Abstract
Background
Currently, the study outcomes of anthropometric markers to predict the risk of hypertension are still inconsistent due to the effect of racial disparities. This study aims to investigate the most effective predictors for screening and prediction of hypertension (HTN) in the Chinese middle-aged and more elderly adult population and to predict hypertension using obesity and lipid-related markers in Chinese middle-aged and older people.
Methods
The data for the cohort study came from the China Health and Retirement Longitudinal Study (CHARLS), including 4423 middle-aged and elderly people aged 45 years or above. We examined 13 obesity- and lipid-related indices, including waist circumference (WC), body mass index (BMI), waist-height ratio (WHtR), visceral adiposity index (VAI), a body shape index (ABSI), body roundness index (BRI), lipid accumulation product index (LAP), conicity index (CI), Chinese visceral adiposity index (CVAI), triglyceride-glucose index (TyG-index) and their combined indices (TyG-BMI, TyG-WC, TyG-WHtR). To compare the capacity of each measure to forecast the probability of developing HTN, the receiver operating characteristic curve (ROC) was used to determine the usefulness of anthropometric indices for screening for HTN in the elderly and determining their cut-off value, sensitivity, specificity, and area under the curve (AUC). Association analysis of 13 obesity-related anthropometric indicators with HTN was performed using binary logistic regression analysis.
Results
During the four years, the incident rates of HTN in middle-aged and elderly men and women in China were 22.08% and 17.82%, respectively. All the above 13 indicators show a modest predictive power (AUC > 0.5), which is significant for predicting HTN in adults (middle-aged and elderly people) in China (P < 0.05). In addition, when WHtR = 0.501 (with an AUC of 0.593, and sensitivity and specificity of 63.60% and 52.60% respectively) or TYg-WHtR = 4.335 (with an AUC of 0.601, and sensitivity and specificity of 58.20% and 59.30% respectively), the effect of predicting the incidence risk of men is the best. And when WHtR = 0.548 (with an AUC of 0.609, and sensitivity and specificity of 59.50% and 56.50% respectively) or TYg-WHtR = 4.781(with an AUC of 0.617, and sensitivity and specificity of 58.10% and 60.80% respectively), the effect of predicting the incidence risk of women is the best.
Conclusions
The 13 obesity- and lipid-related indices in this study have modest significance for predicting HTN in Chinese middle-aged and elderly patients. WHtR and Tyg-WHtR are the most cost-effective indicators with moderate predictive value of the development of HTN.
Similar content being viewed by others
Background
Hypertension (HTN) is a chronic noncommunicable condition in which the Systolic blood pressure (SBP) and/or Diastolic blood pressure (DBP) are elevated, frequently accompanied by functional or physical damage to the heart, brain, kidney, and other organs [1]. One of the most common chronic non-communicable diseases in the world, HTN is also a major risk factor for cardiovascular disease, with HTN complications accounting for approximately 53% of all cardiovascular disease-related deaths [2]. According to current statistics, the global incidence of HTN will climb from 26% in 2000 to 29.2% by 2025 [3]. Although HTN is more prevalent in higher-income countries such as the United States [4], it is quickly growing in low- and middle-income countries [5, 6]. According to hypertension survey data from 2012 to 2015, the incident rate of hypertension among adults in China was 23.2% [7], and the number of fatalities caused by hypertension among Chinese residents was 2.54 million in 2017, with cardiovascular disease deaths accounting for 95.7% [8].
Obesity has become an increasingly important worldwide public health concern as people's living standards have improved and their life rhythms have accelerated. Weight increase and blood pressure rise are clearly linked, according to studies [9,10,11], and these obesity markers have a strong dose–response association with the onset of hypertension [12]. In previous studies, body mass index (BMI) was used as the most prevalent marker of obesity and overweight [13]. In recent years, scholars have proposed many new obesity and lipid-related indicators, but the results of studies on anthropometric markers to predict hypertension risk remain inconsistent due to ethnic differences and various factors [14,15,16,17,18,19,20,21,22,23,24]. However, these studies are not representative for predicting hypertension in Chinese middle-aged and older adults because most of these studies describe only one indicator and do not compare it with other indicators.
Therefore, this study's objective was to investigate the screening and predicting functions of obesity and lipid-related indicators for HTN in middle-aged and elderly Chinese, as well as the ideal predicted cut-off value to provide a basis for HTN prevention and therapy.
Methods
Study design and setting
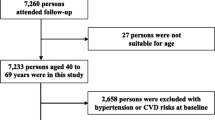
The data for our analysis came from the 2011 China Health and Retirement Longitudinal Survey Wave (CHARLS Wave 2011), a nationally representative longitudinal investigation, which was conducted by the China Center for Economic Research at Peking University [25]. Individuals without HTN in baseline from the CHARLS Wave 2011 study were included in our analysis after missing data subjects were removed. Subsequently, data collection was conducted in 2015. The numbers of individuals who completed both the baseline and follow-up surveys were 4423 for the cohort design. Without any direct interaction with people, all data are provided in the open as microdata at http://charls.pku.edu.cn/index/zh-cn.html. All participants gave their informed consent prior to the collection of data, and the study was approved by the Ethics Committee of the China Center for Economic Research at Peking University.
Individuals
Study subjects for this investigation were chosen from the China Health and Retirement Longitudinal Study (CHARLS), Wave 1 (2011). The CHARLS Wave 2011 was used to choose participants for this study [25]. This research is a cohort study. Patients with undetected hypertension were included to our follow-up group in 2011. In 2015, the incident rate of individuals impacted by 13 indicators was evaluated four years later. The average age of the 4,423 individuals participating in CHARLS was 57.43 years (standard deviation SD = 8.89, range 45–98 years). Males had a mean age of 59.08 years (SD = 8.79, range 45–98 years) while females had a mean age of 56.02 years (SD = 8.74, range 45–90 years).
Baseline characteristics
Baseline characteristics including age, sex (1 = male; 2 = female), education (1 = illiterate; 2 = less than elementary school; 3 = high school; 4 = above vocational school), marital status (1 = married; 2 = single), living place (1 = rural; 2 = urban), smoking status (1 = no; 2 = former smoke; 3 = current smoke), drinking status (1 = no; 2 = less than once a month; 3 = more than once a month), taking activities (1 = no; 2 = yes), and Having regular exercises (1 = no; 2 = less than exercises; 3 = regular exercises),and the counts of Chronic diseases (0 = 0; 1 = 1–2; 2 = 3–14)were collected by self-report. Most variables depended on our previous research studies [26,27,28,29,30,31].
Definition
Participants were divided into hypertensive and non-hypertensive groups. Hypertension was formerly described as having a systolic blood pressure (SBP) ≥ 140 mmHg and/or a diastolic blood pressure (DBP) ≥ 90 mmHg, or with hypertension diagnosed by self-reported physician diagnosis. Non-hypertension was defined as SBP < 140 mm Hg, DBP < 90 mmHg and patients who have not received antihypertensive treatment. This classification was widely used in our previous studies [26, 28, 31,32,33].
Glucose, High-density lipoprotein cholesterol, Triglycerides Measurement
The Chinese Center for Disease Control and Prevention in Beijing received the venous blood samples within two weeks of them leaving the Centers for Disease Control and Prevention station. The samples were immediately stored and frozen at -20 °C before being delivered. When the necessary assays were completed in the lab of the Chinese Medical University, they were put in a deep refrigerator and kept at -80 °C. At the Capital Medical University Youanmen Clinical Laboratory, triglycerides (TG), fasting plasma glucose (FPG), and high-density lipoprotein cholesterol (HDL-C) were measured using the enzyme colorimetric assay. We divided TG levels into two groups, < 150 mg/dL and ≥ 150 mg/dL, in accordance with a classification that has previously been employed in studies [26]. When fasting plasma glucose is ≥ 126 mg/dl or 7.0 mmol/dl and above, it indicates abnormal blood glucose [33]. HDL-C values lower than 40 for men and 50 mg/dL for women were considered abnormal [34].
Measurements
Omron™ HEM-7112 Monitor (Manufacturer: Omron Co., Ltd., Dalian, China) was used to monitor blood pressure on the respondent's left arm three times at 45-s intervals. Respondents were asked to sit with both feet on the floor and their left arm comfortably supported, palm up. Unless they were wearing a short sleeve or a flimsy shirt, respondents were requested to roll their sleeves up. The cuff's bottom was about half an inch above the respondent's elbow, and the air tube went down the center of the respondent's arm. After the interviewer presses the start button, the cuff automatically inflates, and then deflates to show systolic and diastolic blood pressure. After recording the results truthfully, the interviewer uses a stopwatch and waits for 45–60 s before starting the next measurement.
BMI was computed by dividing body weight (kg) by height (m) squared [35]. At the conclusion of expiration, the umbilical level was chosen, and the waist size was measured [36]; when the waist circumference(WC) of women ≥ 85 cm, and men ≥ 90 cm, known as central obesity. Waist-height ratio (WHtR) was calculated by the ratio of WC to height [37]. Visceral adiposity index (VAI) was calculated using BMI, WC, TG and HDL-C, with different formulas for men and women [38]. It is important to note that VAI, Chinese visceral adiposity index (CVAI), lipid accumulation product index (LAP), and triglyceride-glucose (TyG) index were required to perform invasive manipulations to obtain TG and HDL-C. Other indicators were calculated using the following equations [18, 39,40,41,42,43,44,45].
Statistical analysis
Statistical Product Service Solutions (SPSS) software, version 25.0, was used to conduct the analyses (IBM SPSS, Armonk, NY, USA). By sex, sociodemographic traits were analyzed and percentages were provided. To compare the categorical variable distribution across sex, a chi-square test was utilized. The mean and standard deviation were used to express continuous variables. In order to evaluate the variations in mean distributions by sex, independent samples t-tests were utilized. The unadjusted and adjusted relationships between anthropometric and HTN were evaluated using binary logistic regression. We calculated odds ratios (ORs) and 95% confidence intervals (95%CI) adjusting for age, educational levels, marital status, live place, current smoking, alcohol drinking, activities, exercises, and chronic diseases. To determine the area under the curve (AUC) and 95% confidence interval as a predictor of hypertension, the receiver operating characteristic curve (ROC) was utilized [46]. The significance of the area under the curve is that an area greater than 0.9 indicates high accuracy, 0.7–0.9 indicates moderate accuracy, 0.5–0.7 indicates low accuracy, and 0.5 indicates a chance result [47]. The ROC curve can also be used to determine sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio. The Youden index, which is derived using the formula: [maximum (sensitivity + specificity-1)] [48], which is the maximum vertical distance between the ROC curve and the diagonal or chance line, determines the cut-off value of the predictor based on the highest value. Data were analyzed using chi-square test followed by Bonferroni correction to reassess the significance level.
Results
Table 1 shows the basic characteristics of the participants. A total of 4,423 subjects were included in this study, of whom 2038(46.10%) were male and 2385(53.90%) were female. Among them, there were significant differences between men and women in age, education, marital status, alcohol consumption, smoking, BMI, WHtR, VAI, ABSI, body roundness index (BRI), LAP, conicity index (CI), CVAI, TyG index, TyG-BMI, TyG-WC, TyG -WHtR (P < 0.05). However, the current residence, number of chronic diseases, exercise, taking a ctivities and WC were not statistically significant between the male and female subgroups (P > 0.05). Because of these significant differences between males and females (P < 0.05), we performed the main analyses separately by sex.
Table 2 shows the baseline characteristics of the study participants with and without future HTN by sex. According to the study's findings, during the four years, the incident rate of males with hypertension was 22.08%, while the incident rate of women with hypertension was 17.82%. Men with HTN had significant differences in age, current residence, smoking, alcohol consumption, WC, BMI, WHtR, VAI, ABSI, BRI, LAP, CI, CVAI, TyG index, TyG-BMI, TyG-WC and TyG-WHtR (P < 0.05); women with HTN had significant differences in age, education, marital status, WC, BMI, WHtR, VAI, ABSI, BRI, LAP, CI, CVAI, TyG index, TyG-BMI, TyG-WC and TyG-WHtR (P < 0.05). Data were analyzed using chi-square tests, and then Bonferroni adjustments were used to reassess the significance levels in Table 2. Among men, the incidence of hypertension was higher in the 65–74 years-old group compared with the 45–54 years-old group, the 55–64 years-old group, and the ≥ 75 years-old group (Using Bonferroni correction, run 6 comparisons, critical value P = 0.008, post-adjustment P < 0.008). The incidence was higher in participants who were former smokers compared to those who were current smokers (Using Bonferroni correction, run 3 comparisons, critical value P = 0.017, post-adjustment P < 0.017). Participants who drank alcohol more than once a month had a higher incidence compared to those who drank less than once a month (Using Bonferroni correction, run 3 comparisons, critical value P = 0.017, post-adjustment P < 0.017). The incidence rate of male living in urban is higher (P < 0.05). Among women, the incidence of hypertension was higher in the ≥ 75 years-old group than in the 45–54 years-old group, 55–64 years-old group, and 65–74 years-old group (Using Bonferroni correction, run 6 comparisons, critical value P = 0.008, post-adjustment P < 0.008). Illiterate participants were more likely to develop hypertension than participants with less than elementary or high school levels of literacy (Using Bonferroni correction, run 6 comparisons, critical value P = 0.008, post-adjustment P < 0.008). Married women have a higher incidence than single women (P < 0.05).
Table 3 shows the cut-off value between the area under curve, sensitivity, and specificity for obesity and lipid-related indices to detect HTN by sex. The ROC curves of each indicator in the prediction of HTN risk in men and women are shown in Figs. 1 and 2 respectively. The significance of the area under the curve is that an area greater than 0.9 indicates high accuracy, 0.7–0.9 indicates moderate accuracy, 0.5–0.7 indicates low accuracy, and 0.5 indicates a chance result [47]. As shown in the table and figures, among men, the WHtR was the best predictor of HTN in the middle-aged and elderly male population (AUC = 0.593, SE = 0.015, 95% CI [0.563,0.623], and optimal cutoffs = 0.501). Meanwhile, BRI (AUC = 0.593, SE = 0.015, 95%CI [0.563,0.623], and optimal cutoffs = 3.371) had similar predictive values. Moreover, among women, CVAI was the most accurate predictor of HTN in middle-aged and elderly women (AUC = 0.633, SE = 0.015, 95%CI [0.604,0.662], and optimal cutoffs = 99.405). All of the above indicators were statistically different (P < 0.05). From the overall data, the AUC values of the above thirteen indicators were higher than 0.5, indicating that they have predictive value for hypertension.
Table 4 shows the associations of obesity- and lipid-related indices with HTN. According to the values in Table 3, 13 obesity- and lipid-related indices were transformed into two-category variables in this investigation. Table 4 is based on the transformed variables. A larger OR, in general, suggests a higher risk factor. Both before and after adjusting for age, education, marital status, current residence, current smoking, alcohol drinking, social activity, exercise, and chronic disease counts, the odds of elevated BP increased progressively with increasing obesity and units of lipid measurement for both men and women. Each unit rise in WHtR, for example, was related with a 1.036-fold (95% CI:1.024,1.049) increase in the likelihood of developing hypertension in males. Each unit increase in CVAI was linked to a 1.009-fold increase in the likelihood of developing hypertension in women (95% CI:1.007,1.012). In addition, except for female ABSI, which had no significant significance after adjustment of confounding factors (P > 0.05), all other indexes had statistical significance after adjustment of confounding factors (P < 0.05). Figure 3 shows the forest diagram of or value before and after adjustment of confounding factors for males and females.
Discussion
Due to its great incidence and challenging management, hypertension has turned into a threat to public health. Around 1.4 billion individuals worldwide have hypertension, which has increased to 31.3% of the population between 2000 and 2010 [6]. Because of disparities in knowledge, treatment, and capacity to control hypertension, the incidence of hypertension has dropped by 2.6% in high-income nations while increasing by 7.7% in low- and middle-income countries. In a study in China [7], the incident rate of hypertension among Chinese adults was 23.2% from 2012 to 2015, even though the Chinese government has taken many proactive measures, such as providing Essential Public Health Services to screen for chronic diseases and increase the coverage of health insurance [49], limiting salt intake [50], the effect is still not satisfactory [4].
In obese individuals, adipocyte dysfunction contributes to vascular and systemic insulin resistance, as well as malfunction of the sympathetic nervous system and the renin–angiotensin–aldosterone system. It causes contraction of vascular smooth muscle, retention of water and sodium, and pressure increase. The long-term increase of cardiac output and blood volume will lead to the increase of systemic vascular resistance. The development of obesity-associated hypertension is also influenced by structural and functional changes in the kidney, such as the activation of intrarenal angiotensin II [51,52,53]. It has been shown that obese compared with non-obese hypertensive individuals exhibit higher renal sodium reabsorption, and perhaps in association with this functional change, higher total body water, plasma volume, and intracellular body water [54]. Visceral adipose tissue is also resistant to insulin and leptin and is the site of altered secretion of molecules and hormones such as adiponectin, leptin, resistin, tumor necrosis factor and interleukin-6, which exacerbate cardiovascular disease associated with obesity [55].
The incidence rate of hypertension can currently be predicted by the obesity index, according to numerous research. However, the findings of academic studies remain contradictory when taking into account racial factors [56] and variations in body composition. BMI is used as the most widely used anthropometric method in clinical and epidemiological studies [57, 58] to define obesity and overweight. However, BMI can't show the distribution characteristics of fat, and it is influenced by age, sex, and race [59], which also makes more scholars question its accuracy, and put forward many new anthropometric indicators.
In this study, the prediction ability of WHtR and Tyg-WHtR is modest. WHtR is a better indicator for detecting abdominal obesity than BMI and WC because it takes WC and height into account as a whole [60]. A study from Thailand [61] compared nine obesity indices with hypertension and showed that WHtR was the most practical measure of obesity associated with hypertension in both men and women.The WHtR recommended value for predicting hypertension is set to 0.5 [62]. Our research results show that WHtR = 0.501 has the strongest prediction effect, which is closer to the recommended value. It is basically consistent with the research results of other scholars [63, 64]. But some scholars pointed out that the people selected by this standard are mostly Asian people, and perhaps in non-Asian areas, this standard is not applicable due to the differences of race and human body composition [63]. A notion initially introduced by Ko et al. [65]is known as the Tyg index-related parameters, which integrate the TyG index with WC, BMI, and WHtR. Later, it was noted that [66] the combined index of TyG index and obesity index was superior to the single index and more useful in predicting the risk of hypertension development.
In our large national cohort study, we used ROC to determine the cut-off values for obesity and lipid-related indicators. The results of the study showed that women had higher cut-off values for the indicators compared to men. This may be related to the different body composition of men and women [67]. According to the values in Table 3, 13 obesity- and lipid-related indices were transformed into two-category variables in this investigation. The modified variables are used in Table 4. A larger OR, in general, suggests a higher risk factor. Before adjusting for potential confounders, the results of multivariate logistic regression models showed that the ORs of obesity and lipid-related indices were mostly higher in women than in men. However, after adjusting for potential confounders, the ORs of females decreased more than those of males, and even the ORs of some indicators were smaller than those of males. This can be partially explained by the fact that women may be more susceptible to potential confounders. The effect of these potential confounders on hypertension needs to be further investigated.
There are a few limitations to be aware of. First, the relationship should be studied prospectively. Second, we only considered the identified confounders. However, some unknown factors still existed. Thirdly, in order to avoid white-coat hypertension and occult hypertension, it is suggested to use out-of-office blood pressure assessment methods, such as ambulatory BP monitoring (ABPM) or home BP monitoring (HBPM), but our research method does not take this situation into account. Fourth, our results showed that the AUC values mostly hovered around 0.6, with low diagnostic accuracy. In future studies, we need to try to combine two or more indices to see if the diagnostic accuracy can be improved. Fifth, in our study, the sensitivity and specificity of these WHtR and Tyg-WHtR were indeed not high, so they were only modest predictors of hypertension, but in terms of area under the curve, they were indeed more cost-effective than the others. The advantages of this study are as follows: First, cohort research design, relatively large sample size and gender-specific analysis method provide guarantee for determining the causal relationship. Second, the study's huge sample of 4423 middle-aged and older Chinese is another important strength. The analytical approach that managed the various confounders is the last advantage.
Conclusion
In this cohort study, WHtR and Tyg-WHtR are the most cost-effective indicators with moderate predictive value of the development of HTN. In addition, when WHtR = 0.501 or TYg-WHtR = 4.335, the effect of predicting the incidence risk of men is the best, and when WHtR = 0.548 or TYg-WHtR = 4.781, the effect of predicting the incidence risk of women is the best.
Availability of data and materials
The datasets generated and/or analyzed during the current study are publicly available in the http://charls.pku.edu.cn/index.html repository.
Abbreviations
- CHARLS:
-
China Health and Retirement Longitudinal Study
- HTN:
-
Hypertension
- WC:
-
Waist circumference
- BMI:
-
Body mass index
- WHtR:
-
Waist-height ratio
- VAI:
-
Visceral adiposity index
- ABSI:
-
A body shape index
- BRI:
-
Body roundness index
- LAP:
-
Lipid accumulation product index
- CI:
-
Conicity index
- CVAI:
-
Chinese visceral adiposity index
- TyG-index:
-
Triglyceride-glucose index
- ROC:
-
Receiver operating characteristic curve
- AUC:
-
Area under curve
- HDL-C:
-
High-density lipoprotein cholesterol
- BP:
-
Blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TG:
-
Triglycerides
- FPG:
-
Fasting plasma glucose
- SPSS:
-
Statistical Product Service Solutions
- ORs:
-
Odds ratios
- CI:
-
Confidence interval
- SD:
-
Standard deviation
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52.
Islam JY, Zaman MM, Haq SA, Ahmed S, Al-Quadir Z. Epidemiology of hypertension among Bangladeshi adults using the 2017 ACC/AHA Hypertension Clinical Practice Guidelines and Joint National Committee 7 Guidelines. J Hum Hypertens. 2018;32(10):668–80.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390(10112):2549–58.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441–50.
Wang Z, Chen Z, Zhang L. Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344–56.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58.
Rahmouni K, Correia ML, Haynes WG, Mark AL. Obesity-associated hypertension: new insights into mechanisms. Hypertension. 2005;45(1):9–14.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Grootveld LR, Van Valkengoed IG, Peters RJ, Ujcic-Voortman JK, Brewster LM, Stronks K, Snijder MB. The role of body weight, fat distribution and weight change in ethnic differences in the 9-year incidence of hypertension. J Hypertens. 2014;32(5):990–6 (discussion 996-997).
Zhou W, Shi Y, Li YQ, Ping Z, Wang C, Liu X, Lu J, Mao ZX, Zhao J, Yin L, et al. Body mass index, abdominal fatness, and hypertension incidence: a dose-response meta-analysis of prospective studies. J Hum Hypertens. 2018;32(5):321–33.
Ortega FB, Sui X, Lavie CJ, Blair SN. Body Mass Index, the Most Widely Used But Also Widely Criticized Index: Would a Criterion Standard Measure of Total Body Fat Be a Better Predictor of Cardiovascular Disease Mortality? Mayo Clin Proc. 2016;91(4):443–55.
Liu J, Tse LA, Liu Z, Rangarajan S, Hu B, Yin L, Leong DP. Li WJJotAHA: Predictive values of anthropometric measurements for cardiometabolic risk factors and cardiovascular diseases among 44 048 Chinese. J Am Heart Assoc. 2019;8(16):e010870.
Ge Q, Qi Z, Xu Z, Li M, Zheng H, Duan X, Chu M, Zhuang X. Comparison of different obesity indices related with hypertension among different sex and age groups in China. Nutr Metab Cardiovasc Dis. 2021;31(3):793–801.
Janghorbani M, Aminorroaya A, Amini M. Comparison of Different Obesity Indices for Predicting Incident Hypertension. High Blood Press Cardiovasc Prev. 2017;24(2):157–66.
Shimotake Y, Mbelambela EP, Muchanga SM, Villanueva AF, Yan SS, Minami M, Shimomoto R, Lumaya AJ, Suganuma N. Comparative evaluation of anthropometric measurements and prevalence of hypertension: community based cross-sectional study in rural male and female Cambodians. Int J Environ Res Public Health. 2020;6(7):e04432.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012;7(7):e39504.
Cheung YB. “A Body Shape Index” in middle-age and older Indonesian population: scaling exponents and association with incident hypertension. PLoS One. 2014;9(1):e85421.
Li Y, Zhai F, Wang H, Wang Z. A four-year prospective study of the relationship between body mass index and waist circumstances and hypertension in Chinese adults. J Hygiene Res. 2007;36(4):478–80.
Sadeghi M, Talaei M, Gharipour M, Oveisgharan S, Nezafati P, Dianatkhah M, Sarrafzadegan N. Anthropometric indices predicting incident hypertension in an Iranian population: The Isfahan cohort study. Anatol J Cardiol. 2019;22(1):33–43.
Wang Y, Liu W, Sun L, Zhang Y, Wang B, Yuan Y, Li T, Yao R, Han H, Qian Q, et al. A novel indicator, childhood lipid accumulation product, is associated with hypertension in Chinese children and adolescents. Hypertens Res. 2020;43(4):305–12.
Wang C, Fu W, Cao S, Xu H, Tian Q, Gan Y, Guo Y, Yan S, Yan F, Yue W, et al. Association of adiposity indicators with hypertension among Chinese adults. Nutr Metab Cardiovasc Dis. 2021;31(5):1391–400.
Wang Y, Yang W, Jiang X. Association Between Triglyceride-Glucose Index and Hypertension: A Meta-Analysis. Front Cardiovasc Med. 2021;8:644035.
Li C, Liu T, Sun W, Wu L, Zou ZY. Prevalence and risk factors of arthritis in a middle-aged and older Chinese population: the China health and retirement longitudinal study. Rheumatology (Oxford). 2015;54(4):697–706.
Zhang L, Li JL, Guo LL, Li H, Li D, Xu G. The interaction between serum uric acid and triglycerides level on blood pressure in middle-aged and elderly individuals in China: result from a large national cohort study. BMC Cardiovasc Disord. 2020;20(1):174.
Zhang L, Li JL, Zhang LL, Guo LL, Li H, Li D. No association between C-reactive protein and depressive symptoms among the middle-aged and elderly in China: Evidence from the China Health and Retirement Longitudinal Study. Medicine (Baltimore). 2018;97(38):e12352.
Zhang L, Li JL, Zhang LL, Guo LL, Li H, Li D. Body mass index and serum uric acid level: Individual and combined effects on blood pressure in middle-aged and older individuals in China. Medicine (Baltimore). 2020;99(9):e19418.
Zhang L, Li JL, Zhang LL, Guo LL, Li H, Yan W, Li D. Relationship between adiposity parameters and cognition: the “fat and jolly” hypothesis in middle-aged and elderly people in China. Medicine (Baltimore). 2019;98(10):e14747.
Zhang L, Liu K, Li H, Li D, Chen Z, Zhang LL, Guo LL. Relationship between body mass index and depressive symptoms: the “fat and jolly” hypothesis for the middle-aged and elderly in China. BMC Public Health. 2016;16(1):1201.
Zhang L, Yang L, Wang C, Yuan T, Zhang D, Wei H, Li J, Lei Y, Sun L, Li X, et al. Individual and combined association analysis of famine exposure and serum uric acid with hypertension in the mid-aged and older adult: a population-based cross-sectional study. BMC Cardiovasc Disord. 2021;21(1):420.
Zhang L, Li JL, Zhang LL, Guo LL, Li H. Li DJBRI: Association and Interaction Analysis of Body Mass Index and Triglycerides Level with Blood Pressure in Elderly Individuals in China. Biomed Res Int. 2018;2018:1–31.
Kerner W, Bruckel J, German Diabetes A. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2014;122(7):384–6.
Barbalho SM, Tofano RJ, de Oliveira MB, Quesada KR, Barion MR, Akuri MC, Oshiiwa M, Bechara MD. HDL-C and non-HDL-C levels are associated with anthropometric and biochemical parameters. J Vasc Bras. 2019;18:e20180109.
Lee JJ, Ahn J, Hwang J, Han SW, Lee KN, Kim JB, Lee S, Na JO, Lim HE, Kim JW, et al. Relationship between uric acid and blood pressure in different age groups. Clin Hypertens. 2015;21:14.
Zhang L, Yang L, Wang C, Yuan T, Zhang D, Wei H, Li J, Lei Y, Sun L, Li X, et al. Combined Effect of Famine Exposure and Obesity Parameters on Hypertension in the Midaged and Older Adult: A Population-Based Cross-Sectional Study. Biomed Res Int. 2021;2021:5594718.
Zhang FL, Ren JX, Zhang P, Jin H, Qu Y, Yu Y, Guo ZN, Yang Y. Strong Association of Waist Circumference (WC), Body Mass Index (BMI), Waist-to-Height Ratio (WHtR), and Waist-to-Hip Ratio (WHR) with Diabetes: A Population-Based Cross-Sectional Study in Jilin Province. China J Diabetes Res. 2021;2021:8812431.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, Galluzzo A, AlkaMeSy Study G. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–2.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, Maeda Y, McDougall A, Peterson CM, Ravussin E, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring). 2013;21(11):2264–71.
Kahn HS. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord. 2005;5:26.
Xia M-F, Chen Y, Lin H-D, Ma H, Li X-M, Aleteng Q, Li Q, Wang D, Hu Y. Pan B-sJSr: A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese. Sci Rep. 2016;6(1):1–8.
Rato Q. Conicity index: An anthropometric measure to be evaluated. Rev Port Cardiol. 2017;36(5):365–6.
Unger G, Benozzi SF, Perruzza F, Pennacchiotti GL. Triglycerides and glucose index: a useful indicator of insulin resistance. Endocrinol Nutr. 2014;61(10):533–40.
Selvi NMK, Nandhini S, Sakthivadivel V, Lokesh S, Srinivasan AR, Sumathi S. Association of Triglyceride-Glucose Index (TyG index) with HbA1c and Insulin Resistance in Type 2 Diabetes Mellitus. Maedica (Bucur). 2021;16(3):375–81.
Jiang C, Yang R, Kuang M, Yu M, Zhong M, Zou Y. Triglyceride glucose-body mass index in identifying high-risk groups of pre-diabetes. Lipids Health Dis. 2021;20(1):161.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36.
Fischer JE, Bachmann LM, Jaeschke R. A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med. 2003;29(7):1043–51.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J. 2005;47(4):458–72.
Meng Q, Xu L, Zhang Y, Qian J, Cai M, Xin Y, Gao J, Xu K, Boerma JT, Barber SL. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–14.
Wang M, Moran AE, Liu J, Coxson PG, Penko J, Goldman L, Bibbins-Domingo K, Zhao D. Projected Impact of Salt Restriction on Prevention of Cardiovascular Disease in China: A Modeling Study. PLoS One. 2016;11(2):e0146820.
Kurukulasuriya LR, Stas S, Lastra G, Manrique C. America JRSJMCoN: Hypertension in Obesity. Medical Clinics of North America. 2011;95(5):903–17.
Sharma AMJH. Is there a rationale for angiotensin blockade in the management of obesity hypertension? Hypertension. 2004;44(1):12–9.
Sowers JRJH. Diabetes mellitus and vascular disease. Hypertension. 2013;61(5):943–7.
Hall JE, Brands MW, Henegar JR. Mechanisms of Hypertension and Kidney Disease in Obesity. Ann N Y Acad Sci. 1999;892(1):91–107.
DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol. 2014;10(6):364–76.
Harris MM, Stevens J, Thomas N, Schreiner P. Associations of fat distribution and obesity with hypertension in a bi-ethnic population: the ARIC study. Atherosclerosis Risk in Communities Study. Obes Res. 2000;8(7):516–24.
Nuttall FQ. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015;50(3):117–28.
Seo DC, Choe S, Torabi MR. Is waist circumference >/=102/88cm better than body mass index >/=30 to predict hypertension and diabetes development regardless of gender, age group, and race/ethnicity? Meta-analysis Prev Med. 2017;97:100–8.
Jackson AS, Stanforth PR, Gagnon J, Rankinen T, Leon AS, Rao DC, Skinner JS, Bouchard C, Wilmore JH. The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. INT J OBESITY. 2002;26(6):789–96.
Ashwell M, Gunn P. Gibson SJOr: Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–86.
Nguyen Ngoc H, Kriengsinyos W, Rojroongwasinkul N. Aekplakorn WJJoCD, Disease: Association of adiposity indices with hypertension in middle-aged and elderly Thai population: National Health Examination Survey 2009 (NHES-IV). J Cardiovasc Dev Dis. 2019;6(1):13.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23(2):247–69.
Choi JR, Koh SB, Choi E. Waist-to-height ratio index for predicting incidences of hypertension: the ARIRANG study. BMC Public Health. 2018;18(1):767.
Jayawardana R, Ranasinghe P, Sheriff MH, Matthews DR, Katulanda P. Waist to height ratio: a better anthropometric marker of diabetes and cardio-metabolic risks in South Asian adults. Diabetes Res Clin Pract. 2013;99(3):292–9.
Er L-K, Wu S, Chou H-H, Hsu L-A, Teng M-S, Sun Y-C. Ko Y-LJPo: Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS One. 2016;11(3):e0149731.
Wang K, He G, Zhang Y, Yin J, Yan Y, Zhang Y. Wang KJJoHH: Association of triglyceride-glucose index and its interaction with obesity on hypertension risk in Chinese: a population-based study. J Hum Hypertens. 2021;35(3):232–9.
Bredella MA. Sex Differences in Body Composition. Adv Exp Med Biol. 2017;1043:9–27.
Acknowledgements
The authors would like to thank the members of the CHARLS as well as all participants for their contribution.
Funding
This work was supported by the NSFC (70910107022, 71130002) and National Institute on Aging (R03-TW008358-01; R01-AG037031-03S1), World Bank (7159234), and the publication fee was supported by the Support Program for Outstanding Young Talents from the Universities and Colleges of Anhui Province for Lin Zhang(gxyqZD2021118).
Author information
Authors and Affiliations
Contributions
Conceived and designed the research: LZ. Wrote the paper: Y-q L. Analyzed the data: Y-q L and LZ. Revised the paper: Y-q L, J-f G, X–y Z, YW, Y-j M, XY, LZ, H-y L, L-l G, J-l L, Y-x L, X-p L, LS, LY, TY, C-z W, D-m Z, H–h W, JL, M-m L, and YH. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All data are openly published as microdata at http://charls.pku.edu.cn/index/zh-cn.html with no direct contact with all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Gui, J., Zhang, X. et al. Predicting hypertension by obesity- and lipid-related indices in mid-aged and elderly Chinese: a nationwide cohort study from the China Health and Retirement Longitudinal Study. BMC Cardiovasc Disord 23, 201 (2023). https://doi.org/10.1186/s12872-023-03232-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03232-9