tang WH, Wu Y, Mann S, Pepoy M, Shrestha K, Borowski AG, et al. Diminished antioxidant activity of high-density lipoprotein-associated proteins in systolic heart failure. Circ Heart Fail. 2011;4:59–64. https://doi.org/10.1161/CIRCHEARTFAILURE.110.958348.
Uchida G, Mino Y, Suzuki T, Ikeda JI, Suzuki T, Takenaka K, et al. Decomposition and oxidation of methionine and tryptophan following irradiation with a nonequilibrium plasma jet and applications for killing cancer cells [published correction appears in Sci Rep. 2019 Nov 27;9(1):18140]. Sci Rep. 2019;9:6625. https://doi.org/10.1038/s41598-019-42959-4.
Torosantucci R, Schöneich C, Jiskoot W. Oxidation of therapeutic proteins and peptides: structural and biological consequences. Pharm Res. 2014;31:541–53. https://doi.org/10.1007/s11095-013-1199-9.
Huang Y, DiDonato JA, Levison BS, Schmitt D, Li L, Wu Y, et al. An abundant dysfunctional apolipoprotein A1 in human atheroma. Nat Med. 2014;20:193–203. https://doi.org/10.1038/nm.3459.
Harada M, Van Wagoner DR, Nattel S. Role of inflammation in atrial fibrillation pathophysiology and management. Circ J. 2015;79:495–502. https://doi.org/10.1253/circj.CJ-15-0138.
Li JY, He Y, Ke HH, Jin Y, Jiang ZY, Zhong GQ. Plasma oxidative stress and inflammatory biomarkers are associated with the sizes of the left atrium and pulmonary vein in atrial fibrillation patients. Clin Cardiol. 2017;40:89–94. https://doi.org/10.1002/clc.22633.
Gutierrez A, Van Wagoner DR. Oxidant and Inflammatory Mechanisms and Targeted Therapy in Atrial Fibrillation: An Update. J Cardiovasc Pharmacol. 2015;66:523–9. https://doi.org/10.1097/FJC.0000000000000313.
Steinberg D. Atherogenesis in perspective: hypercholesterolemia and inflammation as partners in crime. Nat Med. 2002;8:1211–7. https://doi.org/10.1038/nm1102-1211.
Clarkson CW, Ten Eick RE. On the mechanism of lysophosphatidylcholine-induced depolarization of cat ventricular myocardium. Circ Res. 1983;52:543–56. https://doi.org/10.1161/01.res.52.5.543.
Adamantidis MM, Moreau-Guedon L, Martin-Nizard F, Sqalli-Houssaini H, Duriez P, Fruchart JC, et al. Oxidized low density lipoproteins exert arrhythmogenic effects in rabbit Purkinje fibers. Biochem Biophys Res Commun. 1992;182:548–54. https://doi.org/10.1016/0006-291x(92)91767-k.
Pogwizd SM, Onufer JR, Kramer JB, Sobel BE, Corr PB. Induction of delayed afterdepolarizations and triggered activity in canine Purkinje fibers by lysophosphoglycerides. Circ Res. 1986;59:416–26. https://doi.org/10.1161/01.res.59.4.416.
Çınar T, Tanık VO, Gürkan K. Comparison of apolipoprotein-A1 levels between paroxysmal atrial fibrillation patients and healthy subjects. J Cardiovasc Thorac Res. 2020;12:140–4. https://doi.org/10.34172/jcvtr.2020.23.
Kim SM, Lee JH, Kim JR, Shin DG, Lee SH, Cho KH. Female patients with atrial fibrillation have increased oxidized and glycated lipoprotein properties and lower apolipoprotein A-I expression in HDL. Int J Mol Med. 2011;27:841–9. https://doi.org/10.3892/ijmm.2011.646.
Sun X, Chen R, Yan G, Chen Z, Yuan H, Huang W, et al. Gender-specific associations between apolipoprotein A1 and arterial stiffness in patients with nonalcoholic fatty liver disease. PeerJ. 2020;8:e9757. https://doi.org/10.7717/peerj.9757.
Wang XD, Liu J, Zhang YC, Wang Y, Wang Y, Ma D. Correlation between the elevated uric acid levels and circulating renin-angiotensin-aldosterone system activation in patients with atrial fibrillation. Cardiovasc Diagn Ther. 2021;11:50–5. https://doi.org/10.21037/cdt-20-830.
Watanabe H, Tanabe N, Yagihara N, Watanabe T, Aizawa Y, Kodama M. Association between lipid profile and risk of atrial fibrillation. Circ J. 2011;75:2767–74. https://doi.org/10.1253/circj.cj-11-0780.
Mourtzinis G, Kahan T, BengtssonBoström K, Schiöler L, CedstrandWallin L, Hjerpe P, et al. Relation Between Lipid Profile and New-Onset Atrial Fibrillation in Patients With Systemic Hypertension (From the Swedish Primary Care Cardiovascular Database [SPCCD]). Am J Cardiol. 2018;122:102–7. https://doi.org/10.1016/j.amjcard.2018.03.024.
Faraj M, Lavoie ME, Messier L, Bastard JP, Prud’homme D. Reduction in serum apoB is associated with reduced inflammation and insulin resistance in post-menopausal women: a MONET study. Atherosclerosis. 2010;211:682–8. https://doi.org/10.1016/j.atherosclerosis.2010.04.012.
Rohatgi A, Westerterp M, von Eckardstein A, Remaley A, Rye KA. HDL in the 21st Century: A Multifunctional Roadmap for Future HDL Research. Circulation. 2021;143:2293–309. https://doi.org/10.1161/CIRCULATIONAHA.120.044221.
Acknowledgements
I would like to express my special thanks to my partners and our funding agency for their encouragement and support during this study.
Funding
This study was supported by the Young Qihuang Scholars of the National Administration of Traditional Chinese Medicine (No.2022–256). The funding bodies had no role in the research design, data collection, analysis, interpretation, manuscript writing, and submission.
Author information
Authors and Affiliations
Contributions
Huachen Jiao was the main coordinator of the project and was responsible for the design of the study. Xia Zhong and Huachen Jiao drafted the manuscript of this paper. Dongsheng Zhao was involved in overseeing data collection and stratification. Xia Zhong, Jie Yu, Dongsheng Zhao, and Jing Teng contributed to data compilation and analysis. All authors contributed intellectually to this manuscript and have approved this final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was approved by the Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine. Because the data is anonymized, the Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine (NO.20200512FA62) waived the need for informed consent. We confirm that all the methods and human data involved were carried out in accordance with the relevant guidelines and provisions of the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhong, X., Yu, J., Zhao, D. et al. Association between serum apolipoprotein A1 and atrial fibrillation in the Chinese population: a case–control study. BMC Cardiovasc Disord 23, 269 (2023). https://doi.org/10.1186/s12872-023-03283-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03283-y